Abstract
Rapid antifungal susceptibility testing for the antifungal agent caspofungin can be performed using flow cytometry (FC). An FC procedure using acridine orange provided minimum inhibitory concentration (MIC) results within 7 to 9 h which were compared with results obtained using the NCCLS M27-A2 protocol. To evaluate the consistency of this method, susceptibility testing using caspofungin was performed using 73 isolates of eight different species of Candida from various clinical samples in Central California. Macrotiter or microdilution tests were performed according to the NCCLS M27-A2 protocol, and the MICs were compared to those provided by our flow cytometry method. All isolates tested had results within the sensitive interpretive category, and 90% of the results compared within 1 dilution, showing excellent agreement between the methods. The MIC at which 50% of the isolates tested were inhibited (MIC50) and the MIC90 of caspofungin for all eight Candida species were within 1 dilution. This flow cytometer 7-h protocol for testing the antifungal susceptibility of Candida species to caspofungin provided results equivalent to those obtained with the M27-A2 protocol.
With the introduction of new antifungal agents and the increase in the incidence and severity of yeast infections due to Candida species, the need for antifungal susceptibility testing has become increasingly important. Developing rapid and accurate testing methods would increase the information available to guide the treatment of many critically ill patients. The use of flow cytometry (FC) for more-rapid results has been discussed in several articles (3, 4, 5, 12) as a way to improve the availability of results.
Understanding the mode of action of the antifungal agents helps explain the reactions seen with in vitro testing methods. For example, the mode of action of fluconazole and many other fungistatic antifungal agents is against ergosterol (13), a major component of the yeast cell membrane. This action compromises the cell membrane integrity and inhibits future cell reproduction. Another type of reaction is seen with caspofungin, which inhibits cell wall 1,3-d-beta-glucan synthesis, resulting in a fungicidal reaction (7, 9). The cell destruction from caspofungin often causes the yeast cell to lyse, leaving nearly total clearing in the susceptibility-testing dilutions at the minimum inhibitory concentration (MIC) level, and a near-total absence of cells available to count on the flow cytometer after a 7-h incubation. Due to the fungicidal action of the antifungal agent caspofungin, slight adaptations in the use of the flow cytometry method used for fluconazole testing are needed to accommodate the reactions seen in the various Candida species when testing with caspofungin.
Use of the flow cytometer is an improvement in antifungal susceptibility testing methodology, since it provides rapid and quantifiable results that are equivalent to the results obtained with the NCCLS M27-A2 (6) macrodilution and microdilution methods. The FC results are easily available within 7 to 9 h instead of the 24 to 48 h needed for the standard NCCLS method. After testing several method variations using other dyes, a method using acridine orange (AO) dye with a 7- to 9-h incubation was chosen, because the method is easy to perform and the results are consistent for all yeast species we tested. Previous publications and studies have shown that flow cytometry worked for the testing of Candida albicans and fluconazole or amphotericin B (3, 4, 8, 12), but no results had been published showing that the method could be modified for testing the fungicidal ability of caspofungin.
MATERIALS AND METHODS
Preparation of reagents.
RPMI 1640 containing l-glutamine without bicarbonate, buffered to pH 7.0 with 0.165 morpholinepropanesulfonic acid (MOPS) buffer (Cambrex, Walkersville, MD), was purchased ready to use. AO dye (Hardy, Santa Maria, Calif.) was diluted to a 0.83 μg/ml solution with deionized water.
Preparation of antifungal dilutions.
Caspofungin (Merck Co., Whitehouse Station, Pa.) used in the susceptibility testing panels for the flow cytometry study and that of the NCCLS reference method was diluted with RPMI 1640 containing l-glutamine without bicarbonate, buffered to pH 7.0 with 0.165 MOPS buffer (Cambrex, Walkersville, MD), following the NCCLS protocol. The concentrations for caspofungin covered the MIC range of 0.016 to 8 μg/ml.
Organisms and inoculum preparation.
Eight different Candida species were collected from various hospital laboratories in the San Joaquin Valley of California. The 73 isolates included 20 of C. albicans, 25 of C. glabrata, 12 of C. tropicalis, 8 of C. parapsilosis, 3 of C. krusei, 3 of C. lusitaniae, 1 of C. lipolytica, and 1 of C. zeylenoides. Isolates were stored on Sabouraud dextrose agar and passed at least twice to stimulate activity of growth.
The inocula were prepared from 18- to 24-h cultures of Candida isolates grown on Sabouraud dextrose agar (Hardy Diagnostics, Santa Maria, CA.). For micro- and macrodilution testing, the inocula were prepared in saline and adjusted spectrophotometrically to correspond to a 0.5 McFarland standard with approximately 5 × 106 yeast cells/ml. The suspensions were further diluted to a ratio of 1:100 in 5 ml sterile saline for the macrotube method or 1:50 for the microdilution method and then diluted to a ratio of 1:20 in RPMI 1640. Each dilution was vortexed for 30 seconds before proceeding.
The saline suspension inoculum for flow cytometry testing was slightly heavier than a 0.5 McFarland standard, and fewer dilution steps were needed. The initial inoculum of approximately 5 × 107 cells/ml was diluted to a ratio of 1:10 in RPMI 1640 and vortexed for 30 seconds.
Quality control and test specimens.
The control organisms, C. krusei (ATCC 6258) and C. parapsilosis (ATCC 20019), were used for each batch of tests for the macrotube, microdilution, and flow cytometer methods. Since there are no firm NCCLS-approved quality control ranges for caspofungin, previously published quality control ranges for caspofungin were used (2). Caspofungin susceptibility category interpretation followed suggested criteria published previously (9, 10).
Susceptibility test: NCCLS.
The macrodilution testing tubes for the NCCLS method were set up following the M27-A2 protocol, where 0.9 ml of the yeast inoculum (103 yeast cells/ml) in RPMI 1640 was added to each tube containing a 0.1-ml serial twofold dilution of the antifungal agent. Tubes were capped loosely, mixed, and incubated at 35°C in ambient air for a total of 48 h. The caspofungin MIC result was taken from the first tube exhibiting a prominent clearing or inhibition of growth at 24 h (7, 11). The microdilution NCCLS testing was set up following the M27-A2 protocol, in which 0.1 ml of the yeast inoculum in RPMI 1640 was added to each well containing a 0.1-ml serial twofold dilution of the antifungal agent. Plates were covered loosely and incubated at 35°C in ambient air for 48 h. Results were read at 24 and rechecked at 48 h. The caspofungin MIC result was taken from the first well showing a prominent inhibition of growth at 24 h compared to the growth control.
Susceptibility test: flow cytometer with AO dye.
Dilution tubes for flow cytometer testing were prepared by adding 0.9 ml of yeast inoculum (approximately 106 yeast cells/ml) in RPMI 1640 to 0.1 ml of the serial twofold dilutions of antifungal agent. Candida glabrata, which reproduces rapidly, required an additional 1:6 dilution in RPMI 1640 before being added to the antifungal tubes to keep the results in the countable range.
The tubes were capped loosely, mixed, and incubated at 35°C in ambient air for about 7 h. After incubation, 100 μl of a 0.83-μg/ml AO dye solution was added to the 1 ml of antifungal/yeast cell mixture. Tubes were incubated for 15 min at room temperature while protected from light. For each isolate, the live control tube was read first, with a gating region set to include at least 90% of the yeast cell population. The MIC was interpreted as the concentration of antifungal agent causing a substantial shift of cells (>50%) outside of the live gate or a substantial decrease in the number of events per second. A total of 5,000 cells were counted if cells were intact. If yeast cells were disintegrated, counting was performed for approximately 3 min to measure the number of events per second.
Flow cytometer settings.
The Becton Dickinson FACScan flow cytometer evaluation was performed using FACScan CellQuest software. Readings were in the log/log mode with an argon laser (488 nm). The FSC threshold was set at 052, and the detector was set on E00. Data were collected for side scatter versus green fluorescence at 500 to 560 nm.
RESULTS
Flow cytometry using AO dye was tested for efficacy to improve antifungal susceptibility testing. Our investigation used 73 isolates from eight species of Candida to evaluate testing of caspofungin by the flow cytometry method. These results were compared to results obtained using the NCCLS M27-A2 reference method. Quality control organism results for all methods were within the NCCLS-accepted ranges for susceptibility testing.
On the flow cytometer, the method of reading endpoints for caspofungin was different from the method used for fungistatic reactions. A typical pattern for flow cytometry results of a nonfungicidal reaction shows the movement of the injured yeast cells to an area outside of the live gate when the antifungal concentration is high enough to damage the cell membrane. With fungicidal reactions, this can look very different, since the cells often disintegrate into debris as the concentration of the antifungal agent increases. The endpoint then becomes the concentration of antifungal agent that demonstrates a drastic decrease in the counted number of events per second.
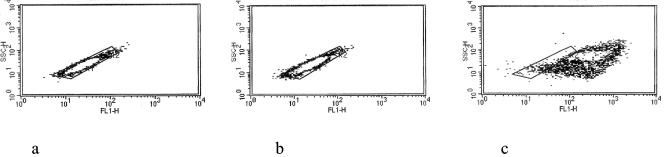
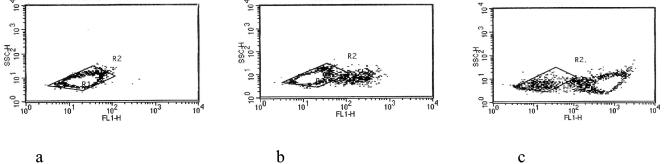
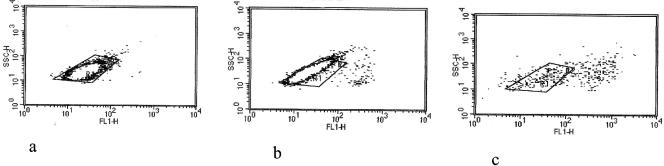
Flexibility in reading the MIC was necessary, since two different types of reactions could be seen. One reaction is shown in Fig. 1 and 2. Figure 1, with the results for C. albicans with caspofungin, showed a movement outside of the live gate. Not evident from the picture is the fact that the number of counted events per second decreased from approximately 1,400 in both the live control and the 0.125-μg/ml specimen to 120 in the 0.25-μg/ml tube. This same type of reaction is seen in Fig. 2, with results for C. glabrata. The dead or damaged yeast cells moved outside the live gate, but there was also a prominent decrease in the number of yeast cells available to count. An application of the other type of reaction showing lysis without enough cells to count at the MIC is shown in Fig. 3, which shows results for C. krusei. Counting, which had taken just seconds with the live control, now took several minutes, because there were so few intact cells in the solution.
FIG. 1.
Density plots showing the response of C. albicans to caspofungin. The live gated area counted 1,400 events per second with 98.7% gated (a), the 0.125 μg/ml caspofungin dilution counted 1,430 events per second with 95.9% gated (b), and the 0.25 μg/ml caspofungin dilution counted 120 events per second with 6.8% gated (c). Note that plots a and b show clear areas in the middles of the gated regions; these are due to heavy concentrations of points at those sites on the graphs.
FIG. 2.
Density plots showing the response of C. glabrata to caspofungin. The live gated area counted 2,160 events per second with 98.7% in the gate (a), the 0.125 μg/ml caspofungin dilution counted 2,200 events per second with 88% gated (b), and the 0.25 μg/ml caspofungin dilution counted 120 events per second with 11.8% gated (c). Note that plots a and b show clear areas in the middles of the gated regions; these are due to heavy concentrations of points at those sites on the graphs.
FIG. 3.
Density plots showing the response of C. krusei to caspofungin. The live gated area counted 560 events per second with 98.2% in the live gate (a), the 0.125 μg/ml caspofungin dilution counted 440 events per second with 93.5% gated (b), and the 0.25 μg/ml caspofungin dilution counted very few events per second with 44.3% events gated (c). Note that plots a and b show clear areas in the middles of the gated regions; these are due to heavy concentrations of points at those sites on the graphs.
For the 73 isolates tested with caspofungin, 90% of the flow cytometry results were within 1 twofold dilution of the NCCLS results, and 100% of the results were within 2 dilutions. Table 1 shows the comparison of the MIC results obtained by the two testing methods for the Candida isolates. The results with the flow cytometry mode for the MICs were 1 dilution lower than those with the NCCLS testing mode in our laboratory. This difference was likely seen because the flow cytometer could detect cellular damage more quickly than we could detect with visual observation of microtiter plates or macrotiter tubes. Table 2 shows the range of MIC results by species. When comparing the two testing methods for caspofungin, the range of results for all Candida species showed the MICs at which 50% of the isolates tested were inhibited (MIC50s) and the MIC90s were within 1 twofold dilution. Table 3 shows a comparison of the MIC50s and the MIC90s by species. All results for caspofungin were within the MIC range of 0.125 to 1.0 μg/ml and were consistent with other published results for caspofungin testing of Candida species (1). The recommended dosing of caspofungin results in plasma concentrations in excess of 8 μg/ml. All MICs in this study were less than four times the estimated plasma concentration and would be considered susceptible (9).
TABLE 1.
Caspofungin MIC distributions with the flow cytometry method and the NCCLS reference method
| Testing method | % MIC distribution at the following concn of caspofungin (μg/ml)a:
|
|||
|---|---|---|---|---|
| 0.125 | 0.25 | 0.5 | 1.0 | |
| NCCLS reference | 27 | 85 | 100 | |
| Flow cytometry | 29 | 82 | 100 | |
Dilutions of 0.063, 2.0, and 4.0 μg/ml were not tested.
TABLE 2.
Ranges of caspofungin MIC results for Candida species
| Candida species | Caspofungin MIC range (μg/ml) with:
|
|
|---|---|---|
| Flow cytometry | NCCLS reference method | |
| C. albicans | 0.125-0.5 | 0.25-1 |
| C. glabrata | 0.125-0.5 | 0.25-0.5 |
| C. tropicalis | 0.125-0.25 | 0.25-0.5 |
| C. parapsilosis | 0.25-0.5 | 0.5-1 |
| C. krusei | 0.25-0.5 | 0.5-1 |
| C. lusitaniae | 0.25-0.5 | 0.5-1 |
| C. lipolytica | 0.5 | 1 |
| C. zeylanoides | 0.25 | 0.5 |
TABLE 3.
Caspofungin MICs
| Candida species | No. tested | Flow cytometry
|
NCCLS reference method
|
||
|---|---|---|---|---|---|
| MIC50a | MIC90a | MIC50 | MIC90 | ||
| C. albicans | 20 | 0.25 | 0.25 | 0.5 | 0.5 |
| C. glabrata | 25 | 0.25 | 0.25 | 0.5 | 0.5 |
| C. tropicalis | 12 | 0.125 | 0.25 | 0.25 | 0.5 |
| C. parapsilosis | 8 | 0.5 | 0.5 | 1 | 1 |
| C. krusei | 3 | 0.5 | 0.5 | 1 | 1 |
| C. lusitaniae | 3 | 0.5 | 0.5 | 0.5 | 1 |
| C. lipolytica | 1 | 0.5 | 0.5 | 1 | 1 |
| C. zeylanoides | 1 | 0.25 | 0.25 | 0.5 | 0.5 |
Values are in micrograms per milliliter.
DISCUSSION
The results obtained by our study support the use of flow cytometry to provide clearly defined results for rapid antifungal susceptibility. Using clinical samples, we have shown that this method was useful for susceptibility testing of caspofungin with eight Candida species. To make the FC method flexible for all Candida species and antifungal agents, slight variations in the criteria for reading the MIC endpoints were needed. The main variation was in reading FC results for isolates that lyse when exposed to increasing levels of antifungal agents such as caspofungin. Since there was an insufficient number of intact cells in the sample after incubation, the yeast cells often could not show migration outside of the live gated area with increasing antifungal concentration but did show a drastic decrease in the number of events per second (3, 4, 5). Therefore, demonstrating a sudden decrease in the number of events per second between the live control and the test that contained an effective concentration of caspofungin provided an accurate designation of the MIC. The events-per-second method of reading results works well for caspofungin testing when a migration out of the live gate of the density plot cannot be evaluated due to a low count of intact cells. Preliminary testing with amphotericin B, another antifungal agent, suggests results could be evaluated using the same criteria as those used when testing caspofungin. The usual reaction seen with the fungistatic antifungal agent fluconazole was a movement outside the live gate with the same number of events per second maintained. Understanding the actions of antifungal agents is needed to correctly interpret the MIC test results.
Flow cytometry testing with AO dye meets the criterion of providing results comparable to the NCCLS microdilution or macrodilution methods and the interpretation criterion of having readings that show a significant change at the MIC endpoint, as recommended by the NCCLS M27-A2 macrotube method. An incubation time of 7 to 9 h was used, because this timing had been verified in our previous studies with other antifungal agents to work well with flow cytometry and AO dye. This incubation time produces clearly definable changes in the flow cytometer density plot and event-per-second statistics. A shorter incubation time of 2 to 4 h, as suggested by other investigators (3, 4), might also work with AO dye, but adjustments in reading the MICs would need to be made to fit the cell reactions at that point in their impairment.
Since FC susceptibility testing has the flexibility to cover different types of cellular reactions while providing clearly defined MICs, it should be given serious consideration as an acceptable method. Aside from the initial capital required for instrument purchase, testing is inexpensive. Because of the shorter incubation time needed to show prominently detectable levels of cellular damage, the results are available to the physician in 7 to 9 h instead of 24 h.
With the high incidence of infections from various Candida species, the rapid availability of information is helpful in directing appropriate treatment for seriously ill patients. MICs can play an important role in the management of candidiasis when clinical failure with standard drug dosing is observed. Changes in the resistance patterns of the different Candida species should be monitored to provide information for empirical treatment, since many species are known to be more resistant to routine azole treatment. Susceptibility testing of yeasts with flow cytometry is a flexible method that can be modified for fungistatic and fungicidal reactions to provide rapid and accurate MIC results for guiding the treatment of seriously ill patients.
Acknowledgments
We thank Merck & Co., Inc., and the College of Science and Mathematics, California State University, Fresno, for funding portions of this study.
REFERENCES
- 1.Bachmann, S. P., T. F. Patterson, and J. L. Lopez-Ribot. 2002. In vitro activity of caspofungin (MK-0991) against Candida albicans clinical isolates displaying different mechanisms of azole resistance. J. Clin. Microbiol. 40:2228-2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barry, A. L., M. A. Pfaller, S. D. Brown, A. Espinel-Ingroff, M. A. Ghannoum, C. Knapp, R. P. Rennie, J. H. Rex, and M. G. Rinaldi. 2000. Quality control limits for broth microdilution susceptibility tests of ten antifungal agents. J. Clin. Microbiol. 38:3457-3459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chaturvedi, V., R. Ramani, and M. A. Pfaller. 2004. Collaborative study of the NCCLS and flow cytometry methods for antifungal susceptibility testing of Candida albicans. J. Clin. Microbiol. 42:2249-2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chaturvedi, V., and R. Ramani. 2000. Flow cytometry antifungal susceptibility testing of pathogenic yeasts other than Candida albicans and comparison with the NCCLS broth microdilution test. Antimicrob. Agents Chemother. 44:2752-2758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kirk, S. M., S. M. Callister, L. C. M. Lim, and R. F. Schell. 1997. Rapid susceptibility testing of Candida albicans by flow cytometry. J. Clin. Microbiol. 35:358-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Committee for Clinical Laboratory Standards. 2002. Reference method for broth dilution antifungal susceptibility testing of yeasts. M27-A2. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 7.Odds, F. C., M. Motyl, R. Andrade, J. Bille, E. Canton, M. Cuenca-Estrella, A. Davidson, C. Durussel, D. Ellis, E. Foraker, A. Fothergill, M. A. Ghannoum, R. A. Giacobbe, M. Gobernado, R. Handke, M. Laverdiere, W. Lee-Yang, W. G. Merz, L. Ostrosky-Zeichner, J. Peman, S. Perea, J. R. Perfect, M. A. Pfaller, L. Proia, J. H. Rex, M. G. Rinaldi, J. Rodriguez-Tudella, W. Schell, C. Shields, D. A. Sutton, P. E. Verweij, and D. W. Warnock. 2004. Interlaboratory comparison of results of susceptibility testing with caspofungin against Candida and Aspergillus species. J. Clin. Microbiol. 42:3475-3482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O'Gorman, M. R. G., and R. L. Hopfer. 1991. Amphotericin B susceptibility testing of Candida species by flow cytometry. Cytometry 12:743-747. [DOI] [PubMed] [Google Scholar]
- 9.Pfaller, M. A., D. J. Diekema, S. A. Messer, R. J. Hollis, and R. N. Jones. 2003. In vitro activities of caspofungin compared with those of fluconazole and itraconazole against 3,959 clinical isolates of Candida spp., including 157 fluconazole-resistant isolates. Antimicrob. Agents Chemother. 47:1068-1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pfaller, M. A., S. A. Messer, L. Boyken, C. Rice, S. Tendolkar, R. J. Hollis, and D. J. Diekema. 2003. Caspofungin activity against clinical isolates of fluconazole-resistant Candida. J. Clin. Microbiol. 41:5729-5731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pfaller, M. A., S. A. Messer, L. Boyken, C. Rice, S. Tendolkar, R. J. Hollis, and D. J. Diekema. 2004. Further standardization of broth microdilution methodology for in vitro susceptibility testing of caspofungin against Candida species by use of an international collection of more than 3,000 clinical isolates. J. Clin. Microbiol. 42:3117-3119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wenisch, C., K. F. Linnau, B. Parschalk, K. Zedtwitz-Lieberwstein, and A. Georgopoulos. 1997. Rapid susceptibility testing of fungi by flow cytometry using vital staining. J. Clin. Microbiol. 35:5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.White, T. C., K. A. Marr, and R. A. Bowden. 1998. Clinical, cellular, and molecular factors that contribute to antifungal drug resistance. Clin. Microbiol. Rev. 11:382-402. [DOI] [PMC free article] [PubMed] [Google Scholar]