Abstract
Inflammatory myofibroblastic tumor and liposarcoma very rarely present as tumors of the chest wall. Never have both been reported together in the same lesion. We present a case wherein a 72-year-old man with a rapidly progressing lesion initially mistaken for a local infection underwent resection with diagnosis of inflammatory myofibroblastic tumor. He experienced recurrence less than 6 months before radical resection revealed well to dedifferentiated liposarcoma with areas of inflammatory myofibroblastic tumor. He is now doing well with over 4 years of follow-up.
Keywords: Oncology, pathology, surgery, inflammatory myofibroblastic tumor, liposarcoma, chest wall tumor, costochondritis, chest wall reconstruction, chest wall surgery
Introduction
Primary chest wall tumors are rare, with incidence reported to be less than 2%. 1 Inflammatory myofibroblastic tumors (IMTs) are rare benign mesenchymal lesions, which are occasionally locally invasive when found in young adults and children. IMTs occur in the hepatobiliary, gastrointestinal, and genitourinary tracts in addition to the retroperitoneum, lung, tracheobronchial tree, heart, mediastinum and chest wall. 2 The true incidence of IMT is unclear as the term now encompasses older pathologic diagnoses of benign fibrohistiocytoma, plasma cell granuloma, and inflammatory pseudotumor. 2 Chest wall IMTs are very rare and have seldom been reported.3,4 Liposarcomas of the chest wall are also quite rare.1,5,6 There are no reported cases of chest wall liposarcomas arising with or misdiagnosed as IMT. IMTs when occurring concomitantly with other tumors have previously been considered to represent distinct processes since they have differing chromosomal rearrangements. 7 The pathogenesis of IMTs is ambiguous; they may stem from local trauma or immunosuppression.2,7,8 IMTs have been occasionally described as having gelatinous components. 7
Besides diagnosis, management can also be confounding. The optimal management is surgical resection with negative margins for both IMT and liposarcoma. However, liposarcoma, as a malignant diagnosis, may merit margins up to 5 cm. 1 Medical therapies have been reported for unresectable disease.2,7
We present a cautionary case report wherein a rapidly progressing lesion initially mistaken for a local infection was resected and diagnosed as IMT, only to recur in less than 6 months before radical resection revealed a liposarcoma with areas of IMT. This is the first such presentation of these two rare entities reported in the literature and is especially noteworthy for the rapidity of its progression.
Case discussion
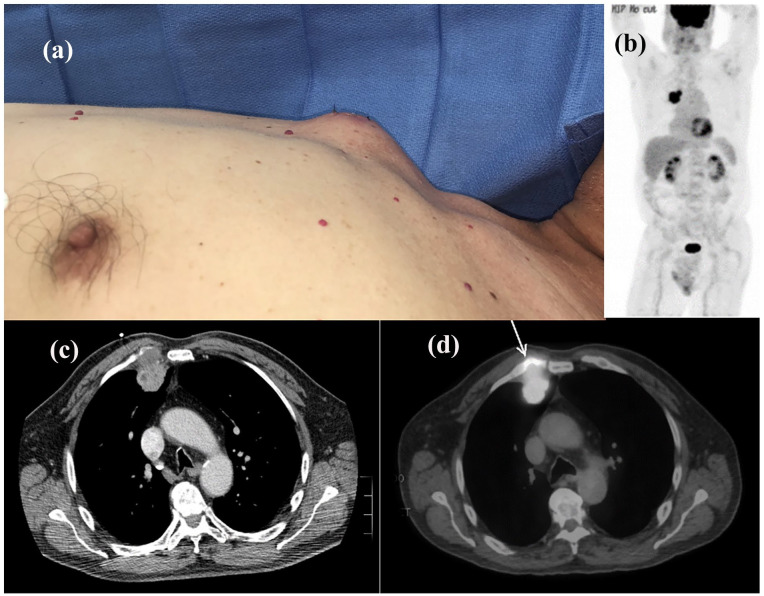
A 72-year-old man with history of hypertension, reflux, and prostate cancer treated with definitive radiation therapy presented to his primary care doctor with the complaint of an anterior chest mass arising between his right second and third ribs. He was treated with a prolonged course of antibiotics for presumed costal cartilage infection. With no remission in the painful mass 2 months later, interventional radiology made multiple biopsy attempts resulting in nonspecific pathologic diagnoses: atypical spindle cell proliferation, abscess, and fragments of fibroconnective tissue. At 4 months, a CT PET showed a hypermetabolic 5.4 cm × 3.3 cm × 3.7 cm mass arising in the area of the second and third rib cartilages with mild bony destruction and no lymph node involvement (Figure 1), so he was referred to thoracic surgery.
Figure 1.
Prior to initial resection. (a) Anterior chest mass, (b) CT PET whole-body, (c) CT axial, and (d) CT PET axial, arrow marking osseous avidity.
Video-assisted thoracoscopy showed the mass adherent to the underside of the chest wall and the lung itself. Frozen and permanent section showed only nonspecific necrotic tissue. The following day, the subfascial mass was almost completely resected along with necrotic costal cartilage. No rib invasion was noted. Pathology consultation from Mayo Clinic on this first operative specimen yielded IMT. Stains were positive for muscle specific actin (MSA), B-catenin, vimentin, and D2-40. Stains were negative for alpha smooth muscle actin (SMA), CD99, p53, desmin, cytokeratin AE1/AE3, S-100, CD34, BCL-2, calretinin, and anaplastic lymphoma kinase (ALK). Out of abundance of caution despite the benign diagnosis, surveillance CT scanning was performed every 3 months postoperatively. At 3 months, the mass had not grown. By 6 months, the mass had regrown to 7 cm and became increasingly symptomatic. Repeat CT PET again showed increased avidity in this region (Figure 2) and nowhere else.
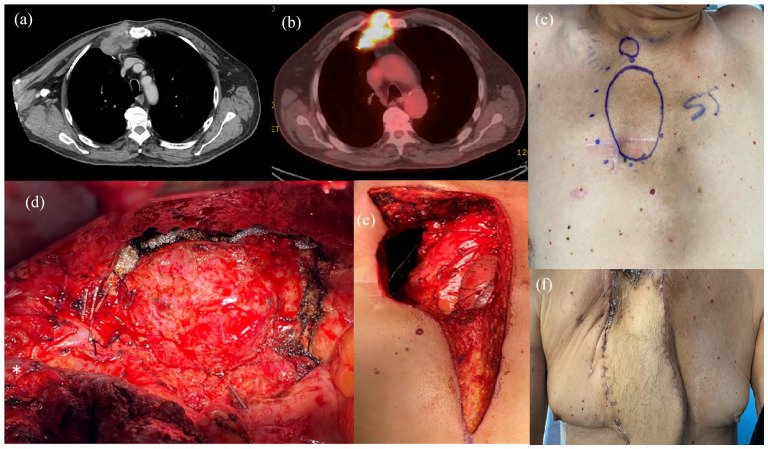
Figure 2.
Re-resection. (a) Regrowth and osteal erosion on 6-month interval CT. (b) Recurrence of avidity on 6-month interval CT PET. (c) Anterior chest wall recurrence with prior resection scar encircled by preoperative plastic surgery markings. (d) Tumor visualized through right posterolateral thoracotomy. Clips are placed on the mammary vessels and branches. Subclavian vein in the lower left-hand corner marked with (*). (e) Postresection anterior chest wall defect with visible mediastinum. The pectoralis muscles were detached from the clavicle to avoid vein injury during the first rib resection, (f) Clinic visit, 1 month postoperatively.
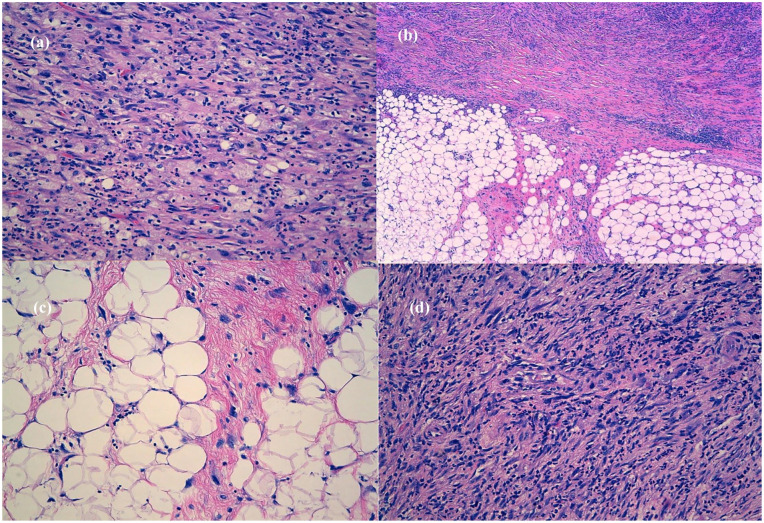
The patient was offered aggressive re-resection of a presumed recurrent benign tumor. Bronchoscopy confirmed no endobronchial involvement. A 7-hr adhesiolysis through a posterior lateral thoracotomy was required to mobilize the lung, pericardium, and great vessels away from the tumor involving the first, second, and third ribs. The right internal mammary vessels were identified and divided (Figure 2). The patient was repositioned, and the mass was approached anteriorly via a partial sternotomy. The mass was resected en bloc along with the first through third ribs. The goal was grossly near-negative margins without extensive morbidity for what at time of operation was still a benign diagnosis. Laterally, the margin was lateral to the prior resection scar. Medially, the margin was the partial sternotomy, where the mass was laboriously dissected from the adherent mediastinal fat. The defect was closed with Marlex mesh, and a TRAM flap was created by plastic surgery (Figure 2). Mayo Clinic pathology consultation revised the original diagnosis to well to dedifferentiated liposarcoma with areas of IMT (Figure 3). The liposarcoma was grade three with two mitoses per 10 high powered fields. Oncogene mouse double minute 2 homologue (MDM2) (12q15) amplification was confirmed by fluorescence in situ hybridization. In two blocks, the margins were microscopically positive from the lateral and the medial/deep sections.
Figure 3.
Final tumor pathology. (a) IMT-like areas: elongated myofibroblasts containing abundant eosinophilic cytoplasm and vesicular nuclei, loose stroma with abundant neutrophils, lymphocytes, and few plasma cells (H&E, 20×), (b) interface between well-differentiated liposarcoma with dedifferentiated foci, well-differentiated liposarcoma with abrupt transition to a nonlipogenic sarcoma (H&E, 5×), (c) well-differentiated liposarcoma component: mature fat with variably sized adipocytes and thick fibrotic bands containing characteristic atypical spindle cells with enlarged, hyperchromatic nuclei. The diagnosis is made by noting the presence of these fibrous bands containing atypical spindle cells (H&E, 20×), (d) cellular high-grade areas of sarcoma component: haphazardly distributed hyperchromatic atypical spindle cells in a fibrous stroma associated mixed inflammatory infiltrate (H&E, 20×).
The patient recovered over a week in the intensive care unit and was well healed by his first clinic visit at 1 month postoperatively (Figure 2). Regarding the positive margins, the local multidisciplinary tumor board recommended close surveillance. It has now been over 4 years since his resection with no sign of recurrence.
Conclusion
The pathological etiology in this case remains obscure. It is unclear whether a small focus of liposarcoma was left behind at the initial resection of a large IMT, whether a new liposarcoma subsequently arose within the context of a recurrent IMT, or whether an IMT itself was a precursor for liposarcoma. The necrotic core may have confounded the initial diagnosis. The key consideration in this case is the potential diagnostic confusion between local infection, IMT, and liposarcoma. Surveillance schedules and operative plans should be arranged accordingly, especially with a rapidly progressing lesion during a pandemic.
Acknowledgments
The authors thank the patient and his family for the opportunity to participate in his care.
Footnotes
Author contributions: FP conducted clinical care, conceived of the report, and authored the manuscript. AT, ACHL, and AG authored the manuscript. MT provided the pathologic diagnoses and descriptions for the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed consent: Written informed consent was obtained from the patient for their anonymized information to be published in this article.
ORCID iD: Andy Tully  https://orcid.org/0000-0003-2109-4504
https://orcid.org/0000-0003-2109-4504
References
- 1. Shah AA, D’Amico TA. Primary chest wall tumors. J Am Coll Surg 2010; 210(3): 360–366. [DOI] [PubMed] [Google Scholar]
- 2. Surabhi VR, Chua S, Patel RP, et al. Inflammatory myofibroblastic tumors: current update. Radiol Clin North Am 2016; 54(3): 553–563. [DOI] [PubMed] [Google Scholar]
- 3. Lee HJ, Kim JS, Choi YS, et al. Treatment of inflammatory myofibroblastic tumor of the chest: the extent of resection. Ann Thorac Surg 2007; 84(1): 221–224. [DOI] [PubMed] [Google Scholar]
- 4. Arikanoglu Z, Akbulut S, Basbug M, et al. Benign fibrous histiocytoma arising from the intercostal space. Gen Thorac Cardiovasc Surg 2011; 59(11): 763–766. [DOI] [PubMed] [Google Scholar]
- 5. Carillo GAO, Ramos MB, Parga GDC, et al. Thoracic liposarcoma: resection and chest wall reconstruction. Asian Cardiovasc Thorac Ann 2014; 22(9): 1112–1115. [DOI] [PubMed] [Google Scholar]
- 6. Lee YJ, Cha WJ, Kim Y, et al. The recurrence of well-differentiated liposarcoma from benign giant intramuscular lipoma: a case (CARE-compliant) report. Medicine (Baltimore) 2021; 100(6): e24711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kovach SJ, Fischer AC, Katzman PJ, et al. Inflammatory myofibroblastic tumors. J Surg Oncol 2006; 94(5):385–391. [DOI] [PubMed] [Google Scholar]
- 8. Héluain V, Hermant C, Borel C, et al. Bronchoscopic treatment of endobronchial inflammatory myofibroblastic tumors. Ann Thorac Surg 2021; 111(2): e109–e111. [DOI] [PubMed] [Google Scholar]