Abstract
Although the most common surgical treatment for traumatic anterior shoulder instability is arthroscopic Bankart repair (ABR), which has shown good postoperative results, a potential risk of postoperative external rotation deficit exists. For overhead-throwing athletes, recovery of postoperative range of motion during abduction and external rotation is essential to return to preinjury performance levels. We consider that the key to returning to play after ABR on the dominant side in overhead-throwing athletes is to simultaneously gain anterior stability and mobility of the shoulder. However, no gold standard method for determining the appropriate tension of the glenohumeral capsular ligaments in overhead-throwing athletes exists. This Technical Note presents the dynamic anterior glenohumeral capsular ligament tensioning in the abduction and external rotation positions during ABR for the dominant side in overhead-throwing athletes. We consider this surgical technique to be reliable for traumatic anterior instability of the dominant shoulder in athletes who wish to return to overhead-throwing sports.
Technique Video
Traumatic instability of the dominant shoulder in overhead-throwing athletes is an uncommon but complex condition. Surgical management of traumatic shoulder instability on the dominant side in overhead-throwing athletes has been reported to have a lower rate of recurrent dislocation compared with that observed with contact or collision athletes.1 However, recent studies have shown that the postoperative return to the same level of performance in overhead-throwing athletes with traumatic shoulder dislocation on the throwing side is less satisfactory, with rates ranging from 45% to 68%.1, 2, 3, 4
The tension in an overhead thrower’s shoulder should be sufficiently lax to allow excessive external rotation in abduction in the late cocking phase while maintaining stability, referred to as the “thrower’s shoulder paradox.”5 Therefore, postoperative instability or deficit in abduction and external rotation (ABER) would cause unsatisfactory surgical results.2,5,6 We believe that it is essential to restore whole anterior glenohumeral ligament retensioning, including the inferior glenohumeral ligament (IGHL) and middle glenohumeral ligament (MGHL), after arthroscopic Bankart repair (ABR) with less restriction of external rotation in the shoulders of overhead-throwing athletes during abduction. However, no gold standard method for determining the appropriate tension of the glenohumeral capsular ligaments in overhead-throwing athletes exists. In this Technical Note, we describe dynamic anterior glenohumeral ligament tensioning (DAGHT) in the ABER position during ABR in overhead-throwing athletes with traumatic shoulder dislocation on the dominant side.
Surgical Technique
This study was approved by the institutional review board (approval number 2301); all patients provided informed consent regarding participation and publication of the study (August 24, 2023). Our surgical technique is demonstrated in Video 1. Surgical indications are summarized in Table 1. Pearls and pitfalls of the surgical technique are summarized in Table 2, and the advantages and disadvantages are listed in Table 3.
Table 1.
Surgical Indications of DAGHT in the ABER Position During ABR on the Dominant Side of Overhead-throwing Athletes
|
ABER, abduction and external rotation; ABR, arthroscopic Bankart repair; DAGHT, dynamic anterior glenohumeral capsular ligament tensioning.
Table 2.
Pearls and Pitfalls of DAGHT in ABER Position During ABR for the Dominant Side in Overhead-Throwing Athletes
Pearls
|
ABER, abduction and external rotation; ABR, arthroscopic Bankart repair; DAGHT, dynamic anterior glenohumeral capsular ligament tensioning; MGHL, middle glenohumeral ligament.
Table 3.
Advantages and Disadvantages of the Surgical Technique
Advantages
|
Anesthesia and Positioning
Both shoulders are preoperatively examined for range of motion and laxity under general anesthesia. An interscalene block is administered to control postoperative pain. Patients are placed in a beach-chair position using a spider limb positioner (Smith & Nephew, Memphis, TN).
Portals and Arthroscopic Diagnosis
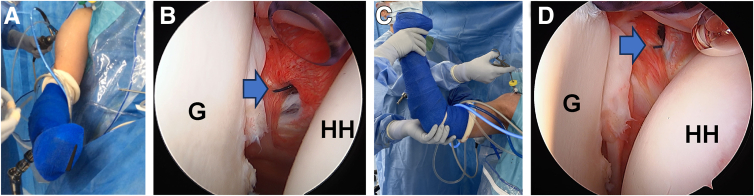
Standard anterior, anterosuperior, and posterior portals are used in all patients. The presence of glenohumeral joint pathologies such as capsulolabral lesions (Fig 1), glenoid defects, glenohumeral ligaments, Hill-Sachs lesions, SLAP lesions, and articular side of the rotator cuff tear are carefully evaluated. Internal impingement of the SLAP lesion and partial rotator cuff articular side tear in the ABER position are evaluated, and debridement is performed until no impingement is observed.
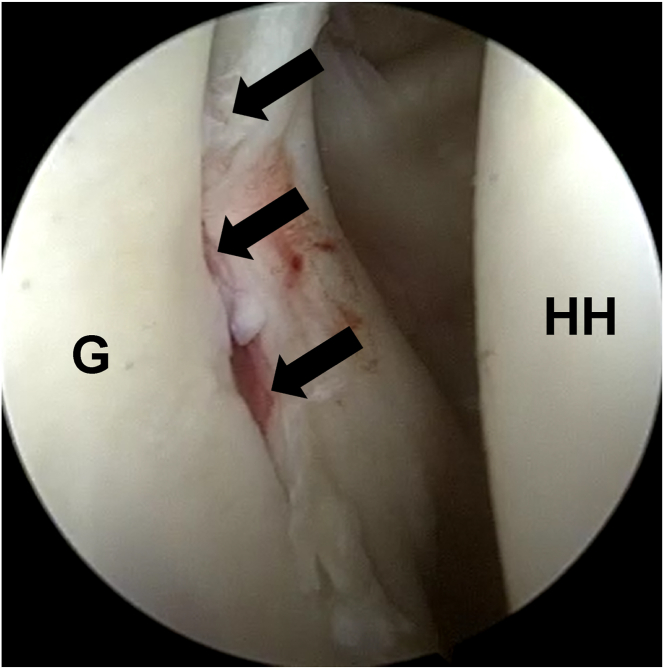
Fig 1.
View from the posterior portal of the right shoulder in the beach-chair position. Capsulolabral lesion is marked by the arrows. (G, glenoid; HH, humeral head.)
Capsulolabral Complex Detachment and Mobilization
The capsulolabral complex is sufficiently detached and mobilized from the glenoid neck using a tissue elevator, starting from the 1- to 2-o’clock position to the 7-o’clock position in the right shoulder, ensuring that the subscapularis muscle is visible (Fig 2). After the capsulolabral complex is released, a small amount of articular cartilage (<3 mm) is removed from the anteroinferior glenoid face to promote tissue healing (Fig 3).
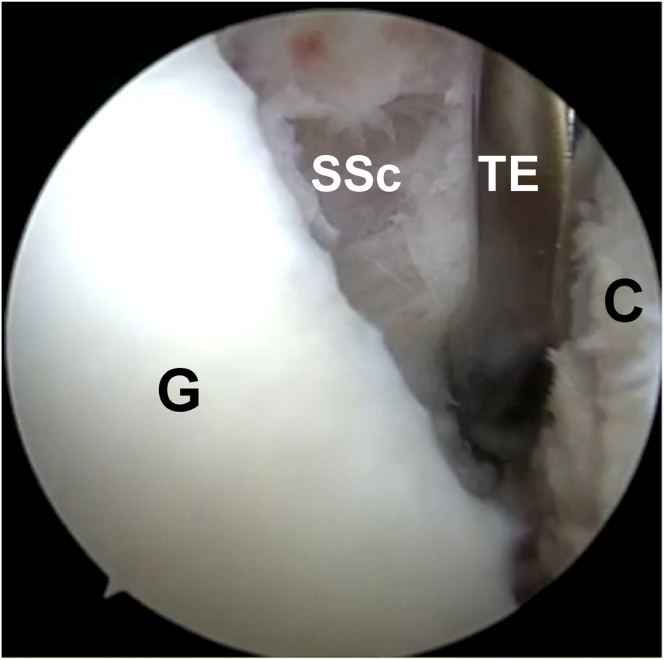
Fig 2.
View from the posterior portal of the right shoulder in the beach-chair position. The capsulolabral complex is sufficiently detached and mobilized from the glenoid neck using a tissue elevator, starting from the 1- to 2-o’clock position to the 7-o’clock position in the right shoulder to ensure that the subscapularis muscle is visible. (C, capsulolabral complex; G, glenoid; SSc, subscapularis; TE, tissue elevator.)
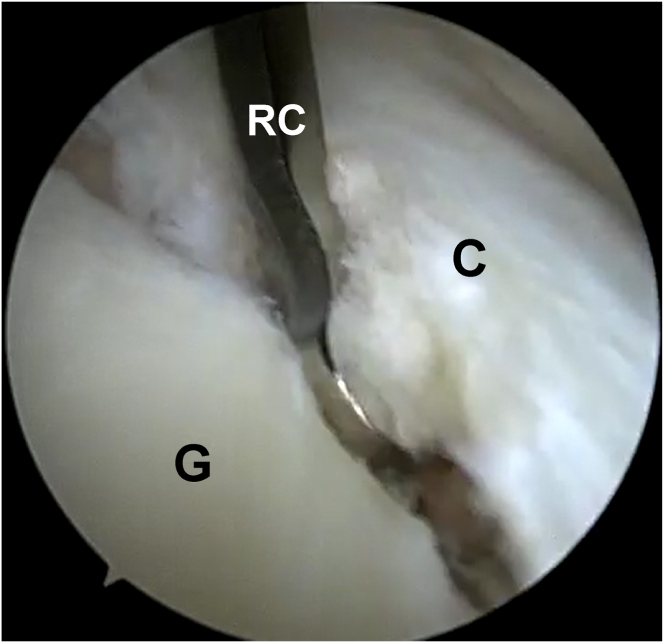
Fig 3.
View from the posterior portal of the right shoulder in the beach-chair position. A small amount of articular cartilage (<3 mm) on the anteroinferior glenoid face is removed using a ring curette to promote tissue healing. (C, capsulolabral complex; G, glenoid; RC, ring curette.)
Anchor Insertion and Suture
Four to six suture anchors loaded with No. 2 high-strength sutures (GRYPHON BR; DePuy Mitek, Raynham, MA) are inserted at the edge of the glenoid from the 6-o'clock position to the 1- to 2-o'clock position. The first anchor is inserted at the 6-o'clock position. While grasping and pulling the anteroinferior capsulolabral complex up, the suture is passed through the IGHL complex using a suture passer (SutureLasso; Arthrex, Naples, FL) (Fig 4) and tied. To prevent overtightening, suture passage, usually 5 mm wide, to the capsule-labrum complex is performed. It is important to avoid creating excessive “bumpers.” The same procedure is repeated once or twice to repair the IGHL complex until it reaches the 4-o’clock position (Fig 5).
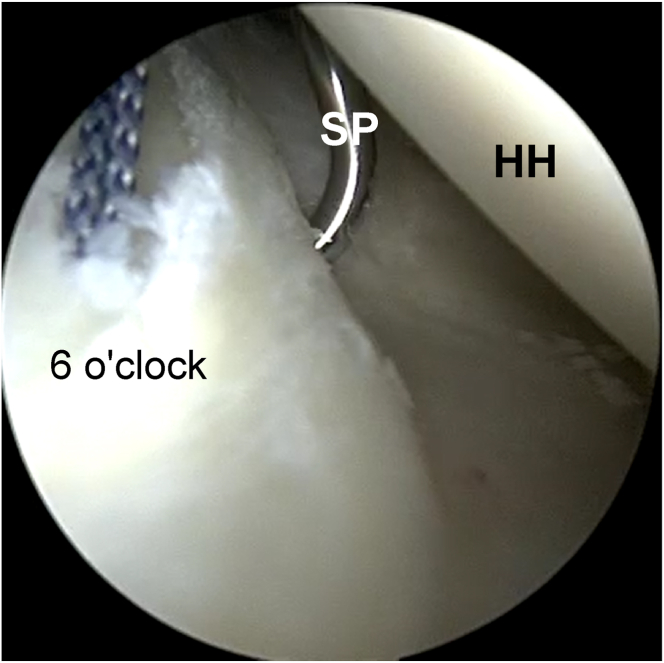
Fig 4.
View from the posterior portal of the right shoulder in the beach-chair position. While grasping and pulling the anteroinferior capsulolabral complex up, the suture is passed through the inferior glenohumeral ligament complex with a 5-mm width using a suture passer. (HH, humeral head.)
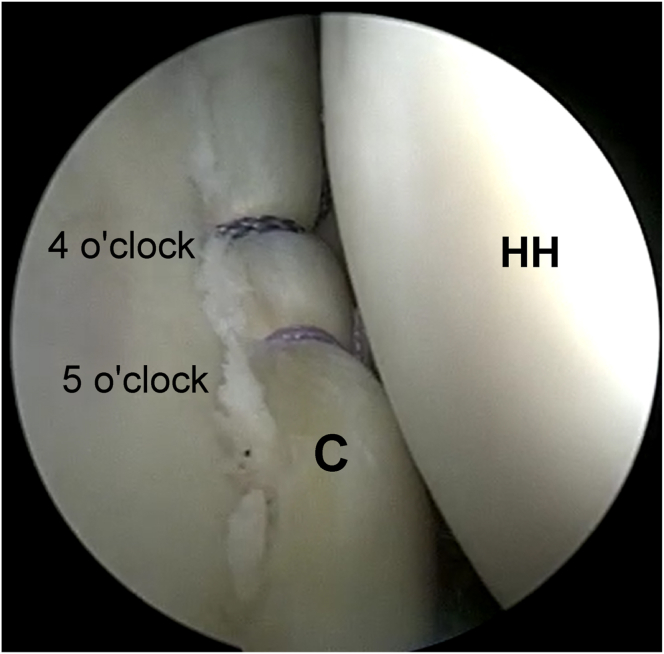
Fig 5.
View from the posterior portal of the right shoulder in the beach-chair position. To avoid creating excessive “bumpers,” the same procedure is repeated once or twice to repair the inferior glenohumeral ligament complex until it reaches approximately the 4-o’clock position. (C, capsulolabral complex; HH, humeral head.)
The highlight of this procedure is to dynamically decide the tensioning of the anterior-to-anterosuperior capsulolabral complex, including the MGHL. Dynamic evaluation of anterosuperior glenohumeral capsular ligament tension is performed at the mimic position during the throwing motion. After anchor insertion, the capsulolabral complex is grasped using a grasper and provisionally reduced to the anchor insertion site. Subsequently, in the ABER position, the proper tension of the anterosuperior glenohumeral capsular ligaments is dynamically evaluated while maintaining the reduced position (Fig 6). The suture is passed through the capsulolabral complex at a location grasped by the grasper (Fig 7A) and tied firmly (Fig 7B). The same procedures are repeated once or twice for anterosuperior capsulolabral complex repair with DAGHT in the ABER position technique from the 3-o'clock position to the 1- to 2-o'clock position (Fig 8).
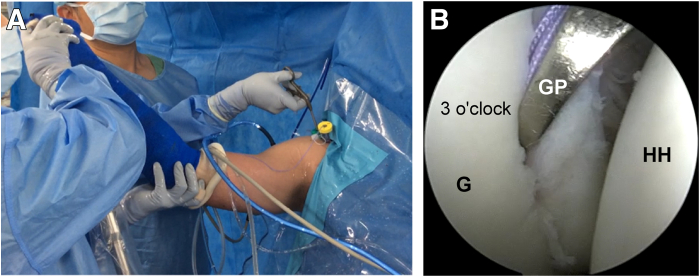
Fig 6.
View from the posterior portal of the right shoulder in the beach-chair position: dynamic anterior glenohumeral capsular ligament tensioning in abduction and external rotation position technique. (A) The anterosuperior glenohumeral capsular ligament is dynamically evaluated in the mimic position during the throwing motion. (B) The ideal tension of the anterosuperior capsule is determined using a grasper. (G, glenoid; GP, grasper; HH, humeral head.)
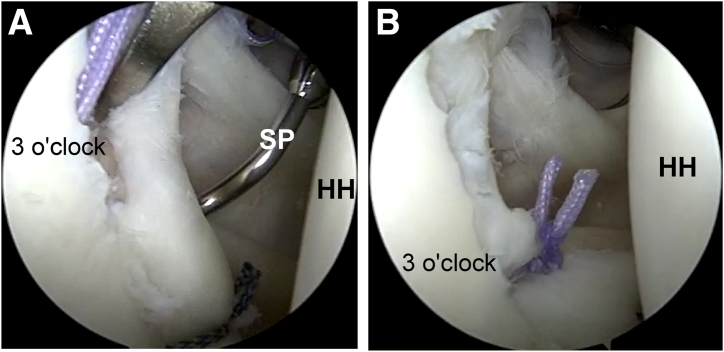
Fig 7.
View from the posterior portal of the right shoulder in the beach-chair position. (A) The suture is passed through the capsulolabral complex of the location grasped by the grasper and (B) tied firmly. (HH, humeral head; SP, suture passer.)
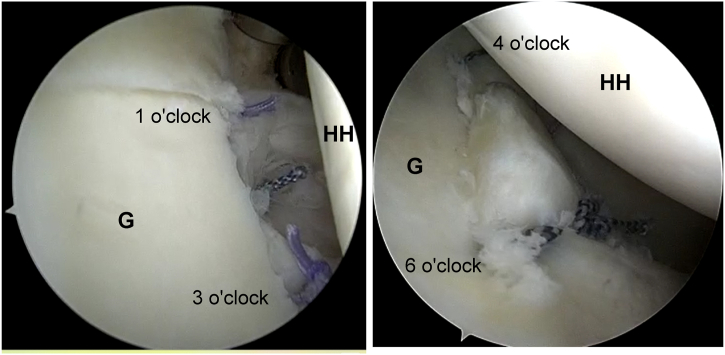
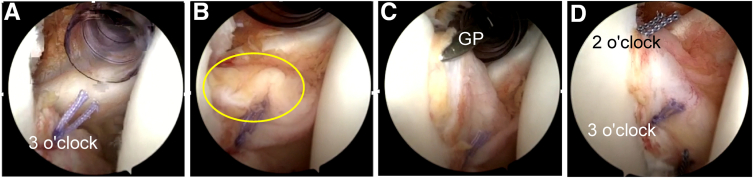
Fig 8.
View from the posterior portal of the right shoulder in the beach-chair position: final view of the anterosuperior sutures after the dynamic anterior glenohumeral capsular ligament tensioning technique. (G, glenoid; HH, humeral head.)
We found that the position of the anterior superior capsular complex changed between the resting (Fig 9A) and ABER positions (Fig 9C). Nylon was sutured as a marker for the MGHL (Fig 9 B and D). Another advantage of the DAGHT technique is that the anterior superior capsule, including the MGHL, is visible in the ABER position (Fig 10A), although it is invisible in the resting position (Fig 10B).
Fig 9.
Dynamic evaluation of the anterosuperior capsule at the mimic position in the throwing motion. (A) Resting position with a limb positioner. (B) Arthroscopic findings of the right shoulder at resting position from the posterior viewing portal: The nylon is sutured to the middle glenohumeral ligament as a mark. (C) Dynamic evaluation of the anterosuperior capsule at the abducted external rotation position without a limb positioner. (D) Arthroscopic findings of the right shoulder at the abducted external rotation position from the posterior viewing portal: The nylon suture shows drastic lateral and cranial movements. (G, glenoid; HH, humeral head.)
Fig 10.
View from the posterior portal of the right shoulder in the beach-chair position: Another case of anterosuperior capsule invisible in the resting position. (A) The anterosuperior capsule is invisible in the resting position. (B) The anterosuperior capsule (oval) is visible in the abduction and external rotation position. (C) The ideal tension of the anterosuperior capsule is confirmed using a grasper. (D) The appearance after securing the anterosuperior capsule. (GP, grasper.)
Postoperative Management
After 3 weeks of immobilization using a sling, passive and assisted active exercises are initiated while avoiding pain provocation. A strengthening program and throwing motion are permitted after 12 weeks of surgery. Full return to play is allowed 6 to 8 months postoperatively, according to the functional recovery of each patient. To avoid recurrence, the patients are prohibited from head-first sliding and diving for 8 months and use a shoulder supporter for 1 year after surgery.
Discussion
Surgical management of traumatic shoulder instability on the dominant side in overhead-throwing athletes remains challenging. Despite the lower rate of recurrent dislocation compared with that in collision athletes, a low return-to-play rate, especially a low return to the same level rate, is considerable.1, 2, 3, 4
Management of postoperative deficits in the range of motion is complicated because some throwers have inherent laxity, which is a large individual difference. A delicate balance between the stability and laxity of the shoulder at maximum external rotation during the late cocking phase is crucial for a better return to the same competition level in overhead-throwing athletes.
Pouliart and Gagey,7 in a morphologic cadaveric study, reported that the MGHL and IGHL were seen as the band defined by arthroscopy in the resting position, and when the arm was moved into full abduction and external rotation, all bands progressively disappeared. This finding indicates that the baseline anterior glenohumeral capsular ligament tension is preferably confirmed at the ABER position, as in our procedures.
Funakoshi et al.8,9 reported that hypoplasia of the MGHL contributes to internal impingement as the result of anterior instability in overhead-throwing athletes. They described that hypoplastic MGHL may cause decreased function in the stabilization of the shoulder joint, especially in the late cocking phase of the throwing motion. We consider that this surgical technique not only provides sufficient postoperative external rotation in abduction but also improves the return to play rate in overhead-throwing athletes because of the retensioning of the anterosuperior glenohumeral capsular ligaments, including the MGHL, an important stabilizer of the anterior shoulder.
One of the advantages of intraoperative tensioning at the ABER (DAGHT) is that it enables determination of appropriate patient-dependent tensioning of the whole anterior glenohumeral capsular ligament to mimic the throwing motion, even though an unaddressed laxity or inherent looseness of the anterior glenohumeral ligament exists. Conventional ABR techniques may have achieved the end range before the ABER position, which is required for the throwing motion, resulting in the restriction of external rotation in abduction.
This study has the following limitations. This report describes a surgical technique, and clinical and biomechanical studies comparing this technique with conventional ABR are necessary to confirm its efficacy. To avoid intraoperative glenohumeral capsular ligament overtightening, the site of suture passage in the ABER position was decided on the basis of the subjective judgement of the operating surgeon. Finally, if the anterosuperior glenohumeral capsular ligaments, including the MGHL, are hypoplastic, restoring anterior stability using our surgical technique would be difficult.
In conclusion, ABR with DAGHT allows less restriction of external rotation during abduction. Therefore, we consider this surgical technique to be reliable for traumatic anterior instability of the dominant shoulder in athletes who wish to return to overhead-throwing sports.
Disclosures
All authors (Y.M., T.F., Ko.H., Ka.H., A.M., H.N., and M.G.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors acknowledge Mr. Shuichiro Sakai and Mr. Chihiro Tachikawa for their assistance with the video production and Mr. Rick Packebush for video narration.
Footnotes
Presented at the 2024 AANA Annual Meeting (AANA24), May 9-11, 2024, Boston, Massachusetts, U.S.A.
Supplementary Data
We demonstrate the steps for dynamic anterior glenohumeral capsular ligament tensioning during arthroscopic right shoulder stabilization in overhead-throwing athletes. The patients undergo surgery in the beach-chair position, and a limb positioner is applied. Three standard portals are used: anterior, anterosuperior, and posterior. First, the capsulolabral complex is adequately detached and mobilized from the glenoid neck, revealing the subscapularis muscle. To promote tissue healing, a small amount of the articular cartilage is removed from the anteroinferior glenoid face. The first anchor is inserted at the 6-o'clock position. While grasping and pulling the anteroinferior capsulolabral complex up, the suture is passed through the IGHL complex with a 5-mm width using a suture passer. The relayed sutures are then tied with a sliding knot and three half-hitches. To avoid creating excessive “bumpers,” the same procedure is repeated to repair the IGHL complex until it reaches the 4-o’clock position. We would like to highlight the following steps: after anchor insertion at the 3-o’clock position, the capsulolabral complex is grasped using a grasper and provisionally reduced to the anchor insertion site. Then, in the abduction and external rotation positions, the tension of the anterosuperior glenohumeral capsular ligaments is dynamically evaluated while maintaining the reduced position. The suture is passed through the capsulolabral complex at a location grasped by the grasper. The suture is relayed and tied with a sliding knot and 3 half-hitches. These procedures are repeated to repair the anterior-superior capsulolabral complex until the 1- to 2-o'clock position is reached. We consider this surgical technique to be reliable for traumatic anterior instability of the dominant shoulder in athletes who wish to return to overhead-throwing sports. (IGHL, inferior glenohumeral ligament.)
References
- 1.Trinh T.Q., Naimark M.B., Bedi A., et al. Clinical outcomes after anterior shoulder stabilization in overhead athletes: An analysis of the MOON shoulder instability consortium. Am J Sports Med. 2019;47:1404–1410. doi: 10.1177/0363546519837666. [DOI] [PubMed] [Google Scholar]
- 2.Ide J., Maeda S., Takagi K. Arthroscopic Bankart repair using suture anchors in athletes: Patient selection and postoperative sports activity. Am J Sports Med. 2004;32:1899–1905. doi: 10.1177/0363546504265264. [DOI] [PubMed] [Google Scholar]
- 3.Park J.Y., Lee J.H., Oh K.S., Chung S.W., Lim J.J., Noh Y.M. Return to play after arthroscopic treatment for shoulder instability in elite and professional baseball players. J Shoulder Elbow Surg. 2019;28:77–81. doi: 10.1016/j.jse.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 4.Harada Y., Iwahori Y., Kajita Y., et al. Return to sports after arthroscopic Bankart repair on the dominant shoulder in overhead athletes. J Orthop Sci. 2022;27:1240–1245. doi: 10.1016/j.jos.2021.07.014. [DOI] [PubMed] [Google Scholar]
- 5.Wilk K.E., Meister K., Andrews J.R. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med. 2002;30:136–151. doi: 10.1177/03635465020300011201. [DOI] [PubMed] [Google Scholar]
- 6.Castagna A., Delle Rose G., Borroni M., et al. Arthroscopic stabilization of the shoulder in adolescent athletes participating in overhead or contact sports. Arthroscopy. 2012;28:309–315. doi: 10.1016/j.arthro.2011.08.302. [DOI] [PubMed] [Google Scholar]
- 7.Pouliart N., Gagey O.J. The arthroscopic view of the glenohumeral ligaments compared with anatomy: Fold or fact? J Shoulder Elbow Surg. 2005;14:324–328. doi: 10.1016/j.jse.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 8.Funakoshi T., Takahashi T., Shimokobe H., et al. Arthroscopic findings of the glenohumeral joint in symptomatic anterior instabilities: Comparison between overhead throwing disorders and traumatic shoulder dislocation. J Shoulder Elbow Surg. 2023;32:776–785. doi: 10.1016/j.jse.2022.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Funakoshi T., Furushima K., Takahashi T., et al. Anterior glenohumeral capsular ligament reconstruction with hamstring autograft for internal impingement with anterior instability of the shoulder in baseball players: Preliminary surgical outcomes. J Shoulder Elbow Surg. 2022;31:1463–1473. doi: 10.1016/j.jse.2021.12.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
We demonstrate the steps for dynamic anterior glenohumeral capsular ligament tensioning during arthroscopic right shoulder stabilization in overhead-throwing athletes. The patients undergo surgery in the beach-chair position, and a limb positioner is applied. Three standard portals are used: anterior, anterosuperior, and posterior. First, the capsulolabral complex is adequately detached and mobilized from the glenoid neck, revealing the subscapularis muscle. To promote tissue healing, a small amount of the articular cartilage is removed from the anteroinferior glenoid face. The first anchor is inserted at the 6-o'clock position. While grasping and pulling the anteroinferior capsulolabral complex up, the suture is passed through the IGHL complex with a 5-mm width using a suture passer. The relayed sutures are then tied with a sliding knot and three half-hitches. To avoid creating excessive “bumpers,” the same procedure is repeated to repair the IGHL complex until it reaches the 4-o’clock position. We would like to highlight the following steps: after anchor insertion at the 3-o’clock position, the capsulolabral complex is grasped using a grasper and provisionally reduced to the anchor insertion site. Then, in the abduction and external rotation positions, the tension of the anterosuperior glenohumeral capsular ligaments is dynamically evaluated while maintaining the reduced position. The suture is passed through the capsulolabral complex at a location grasped by the grasper. The suture is relayed and tied with a sliding knot and 3 half-hitches. These procedures are repeated to repair the anterior-superior capsulolabral complex until the 1- to 2-o'clock position is reached. We consider this surgical technique to be reliable for traumatic anterior instability of the dominant shoulder in athletes who wish to return to overhead-throwing sports. (IGHL, inferior glenohumeral ligament.)