Abstract
Background:
There are few studies that have examined clinical and radiological outcomes at 5 years after isolated medial patellofemoral ligament (MPFL) reconstruction. To date, midterm outcomes after isolated double-bundle (DB) MPFL reconstruction are not well known.
Hypothesis:
Isolated DB MPFL reconstruction using a patellar suture anchor technique would lead to improved functional scores and radiological findings, and these improvements would remain stable over the 5-year postoperative period.
Study Design:
Case series; Level of evidence, 4.
Methods:
Isolated MPFL reconstruction was performed in patients with recurrent patellar instability between March 2013 and February 2017. Clinical and functional evaluations were performed via an interview using the Kujala, Lysholm, and Tegner scores preoperatively and at 6, 12, 24, and 60 months postoperatively. Radiographs were taken preoperatively, immediately postoperatively, and at 24 and 60 months after surgery. Radiographic assessments included measuring the modified Insall-Salvati ratio, congruence angle, and lateral patellofemoral angle.
Results:
A total of 31 patients (31 knees) underwent isolated MPFL reconstruction; 4 patients did not complete 5-year follow-up, and thus, 27 patients (27 knees) were enrolled in the study. The mean age at the time of surgery was 22.0 ± 6.4 years (range, 14-32 years). All clinical and functional scores significantly improved in the first 2 years (P < .001), with the mean Kujala, Lysholm, and Tegner scores improving from 52.7 to 90.7, 49.6 to 92.7, and 2.9 to 5.1, respectively. There was no significant difference in scores between 2- and 5-year follow-up. All radiographic parameters significantly improved between preoperatively and immediately postoperatively (P < .001), with mean values for the modified Insall-Salvati ratio, congruence angle, and lateral patellofemoral angle improving from 1.7° to 1.6°, 5.7° to −6.6°, and 3.0° to 5.9°, respectively. No significant differences were observed in radiographic measurements between the postoperative time points. No patients experienced a patellar redislocation or fracture.
Conclusion:
The prospective analysis of isolated DB MPFL reconstruction at 5-year follow-up showed that clinical and radiological outcomes significantly improved postoperatively and were maintained to 5 years. These midterm results suggest that isolated DB MPFL reconstruction is an effective treatment option for patients with patellar instability.
Keywords: knee, ligament, patella, general sports trauma, clinical assessment/grading scale, patellar instability, medial patellofemoral ligament reconstruction, suture anchor fixation
The medial patellofemoral ligament (MPFL) is known to be the primary soft tissue restraint against lateralization of the patella.5,39,41,46 It has been reported that the MPFL is ruptured in the majority of acute patellar dislocations, and insufficiency or slackening of the MPFL is an essential component of recurrent patellar dislocations.24,48 Accordingly, it appears that surgical treatment is required to restore stability of the MPFL in patients with symptomatic recurrent patellar instability. Currently, MPFL reconstruction is the primary treatment approach for recalcitrant patellar instability.9,11,31
Over the past few decades, several surgical techniques have been described for MPFL reconstruction. Various methods, such as bone tunnels,13,20,33,38 suture anchors,3,36,40 and small interference screws, 16 have been used to fix the graft to the patella. MPFL reconstruction can be performed using either a single-bundle or double-bundle (DB) technique, and various graft options are available, including autografts (eg, semitendinosus, gracilis, quadriceps, and adductor magnus tendons) and allografts. Despite the variety of techniques and graft options, no single method has proven to be superior. A recent systematic review found that isolated MPFL reconstruction for recurrent patellar dislocations led to satisfactory outcomes, regardless of the surgical technique and graft type used. 30 Numerous studies have reported promising clinical and functional outcomes in patients with patellar instability after isolated MPFL reconstruction.1,4,6,15,21,44 A systematic review and meta-analysis found that a high percentage of young patients return to sports with favorable functional results and a low incidence of recurrent instability and reoperations after isolated MPFL reconstruction. 34 However, the majority of studies on isolated MPFL reconstruction have only reported short-term outcomes. Although a few retrospective studies have shown generally favorable midterm clinical results,2,6 midterm to long-term outcomes after isolated MPFL reconstruction are not well known. There is no prospective study that has addressed the midterm clinical outcomes of isolated DB MPFL reconstruction using the patellar suture anchor technique.
The purpose of this study was to prospectively evaluate the 5-year clinical and radiological results of isolated DB MPFL reconstruction using patellar suture anchor fixation with a hamstring tendon autograft. We hypothesized that isolated DB MPFL reconstruction using the patellar suture anchor technique would lead to improved functional scores and radiological findings, exceeding the threshold of the minimal clinically important difference (MCID), and these improvements would remain stable over the 5-year postoperative period.
Methods
This study was approved by the institutional review board at our institution, and all participants provided informed consent. A prospective study was performed on patients with recurrent patellar instability between March 2013 and February 2017. A CONSORT (Consolidated Standards of Reporting Trials) flow diagram is shown in Figure 1.
Figure 1.
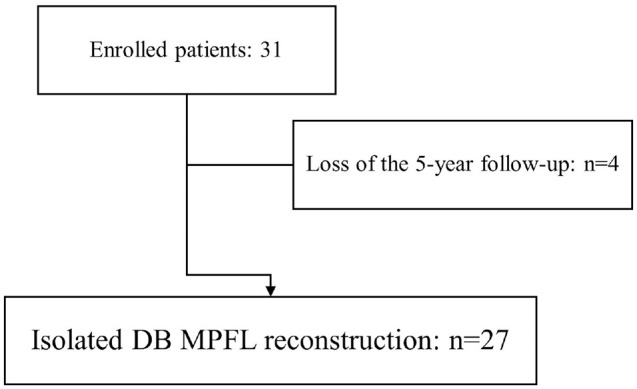
Flowchart of patient inclusion. DB, double bundle; MPFL, medial patellofemoral ligament.
Isolated MPFL reconstruction was indicated in symptomatic patients who had experienced at least 2 episodes of a patellar dislocation. A patellar dislocation was diagnosed by history taking, a physical examination, radiography, and magnetic resonance imaging (MRI). The contraindications for isolated MPFL reconstruction without additional bony procedures were (1) severe anatomic abnormalities, such as a high degree of trochlear dysplasia (Dejour type D) and an atypical tibial tuberosity–trochlear groove (TT-TG) distance (≥20 mm), and (2) congenital or habitual dislocations. Patients who were able to participate throughout the 5-year follow-up period were included in this study. The exclusion criteria were as follows: (1) MPFL reconstruction combined with a bony realignment procedure and (2) no acquisition of a regular series of radiographs.
Clinical Assessments
Clinical and functional evaluations, composed of the patient-reported outcome measures of the Kujala, 22 Lysholm, 26 and Tegner 42 scores, were performed via an interview preoperatively and at 6, 12, 24, and 60 months after surgery. The physical examination consisted of the apprehension test 10 and range of motion testing. Redislocations and complications were also observed. All clinical data were collected by interviews during the clinic visit and not by mail or telephone.
Radiological Assessments
Anteroposterior, lateral, and Merchant (axial) views of the knee were taken preoperatively, immediately postoperatively, and at 24 and 60 months after surgery. In the lateral view, the modified Insall-Salvati (MIS) ratio was calculated to assess patellar height. The MIS ratio was calculated by dividing the distance between the lowest point of the articular surface of the patella and tibial tuberosity by the length of the articular surface of the patella 18 and recorded to the nearest 0.01 mm. In the Merchant view, the congruence angle and lateral patellofemoral angle were measured to assess patellar tilt, and the type of femoral trochlear dysplasia was classified in the lateral view according to Dejour et al. 8 The congruence angle was measured by bisecting the sulcus angle to construct a reference line and then projecting a second line from the apex of the sulcus angle to the lower point of the articular surface of the patella. 27 The lateral patellofemoral angle was formed by one line connecting the superior points of the medial and lateral trochlear facets and a second line tangent to the lateral facet of the patella. 23 These angular values were recorded to the nearest 0.1°. The severity of patellofemoral osteoarthritis was evaluated preoperatively, immediately postoperatively, and at 24 and 60 months after surgery using the classification system of Iwano et al. 19 Preoperative MRI was performed on all patients. The TT-TG distance was measured using MRI as described by Schoettle et al. 35 Radiological measurements using a picture archiving and communication system were performed twice, with an interval of 2 weeks, by 2 fellowship-trained orthopaedic surgeons, who were blinded to the prior measurements (H.B.L. and Y.J.S.). The intraobserver and interobserver agreements of each measurement were assessed using the intraclass correlation coefficient (ICC).
Surgical Technique
All surgical procedures were performed by a single surgeon (S.Y.S.). The surgical technique used was in accordance with the method described by Song et al. 40 Briefly, arthroscopic surgery was routinely performed to evaluate any intra-articular lesions and patellar tracking throughout knee motion. Arthroscopic lateral release was performed for patients exhibiting tightness of the lateral structures, as determined by examination under anesthesia. The semitendinosus tendon was harvested. After a 2-cm medial parapatellar incision was made along the proximal two-thirds of the patella, the medial retinaculum was incised. Using a small bur, a longitudinal bony sulcus with a depth of approximately 5 mm was created at the insertion site of the MPFL, and this depth was sufficient for embedding the harvested graft. Then, 2 suture anchors (Corkscrew; Arthrex) were fixed at the proximal and distal ends of the sulcus. The femoral entry point described by Schöttle et al 37 was identified under C-arm guidance. A Beath pin was placed at this point, and a 6-mm reamer was used to drill a femoral tunnel over this pin to a depth of 40 mm. Using curved blunt forceps, a soft tissue tunnel connecting the medial parapatellar incision to the femoral incision was created in the second layer, and the 2 limbs of the graft were then passed through the soft tissue tunnel. Both free ends of the graft were whip-stitched with No. 1 Vicryl suture (Ethicon) for a length of 30 mm, and the whip-stitched sutures and graft were pulled into the femoral tunnel using a Beath pin. The knee was cycled several times, from full flexion to full extension, with the graft under tension. The proper tension applied to the graft was assessed arthroscopically by observing patellar tracking under direct visualization via the superolateral portal. The tendons were tensioned with the knee in extension, and then, the patella was manually lateralized 10 mm. Once proper tension was obtained, femoral fixation with a bioabsorbable screw was performed at 20° of knee flexion. Patellar stability and tracking were checked again throughout range of motion, particularly in early knee flexion.
Postoperative Rehabilitation
After surgery, the knee was immobilized for 1 week in an extended position. Subsequently, gradual range of motion was initiated with a hinged brace, and 90° of knee flexion was achieved by 4 weeks postoperatively, which further increased to 120° of knee flexion by 6 weeks postoperatively. At 6 weeks after surgery, the brace was removed. Walking using crutches with partial weightbearing was allowed for the first 3 weeks. At 3 weeks after surgery, full weightbearing was allowed without crutches. Leg-raising and quadriceps isometric strength exercises were initiated immediately. At 6 weeks after surgery, the patient returned to normal daily activities. Noncontact sports were permitted at 3 months and contact sports at 6 months after surgery.
Statistical Analysis
Results are expressed as mean ± standard deviation. The differences in clinical scores and radiological measurements between each follow-up time point were analyzed using the Friedman rank-sum test, followed by post hoc multiple pairwise comparisons with the Conover test. The level of significance was set at P < .05. Statistical analysis was performed using R (Version 3.6.1; R Foundation). Cohort-specific MCID analysis was conducted as part of the statistical analysis for this study. Its methodology involved the calculation of the standard deviation of changes in the Kujala, Lysholm, and Tegner scores between the preoperative and 5-year postoperative time points. Subsequently, this value was divided by 2 to ascertain the cohort-specific MCID. A post hoc power analysis was performed for the Kujala score obtained preoperatively and at 5-year follow-up. With a given alpha level of .05 and the calculated effect size, a statistical power of 88.6% was found.
Results
A total of 31 patients (31 knees) underwent isolated MPFL reconstruction during the study period, but 4 patients did not complete 5-year follow-up. As a result, 27 patients (27 knees) were ultimately enrolled in this study. The mean age at the time of surgery was 22.0 ± 6.4 years (range, 14-32 years). Patient characteristics are presented in Table 1. Concomitant procedures included lateral release in 7 patients and chondroplasty in 5 patients. None of the patients underwent additional medial tibial tuberosity transfer or trochleoplasty.
Table 1.
Patient Characteristics a
| Value (n = 27) | |
|---|---|
| Sex | |
| Male | 16 |
| Female | 11 |
| Age, mean ± SD (range), y | 22.0 ± 6.4 (14-32) |
| Side | |
| Right | 12 |
| Left | 15 |
| Trochlear dysplasia | |
| None | 5 |
| Dejour type A | 11 |
| Dejour type B | 10 |
| Dejour type C | 1 |
| Dejour type D | 0 |
Data are presented as No. unless otherwise indicated.
Clinical Outcomes
Clinical and functional scores are summarized in Table 2. A significant improvement in all clinical and functional scores was observed at each follow-up time point for 2 years postoperatively (P < .001). There was no significant difference in scores between 2- and 5-year follow-up (P > .05). Additionally, the calculated MCID thresholds for the Kujala, Lysholm, and Tegner scores were 2.26, 3.09, and 0.32, respectively. Patients’ rates of achieving the MCID for the Kujala, Lysholm, and Tegner scores were 100.0%, 100.0%, and 63.0%, respectively. None of the patients experienced a patellar redislocation between surgery and 5 years after surgery. Preoperative apprehension was positive in all patients. At 5 years after surgery, the apprehension test result was positive in only 1 patient. All patients achieved full range of knee motion at 6 months after surgery and maintained it until 5-year follow-up. There were no complications, such as patellar fractures, infections, or reoperations.
Table 2.
Clinical and Functional Scores a
| Preoperative | 6 mo | 12 mo | 24 mo | 60 mo | |
|---|---|---|---|---|---|
| Kujala | 52.7 ± 11.7 b | 71.6 ± 6.4 b , c | 83.2 ± 4.8 b - d | 90.7 ± 4.1 b - e | 91.1 ± 4.8 b - e |
| Lysholm | 49.6 ± 10.1 b | 75.7 ± 4.9 b , c | 89.2 ± 3.6 b - d | 92.7 ± 3.3 b - e | 92.5 ± 3.6 b - e |
| Tegner | 2.9 ± 0.8 b | 3.6 ± 0.7 b , c | 4.2 ± 0.9 b - d | 5.1 ± 1.0 b - e | 5.2 ± 0.9 b - e |
Data are presented as mean ± SD.
Each paired letter indicates a statistically significant difference between values (P < .001).
Each paired letter indicates a statistically significant difference between values (P < .001).
Each paired letter indicates a statistically significant difference between values (P < .001).
Each paired letter indicates no statistically significant difference between values (P > .05).
Radiological Outcomes
The ICCs for all radiographic measurements were >0.7. All radiological data are presented in Table 3. Significant improvements on all radiological parameters were observed between preoperatively and immediately postoperatively (P < .001). There was no significant difference in radiographic measurements between all follow-up time points after surgery (P > .05). There was no progression in patellofemoral osteoarthritis observed during the 5-year follow-up period. There were 4 patients who had patella alta (MIS ratio of >2.0) preoperatively, whereas no patient had patella alta at 5-year follow-up. According to the Dejour classification system, 5 knees had no trochlear dysplasia, and 22 had trochlear dysplasia (Table 1). The mean preoperative TT-TG distance was 15.5 ± 4.2 mm; 13 patients had a TT-TG distance of <15 mm, and 14 patients had a TT-TG distance of 15 to 20 mm. None of the patients had a TT-TG distance of >20 mm.
Table 3.
Radiological Measurements a
| Preoperative | Immediately Postoperative | 24 mo | 60 mo | |
|---|---|---|---|---|
| MIS ratio | 1.71 ± 0.17 b | 1.59 ± 0.11 b , c | 1.60 ± 0.13 c , d | 1.61 ± 0.14 c , d |
| Congruence angle, deg | 5.7 ± 13.9 b | −6.7 ± 6.8 b , c | −6.8 ± 6.7 c , d | −6.6 ± 6.3 c , d |
| Lateral patellofemoral angle, deg | 3.0 ± 7.5 b | 5.9 ± 4.8 b , c | 5.9 ± 4.9 c , d | 5.8 ± 4.8 c , d |
| Iwano osteoarthritis classification, grade 0/1/2/3/4, n | 24/2/1/0/0 | 24/2/1/0/0 | 24/2/1/0/0 | 24/2/1/0/0 |
Data are presented as mean ± SD unless otherwise indicated. MIS, modified Insall-Salvati.
Each paired letter indicates a statistically significant difference between values (P < .001).
Each paired letter indicates no statistically significant difference between values (P > .05).
Each paired letter indicates no statistically significant difference between values (P > .05).
Discussion
The most important finding of this study was that the Kujala, Lysholm, and Tegner scores after isolated DB MPFL reconstruction using patellar suture anchor fixation with a hamstring tendon autograft significantly improved for 2 years postoperatively. Furthermore, these improvements persisted up to 5-year follow-up without redislocations.
Many reports describing good short-term results after isolated MPFL reconstruction have been published, which has increased enthusiasm for this procedure.13,28,40,47 They reported satisfactory short-term clinical results, irrespective of surgical techniques and graft types. Recently, a few researchers have reported midterm results after isolated MPFL reconstruction.4,17,33 A retrospective investigation of 89 knees undergoing isolated MPFL reconstruction found a significant improvement in clinical scores. 4 The mean follow-up in that study was 69.8 months (range, 59-86 months), with improvements in the Kujala (from 68.8 to 88.2) and Lysholm (from 71.3 to 88.4) scores. Another retrospective study of 80 knees, with a mean follow-up of 66.1 months (range, 60-78 months), reported that isolated MPFL reconstruction with the double patellar tunnel technique resulted in significant clinical improvements. 17 In that study, the mean Kujala, Lysholm, and Tegner scores improved from 69.4 to 96.1, 73.5 to 95.3, and 3.1 to 5.9, respectively. The results of the present study are similar to those of these other recent clinical studies, demonstrating the procedure's effectiveness in enhancing clinical outcomes and avoiding instability at midterm follow-up. Unlike many previous retrospective studies,1,2,7,17,44 the current study was conducted prospectively using on-site clinical evaluations. Additionally, this study had a more consistent follow-up period of 60 months compared to the inconsistent follow-up periods in previous studies, which varied from one patient to another.
The radiological findings of this study revealed a statistically significant difference between preoperative and postoperative patellar tilt angles, such as the congruence angle and lateral patellofemoral angle. However, there was no significant difference in these values between postoperatively and 2- and 5-year follow-up. Isolated MPFL reconstruction has been shown to improve patellofemoral joint alignment and reduce patellar tilt, and good clinical results have been correlated with a significant correction of patellar tilt according to recent studies.12,29 The present study also found that isolated MPFL reconstruction led to a sustained correction of patellar tilt up to 5 years postoperatively.
An additional finding of this study was the statistically significant difference between preoperative and postoperative MIS ratios. The high preoperative MIS ratio was significantly reduced postoperatively likely because of the effect of isolated MPFL reconstruction, which decreased patellar height. This decrease in patellar height was maintained for 5 years after the procedure. Similar results have been reported by Fabricant et al14,25,45 that isolated MPFL reconstruction significantly improved patellar height according to measures such as the Insall-Salvati ratio, MIS ratio, and Caton-Deschamps index and these values fell within normal ranges postoperatively (P < .001). Because a high patella is a risk factor for patellar dislocations, reducing patellar height through isolated MPFL reconstruction may improve patellar stability and patellofemoral kinematics. Studies have shown that isolated MPFL reconstruction reduces patellar height and restores trochlear groove tracking.14,25,45 Although the exact reason for this alteration in patellar height could not be determined from this study, it may be caused by inferomedial patellar traction of the reconstructed ligament.
Isolated MPFL reconstruction has a low rate of redislocations, with <5% reported at short-term follow-up.40,43,47 A systematic review and meta-analysis found that the pooled risk of recurrent instability after isolated MPFL reconstruction was 1.2%. 34 There are few midterm studies on redislocation rates after isolated MPFL reconstruction with a minimum follow-up of 5 years.4,17 A recent retrospective study reported that 5 (5.6%) of 89 knees undergoing isolated MPFL reconstruction with patellar soft tissue fixation had redislocations at a mean follow-up of 5.8 years (range, 59-86 months). 4 Another retrospective study of 80 knees that underwent isolated MPFL reconstruction using the patellar bone tunnel technique showed a redislocation rate of 2.5% at a mean follow-up of 66.1 months (range, 60-78 months). 17 The current prospective study showed that 27 knees undergoing isolated MPFL reconstruction using the patellar suture anchor technique had no redislocations at 5-year follow-up. Based on these studies, the low redislocation rates observed in the short term seem to be maintained at midterm follow-up.
Our study, which used the patellar suture anchor technique, did not have any cases of patellar fractures during the 5-year follow-up period. Despite surgical advancements in bone tunnel formation, which have led to a decrease in patellar fractures, the patellar bone tunnel technique still has a risk of patellar fractures. 32 In contrast, most previous studies using the patellar suture anchor technique have reported no patellar fractures. The suture anchor technique is thought to have an advantage over the bone tunnel technique in terms of the risk of patellar fractures.
Limitations and Strengths
This study had several limitations. First, the sample size was small, which may affect the generalizability of the results. Second, this study was based on clinical scales and physical examinations instead of more objective measures such as follow-up MRI. Postoperative MRI was not used in this study, as it is not a standard practice in the field, especially for patients who are considered clinically stable. Third, this study did not investigate the long-term results of the procedure; therefore, it is unclear if the benefits seen in the short term and midterm will be sustained over a longer period of time. Future studies with larger sample sizes and long-term clinical and radiological outcomes are required to validate these findings.
Despite these limitations, this study had the advantages of a prospective study design and serial clinical data collection, including face-to-face interviews with patients at each follow-up visit, while also demonstrating a lower rate of follow-up loss throughout the 5-year period.
Conclusion
This prospective analysis of isolated DB MPFL reconstruction with 5-year follow-up showed that clinical and radiological outcomes significantly improved postoperatively and were maintained without redislocations. These midterm results suggest that isolated DB MPFL reconstruction is an effective treatment option for patients with patellar instability.
Footnotes
Final revision submitted April 9, 2024; accepted May 7, 2024.
The authors have declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Dongtan Sacred Heart Hospital (2014-048).
References
- 1. Aliberti GM, Kraeutler MJ, Miskimin C, et al. Autograft versus allograft for medial patellofemoral ligament reconstruction: a systematic review. Orthop J Sports Med. 2021;9(10):23259671211046639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Astur DC, Gouveia GB, Borges JH, et al. Medial patellofemoral ligament reconstruction: a longitudinal study comparison of 2 techniques with 2 and 5-years follow-up. Open Orthop J. 2015;9:198-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Berruto M, Ferrua P, Tradati D, et al. Suture anchors fixation in MPFL reconstruction using a bioactive synthetic ligament. Joints. 2017;5(3):188-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Boelch SP, Gurok A, Gilbert F, et al. Why compromise the patella? Five-year follow-up results of medial patellofemoral ligament reconstruction with soft tissue patellar fixation. Int Orthop. 2021;45(6):1493-1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chahla J, Smigielski R, LaPrade RF, Fulkerson JP. An updated overview of the anatomy and function of the proximal medial patellar restraints (medial patellofemoral ligament and the medial quadriceps tendon femoral ligament). Sports Med Arthrosc Rev. 2019;27(4):136-142. [DOI] [PubMed] [Google Scholar]
- 6. Csintalan RP, Latt LD, Fornalski S, et al. Medial patellofemoral ligament (MPFL) reconstruction for the treatment of patellofemoral instability. J Knee Surg. 2014;27(2):139-146. [DOI] [PubMed] [Google Scholar]
- 7. Damasena I, Blythe M, Wysocki D, Kelly D, Annear P. Medial patellofemoral ligament reconstruction combined with distal realignment for recurrent dislocations of the patella: 5-year results of a randomized controlled trial. Am J Sports Med. 2016;45(2):369-376. [DOI] [PubMed] [Google Scholar]
- 8. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19-26. [DOI] [PubMed] [Google Scholar]
- 9. Diduch DR, Kandil A, Burrus MT. Lateral patellar instability in the skeletally mature patient: evaluation and surgical management. J Am Acad Orthop Surg. 2018;26(12):429-439. [DOI] [PubMed] [Google Scholar]
- 10. Dimon JH, 3rd. Apprehension test for subluxation of the patella. Clin Orthop Relat Res. 1974;(103):39. [DOI] [PubMed] [Google Scholar]
- 11. Duerr RA, Chauhan A, Frank DA, DeMeo PJ, Akhavan S. An algorithm for diagnosing and treating primary and recurrent patellar instability. JBJS Rev. 2016;4(9):e2. [DOI] [PubMed] [Google Scholar]
- 12. Elias JJ, Jones KC, Lalonde MK, et al. Allowing one quadrant of patellar lateral translation during medial patellofemoral ligament reconstruction successfully limits maltracking without overconstraining the patella. Knee Surg Sports Traumatol Arthrosc. 2018;26(10):2883-2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Erickson BJ, Nguyen J, Gasik K, et al. Isolated medial patellofemoral ligament reconstruction for patellar instability regardless of tibial tubercle-trochlear groove distance and patellar height: outcomes at 1 and 2 years. Am J Sports Med. 2019;47(6):1331-1337. [DOI] [PubMed] [Google Scholar]
- 14. Fabricant PD, Ladenhauf HN, Salvati EA, Green DW. Medial patellofemoral ligament (MPFL) reconstruction improves radiographic measures of patella alta in children. Knee. 2014;21(6):1180-1184. [DOI] [PubMed] [Google Scholar]
- 15. Feller JA, Richmond AK, Wasiak J. Medial patellofemoral ligament reconstruction as an isolated or combined procedure for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2470-2476. [DOI] [PubMed] [Google Scholar]
- 16. Ferrari MB, Sanchez G, Chang A, Ferdousian S, Provencher MT. Medial patellofemoral ligament reconstruction in a revision setting: anchor and interference screw fixation. Arthrosc Tech. 2017;6(4):e927-e932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gao G, Liu P, Xu Y. Treatment of patellar dislocation with arthroscopic medial patellofemoral ligament reconstruction using gracilis tendon autograft and modified double-patellar tunnel technique: minimum 5-year patient-reported outcomes. J Orthop Surg Res. 2020;15(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Grelsamer RP, Meadows S. The modified Insall-Salvati ratio for assessment of patellar height. Clin Orthop Relat Res. 1992;(282):170-176. [PubMed] [Google Scholar]
- 19. Iwano T, Kurosawa H, Tokuyama H, Hoshikawa Y. Roentgenographic and clinical findings of patellofemoral osteoarthrosis: with special reference to its relationship to femorotibial osteoarthrosis and etiologic factors. Clin Orthop Relat Res. 1990;(252):190-197. [PubMed] [Google Scholar]
- 20. Ji G, Wang H, Su X, Wang J, Wang F. The modified semi-tunnel bone bridge technique achieved statistically better knee function than the suture anchor technique. Knee Surg Sports Traumatol Arthrosc. 2020;28(3):995-1001. [DOI] [PubMed] [Google Scholar]
- 21. Kang H, Cao J, Yu D, Zheng Z, Wang F. Comparison of 2 different techniques for anatomic reconstruction of the medial patellofemoral ligament: a prospective randomized study. Am J Sports Med. 2013;41(5):1013-1021. [DOI] [PubMed] [Google Scholar]
- 22. Kujala UM, Jaakkola LH, Koskinen SK, et al. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(2):159-163. [DOI] [PubMed] [Google Scholar]
- 23. Laurin CA, Dussault R, Levesque HP. The tangential x-ray investigation of the patellofemoral joint: x-ray technique, diagnostic criteria and their interpretation. Clin Orthop Relat Res. 1979;(144):16-26. [PubMed] [Google Scholar]
- 24. Liu Z, Yi Q, He L, et al. Comparing nonoperative treatment, MPFL repair, and MPFL reconstruction for patients with patellar dislocation: a systematic review and network meta-analysis. Orthop J Sports Med. 2021;9(9):23259671211026624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Luceri F, Roger J, Randelli PS, Lustig S, Servien E. How does isolated medial patellofemoral ligament reconstruction influence patellar height? Am J Sports Med. 2020;48(4):895-900. [DOI] [PubMed] [Google Scholar]
- 26. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150-154. [DOI] [PubMed] [Google Scholar]
- 27. Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56(7):1391-1396. [PubMed] [Google Scholar]
- 28. Nelitz M, Dreyhaupt J, Williams SRM. Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents using a pedicled quadriceps tendon graft shows favourable results at a minimum of 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1210-1215. [DOI] [PubMed] [Google Scholar]
- 29. Neri T, Parker DA, Putnis S, et al. Clinical and radiological predictors of functional outcome after isolated medial patellofemoral ligament reconstruction at midterm follow-up. Am J Sports Med. 2019;47(6):1338-1345. [DOI] [PubMed] [Google Scholar]
- 30. Nha KW, Bae JH, Hwang SC, et al. Medial patellofemoral ligament reconstruction using an autograft or allograft for patellar dislocation: a systematic review. Knee Surg Relat Res. 2019;31(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Repo JP, Uimonen MM, Nevalainen MT, et al. Outcomes following the operative treatment of intra-articular fracture combined with medial patellofemoral ligament reconstruction after patellar dislocation. Knee Surg Relat Res. 2022;34(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Schiphouwer L, Rood A, Tigchelaar S, Koëter S. Complications of medial patellofemoral ligament reconstruction using two transverse patellar tunnels. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):245-250. [DOI] [PubMed] [Google Scholar]
- 33. Schlumberger M, Schuster P, Hofmann S, et al. Midterm results after isolated medial patellofemoral ligament reconstruction as first-line surgical treatment in skeletally immature patients irrespective of patellar height and trochlear dysplasia. Am J Sports Med. 2021;49(14):3859-3866. [DOI] [PubMed] [Google Scholar]
- 34. Schneider DK, Grawe B, Magnussen RA, et al. Outcomes after isolated medial patellofemoral ligament reconstruction for the treatment of recurrent lateral patellar dislocations: a systematic review and meta-analysis. Am J Sports Med. 2016;44(11):2993-3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Schoettle PB, Zanetti M, Seifert B, et al. The tibial tuberosity-trochlear groove distance: a comparative study between CT and MRI scanning. Knee. 2006;13(1):26-31. [DOI] [PubMed] [Google Scholar]
- 36. Schöttle PB, Fucentese SF, Romero J. Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):516-521. [DOI] [PubMed] [Google Scholar]
- 37. Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801-804. [DOI] [PubMed] [Google Scholar]
- 38. Siebold R, Chikale S, Sartory N, et al. Hamstring graft fixation in MPFL reconstruction at the patella using a transosseous suture technique. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1542-1544. [DOI] [PubMed] [Google Scholar]
- 39. Smirk C, Morris H. The anatomy and reconstruction of the medial patellofemoral ligament. Knee. 2003;10(3):221-227. [DOI] [PubMed] [Google Scholar]
- 40. Song SY, Kim IS, Chang HG, et al. Anatomic medial patellofemoral ligament reconstruction using patellar suture anchor fixation for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2431-2437. [DOI] [PubMed] [Google Scholar]
- 41. Song SY, Pang CH, Kim CH, et al. Length change behavior of virtual medial patellofemoral ligament fibers during in vivo knee flexion. Am J Sports Med. 2015;43(5):1165-1171. [DOI] [PubMed] [Google Scholar]
- 42. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;(198):43-49. [PubMed] [Google Scholar]
- 43. Wagner D, Pfalzer F, Hingelbaum S, et al. The influence of risk factors on clinical outcomes following anatomical medial patellofemoral ligament (MPFL) reconstruction using the gracilis tendon. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):318-324. [DOI] [PubMed] [Google Scholar]
- 44. Wang HD, Dong JT, Gao SJ. Medial patellofemoral ligament reconstruction using a bone groove and a suture anchor at patellar: a safe and firm fixation technique and 3-year follow-up study. J Orthop Surg Res. 2016;11(1):138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Woodmass JM, Johnson NR, Cates RA, et al. Medial patellofemoral ligament reconstruction reduces radiographic measures of patella alta in adults. Orthop J Sports Med. 2018;6(1):2325967117751659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Yoo YS, Chang HG, Seo YJ, et al. Changes in the length of the medial patellofemoral ligament: an in vivo analysis using 3-dimensional computed tomography. Am J Sports Med. 2012;40(9):2142-2148. [DOI] [PubMed] [Google Scholar]
- 47. Yoon KH, Kim EJ, Kwon YB, Hwang IU, Kim SG. Comparison of clinical and radiological outcomes between transosseous tunnel and suture anchor patellar fixation for medial patellofemoral ligament reconstruction: a cohort study with 2-year follow-up. Orthop J Sports Med. 2020;8(5):2325967120917660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Zheng X, Hu Y, Xie P, et al. Surgical medial patellofemoral ligament reconstruction versus non-surgical treatment of acute primary patellar dislocation: a prospective controlled trial. Int Orthop. 2019;43(6):1495-1501. [DOI] [PubMed] [Google Scholar]


