Abstract
Immune reconstitution inflammatory syndrome is a common manifestation in human immunodeficiency virus (HIV)-positive patients infected with tuberculosis (TB). One of the unusual complications of this condition is the development of psoas abscess. We describe a case of immune reconstitution inflammatory syndrome (IRIS) in a patient with disseminated TB under treatment, HIV-positive with a low CD4 cell count, complicated by bilateral psoas abscess. Our patient presented with fever, abdominal pain, and lymphadenopathy, typical symptoms of TB-IRIS. Diagnosis was confirmed by surgical drainage of the abscess of the right iliac psoas muscle with detection of acid-fast bacteria on Ziehl-Neelsen staining and negative culture of purulent discharge. Treatment with prednisone was started in addition to continuation of antituberculosis therapy and antiretroviral therapy.
Keywords: immune reconstitution inflammatory syndrome, tuberculosis, psoas abscess, HIV, antiretroviral therapy
Introduction
Paradoxical immune reconstitution inflammatory syndrome associated with tuberculosis (Paradoxical TB-IRIS) consists of worsening TB symptoms and signs despite a favorable response to antituberculosis therapy (ATT) prior to antiretroviral therapy (ART). Paradoxical TB-IRIS usually presents in the first 1 to 8 weeks after ART initiation; however, in this case, we see a late presentation after 3 months.1-4 Development of bilateral psoas abscess in our patient is a rare manifestation of paradoxical TB-IRIS with few reported cases. 5
Case Presentation
A 33-year-old male on ATT and antiretroviral therapy presented to the emergency department at Hospital Nacional Dos de Mayo, in Peru, with a 2 week history of nonradiating stabbing pain, in the right hip greater than the left, that limited walking, after a low-impact bicycle accident; and fever.
Four months prior to admission, he presented with respiratory symptoms and was found to have a CD4 count of 96 cells/mm3 and HIV viral load of 2.878.385 million copies/mL of plasma. He was diagnosed with sensitive disseminated tuberculosis (positive Ogawa culture for Mycobacterium tuberculosis in feces and sputum samples with rifampicin and isoniazid sensitivity on the line probe assay Genotype MTBDRplus). He started ATT with rifampin, isoniazid, ethambutol, and pyrazinamide; and received cotrimoxazole for prophylaxis. Four weeks later he started ART with tenofovir disoproxil fumarate (TDF), emtricitabine, and efavirenz. ART was changed to TDF, emtricitabine, lopinavir, and ritonavir; and the dose of lopinavir/ritonavir was doubled 2 months prior to admission. At that time, HIV viral load had dropped to 1 million.
On physical examination, the abdomen was distended with diffuse dullness to percussion and intense pain with abduction and extension of the right leg; and decreased muscle strength. Laboratory test results are shown in Table 1. The clinical presentation, and the medical history of the patient, raised suspicion of an infectious process.
Table 1.
Laboratory Data.
| Variable | Reference range | 3 Days prior to hospitalization | Day 1 | Day 2 | Day 26 | Day 27 | Day 30 | Day 31 | 2 Months after hospitalization | |
|---|---|---|---|---|---|---|---|---|---|---|
| Hemoglobin (g/dL) | 13.5-17.5 | 9.5 | 8.2 | — | — | — | 8.5 | — | — | |
| Hematocrit (%) | 41-53 | 30.6 | 26.4 | — | — | — | 26.7 | — | — | |
| White-cell count (per μL) | 4000-12000 | 13 630 | 10 910 | — | — | — | 4520 | — | — | |
| Platelet count (per μL) | 150 000-450 000 | 569 000 | 444 000 | — | — | — | 350 000 | — | — | |
| Lactate dehydrogenase (U/L) | 313-618 | 496 | 413 | — | — | — | — | — | — | |
| Erythrocyte sedimentation rate (mm/h) | 0-20 | 105 | 105 | — | — | — | — | — | — | |
| C-reactive protein (mg/L) | 0-10 | 233 | — | — | — | — | 27.9 | — | — | |
| Alanine aminotransferase (U/L) | 9-52 | — | 25.8 | — | — | 37.5 | — | — | ||
| Aspartate aminotransferase (U/L) | 14-36 | — | 65.6 | — | — | 17.3 | — | — | ||
| Gamma-glutamyl transferase (U/L) | 12-43 | — | 287 | — | — | 348 | — | — | ||
| Alkaline phosphatase (U/L) | 38-126 | — | 190 | — | — | 98 | — | — | ||
| Blood culture | — | Negative | — | — | — | — | — | |||
| Mycobacterium tuberculosis | Gram of abdominal discharge | — | — | — | Negative | — | — | — | — | |
| Baciloscopy (Ziehl-Neelsen) | — | Urine: negative | — | — | Abdominal abscess: positive (++) | — | Sputum: negative, stool: negative | — | ||
| Culture of abdominal discharge | — | — | — | — | — | — | — | Negative | ||
The patient initiated treatment with vancomycin and ceftriaxone. Blood cultures and image studies were requested. One week after admission, the requested contrast-enhanced abdominal computed tomography showed multiple enlarged nodes in the gastric, mesenteric, and periaortic regions with hypodense centers and collections were observed over both psoas muscles (Figure 1).
Figure 1.
Abdominal computed tomography with contrast in the coronal (A) and axial (B) planes. Collections in both psoas muscles, predominantly in the right psoas with an extension of 209×75×72 mm and the left collection measured 111×37×38 mm.
The patient received vancomycin and ceftriaxone for 10 days. However, as the pain and fever continued, combined with abdominal pain in the right iliac region, it was decided to change antibiotics to metronidazole and ceftriaxone to cover an intra-abdominal infection. Corticoids were also administrated.
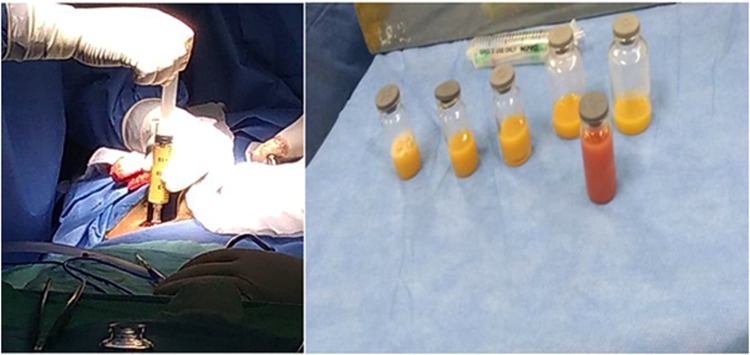
The patient underwent surgical drainage of the abscess of the right iliac psoas muscle, 350 cc of purulent secretion was obtained (Figure 2) and a Jackson-Pratt drain was placed. In the Gram stain of the purulent material, no microorganisms were detected. Bacilloscopy and culture on Ogawa medium were performed to verify the presence of M. tuberculosis. The bacilloscopy samples were positive for acid-fast bacteria on Ziehl-Neelsen stain (Table 1).
Figure 2.
Right psoas abscess drainage. Purulent discharge 350cc.
Jackson-Pratt drain and antibiotics metronidazole and ceftriaxone were removed 5 days after surgery. Some days later, the patient was discharged due to clinical improvement, and continued ATT and ART with prednisone. HIV viral load was undetectable and CD4 count was 531 cell/mm3 1 month after the current disease. The abdominal abscess culture on Ogawa medium for tuberculosis was negative after 2 months (Table 1).
Discussion
The main risk factors for paradoxical TB-IRIS are low CD4 cell count at ART initiation (<100 cells/mm3), high HIV viral load prior to ART (>100,000 copies/mL) and disseminated or extra-pulmonary TB before ART1-7; all present in our patient. The incidence of paradoxical TB-IRIS in adult HIV-positive patients is 18% and the mortality attributable to paradoxical TB-IRIS is 2%. 5 In severe paradoxical TB-IRIS, the first-line treatment is the use of corticosteroids, and it is the only therapeutic intervention so far supported by a randomized clinical trial. 8 The patient was prescribed prednisone.
Antiretroviral therapy should not be interrupted in patients with IRIS; except in life-threatening cases.1,4 Additionally, the risks of discontinuing ART include the acquisition of new opportunistic infections, recurrence of IRIS when treatment is restarted later, and the emergence of ART resistance.3,4
Our patient had disseminated tuberculosis under treatment. Positive smears for acid-fast bacteria on Ziehl-Neelsen stain, negative culture on Ogawa medium and improvement of the patient without the need for change of TB treatment regimen or treatment for other mycobacteria suggests the presence of nonviable M. tuberculosis in the smears and efficacy of anti-TB treatment. Also, it is important to remember that despite the severe inflammation typical of TB-IRIS, the paucity or absence of viable M. tuberculosis is characteristic of this presentation.3,7 This explains the cause of the bilateral psoas abscess in our patient.
On the other hand, psoas muscle is very prone to primary and secondary infections due to its large blood and lymphatic supply and its proximity to retroperitoneal structures. Treatment of psoas abscesses includes intravenous antibiotics and percutaneous or open surgical drainage, depending on the patient's condition and available materials. 9 In this case, surgical drainage was performed due to the retroperitoneal location of the right psoas abscess.
The presence of an inflammatory condition after recent initiation of antiretroviral therapy and worsening of previously diagnosed and on treatment TB (psoas abscess with acid-fast bacteria); the lack of another infectious process or undiagnosed multidrug-resistant TB, proven by negative blood cultures and negative culture on Ogawa medium; and the absence of conditions that reduce the efficacy of anti-TB drugs in the patient (poor compliance, drug malabsorption, and drugs side effects) confirm the diagnosis of paradoxical TB-IRIS.1-7
Conclusion
We describe the first reported case of psoas abscess as a complication of TB-IRIS in Peru. The case described demonstrates the need for careful management and ongoing assessment of patients receiving ART, especially if an opportunistic infection such as M. tuberculosis is also present. This case reinforces the use of corticosteroids as first-line treatment for severe TB-IRIS.
Footnotes
Authors’ Contribution: AMC-E was involved in writing—review & editing and visualization; VRSS in writing—original draft; HA-D and JEB-B in writing—review & editing; and PLR in writing—original draft, writing—review & editing, and supervision.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval and Informed Consent: Our institution does not require ethical approval for reporting individual cases or case series. Verbal informed consent was obtained from the patient for the publication of this case report.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Adriam M. Castilla-Encinas https://orcid.org/0009-0006-2837-6423
References
- 1.Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV. National Institutes of Health, Centers for Disease Control and Prevention, HIV Medicine Association, and Infectious Diseases Society of America. Available at: https://clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-opportunistic-infections/mycobacterium?view=full (accessed 24 August 2024) [Google Scholar]
- 2.Thapa S, Shrestha U. Immune reconstitution inflammatory syndrome. StatPearls Publishing; 2024, PMID: 33620872. [PubMed] [Google Scholar]
- 3.Walker NF, Scriven J, Meintjes G, Wilkinson RJ. Immune reconstitution inflammatory syndrome in HIV-infected patients. HIV AIDS (Auckl). 2015;7:49-64. doi: 10.2147/HIV.S42328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brust JCM, McGowan JP, Fine SM, et al. Management of immune reconstitution inflammatory syndrome (IRIS). Johns Hopkins University; 2024, PMID: 34029021. [PubMed] [Google Scholar]
- 5.Namale PE, Abdullahi LH, Fine S, Kamkuemah M, Wilkinson RJ, Meintjes G. Paradoxical TB-IRIS in HIV-infected adults: a systematic review and meta-analysis. Future Microbiol. 2015;10(6):1077-1099. doi: 10.2217/fmb.15.9 [DOI] [PubMed] [Google Scholar]
- 6.Meintjes G, Lawn SD, Scano F, et al. Tuberculosis-associated immune reconstitution inflammatory syndrome: case definitions for use in resource-limited settings. Lancet Infect Dis. 2008;8(8):516-523. doi: 10.1016/S1473-3099(08)70184-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lanzafame M, Vento S. Tuberculosis-immune reconstitution inflammatory syndrome. J Clin Tuberc Other Mycobact Dis. 2016;3:6-9. doi: 10.1016/j.jctube.2016.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meintjes G, Wilkinson RJ, Morroni C, et al. Randomized placebo-controlled trial of prednisone for paradoxical tuberculosis-associated immune reconstitution inflammatory syndrome. AIDS. 2010;24(15):2381-2390. doi: 10.1097/QAD.0b013e32833dfc68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aboobakar R, Cheddie S, Singh B. Surgical management of psoas abscess in the human immunodeficiency virus era. Asian J Surg. 2018;41(2):131-135. doi: 10.1016/j.asjsur.2016.10.003 [DOI] [PubMed] [Google Scholar]