Abstract
Background:
Researchers have developed several instruments to measure recovery capital—the social, physical, human, and cultural resources that help people resolve alcohol and other drug problems. However, existing measures are hampered by theoretical and psychometric weaknesses. The current study reports on process and psychometric outcomes for the Multidimensional Inventory of Recovery Capital (MIRC), a novel measure of recovery capital.
Methods:
We used a three-phase, mixed methods approach to develop the MIRC. Individuals who identified as having resolved alcohol problems were recruited in each phase. Phase one focused on item development, with participants providing qualitative feedback on potential items. In phase two (pilot testing) and phase three (final psychometric evaluation), participants completed revised versions of the MIRC to assess its psychometric strength and item performance.
Results:
Phase one (n=44) resulted in significant item alteration, culminating in a 48-item pilot measure. Pilot testing analyses (n=497) resulted in the deletion or replacement of 17 items. In the final psychometric evaluation (n=482), four additional items were deleted, resulting in a 28-item MIRC comprising four subscales measuring social, physical, human, and cultural capital. The psychometric properties of the final MIRC and its subscales ranged from sound to strong, with high response variability suggesting appropriate item discrimination.
Conclusion:
Results confirm the psychometric strength of the MIRC and underscore the importance of incorporating the insights of diverse samples of people in recovery. The MIRC holds promise as an assessment tool in future research and is available for use at no cost in treatment and community-based settings.
Keywords: alcohol, measure, psychometric, recovery, recovery capital
1. Introduction
There is a growing consensus among stakeholders that resolving alcohol and other substance use disorders, or recovering, is a complex and dynamic process of change extending beyond abstinence (Kaskutas et al., 2014; Laudet, 2007; Witkiewitz et al., 2020). Recognizing this, the National Institute on Alcohol Abuse and Alcoholism (NIAAA) defines recovery as a process and an outcome marked by the remission of Alcohol Use Disorder (AUD) criteria as specified in the DSM-5, cessation of heavy drinking, and improvements in well-being (Hagman et al., 2022). Relatedly, the concept of recovery capital (Cloud & Granfield, 2001; Granfield & Cloud, 1999) has broadened notions of recovery by aiming to capture the full spectrum of recovery determinants within a resource-based ecological framework.
The concept of recovery capital was initially developed among a sample of individuals who resolved their substance use problems without treatment, known as natural recovery (Cloud & Granfield, 2001). Although the original theory centered on social capital within this context (i.e., social networks and resources that promote recovery), Cloud and Granfield (2008) later expanded recovery capital to include physical, human, and cultural capital. Physical capital encapsulates the tangible resources that impact recovery, such as finances, transportation, and housing. Human capital includes internal resources involved in recovery, such as mental and physical health, having a hopeful outlook, and motivation. Finally, cultural capital includes cultural and community determinants of recovery, such as cultural traditions that are conducive to recovery and access to community-level resources. The theoretical expansion also introduced negative capital, referring to factors within each of the four domains that deter recovery (Cloud & Granfield, 2008).
Recovery capital has been researched among many populations, including adolescents, people in rural communities, formerly incarcerated individuals, older adults, and people with varying levels of treatment experience (Hennessy et al., 2019; LaBarre et al., 2021; Lyons & Lurigio, 2010; Palombi et al., 2019). Across populations, researchers have theorized that recovery capital can act as a mechanism that reduces psychological distress and promotes sustained recovery (Kelly & Hoeppner, 2015). In sum, recovery capital comprises internal and external resources that interact with the environment across time and domains in dynamic fashion, influencing one’s ability to meet recovery goals (Best & Hennessy, 2022).
1.1. Recovery capital measurement
Since the concept debuted in the literature more than two decades ago, interest in recovery capital measurement has increased steadily. We identified six measurement tools to assess recovery capital. Sterling and colleagues (2008) created a 23-item measure of recovery capital culled from existing assessments. Similarly, Burns and Mark (2013) created a seminal Recovery Capital Questionnaire (RCQ) based on Cloud and Granfield’s (2008) conceptualization. Though these two scales provided an essential foundation for measurement, neither has been extensively tested since their initial formation. The Assessment of Recovery Capital (ARC) and its briefer version, the BARC-10, are the most widely utilized contemporary recovery capital measures (Groshokova et al., 2013; Vilsaint et al., 2017). In addition, Hanauer and colleagues (2019) developed a ten-item measure that mirrors the BARC-10’s theoretical structure. Finally, the REC-CAP allows patients in recovery to assess their recovery capital access over time (Cano et al., 2017; see http://www.recoveryoutcomes.com/rec-cap/) and is accessed through a paid software system.
Though existing tools have helped assess recovery capital in research and practice, conceptual inconsistencies have constrained research advancement on this multifaceted construct (Best & Hennessy, 2022; Hennessy, 2017). For instance, with exception of the REC-CAP, which assesses recovery barriers, the RCQ, ARC, and BARC-10 do not systematically assess negative recovery capital. Furthermore, the ARC, BARC-10, and the scales developed by Sterling et al. (2008) and Hanauer et al. (2019) contain items that do not reflect recovery capital theory, such as items implying an abstinence-centered view of recovery (Bowen et al., 2020; Cloud & Granfield, 2008). Additionally, although most of the U.S. population that has resolved an alcohol use disorder has done so without formal treatment (Tucker et al., 2020), to our knowledge, all prior measures were primarily or exclusively tested among individuals in clinical and self-help settings. Finally, the ARC and BARC-10 were created without significant community involvement in developing measurement items and evaluated within somewhat homogenous samples. For instance, the BARC-10 was tested with a sample that was 93% White (Vilsaint et al., 2017). In light of these limitations, our research team aimed to develop a robust new measure of recovery capital, termed the Multidimensional Inventory of Recovery Capital (MIRC).
1.2. Current study
The purpose of this paper is to describe the development and psychometric evaluation of the MIRC. We aimed to address the limitations of previously developed measures through the inclusion of physical, human, social, and cultural capital domains, as well as the assessment of negative capital within each domain (Cloud & Granfield, 2008). Furthermore, we sought to create items aligned with recovery capital theory, informed by the insights of a diverse sample of individuals representing multiple recovery pathways (i.e., individuals in natural recovery or using a combination of treatment and self-help resources). The MIRC is intended to assess recovery capital in adults (age 18 and over) at any time point in recovery in a range of community settings (e.g. outpatient treatment; social service programs; self-assessment).
We used a three-phase, mixed methods approach to develop and test the MIRC, as conveyed in Figure 1. In this paper, we summarize the results of each phase, including the development and vetting of measurement items with a sample of service providers and people in recovery (Phase 1); psychometric evaluation of item performance and scale reliability for the pilot MIRC (Phase 2); and psychometric evaluation of item performance, reliability, and validity for the final MIRC (Phase 3).
Figure 1:
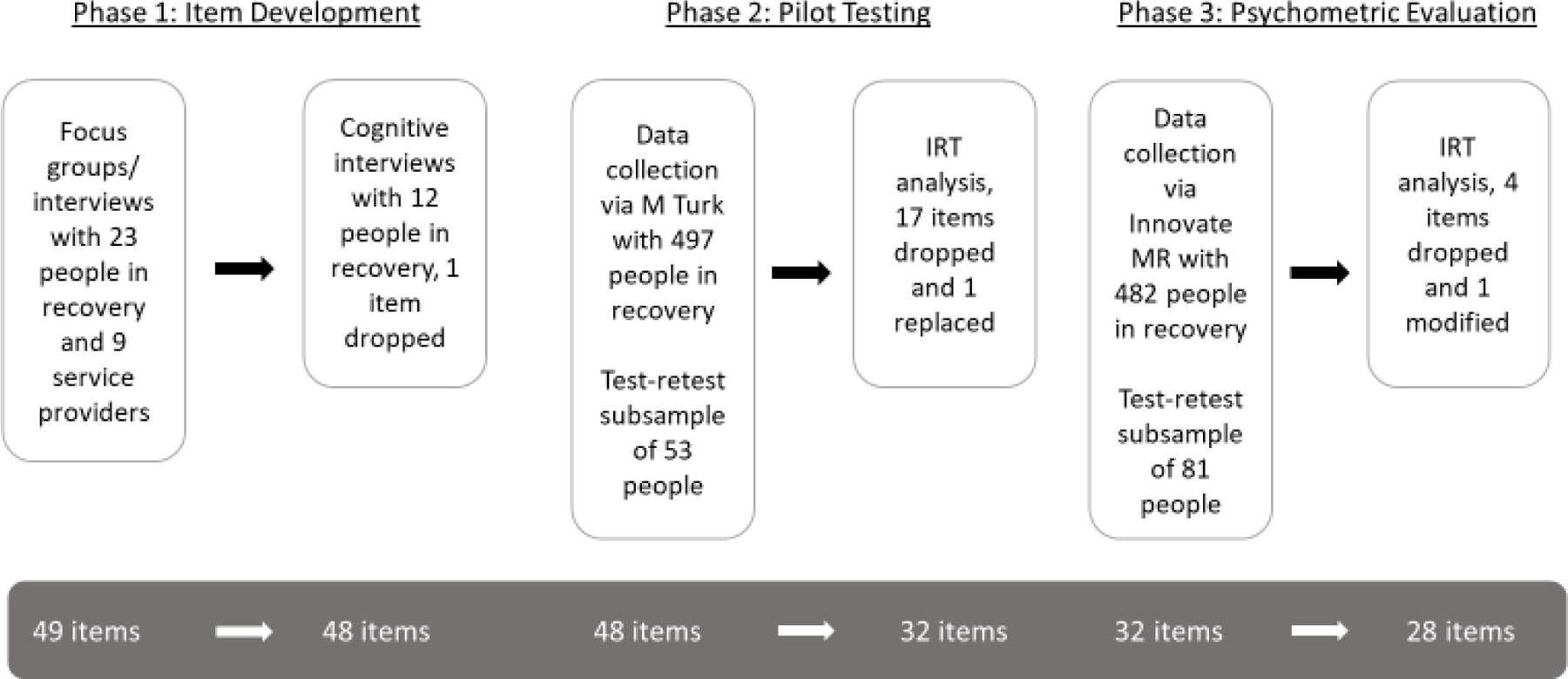
Overview of MIRC development and evaluation process
2. Methods
2.1. Overview
Participant eligibility across the three phases was based on the following criteria: (1) age 18 or older; (2) living in the United States; (3) able to communicate in English; and (4) identifying as having resolved a prior problem with alcohol (alone or with other drugs) for at least 30 days. Our focus on alcohol recovery was informed by funder priorities as well as recognition of the unique recovery context of alcohol as a legal and widely available and acceptable substance. In addition, service providers in the addiction treatment field were included in the item development phase, as described below. Data collection took place between October 2020 and April 2022 and all study procedures were approved by the University at Buffalo Institutional Review Board.
2.2. Sample characteristics
Table 1 summarizes characteristics of the sample across study phases. The item development sample included people in recovery from alcohol problems (n=35) and nine service providers, who are not included in the table as providers did not complete recovery-related measures. The pilot testing (n=497) and final psychometric evaluation (n=482) samples were diverse with regard to gender, race, ethnicity, and sexual orientation and included 40–45% lower income individuals. The final evaluation sample closely reflected 2020 Census demographics for the U.S. over-18 population, with minor over-representation of individuals identifying only as White (70.8% vs. 64.1% Census) and American Indian (5% vs. 1.1% Census) and under-representation of Asian Americans (2.9% vs. 6.1% Census) and individuals identifying as more than one race (3.9% vs. 8.8% Census).
Table 1:
Sample characteristics
| Characteristic | Item development (Phase 1) (n=35) % |
Pilot testing (Phase 2) (n=497) % |
Psychometric evaluation (Phase 3) (n=482) % |
|---|---|---|---|
| Gender Cisgender female Cisgender male Other gender identities |
57.1 37.1 5.7 |
43.7 54.5 1.6 |
48.8 50.2 1.0 |
| Race American Indian Asian American Hawaiian / Pacific Islander Black White More than one race Other race |
2.9 0 0 34.3 51.4 8.6 2.9 |
2.2 2.8 0 8.3 84.5 1.2 1.0 |
5.0 2.9 0.4 11.6 70.8 3.9 5.4 |
| Hispanic/Latinx ethnicity | 5.7 | 17.2 | 17.2 |
| Sexual orientation Gay or lesbian Heterosexual Bisexual Other |
5.7 68.6 22.9 2.9 |
4.8 77.8 16.3 1.0 |
6.0 83.0 8.3 1.9 |
| Age in years (M) | 44 | 39 | 43 |
| Education – bachelors or greater | 54.3 | 72.6 | 25.7 |
| Low-income (< 200% federal poverty level) | 42.9 | 45.4 | 40.9 |
| Time since resolving alcohol problems > 5 years 1–5 years 6–12 months 3–6 months 1–3 months |
40.0 14.3 17.1 20.0 8.6 |
13.1 14.8 20.3 29.1 22.8 |
34.0 40.9 10.0 7.1 8.1 |
| Treatment and self-help group history Ever received inpatient treatment Ever received outpatient treatment Attended self-help groups in past 30 days (in person or online) Attended self-help groups previously but not in past 30 days Natural recovery |
45.7 52.9 54.3 22.9 8.6 |
19.3 33.1 34.8 29.2 23.1 |
27.6 39.4 23.7 39.8 31.7 |
| SIP Score (range 0–15) – Alcohol (M) | 12.5 | 9.4 | 10.2 |
| Current alcohol use None Monthly or less 2–4 times/month Weekly or greater |
62.9 25.7 2.9 8.6 |
24.4 22.5 27.8 25.4 |
47.7 25.5 13.1 13.7 |
Note. Natural recovery was defined as having no lifetime history of participation in inpatient treatment, outpatient treatment, or any self-help group (online or in-person).
Participants in early, middle, and long-term recovery were represented across the three samples. Although most participants had experience with treatment and/or mutual aid groups, a substantial minority met the definition for natural recovery, including 23.1% in pilot testing and 31.7% in psychometric evaluation. Mean scores on the Short Inventory of Problems (SIP)-Lifetime version, an indicator of alcohol problem severity (Morse & Roberson, 2017; range 0–15), were 12.5 in item development, 9.4 in pilot testing, and 10.2 in psychometric evaluation. The majority of participants reported no or occasional alcohol use (monthly or less), with 8.6 to 25.4% reporting regular use (weekly or greater) across the three phases.
2.3. Item development (Phase 1)
The purpose of Phase 1 was to vet and refine potential MIRC items through interviews and focus groups with people in recovery and service providers. Item development methods and results are described in depth in Bowen et al. (2022). Briefly, after preparing an initial list of items based on a literature review and consultation with nine recovery research experts, we gathered feedback on the items via seven focus groups with two to four participants each and 13 individual interviews. Data collection took place via Zoom and participants were compensated with $30 e-gift cards. Two researchers coded participants’ feedback using verbatim transcriptions and guided the research team in revising the items based on the coded results. Next, we conducted cognitive interviews (Willson & Miller, 2014) via Zoom with 12 individuals in recovery, who completed a test version of the MIRC with 49 items and described their reaction to the items and their thought process in answering them. Participants received $20 e-gift cards. Following a review of the cognitive interviewing feedback, the research team made further revisions, including dropping one item.
Only nine items from an initial list of 90 potential items were retained in their original form on the 48-item pilot MIRC. Items were organized into five subscales (social, physical, human, cultural, and community capital). Each subscale contained items measuring positive recovery capital (e.g., “my family supports my recovery” under social capital) and negative recovery capital (e.g., “I feel disconnected from my culture or not part of any culture” under cultural capital). Items had four response options: strongly disagree, disagree, agree, and strongly agree. The choice to use four options was based on Simms et al.’s (2019) finding that having a middle response option generates ambiguity and that there are diminishing returns to increasing the number of potential responses. Cognitive interviewing indicated that the question formatting and response options were acceptable to participants and easy to administer.
2.4. Pilot testing (Phase 2)
The aim of Phase 2 was to evaluate item performance, internal consistency, and test-retest reliability for the pilot MIRC in a national sample. We used Amazon’s Mechanical Turk (MTurk), a crowdsourcing platform, for recruitment and data collection (n=497). Prior research with people with alcohol problems indicates comparability between MTurk samples and samples recruited through in-person methods (Kim & Hodgins, 2017; Strickland & Stoops, 2018; Strickland et al., 2019). Potential participants completed an eligibility screening within the MTurk portal, which contained decoy questions to mask the study’s aims (e.g. “Do you use tobacco products at least once a month?”). Participants who screened as eligible were invited to take the full study survey, which included the MIRC; questions about current and past alcohol and other drug use and treatment history; the SIP-Lifetime version (Morse & Roberson, 2017); and demographic questions. Participants were compensated $4 through MTurk. A subsample of participants (n=53) retook the MIRC approximately one week later and were compensated $2.
2.5. Psychometric evaluation (Phase 3)
Following analysis of pilot testing data (described further in the results), we modified the MIRC and tested the final version in Phase 3. We used Innovate MR, a national market research and digital sampling provider, to recruit the sample (n=482). Innovate MR maintains a diverse online panel of more than 1 million respondents and employs several practices to ensure data quality, including benchmark quality testing, pattern detection, and digital fingerprinting (Lee et al., 2018). Participants completed the same survey as in the pilot testing phase, with the following measures added to calculate concurrent validity: Brief 2-Way Social Support Scale (Obst et al., 2019); Sense of Community subscale of the Perceived Neighborhood Scale (Martinez et al., 2002); and the 26-item version of the World Health Organization’s Quality of Life measure (WHOQOL-BREF; Skevington et al., 2004). A subsample (n=81) retook the MIRC approximately one week later. Participants were compensated through Innovate MR’s panel platform by earning points redeemable for gift cards worth $15-$17.
2.6. Quantitative analysis process
We reverse coded all items assessing negative recovery capital, so that higher values denoted higher levels of capital. Next, we summarized item distributions using frequencies and relative frequencies. In order to ensure that only discriminative items were included in the final MIRC, in the pilot testing phase, we utilized graded response models (GRMs), which are extensions of traditional item response models. With this approach, we summarized the discriminative ability of each item using the estimated model slope, item characteristic curve, and item information curve. Internal consistency among items designed to measure a given construct (i.e., subscale) was examined using Cronbach’s alpha and intraclass correlation coefficients (ICCs). To determine how each item reflected the overall consistency, we computed the alpha coefficient for the subscale after deleting each item. In addition, we calculated the correlation of each item with the total of the remaining items in the subscale. The test-retest reliability of individual items was assessed using simple and weighted kappa coefficients, along with corresponding 95% confidence intervals. The research team then convened to review the results and make decisions about item retention and elimination as well as subscale composition.
For the final psychometric evaluation, using the revised version of the MIRC, we applied the same methods as in the pilot testing phase to assess item discrimination, subscale and total measure internal consistency, and test-retest reliability. Furthermore, we used confirmatory factor analysis to validate GRM results through examination of the factor loadings and the squared multiple correlations. Subscale scores and the total score were calculated using the simple sum of corresponding items (following reverse coding of items measuring negative capital), which were then summarized. Construct validity, in terms of the associations between MIRC subscale scores, total score, and related measures, was examined through the use of standard scatterplots and calculated correlations. The test-retest reliability of the subscales and total measure was assessed using Bland-Altman plots and calculation of ICCs based on a fitted one-way random effects model. All statistical tests were two-sided and tested at a 0.05 nominal significance level. Analyses were carried out using SAS version 9.4 (or higher) statistical software.
3. Results
3.1. Pilot testing (Phase 2) results
Following data cleaning, we completed item and scale-level analyses on pilot testing data (n=497). The research team reviewed key item performance indicators, including changes to subscale alpha when an item was deleted; correlation with the subscale remaining total; slope; and weighted kappa for the test-retest subsample (n=53). We identified 17 poorly performing items to cut from the MIRC (see Table 2). These items were problematic in terms of low correlations with subscale totals; negative impact on Cronbach’s alpha; and low slopes associated with fitted GRMs, indicating lower item discriminability. We then prepared a revised MIRC with 32 items across four subscales (seven social capital items; eight physical capital items; nine human capital items; and eight cultural capital items) for evaluation in Aim 3. GRM slopes of these items ranged from 0.61 to 3.48. We also established the MIRC’s feasibility for self-administration, with 90% of participants completing the measure in under 10 minutes with few skipped items.
Table 2:
MIRC items dropped in pilot testing (n=497)
| Item and Subscale | Subscale α with item deleted | Correlation with subscale remaining total | Slope (SE) | Weighted kappa |
|---|---|---|---|---|
| Social Capital (α = .63) | ||||
| People using alcohol or drugs around me makes my recovery more difficult. | .67 | .12 | 0.28 (.11) | .56 |
| Physical Capital (α = .73) | ||||
| I have a steady job (full-time or part-time). | .73 | .19 | 0.81 (.14) | * |
| My legal problems cause me stress. | .73 | .18 | 0.50 (.13) | * |
| Having a criminal record is a barrier to my recovery. | .74 | .14 | 0.31 (.12) | * |
| Human Capital (α = .81) | ||||
| I have effective coping skills that I use in my recovery. | .80 | .41 | 1.03 (0.12) | .30 |
| I have a hopeful outlook on my recovery. | .81 | .39 | 0.92 (.12) | .56 |
| I feel mentally healthy most days. | .80 | .53 | 1.47 (.15) | .52 |
| I have problems with my physical health. | .80 | .64 | 1.33 (.14) | * |
| I have a spiritual practice that helps me in recovery. | .82 | .17 | 0.46 (.10) | .80 |
| I have a job that is meaningful to me. | .82 | .10 | 0.23 (.11) | * |
| There are activities I enjoy doing without using alcohol or drugs. | .82 | .19 | 0.55 (.10) | .20 |
| Cultural Capital (α = .67) | ||||
| I would have a lot to lose if my alcohol or drug problem came back. | .72 | .06 | 0.18 (.01) | .46 |
| I help out with what’s needed in my community. | .68 | .20 | 0.75 (.11) | .62 |
| Discrimination related to my race, gender, or sexual orientation is making my recovery harder. | .66 | .32 | 0.84 (.11) | .63 |
| Community Capital (α = .61) | ||||
| I feel like people judge me because of my past problems with alcohol or drugs. | .61 | .21 | 0.48 (.12) | .63 |
| There are not a lot of programs or services for people in recovery like me in my neighborhood or town. | .58 | .30 | 0.87 (.14) | .28 |
| It’s hard to avoid the alcohol and drug use in my neighborhood or town. | .55 | .37 | 1.01 (.17) | .37 |
Item included a “not applicable” response option making the weighted kappa inappropriate
3.2. Psychometric evaluation (Phase 3) results
After reviewing and cleaning the data, we conducted analyses of item performance, similar to the pilot testing phase. We cut four items that performed weakly: “Having money is a trigger for me to drink or use drugs” (physical capital); “I have trouble sleeping” (human capital); “I have work (paid or unpaid) that is meaningful to me” (human capital); and “I know of good examples of people in my community who are succeeding in their recovery” (cultural capital). The resulting final MIRC contained 28 items, split equally across four subscales (see Table 3). Table 4 summarizes the distribution, reliability (Cronbach’s alpha and ICC), and concurrent validity for the final MIRC and its four subscales. The full measure is available in Appendix 1.
Table 3:
Items performance for final MIRC (n=482)
| Item and subscale | Subscale α with item deleted | Correlation with subscale remaining total | Slope (SE) | Weighted kappa |
|---|---|---|---|---|
| Social Capital (α = .65) | ||||
| I actively support other people who are in recovery. | .67 | .12 | 0.37 (.13) | .28 |
| My family makes my recovery more difficult. | .56 | .47 | 1.58 (.20) | .52 |
| I have at least one friend who supports my recovery. | .61 | .38 | 1.22 (.18) | .56 |
| My family supports my recovery. | .57 | .52 | 2.33 (.37) | .37 |
| Some people in my life do not think I’ll make it in my recovery. | .65 | .25 | 0.73 (.13) | .65 |
| I feel alone. | .56 | .50 | 1.52 (.20) | .78 |
| I feel like I’m part of a recovery community. | .63 | .30 | 0.81 (.12) | .56 |
| Physical Capital (α = .81) | ||||
| My housing situation is helpful for my recovery. | .79 | .51 | 1.52 (.15) | .76 |
| I have difficulty getting transportation. | .79 | .52 | 1.67 (.11) | .74 |
| My housing situation is unstable. | .76 | .70 | 3.04 (.16) | .78 |
| I have enough money every week to buy the basic things I need. | .77 | .64 | 2.08 (.35) | .65 |
| Not having enough money makes my recovery more difficult. | .79 | .51 | 1.51 (.20) | .64 |
| I can afford the care I need for my health, mental health, and recovery. | .78 | .58 | 1.77 (.15) | .68 |
| I have reliable access to a phone and the internet. | .81 | .38 | 1.23 (.17) | .31 |
| Human Capital (α = .80) | ||||
| I find it hard to have fun. | .77 | .55 | 1.62 (.16) | .79 |
| I feel physically healthy most days. | .80 | .39 | 1.03 (.12) | .71 |
| I am struggling with guilt or shame. | .77 | .59 | 2.05 (.19) | .81 |
| I am experiencing a lot of stress. | .76 | .63 | 2.47 (.25) | .78 |
| My education and training have prepared me to handle life’s challenges. | .80 | .40 | 0.94 (.18) | .62 |
| I have problems with my mental health. | .76 | .63 | 2.30 (.22) | .77 |
| I feel my life has purpose and meaning. | .77 | .54 | 1.43 (.15) | .72 |
| Cultural Capital (α = .78) | ||||
| It’s hard for me to trust others. | .76 | .47 | 1.24 (.13) | .69 |
| I have opportunities to participate in fun activities that do not involve drugs and alcohol. | .75 | .50 | 1.22 (.14) | .63 |
| I feel disconnected from my culture or not part of any culture. | .73 | .60 | 2.55 (.24) | .74 |
| I feel like an outcast. | .71 | .68 | 3.80 (.49) | .75 |
| There are helpful services and resources accessible to me. | .77 | .40 | 1.04 (.13) | .72 |
| It’s hard to let go of the part of my identity that was linked to my drinking or drug use. | .76 | .48 | 1.35 (.14) | .65 |
| My neighborhood or town feels safe. | .78 | .37 | 0.86 (.12) | .68 |
Table 4:
Distribution, reliability, and validity of final MIRC and subscales (n=482)
| 10th percentile score | Median score | 90th percentile score | M (SD) | α | ICC | Concurrent validity correlation* | |
|---|---|---|---|---|---|---|---|
| Social Capital | 17 | 21 | 26 | 20.8 (3.5) | .65 | .72 | .41 |
| Physical Capital | 15 | 21 | 27 | 20.6 (4.5) | .81 | .87 | .74 |
| Human Capital | 11 | 17 | 23 | 17.6 (4.1) | .80 | .92 | .55 |
| Cultural Capital | 12 | 18 | 23 | 18.4 (3.8) | .78 | .85 | .42 |
| Total Measure | 55 | 77 | 95 | 77.4 (13.1) | .91 | .91 | .76 |
Social Capital: Brief 2-way Social Support Scale; Physical Capital: WHOQOL-BREF Domain 4; Human Capital: WHOQOL-BREF Domains 1, 2; Cultural Capital: Perceived Neighborhood Scale - Sense of Community Subscale; Total MIRC: WHOQOL-BREF total score
3.2.1. Distribution and reliability
Each of the four subscales has a potential range of 7–28. The range of scores across subscales was similar at the 10th percentile, median, and 90th percentile. Mean scores for human capital and cultural capital were somewhat lower than social and physical capital scores. Mean and median scores for the full measure were nearly equal, suggesting low skewness and indicating an average per-item response of 2.75. Internal consistency was moderate to strong for each subscale (α=.65 to .81; ICC=.72 to .92) and strong for the full measure (α=.91; ICC=.91).
3.2.2. Validity
To assess concurrent validity, subscale correlations were calculated between social capital and the Brief 2-way Social Support Scale (r=.41); physical capital and domain 4 of the WHOQOL-BREF (r=.74); human capital and domains 1 (r=.55) and 2 (r=.76) of the WHOQOL-BREF; cultural capital and the sense of community subscale of the Perceived Neighborhood Scale (r=.42); and the full MIRC and the full WHOQOL-BREW (r=.76). Results from a fitted confirmatory factor analysis showed similar results as those seen with the GRM-based analysis, based on the relative magnitudes of obtained factor loadings and factor score regression coefficients.
Lastly, Table 5 shows the correlation matrix for the MIRC subscales and total measure. Correlations between subscales showed moderate strength, ranging from physical and human capital (r=.50) at the weakest to human and cultural capital (r=.71) at the strongest. Most correlations were on the order of r=.55, while cultural-social (r=.63) and cultural-human (r=.71) were higher. Correlations between each subscale and the total measure showed a stronger relationship (r=.80-.87).
Table 5:
Correlation matrix for MIRC subscales and total measure (n=482)
| Social Capital | Physical Capital | Human Capital | Cultural Capital | Total Measure | |
|---|---|---|---|---|---|
| Social Capital | 1 | - | - | - | - |
| Physical Capital | .56 | 1 | - | - | - |
| Human Capital | .55 | .50 | 1 | - | - |
| Cultural Capital | .63 | .55 | .71 | 1 | - |
| Total Measure | .81 | .80 | .83 | .87 | 1 |
4. Discussion
In this study, we sought to develop a new measure of recovery capital that improved on existing measures through greater fidelity to the theoretical construct; incorporating qualitative and quantitative data from diverse samples with respect to race, class, gender, and recovery experience; and improving psychometric performance through GRM-based analyses. The items in the MIRC cover some of the same topics included in prior measures, such as the ARC (Groshkova et al., 2013); for example, both include items assessing social support for recovery. However, the MIRC is distinctive in its alignment with the theoretical domains of social, physical, human, and cultural capital, as specified by Cloud and Granfield (2008), and its systematic assessment of negative as well as positive capital. Our analyses indicate that the MIRC is feasible to self-administer and that the full measure and its subscales have acceptable reliability. Of note, the 10th percentile and especially 90th percentile scores for the subscales are somewhat near their range limits, indicating high variability, whereby some persons have little recovery capital and others have a high amount. This is clinically relevant and suggests sound performance with respect to item discrimination.
We also measured concurrent validity for each of the subscales (r=.41-.76) and the total measure (r=.76) comparing to other relevant, established measures. The comparative instruments assessed similar but not identical concepts and none were recovery-specific. Given this, the moderate strength of the correlations appropriately show some shared space, while maintaining conceptual distinction. For example, the sense of community subscale of the Perceived Neighborhood Scale assesses a neighborhood-based notion of community, whereas items on the cultural capital subscale of the MIRC measure broader notions of culture and community connected to recovery. Given this, the moderate correlation of r=.42 is reasonable, consistent with shared conceptual territory in the domain of community characteristics, but also differentiability between the two measures based on their conceptual distinctions. In sum, the internal consistency, test-retest reliability, and concurrent validity results all support the soundness of the measure.
In assessing theoretical model fit, we note that the face validity of items is strong, having been shaped through iterative feedback from research experts, service providers, and persons in recovery (Bowen et al., 2022). In addition, subscale and full measure correlations are consistent with a proper theoretical fit. We expected to see some, but not very high, correlation between each of the subscales given that we do not believe they are independent, but that they should differentiate. This is in fact what we discovered in the range of correlations (r=.50-.71). Further, we expected to see higher correlation between subscales and the overall measure because for any individual, any one given capital subscale may be an outlier, but overall recovery capital cannot be. This expectation was also observed in the data (r=.80-.87). In total, each subscale was substantially related to the others, though not to the degree that would call conceptual independence into question. Further, subscales were strongly but not identically related to the overall measure, suggesting that they each constitute but do not independently represent overall recovery capital.
We acknowledge some limitations regarding the MIRC and our measurement development process. First, samples across study phases were comprised of people in recovery from alcohol problems. Although many participants reported past problems with drugs other than alcohol and MIRC items do not refer specifically to alcohol, the validity of the measure for people whose recovery histories do not involve alcohol is not established. Another limitation is that although the study samples are diverse with regard to characteristics including race, ethnicity, gender, sexual orientation, and recovery experience, they are not perfectly representative, with some groups under or over-represented in different phases.
In addition, a limitation is that relative to the other subscales, the social capital subscale had weaker internal consistency and test-retest reliability (α=.65, ICC=.72). The measurement of social capital, by nature a relatively intangible dimension of social life, poses many challenges, especially when applied to understanding a person’s capacity for overcoming complex problems, such as substance use disorders (Erickson & Benton, 2019). In our study, the item that most reduced the social capital subscale alpha was “I support other people who are in recovery.” Despite subpar performance, we decided to retain the item based on the research literature establishing this concept as a key factor in recovery (Krieger et al., 2021; Pagano et al., 2013; Zemore & Kaskutas, 2004). We altered the item to read “actively support” on the hypothesis that active support involving personal engagement, rather than passive “well-wishing”-type support, would better discriminate and capture the construct. While this item captures a type of bonding social capital that could expand a person’s connection with others like themselves, not everyone who is in the process of recovering feels the need to bond with others in recovery, and some people may choose to deliberately withdraw (Granfield & Cloud, 1999).
Despite these limitations, the MIRC holds promise for future research. One potential use is to explore relationships between the four domains of recovery capital, an endeavor that was not possible with earlier measures that did not include social, physical, human, and cultural capital subscales. For example, future research could examine possible interactions between recovery capital domains and their effects on recovery outcomes. Broadly speaking, we see benefit in using the MIRC to understand if and how recovery capital is predictive of successful recovery outcomes based on the current NIAAA recovery definition, e.g., resolution of AUD symptoms, cessation of heavy drinking, and quality of life improvements (Hagman et al., 2022). In particular, the MIRC may be useful in understanding the role that recovery capital could play in mediating disparities in recovery outcomes for various groups (e.g. lower income people, people of color, and sexual and gender minorities) and elucidating if and how recovery capital varies for individuals on differing recovery pathways, such as those in natural recovery and those using treatment and mutual aid groups (Collins, 2016; Wagner & Baldwin, 2020). Further, it is our hope that the MIRC will also be used in practice, as a free tool for ongoing service planning and self-assessment (Neale & Bowen, 2022).
4. 1. Conclusion
In order to best support people in recovery, researchers and clinicians must have an understanding of how people view their recovery and the many factors that influence this complex process. Essential to this understanding is a high-quality recovery capital measurement tool that is resonant and accurate for those using it. The MIRC provides an improved way of quantitatively assessing recovery capital – one that is grounded in people’s lived experiences, psychometrically sound, and comprehensive across four domains and positive and negative dimensions of the construct (Cloud & Granfield, 2008). As holistic and nuanced definitions of recovery evolve (Hagman et al., 2022), greater specificity in measuring recovery capital may provide the foundation for conceptual and clinical advancements for people in recovery.
Supplementary Material
Acknowledgements
Research reported in this publication was supported by the U.S. National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health under Award Number R21AA028099 and T32AA007583 to the University at Buffalo. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors also acknowledge recruitment and other technical assistance from key partners including: the Buffalo Research Registry of the Clinical and Translational Science Institute, Bettina Hoeppner and the Recovery Research Institute, the African American Federation of Recovery Organizations, Melissa Miller and the Buffalo Center for Social Research, and the recovery research experts who reviewed our initial items. Finally, we acknowledge and thank participants for key input at each phase of the study.
Footnotes
CRediT authorship contribution statement
Elizabeth Bowen: led research and manuscript writing. Andrew Irish: assisted in research, analysis, and manuscript writing. Gregory Wilding: led analysis and assisted in manuscript writing. Charles LaBarre: assisted in research and manuscript writing. Nicole Capozziello: assisted in research and manuscript writing. Thomas Nochajski: assisted in research and analysis. Robert Granfield: assisted in research and manuscript writing. Lee Ann Kaskutas: in research and consulted on analysis. All authors assisted in preparing and approved the final manuscript.
Declaration of Competing Interest
The authors have no conflicts of interest to declare.
References
- Best D, & Hennessy EA (2022). The science of recovery capital: Where do we go from here? Addiction, 117(4), 1139–1145. 10.1111/add.15732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen E, Irish A, LaBarre C, Capozziello N, Nochajski T, & Granfield R (2022). Qualitative insights in item development for a comprehensive and inclusive measure of recovery capital. Addiction Research & Theory, 30(6), 403–413. 10.1080/16066359.2022.2055002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen EA, Scott CF, Irish A, & Nochajski TH (2020). Psychometric properties of the Assessment of Recovery Capital (ARC) instrument in a diverse low-income sample. Substance Use & Misuse, 55(1), 108–118. 10.1080/10826084.2019.1657148 [DOI] [PubMed] [Google Scholar]
- Burns J, & Marks D (2013). Can recovery capital predict addiction problem severity? Alcoholism Treatment Quarterly, 31(3), 303–320. 10.1080/07347324.2013.800430 [DOI] [Google Scholar]
- Cano I, Best D, Edwards M, & Lehman J (2017). Recovery capital pathways: Modelling the components of recovery wellbeing. Drug and Alcohol Dependence, 181, 11–19. 10.1016/j.drugalcdep.2017.09.002 [DOI] [PubMed] [Google Scholar]
- Cloud W, & Granfield R (2001). Natural recovery from substance dependency. Journal of Social Work Practice in the Addictions, 1(1), 83–104. 10.1300/J160v01n01_07 [DOI] [Google Scholar]
- Cloud W, & Granfield R (2008). Conceptualizing recovery capital: Expansion of a theoretical construct. Substance Use and Misuse, 43(12–13), 1971–1986. https://doi.org/10/1080/10826080802289762 [DOI] [PubMed] [Google Scholar]
- Cobanoglu C, Cavusoglu M, & Turktarhan G (2021). A beginner’s guide and best practices for using crowdsourcing platforms for survey research: The case of Amazon Mechanical Turk (MTurk). Journal of Global Business Insights, 6(1), 92–97. 10.5038/2640-6489.6.1.1177 [DOI] [Google Scholar]
- Erickson L, & Benton A (2019). Measuring social capital in human services programs. U.S. Department of Health and Human Services. https://aspe.hhs.gov/sites/default/files/private/pdf/262956/FINALSocialCapitalMeasurementBrief.pdf [Google Scholar]
- Granfield R, & Cloud W (1999). Coming clean: Overcoming addiction without treatment. NYU Press. [Google Scholar]
- Groshkova T, & Best D, & White W (2013). The assessment of recovery capital: Properties psychometrics of a measure of addiction recovery strengths. Drug and Alcohol Review, 32(2), 187–194. https://doi.org.10.1111/j.1465-3362.2012.00489.x [DOI] [PubMed] [Google Scholar]
- Hagman BT, Falk D, Litten R, & Koob GF (2022). Defining recovery from alcohol use disorder: Development of an NIAAA definition. The American Journal of Psychiatry . Advance online publication. 10.1176/appi.ajp.21090963 [DOI] [PubMed] [Google Scholar]
- Hanauer M, Sielbeck-Mathes K, & Berny L (2019). Invariance of a recovery capital scale across gender, ethnicity, and sexual orientation in a substance use disorder treatment program. The American Journal of Drug and Alcohol Abuse, 45(3), 254–263. 10.1080/00952990.2018.1558228 [DOI] [PubMed] [Google Scholar]
- Hennessy EA (2017). Recovery capital: A systematic review of the literature. Addiction Research & Theory, 25(5), 349–360. 10.1080/16066359.2017.1297990 [DOI] [Google Scholar]
- Hennessy EA, Cristello JV, & Kelly JF (2019). RCAM: A proposed model of recovery capital for adolescents. Addiction Research & Theory, 27(5), 429–436. 10.1080/16066359.2018.1540694 [DOI] [Google Scholar]
- Kaskutas LA, Borkman TJ, Laudet A, Ritter LA, Witbrodt J, Subbaraman MS, Stunz A, & Bond J (2014). Elements that define recovery: The experiential perspective. Journal of Studies on Alcohol and Drugs, 75(6), 999–1010. 10.15288/jsad.2014.75.999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, & Hoeppner B (2015). A biaxial formulation of the recovery construct. Addiction Research & Theory, 23(1), 5–9. 10.3109/16066359.2014.930132 [DOI] [Google Scholar]
- Kim HS, & Hodgins DC (2017). Reliability and validity of data obtained from alcohol, cannabis, and gambling populations on Amazon mechanical turk. Psychology of Addictive Behaviors, 31(1), 85–94. 10.1037/adb0000219 [DOI] [PubMed] [Google Scholar]
- Krieger MA, Balint S, & LaBelle O (2021). Predictors of physical and mental health in recovery: The role of state and trait gratitude, social contact, and helping others. International Journal of Mental Health and Addiction . 10.1007/s11469-021-00644-6 [DOI] [Google Scholar]
- LaBarre C, Linn BK, Bradizza CM, Bowen EA, & Stasiewicz PR (2021). Conceptualizing recovery capital for older adults with substance use disorders. Journal of Social Work Practice in the Addictions, 21(4), 417–427. 10.1080/1533256X.2021.1973827 [DOI] [Google Scholar]
- Laudet AB (2007). What does recovery mean to you? Lessons from the recovery experience for research and practice. Journal of Substance Abuse Treatment, 33(3), 243–256. 10.1016/j.jsat.2007.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y, Ho FN, & Wu MC (2018). How do form and functional newness affect adoption preference? The moderating role of consumer need for uniqueness. Journal of Consumer Marketing, 35(1), 79–90. 10.1108/JCM-10-2015-1578 [DOI] [Google Scholar]
- Lyons T, & Lurigio AJ (2010). The role of recovery capital in the community reentry of prisoners with substance use disorders. Journal of Offender Rehabilitation, 49(7), 445–455. 10.1080/10509674.2010.510769 [DOI] [Google Scholar]
- Martinez ML, Black M, & Starr RH (2002). Factorial structure of the perceived neighborhood scale (PNS): A test of longitudinal invariance. Journal of Community Psychology, 30(1), 23–43. 10.1002/jcop.1048 [DOI] [Google Scholar]
- Morse DT, & Robertson AA (2017). Psychometric properties of the Short Inventory of Problems (SIP) with adjudicated DUI intervention participants. Psychology of Addictive Behaviors, 31(1), 110–116. 10.1037/adb0000249 [DOI] [PubMed] [Google Scholar]
- Neale J, & Bowen AM (2022). Lessons for uptake and engagement of a smartphone app (SURE recovery) for people in recovery from alcohol and other drug problems: Interview study of app users. JMIR Human Factors, 9(1), 33038. 10.2196/33038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obst P, Shakespeare-Finch J, Krosch DJ, & Rogers EJ (2019). Reliability and validity of the Brief 2-Way Social Support Scale: An investigation of social support in promoting older adult well-being. SAGE Open Medicine, 7, 1–10. 10.1177/2050312119836020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagano ME, White WL, Kelly JF, Stout RL, & Tonigan JS (2013). The 10 year course of Alcoholics Anonymous participation and long-term outcomes: A follow-up study of outpatient subjects in project MATCH. Substance Abuse, 34(1), 51–59. 10.1080/08897077.2012.691450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palombi L, Hawthorne AN, Irish A, Becher E, & Bowen E (2019). “One out of ten ain’t going to make it”: An analysis of recovery capital in the rural upper Midwest. Journal of Drug Issues, 49(4), 680–702. 10.1177/0022042619859309 [DOI] [Google Scholar]
- Simms LJ, Zelazny K, Williams TF, & Bernstein L (2019). Does the number of response options matter? Psychometric perspectives using personality questionnaire data. Psychological Assessment, 31(4), 557–566. 10.1037/pas0000648 [DOI] [PubMed] [Google Scholar]
- Skevington SM, Lotfy M, & O’Connell KA (2004). The World health organization’s WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial: A report from the WHOQOL Group. Quality of Life Research, 13(2), 299–310. 10.1023/B:QURE.0000018486.91360.00 [DOI] [PubMed] [Google Scholar]
- Sterling R, Slusher C, & Weinstein S (2008). Measuring recovery capital and determining its relationship to outcome in an alcohol dependent sample. The American Journal of Drug and Alcohol Abuse, 34(5), 603–610. 10.1080/00952990802308114 [DOI] [PubMed] [Google Scholar]
- Strickland JC, & Stoops WW (2019). The use of crowdsourcing in addiction science research: Amazon Mechanical Turk. Experimental and Clinical Psychopharmacology, 27(1), 1–18. 10.1037/pha0000235 [DOI] [PubMed] [Google Scholar]
- Strickland JC, Hill JC, Stoops WW, & Rush CR (2019). Feasibility, acceptability, and initial efficacy of delivering alcohol use cognitive interventions via crowdsourcing. Alcoholism: Clinical and Experimental Research, 43(5), 888–899. 10.1111/acer.13987 [DOI] [PubMed] [Google Scholar]
- Tucker JA, Chandler SD, & Witkiewitz K (2020). Epidemiology of recovery from alcohol use disorder. Alcohol Research: Current Reviews, 40(3), 01. 10.35946/arcr.v40.3.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vilsaint CL, Kelly JF, Bergman BG, Groshkova T, Best D, & White W (2017). Development and validation of a brief assessment of recovery capital (BARC-10) for alcohol and drug use disorder. Drug and Alcohol Dependence, 177, 71–76. 10.1016/j.drugalcdep.2017.03.022 [DOI] [PubMed] [Google Scholar]
- Willson S, & Miller K (2014). Data collection. In Miller K, Willson S, Chepp V, and Padilla J-L (Eds.), Cognitive interviewing methodology: A sociological approach for survey question evaluation . John Wiley & Sons. [Google Scholar]
- Witkiewitz K, Montes KS, Schwebel FJ, & Tucker JA (2020). What is recovery? Alcohol Research: Current Reviews, 40(3). 10.35946/arcr.v40.3.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore SE, & Kaskutas LA (2004). Helping, spirituality, and Alcoholics Anonymous in recovery. Journal of Studies on Alcohol, 65(3), 383–391. 10.15288/jsa.2004.65.383 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


