Abstract
We present a technique for the combined anterior cruciate ligament (ACL) and anterolateral ligament (ALL) reconstruction using the superficial layer quadriceps tendon graft. Anatomic reconstruction is achieved with outside-in femoral tunnel drilling. The femoral drill guide has an intra-articular placement at the femoral footprint of the ACL and an extra-articular placement at the femoral ALL attachment. This surgical technique does not need any special instruments and consists of 3 bone tunnels. The long length and customized superficial quadriceps tendon graft is harvested in a minimally invasive manner and allows an accessible and low-cost reconstruction of both ligaments.
Technique Video
The anterior cruciate ligament (ACL) is the most often injured ligament in the knee that requires surgical treatment.1 Regardless of advances in surgical technique, high failure rates are reported, especially in younger and physically active individuals.2, 3, 4, 5, 6
The anterolateral ligament (ALL) has received enhanced attention recently.7, 8, 9 Despite biomechanical controversies, rotatory instability due to ACL plus anterolateral structure injuries may be one of the causes for isolated ACL reconstruction failures.10,11 Clinical studies have shown that combined ACL and ALL reconstruction can decrease graft failure and provide better rotational control compared with isolated reconstruction.12, 13, 14, 15 The most common graft utilized in combined reconstruction is the hamstring (HT) autograft.16
The quadriceps tendon (QT) graft is gaining popularity in ACL reconstruction,17,18 but it is still the least used autograft.19 Biomechanical studies indicate the QT graft with higher structural properties than bone–patellar tendon–bone (BPTB),20,21 and a meta-analysis showed comparable functional outcomes to HT and BPTB.22 Furthermore, the QT is an adjustable graft that can be harvested in different ways.23,24
The purpose of this technical note is to present a combined ACL and ALL reconstruction technique using a superficial layer quadriceps tendon graft harvested in a minimally invasive approach without specialized instruments.
Surgical Technique
The patient is placed in a supine position, and the knee is allowed to move through full range of motion. Examination under anesthesia should confirm the insufficiency of the ACL and associated rotational instability.
The anatomic landmarks identified are the patella, the QT, the lateral epicondyle, the Gerdy tubercle, the head of the fibula, and the lateral tibial plateau.
Graft Harvest
A padded tourniquet is applied to the thigh. A 3-cm longitudinal skin incision is made from the superior pole of the patella at the junction of the lateral and middle third extending proximally (Fig 1). After appropriate dissection, the QT is identified. The graft is harvested from the lateral portion of the rectus femoris tendon, which is the superficial lamina of the QT. The surgical plane between the superficial and intermediate laminae is identified around 3 cm proximal to the patella (Fig 2, Video 1). After 2 longitudinal incisions in the superficial lamina, a 10-mm-wide graft is created. The superficial layer quadriceps tendon graft is elevated (Fig 3), and its distal end is detached from the patella (Fig 4). The distal free end of the graft is whipstitched with nonabsorbable sutures. The dissection of the superficial lamina is extended proximally for 8 cm using Metzenbaum scissors (Fig 5), ensuring that intermediate and deep layers of the QT are preserved. A closed tendon stripper (Sartori) is pushed carefully with the knee in 20° of flexion, and the graft is harvested (Fig 6). Paratenon, subcutaneous tissue, and skin are closed.
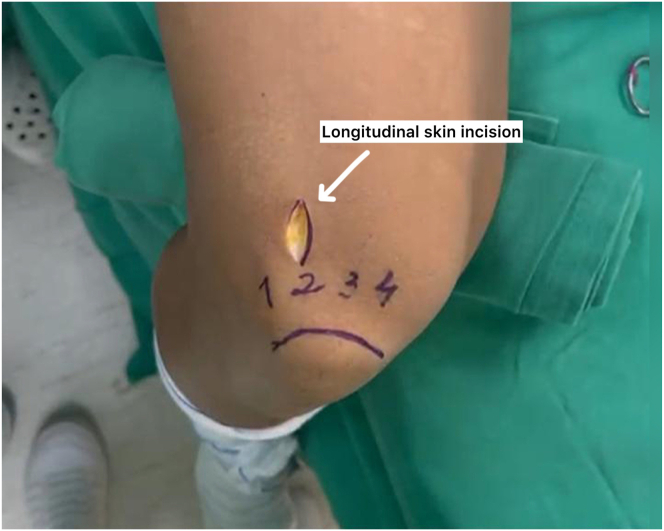
Fig 1.
The right knee is shown. A 3-cm longitudinal skin incision is made from the superior pole of the patella at the junction of the lateral and middle third of the quadriceps tendon.
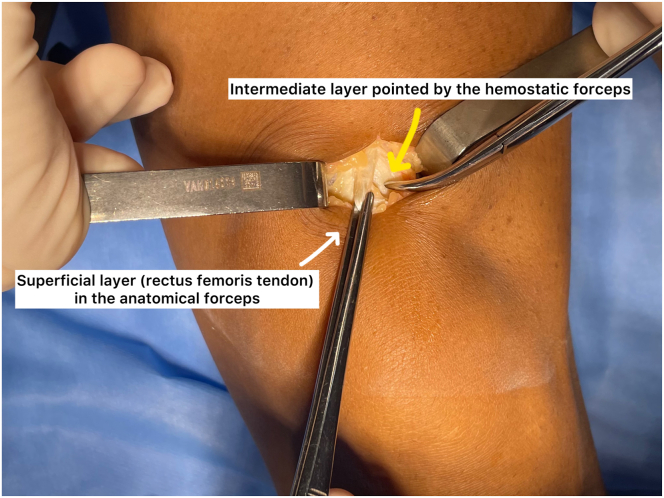
Fig 2.
The left knee is shown. The surgical plane between the superficial and the intermediate laminae of the quadriceps tendon is identified.
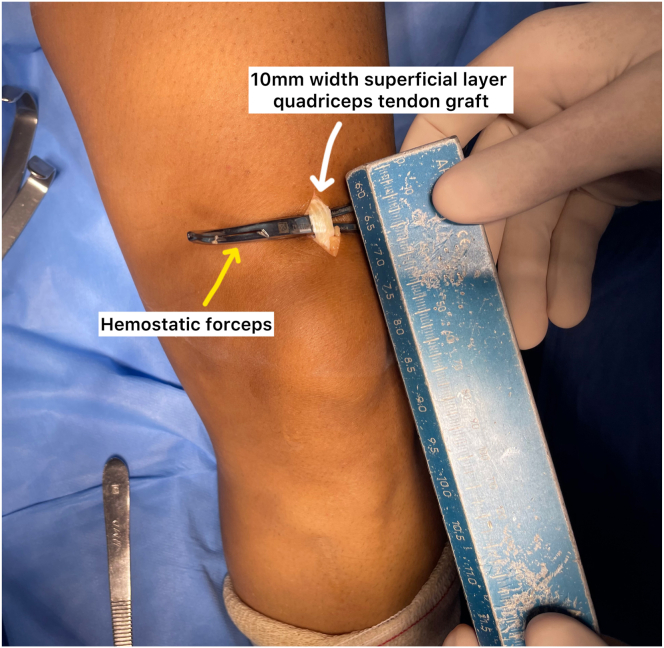
Fig 3.
The left knee is shown. After 2 longitudinal incisions in the superficial layer quadriceps tendon, a 10-mm-wide graft is created. The superficial layer is elevated from the remaining quadriceps tendon with the aid of a hemostatic forceps.
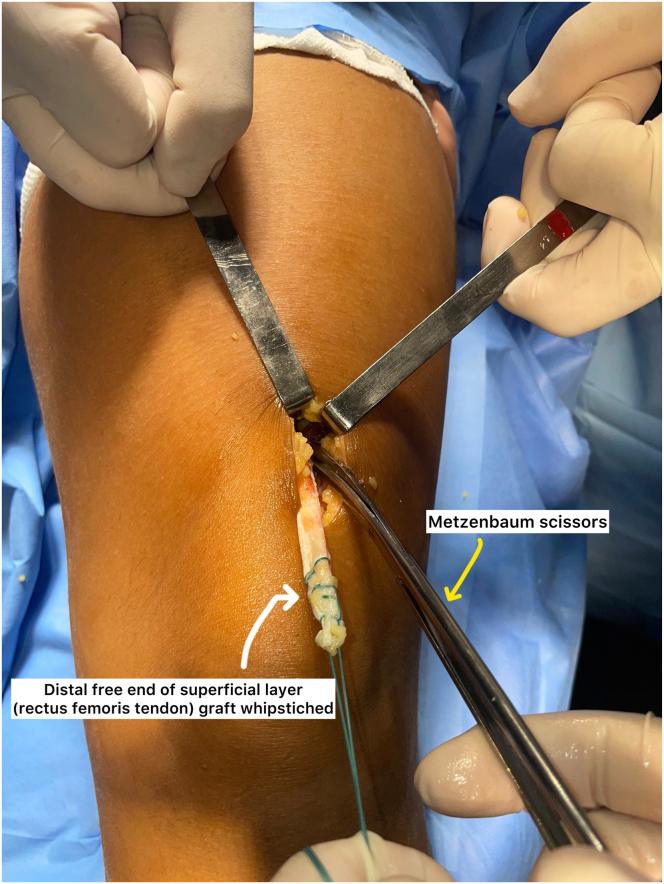
Fig 4.
The left knee is shown. The distal end of the superficial quadriceps tendon graft is detached from the proximal pole of the patella. The intermediate and deep layers of the quadriceps tendon are preserved.
Fig 5.
The left knee is shown. The distal free end of the graft is whipstitched with nonabsorbable sutures. The dissection of the superficial quadriceps tendon graft is extended proximally for 8 cm.
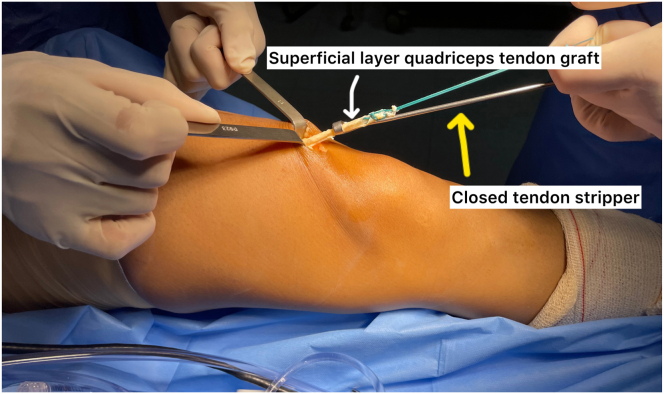
Fig 6.
The left knee is shown. A closed tendon stripper is pushed carefully with the knee in 20° of flexion and the superficial layer quadriceps tendon graft is harvested.
Graft Preparation
The total length normally ranges from 28 to 35 cm (Fig 7). The muscle fibers are removed and measured. The graft is folded in an asymmetric fashion. The distal portion is folded to form a double or triple graft for the ACL portion of the graft. The ALL portion of the graft is the proximal remainder without folding (Fig 8). The ACL graft should be at least 9 cm in length and 8 mm in diameter.
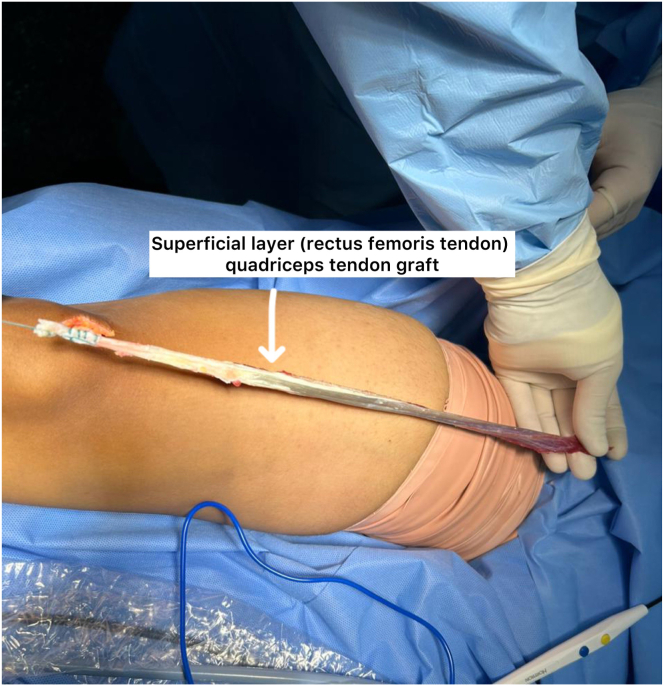
Fig 7.
The right knee is shown. The superficial layer quadriceps graft total length normally ranges from 28 to 35 cm.
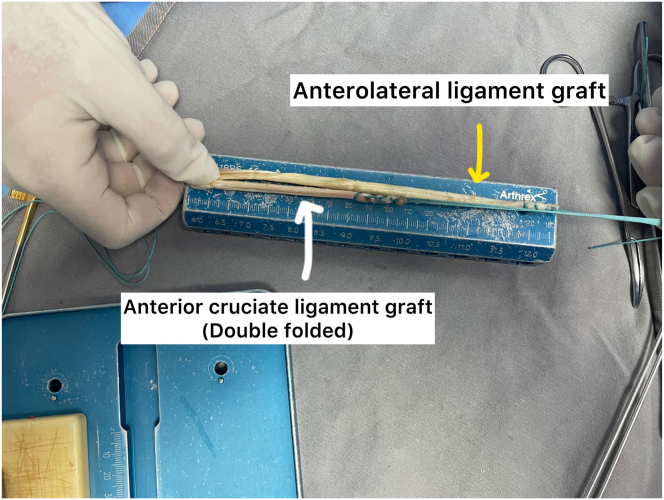
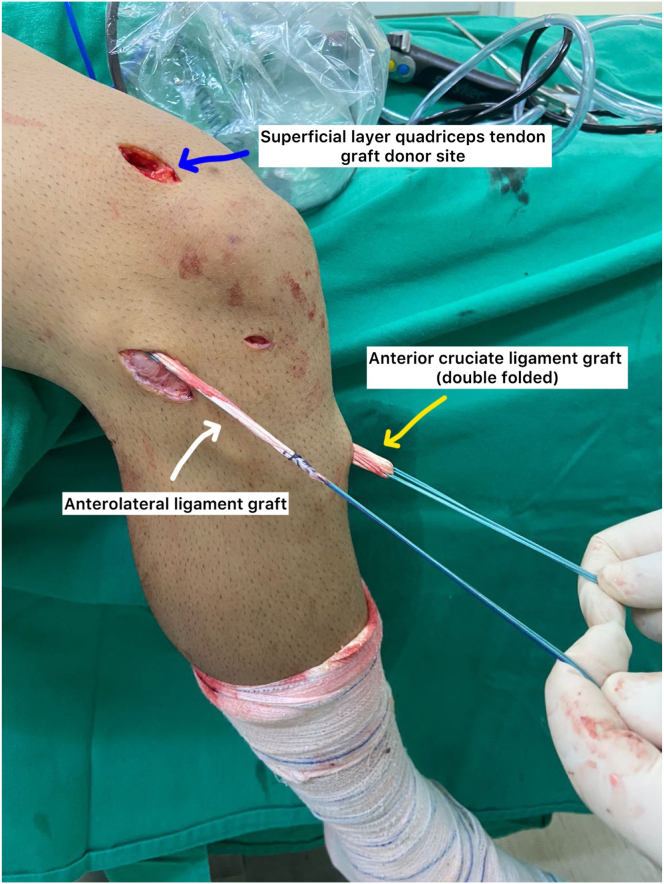
Fig 8.
The muscle fibers are removed from the superficial quadriceps graft. The distal portion is folded to form a double graft for the anterior cruciate ligament reconstruction. The anterolateral ligament reconstruction is achieved with the proximal remainder of the graft without folding.
Arthroscopic Evaluation
A high anterolateral portal is created and a low anteromedial portal is established under direct vision (Fig 9). Evaluation of the cruciate ligaments and possible associated lesions is performed.
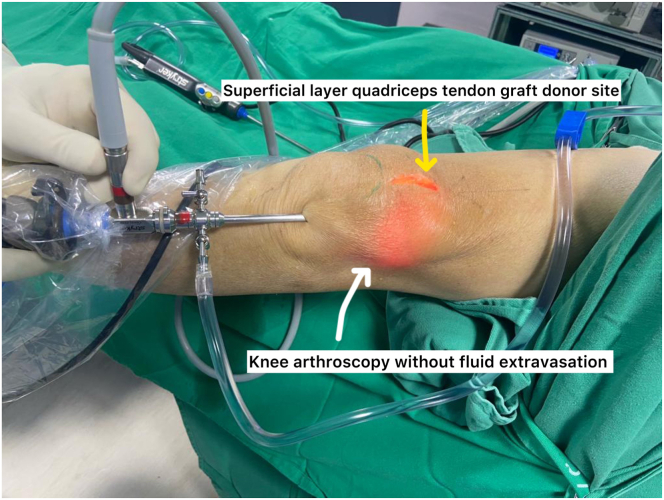
Fig 9.
The left knee is shown. Knee arthroscopy. A high anterolateral portal is created. The knee arthroscopy is done without fluid extravasation after superficial layer quadriceps tendon graft harvest.
ACL Reconstruction
The intercondylar area is prepared by shaving the inside wall of the lateral femoral condyle. The femoral tunnel for the ACL reconstruction is the same used for the ALL reconstruction. The femoral tunnel is made using an outside-in technique.25 A 3-cm lateral skin incision is made along the lateral aspect of the distal femur over the lateral epicondyle, and the iliotibial tract is split longitudinally. The tip of the drill guide (Sartori) is placed at the femoral footprint of the ACL and the external arm of the drill guide lies slightly posterior and proximal to the lateral epicondyle, to replicate the ALL femoral attachment (Fig 10). A guidewire is inserted and then the drilling of the tunnel is performed. The tibial tunnel is made within the topography of the native ACL tibial footprint.26 The diameter of the tunnels is equal to the diameter of the previously prepared ACL graft. The graft is passed from the tibial to femoral tunnel using a suture shuttle (Fig 11). The proximal portion of the graft, which will be used for ALL reconstruction, exits through the lateral condyle (Fig 12).
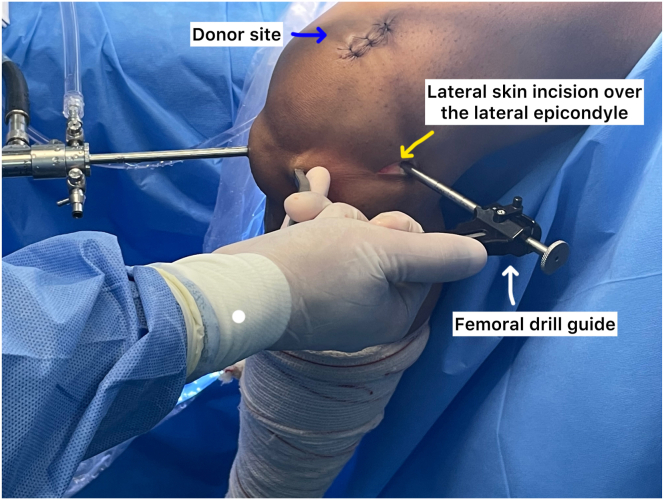
Fig 10.
The left knee is shown. A lateral skin incision of 3 cm is made along the lateral aspect of the distal femur over the lateral epicondyle. The femoral tunnel is made using an outside-in technique. The tip of the drill guide is placed in an intra-articular position at the femoral footprint of the anterior cruciate ligament, and the external arm of the drill guide lies slightly posterior and proximal to the lateral epicondyle to replicate the anterolateral ligament femoral attachment.
Fig 11.
The right knee is shown. The superficial quadriceps tendon graft is passed from the tibial to the femoral tunnel of the anterior cruciate ligament reconstruction using a suture shuttle.
Fig 12.
The right knee is shown. The proximal portion of the superficial layer quadriceps tendon graft, which will be used for anterolateral ligament reconstruction, exits through the lateral femoral condyle.
Femoral ACL graft fixation is performed in an outside-in manner using an interference screw with a diameter equal to the size of the tunnel. Tibial ACL graft fixation is performed with the graft tensioned and the knee at 20° of flexion with an interference screw 1 size greater than the tunnel diameter.
ALL Reconstruction
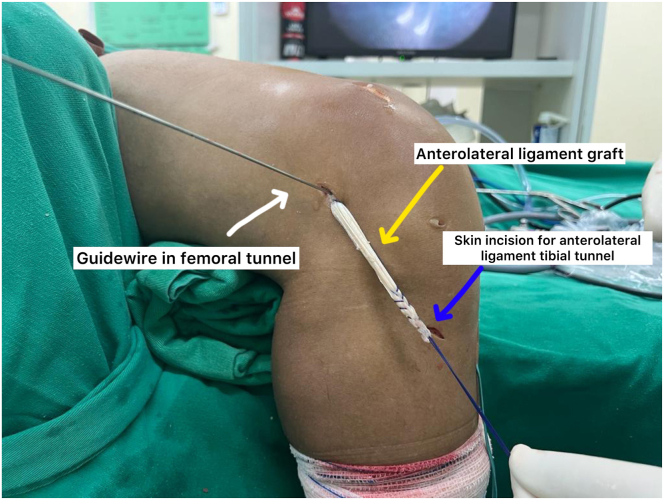
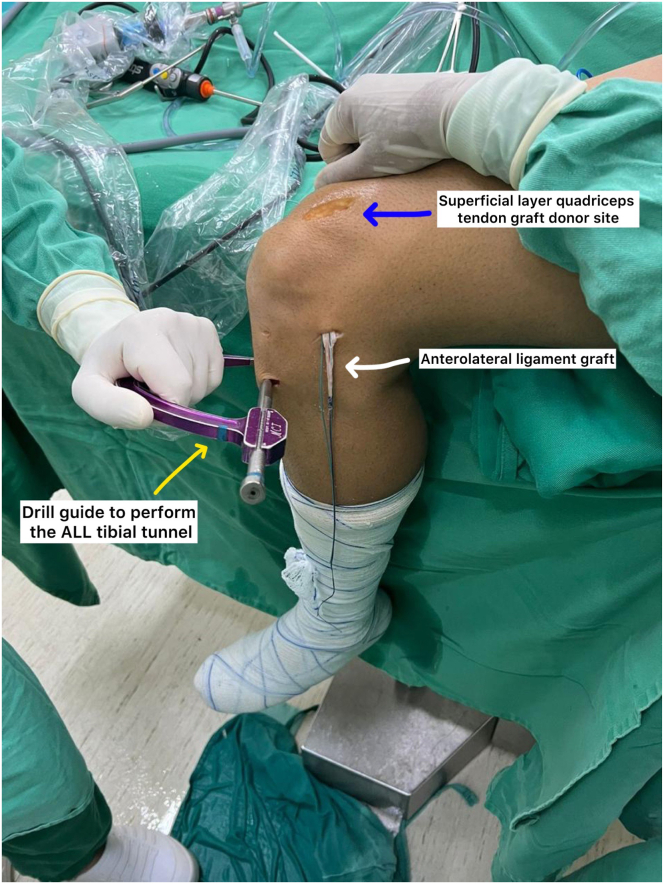
The remaining proximal portion of graft is used for ALL reconstruction. The tibial tunnel for the ALL is created between the Gerdy tubercle and the fibular head, approximately 5 to 10 mm below the lateral articular plateau. The drill guide (Sartori) helps in performing the ALL tibial tunnel exit distal to the ACL tibial tunnel (Fig 13). It is also possible to drill the tunnel freehand. The graft is passed beneath the iliotibial tract (Fig 14) and shuttled with a suture in the tibial tunnel. Tibial fixation is performed with an interference screw in neutral rotation and full extension27 (Fig 15, Video 1).
Fig 13.
The left knee is shown. The tibial tunnel for the anterolateral ligament reconstruction is created between the Gerdy tubercle and the fibular head, approximately 5 to 10 mm below the lateral articular plateau. The drill guide helps in performing the anterolateral ligament tunnel exit distal to the anterior cruciate ligament tibial tunnel.
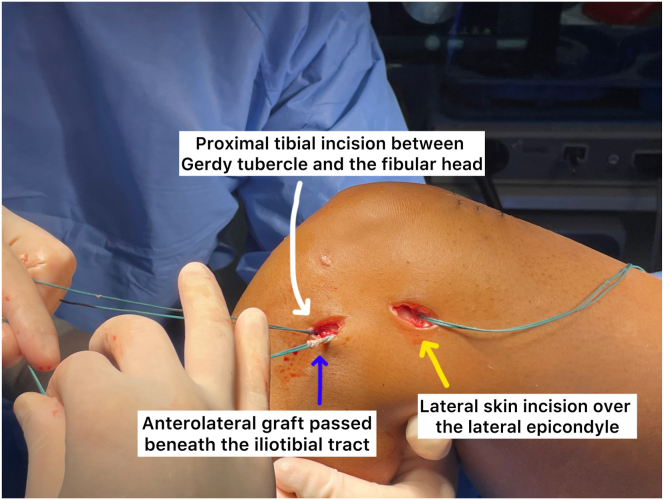
Fig 14.
The left knee is shown. The remaining proximal portion of the graft for the anterolateral ligament reconstruction is passed beneath the iliotibial tract.
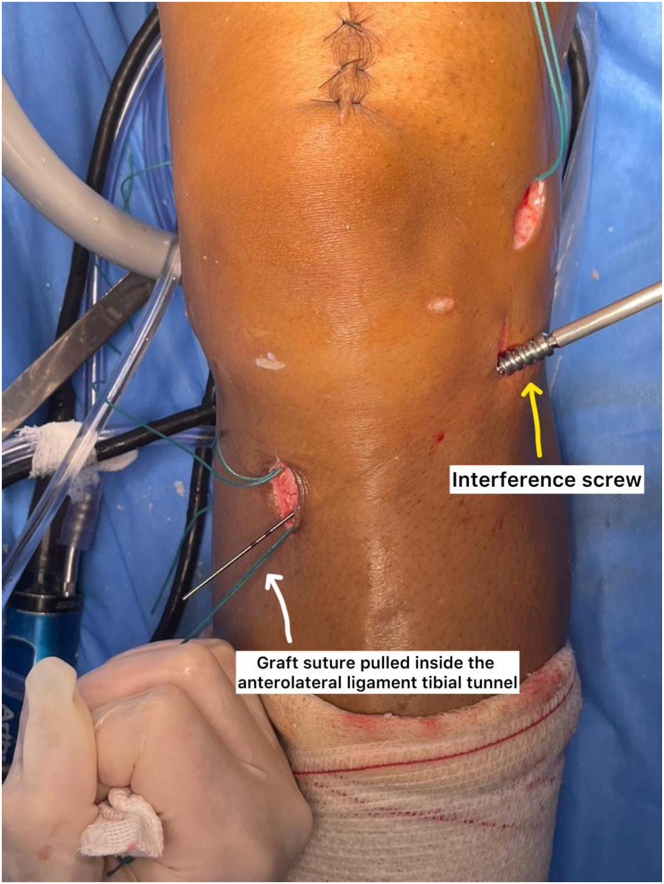
Fig 15.
The left knee is shown. After the graft is passed in the anterolateral ligament tibial tunnel created between the Gerdy tubercle and the fibular head, tibial fixation is performed with an interference screw in neutral rotation and full extension.
After reconstruction, closure in layers is performed. We do not use drain or immobilize. A routine ACL rehabilitation plan is instituted.
Discussion
The harvest approach described by Raman et al.24 and Thamrongskulsiri et al.28 makes possible a superficial layer quadriceps autograft of sufficient length and diameter for the combined ACL and ALL reconstruction.
ACL reconstruction techniques may not restore normal tibial rotation,29, 30, 31 and some patients persist with a positive pivot shift.32, 33, 34 Anterolateral complex injuries are one possible cause of high-grade pivot shift and residual rotational instability after surgery.35,36 Despite conflicting data from biomechanical studies,37, 38, 39, 40 in the clinical scenario, combined ACL and ALL reconstruction presents good functional outcomes, improved knee stability, and less failure rate than isolated ACL reconstruction, especially in high-risk populations.12, 13, 14, 15,41,42 The tunnel preparation for anatomic ALL reconstruction described utilizes the procedure published with a single gracillis.15 The rectus femoris tendon graft option can be used in the same manner and probably with an increased diameter.
Biomechanical data have shown that QT autograft has favorable characteristics43,44 with a greater cross-sectional area20,45 to both HT and BPTB. Recent studies have concluded that QT autograft has similar outcomes, knee stability, and failure rate compared to HT and BPTB46,47 in ACL surgery.
The QT graft has an outstanding versatility. Clinical data show similar outcomes with partial or full thickness48 and with or without bone block graft.49,50 Despite variability in QT anatomy,51 it is possible to harvest the rectus femoris tendon before the layers merge. Soft tissue QT autografts appear to have fewer complications.49 Knee muscle strength deficits are a major issue in ACL rehabilitation. Knee extensor strength after QT autograft is similar to BPTB.52 The harvest utilized in this report could raise the possibility of hematoma in the donor site and decrease extensor knee strength.
The described technique utilizing the superficial layer quadriceps tendon graft harvested in a minimally invasive manner is a feasible alternative to combined ACL and ALL reconstruction in primary and revision surgery (Tables 1 and 2). Clinical studies are necessary to demonstrate the effectiveness of this technique.
Table 1.
Advantages and Disadvantages of the Procedure
| Advantages | Disadvantages |
|---|---|
| Predictable graft diameter | Quadriceps strength reduction |
| Graft harvest with standard instruments | Risk of hematoma formation |
| Preservation of hamstring strength | Additional incision in lateral leg |
| Low morbidity | Additional screw for ligament fixation |
Table 2.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Identification of surgical plane between the superficial and intermediate quadriceps tendon layer | Disrupting the knee capsule |
| Dissection of the superficial quadriceps tendon graft before using the tendon stripper | Tibial tunnel confluence |
| Whipstitching the graft with a strong nonabsorbable suture, with reasonable force applied to the tendon stripper | Cautious anterolateral tibial tunnel positioning to avoid plateau fracture |
| Knee in 20° of flexion for graft harvest | Protruding screws can irritate the iliotibial tract |
| Skin incision proximal and posterior to the lateral epicondyle | |
| Adequate femoral drill guide placement to ensure anatomic reconstruction of both ligaments | |
| Passing the anterolateral graft under the iliotibial tract |
Disclosures
All authors (B.G.B., S.M de G.C., C.P.H., M.C.F.R., F.S.M., M.C.F.R.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Supplementary Data
Technique description of the superficial layer quadriceps tendon graft harvest in a minimally invasive approach without special instruments, the long length graft preparation, and combined anterior cruciate ligament and anterolateral ligament reconstruction using the superficial quadriceps tendon graft. The technique is demonstrated in a left knee.
References
- 1.Gianotti S.M., Marshall S.W., Hume P.A., Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: A national population-based study. J Sci Med Sport. 2009;12:622–627. doi: 10.1016/j.jsams.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Kamath G.V., Murphy T., Creighton R.A., Viradia N., Taft T.N., Spang J.T. Anterior cruciate ligament injury, return to play, and reinjury in the elite collegiate athlete: Analysis of an NCAA Division I cohort. Am J Sports Med. 2014;42:1638–1643. doi: 10.1177/0363546514524164. [DOI] [PubMed] [Google Scholar]
- 3.Rahardja R., Zhu M., Love H., Clatworthy M.G., Monk A.P., Young S.W. Factors associated with revision following anterior cruciate ligament reconstruction: A systematic review of registry data. Knee. 2020;27:287–299. doi: 10.1016/j.knee.2019.12.003. [DOI] [PubMed] [Google Scholar]
- 4.Morgan M.D., Salmon L.J., Waller A., Roe J.P., Pinczewski L.A. Fifteen-year survival of endoscopic anterior cruciate ligament reconstruction in patients aged 18 years and younger. Am J Sports Med. 2016;44:384–392. doi: 10.1177/0363546515623032. [DOI] [PubMed] [Google Scholar]
- 5.Astur D.C., Cachoeira C.M., da Silva Vieira T., Debieux P., Kaleka C.C., Cohen M. Increased incidence of anterior cruciate ligament revision surgery in paediatric verses adult population. Knee Surg Sports Traumatol Arthrosc. 2018;26:1362–1366. doi: 10.1007/s00167-017-4727-z. [DOI] [PubMed] [Google Scholar]
- 6.Webster K.E., Feller J.A. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44:2827–2832. doi: 10.1177/0363546516651845. [DOI] [PubMed] [Google Scholar]
- 7.Vincent J.P., Magnussen R.A., Gezmez F., et al. The anterolateral ligament of the human knee: An anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc. 2012;20:147–152. doi: 10.1007/s00167-011-1580-3. [DOI] [PubMed] [Google Scholar]
- 8.Claes S., Vereecke E., Maes M., Victor J., Verdonk P., Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223:321–328. doi: 10.1111/joa.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ariel de Lima D., Helito C.P., Lacerda de Lima L., de Castro Silva D., Costa Cavalcante ML., Dias Leite J.A. Anatomy of the anterolateral ligament of the knee: A systematic review. Arthroscopy. 2019;35:670–681. doi: 10.1016/j.arthro.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 10.Kunze K.N., Manzi J., Richardson M., et al. Combined anterolateral and anterior cruciate ligament reconstruction improves pivot shift compared with isolated anterior cruciate ligament reconstruction: A systematic review and meta-analysis of randomized controlled trials. Arthroscopy. 2021;37:2677–2703. doi: 10.1016/j.arthro.2021.03.058. [DOI] [PubMed] [Google Scholar]
- 11.Sobrado M.F., Giglio P.N., Bonadio M.B., et al. Outcomes after isolated acute anterior cruciate ligament reconstruction are inferior in patients with an associated anterolateral ligament injury. Am J Sports Med. 2020;48:3177–3182. doi: 10.1177/0363546520956266. [DOI] [PubMed] [Google Scholar]
- 12.Sonnery-Cottet B., Saithna A., Cavalier M., et al. Anterolateral ligament reconstruction is associated with significantly reduced ACL graft rupture rates at a minimum follow-up of 2 years: A prospective comparative study of 502 patients from the SANTI Study Group. Am J Sports Med. 2017;45:1547–1557. doi: 10.1177/0363546516686057. [DOI] [PubMed] [Google Scholar]
- 13.Helito C.P., Camargo D.B., Sobrado M.F., et al. Combined reconstruction of the anterolateral ligament in chronic ACL injuries leads to better clinical outcomes than isolated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26:3652–3659. doi: 10.1007/s00167-018-4934-2. [DOI] [PubMed] [Google Scholar]
- 14.Lee D.W., Kim J.G., Cho S.I., Kim D.H. Clinical outcomes of isolated revision anterior cruciate ligament reconstruction or in combination with anatomic anterolateral ligament reconstruction. Am J Sports Med. 2019;47:324–333. doi: 10.1177/0363546518815888. [DOI] [PubMed] [Google Scholar]
- 15.Helito C.P., Sobrado M.F., Giglio P.N., et al. Combined reconstruction of the anterolateral ligament in patients with anterior cruciate ligament injury and ligamentous hyperlaxity leads to better clinical stability and a lower failure rate than isolated anterior cruciate ligament reconstruction. Arthroscopy. 2019;35:2648–2654. doi: 10.1016/j.arthro.2019.03.059. [DOI] [PubMed] [Google Scholar]
- 16.Chalidis B., Pitsilos C., Kitridis D., Givissis P. Graft choices for anterolateral ligament knee reconstruction surgery: Current concepts. World J Clin Cases. 2022;10:8463–8473. doi: 10.12998/wjcc.v10.i24.8463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Middleton K.K., Hamilton T., Irrgang J.J., Karlsson J., Harner C.D., Fu F.H. Anatomic anterior cruciate ligament (ACL) reconstruction: A global perspective. Part 1. Knee Surg Sports Traumatol Arthrosc. 2014;22:1467–1482. doi: 10.1007/s00167-014-2846-3. [DOI] [PubMed] [Google Scholar]
- 18.Winkler P.W., Vivacqua T., Thomassen S., et al. Quadriceps tendon autograft is becoming increasingly popular in revision ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2022;30:149–160. doi: 10.1007/s00167-021-06478-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arnold M.P., Calcei J.G., Vogel N., et al. ACL study group survey reveals the evolution of anterior cruciate ligament reconstruction graft choice over the past three decades. Knee Surg Sports Traumatol Arthrosc. 2021;29:3871–3876. doi: 10.1007/s00167-021-06443-9. [DOI] [PubMed] [Google Scholar]
- 20.Shani R.H., Umpierez E., Nasert M., Hiza E.A., Xerogeanes J. Biomechanical comparison of quadriceps and patellar tendon grafts in anterior cruciate ligament reconstruction. Arthroscopy. 2016;32:71–75. doi: 10.1016/j.arthro.2015.06.051. [DOI] [PubMed] [Google Scholar]
- 21.Xerogeanes J.W., Mitchell P.M., Karasev P.A., Kolesov I.A., Romine S.E. Anatomic and morphological evaluation of the quadriceps tendon using 3-dimensional magnetic resonance imaging reconstruction: Applications for anterior cruciate ligament autograft choice and procurement. Am J Sports Med. 2013;41:2392–2399. doi: 10.1177/0363546513496626. [DOI] [PubMed] [Google Scholar]
- 22.Mouarbes D., Menetrey J., Marot V., Courtot L., Berard E., Cavaignac E. Anterior cruciate ligament reconstruction: A systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone-patellar tendon-bone and hamstring-tendon autografts. Am J Sports Med. 2019;47:3531–3540. doi: 10.1177/0363546518825340. [DOI] [PubMed] [Google Scholar]
- 23.Fink C., Herbort M., Abermann E., Hoser C. Minimally invasive harvest of a quadriceps tendon graft with or without a bone block. Arthrosc Tech. 2014;3(4):e509–e513. doi: 10.1016/j.eats.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Raman R., Mishra B.N., Sen A. A minimally invasive and simple technique of superficial quadriceps tendon graft harvesting. Arthrosc Tech. 2022;11:e2347–e2355. doi: 10.1016/j.eats.2022.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Garofalo R., Mouhsine E., Chambat P., Siegrist O. Anatomic anterior cruciate ligament reconstruction: The two-incision technique. Knee Surg Sports Traumatol Arthrosc. 2006;14:510–516. doi: 10.1007/s00167-005-0029-y. [DOI] [PubMed] [Google Scholar]
- 26.Siebold R., Schuhmacher P., Fernandez F., et al. Flat midsubstance of the anterior cruciate ligament with tibial "C"-shaped insertion site. Knee Surg Sports Traumatol Arthrosc. 2015;23:3136–3142. doi: 10.1007/s00167-014-3058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Inderhaug E., Stephen J.M., Williams A., Amis A.A. Anterolateral tenodesis or anterolateral ligament complex reconstruction: effect of flexion angle at graft fixation when combined with ACL reconstruction. Am J Sports Med. 2017;45:3089–3097. doi: 10.1177/0363546517724422. [DOI] [PubMed] [Google Scholar]
- 28.Thamrongskulsiri N., Limskul D., Tanpowpong T., Kuptniratsaikul S., Itthipanichpong T. Minimally invasive harvesting of triple-fold superficial layer quadriceps autograft for knee ligament reconstruction. Arthrosc Tech. 2023;12:e2239–e2246. doi: 10.1016/j.eats.2023.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lie D.T., Bull A.M., Amis A.A. Persistence of the mini pivot shift after anatomically placed anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 2007;457:203–209. doi: 10.1097/BLO.0b013e3180314b01. [DOI] [PubMed] [Google Scholar]
- 30.Chouliaras V., Ristanis S., Moraiti C., Stergiou N., Georgoulis A.D. Effectiveness of reconstruction of the anterior cruciate ligament with quadrupled hamstrings and bone-patellar tendon-bone autografts: An in vivo study comparing tibial internal-external rotation. Am J Sports Med. 2007;35:189–196. doi: 10.1177/0363546506296040. [DOI] [PubMed] [Google Scholar]
- 31.Ristanis S., Stergiou N., Patras K., Vasiliadis H.S., Giakas G., Georgoulis A.D. Excessive tibial rotation during high-demand activities is not restored by anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:1323–1329. doi: 10.1016/j.arthro.2005.08.032. [DOI] [PubMed] [Google Scholar]
- 32.Sajovic M., Stropnik D., Skaza K. Long-term comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: A 17-year follow-up of a randomized controlled trial. Am J Sports Med. 2018;46:1800–1808. doi: 10.1177/0363546518768768. [DOI] [PubMed] [Google Scholar]
- 33.Mohtadi N.G., Chan D.S. A randomized clinical trial comparing patellar tendon, hamstring tendon, and double-bundle ACL reconstructions: Patient-reported and clinical outcomes at 5-year follow-up. J Bone Joint Surg Am. 2019;101:949–960. doi: 10.2106/JBJS.18.01322. [DOI] [PubMed] [Google Scholar]
- 34.Getgood A.M.J., Bryant D.M., Litchfield R., et al. Lateral extra-articular tenodesis reduces failure of hamstring tendon autograft anterior cruciate ligament reconstruction: 2-Year outcomes from the STABILITY Study Randomized Clinical Trial. Am J Sports Med. 2020;48:285–297. doi: 10.1177/0363546519896333. [DOI] [PubMed] [Google Scholar]
- 35.Monaco E., Ferretti A., Labianca L., et al. Navigated knee kinematics after cutting of the ACL and its secondary restraint. Knee Surg Sports Traumatol Arthrosc. 2012;20:870–877. doi: 10.1007/s00167-011-1640-8. [DOI] [PubMed] [Google Scholar]
- 36.Willinger L., Athwal K.K., Holthof S., Imhoff A.B., Williams A., Amis A.A. Role of the anterior cruciate ligament, anterolateral complex, and lateral meniscus posterior root in anterolateral rotatory knee instability: A biomechanical study. Am J Sports Med. 2023;51:1136–1145. doi: 10.1177/03635465231161071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huser L.E., Noyes F.R., Jurgensmeier D., Levy M.S. Anterolateral ligament and iliotibial band control of rotational stability in the anterior cruciate ligament-intact knee: Defined by tibiofemoral compartment translations and rotations. Arthroscopy. 2017;33:595–604. doi: 10.1016/j.arthro.2016.08.034. [DOI] [PubMed] [Google Scholar]
- 38.Noyes F.R., Huser L.E., Levy M.S. Rotational knee instability in ACL-deficient knees: Role of the anterolateral ligament and iliotibial band as defined by tibiofemoral compartment translations and rotations. J Bone Joint Surg Am. 2017;99:305–314. doi: 10.2106/JBJS.16.00199. [DOI] [PubMed] [Google Scholar]
- 39.Monaco E., Fabbri M., Mazza D., et al. The effect of sequential tearing of the anterior cruciate and anterolateral ligament on anterior translation and the pivot-shift phenomenon: A cadaveric study using navigation. Arthroscopy. 2018;34:1009–1014. doi: 10.1016/j.arthro.2017.09.042. [DOI] [PubMed] [Google Scholar]
- 40.Inderhaug E., Stephen J.M., Williams A., Amis A.A. Biomechanical comparison of anterolateral procedures combined with anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:347–354. doi: 10.1177/0363546516681555. [DOI] [PubMed] [Google Scholar]
- 41.Helito C.P., Sobrado M.F., Moreira da Silva A.G., et al. The addition of either an anterolateral ligament reconstruction or an iliotibial band tenodesis is associated with a lower failure rate after revision anterior cruciate ligament reconstruction: A retrospective comparative trial. Arthroscopy. 2023;39:308–319. doi: 10.1016/j.arthro.2022.06.039. [DOI] [PubMed] [Google Scholar]
- 42.Ariel de Lima D., de Lima L.L., de Souza N.G.R., et al. Clinical outcomes of combined anterior cruciate ligament and anterolateral ligament reconstruction: A systematic review and meta-analysis. Knee Surg Relat Res. 2021;33:33. doi: 10.1186/s43019-021-00115-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sasaki N., Farraro K.F., Kim K.E., Woo S.L. Biomechanical evaluation of the quadriceps tendon autograft for anterior cruciate ligament reconstruction: A cadaveric study. Am J Sports Med. 2014;42:723–730. doi: 10.1177/0363546513516603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Adams D.J., Mazzocca A.D., Fulkerson J.P. Residual strength of the quadriceps versus patellar tendon after harvesting a central free tendon graft. Arthroscopy. 2006;22:76–79. doi: 10.1016/j.arthro.2005.10.015. [DOI] [PubMed] [Google Scholar]
- 45.Hart D., Gurney-Dunlop T., Leiter J., et al. Biomechanics of hamstring tendon, quadriceps tendon, and bone-patellar tendon-bone grafts for anterior cruciate ligament reconstruction: A cadaveric study. Eur J Orthop Surg Traumatol. 2023;33:1067–1074. doi: 10.1007/s00590-022-03247-6. [DOI] [PubMed] [Google Scholar]
- 46.Dai W., Leng X., Wang J., Cheng J., Hu X., Ao Y. Quadriceps tendon autograft versus bone-patellar tendon-bone and hamstring tendon autografts for anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Am J Sports Med. 2022;50:3425–3439. doi: 10.1177/03635465211030259. [DOI] [PubMed] [Google Scholar]
- 47.Ashy C., Bailey E., Hutchinson J., et al. Quadriceps tendon autograft has similar clinical outcomes when compared to hamstring tendon and bone-patellar tendon-bone autografts for revision ACL reconstruction: A systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2023;31:5463–5476. doi: 10.1007/s00167-023-07592-9. [DOI] [PubMed] [Google Scholar]
- 48.Kanakamedala A.C., de Sa D., Obioha O.A., et al. No difference between full thickness and partial thickness quadriceps tendon autografts in anterior cruciate ligament reconstruction: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2019;27:105–116. doi: 10.1007/s00167-018-5042-z. [DOI] [PubMed] [Google Scholar]
- 49.Crum R.J., Kay J., Lesniak B.P., Getgood A., Musahl V., de Sa D. Bone versus all soft tissue quadriceps tendon autografts for anterior cruciate ligament reconstruction: A systematic review. Arthroscopy. 2021;37:1040–1052. doi: 10.1016/j.arthro.2020.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Meena A., D'Ambrosi R., Runer A., et al. Quadriceps tendon autograft with or without bone block have comparable clinical outcomes, complications and revision rate for ACL reconstruction: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2023;31:2274–2288. doi: 10.1007/s00167-022-07281-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Waligora A.C., Johanson N.A., Hirsch B.E. Clinical anatomy of the quadriceps femoris and extensor apparatus of the knee. Clin Orthop Relat Res. 2009;467:3297–3306. doi: 10.1007/s11999-009-1052-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Johnston P.T., McClelland J.A., Feller J.A., Webster K.E. Knee muscle strength after quadriceps tendon autograft anterior cruciate ligament reconstruction: Systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2021;29:2918–2933. doi: 10.1007/s00167-020-06311-y. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technique description of the superficial layer quadriceps tendon graft harvest in a minimally invasive approach without special instruments, the long length graft preparation, and combined anterior cruciate ligament and anterolateral ligament reconstruction using the superficial quadriceps tendon graft. The technique is demonstrated in a left knee.