Abstract
Background
To evaluate the feasibility and safety of the superficial circumflex iliac perforator flap (SCIP) for maxillary reconstruction with intraoral anastomosis, pedicle elongation, and super-microsurgery techniques to overcome its anatomical shortcomings due to the attractive merits of the flap.
Methods
Patients who underwent reconstruction of maxillary defects with SCIPs from July 2020 to December 2022 were included. Intraoral anastomosis, pedicle elongation, and super-microsurgery were performed during surgery with or without a neck incision. The sizes, pedicle lengths, inner calibres of vessels, complications and flap survival statuses were recorded.
Results
A total of 12 patients were included, with 3 males and 9 females, and the median age was 45 years, ranging from 14 to 74 years. There were 5 class IIa and 7 class IIb defects, 6 cases underwent maxillary defect reconstruction via SCIPs with intraoral anastomosis, and the other 6 cases with distally design and/or de-epidermis pedicle elongation. Super-microsurgery interventions were needed in 5 patients. The size ranged from 3 cm×4 cm to 6 cm×8 cm. The pedicle length ranged from 4 cm to 12 cm, with a median of 6 cm. The inner caliber of the arteries ranged from 0.7 mm to 2 mm, with a median of 1 mm, and the veins ranged from 1.5 mm to 4 mm, with a median of 2.5 mm. All the flaps survived, and no donor site complications occurred.
Conclusion
Superficial circumflex iliac perforator flaps can be regarded as feasible and safe choices for maxillary defects with the support of intraoral anastomosis, pedicle elongation and super-microsurgery.
Keywords: Iliac artery, Rehabilitation, Surgical anastomosis, Free tissue flaps, Microsurgery
Introduction
Defects in the region of the maxilla are regarded as the most complex and controversial problem in head and neck reconstructive surgery for not only primary disease control but also the result of rehabilitation [1]. The main difficulties are the need for aesthetics of the middle face, the function of swallowing and speech, and the frame completeness of hard tissue [2].
Multiple options exist for different classes, including obturation, nonvascular bone graft, local tissue flaps, or microvascular free flap transfer [1, 3, 4]. All these modalities are suitable for various types of defects with different advantages; however, for relatively larger defects, such as defects after tumor resection, microvascular-free flaps are used [1, 5]. In free flaps for class II defects, the radial forearm is the most commonly used choice [1], and the fibula is the first choice when the bone is needed [6]. These choices, including the anterolateral thigh flap, are associated with donor site morbidities such as functional impairment and a large scar and are unsuitable for the development of aesthetic and functional reserves [2, 7].
The superficial circumflex iliac perforator flap (SCIP), which evolved from the groin flap, can meet the previous demand [8]. SCIP is regarded as a versatile option to cover soft tissue defects because of its advantages of a suitable texture, easily adjustable volume, long-term volume retention, chimeric options [9], maximum donor site concealment, and minimal donor site morbidity [10]. Since its introduction in 2004 [7], SCIP has been widely used mostly for extremity, tongue and oral base reconstruction [8, 10, 11]. However, limitations have also been reported, such as short pedicles with a small caliber and wide variations in vascular anatomy [8, 10, 12], which are believed to restrict the use of SCIP in the reconstruction of the maxilla because of the relatively long distance between the maxilla and neck and the associated technical difficulty [13].
However, with the development of the intraoral anastomosis technique [14, 15], the pedicle elongation technique [16, 17], and the super-microsurgery technique [18], the application range of SCIP has increased widely, making SCIP for maxillary reconstruction possible. Therefore, in this study, which was supported by advanced techniques, we attempted to evaluate the feasibility and safety of SCIPs for maxillary reconstruction.
Patients and methods
Patients
Under the guidance of the Ethics Committee of Peking University School and Hospital of Stomatology (IRB number: PKUSSIRB-202167124), patients who underwent reconstruction of the maxilla via an SCIP flap or a chimeric SCIP flap with iliac bone from July 2020 to December 2022 at the Peking University School of Stomatology were included in this study. Informed consent was obtained and well documented. Patients who previously received radiation therapy in the head and neck region were excluded. Patients’ basic information, including age, sex, pathology results, and previous treatment history, was collected.
Surgical procedure
The donor site was evaluated through clinical examination, CT angiography, and/or Doppler ultrasound. All procedures were performed under general anesthesia with two teams for the tumor and flap simultaneously. The tumors were resected as usual, with the facial artery in the neck being carefully reserved and the intraoral part being prepared before the flap was raised if neck dissection and intraoral anastomosis were needed. The defect site and Brown classification [1] were recorded.
The locations of the femoral artery and iliac crest were identified during surgery by palpation. Then the flaps were designed according to pedicle elongation techniques, including distal flap design and de-epidermis technique (Figs. 1 and 2), for insufficient pedicle length [16]. Then, the flaps were raised by first detecting and dissecting the perforators through an incision made between the anterior superior iliac spine (ASIS) and the inguinal ligament on the supra-Scarpa fascial plane and then extending to the femoral artery. The superficial vein was found and dissected in the adipose tissue layer according to CT angiography [17]. The flaps were trimmed to remove the unnecessary skin peddle for a longer movable pedicle (Fig. 2) to meet the need for anastomosis in the neck. If the bone was needed, the SCIA-based iliac bone flap perfused by both the superficial and deep branches of the SCIA [9] was raised, and the bone was fixed with a miniplate or only screws (Fig. 1).
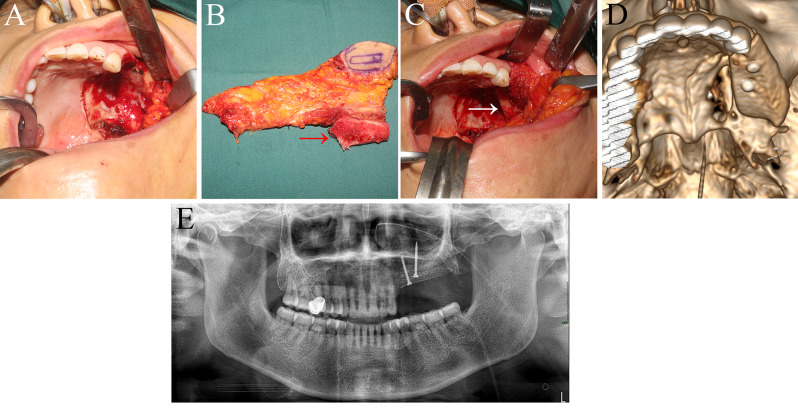
Fig. 1.
Surgical procedure and postoperative imaging of Patient No. 11, in which a chimeric SCIP flap with the iliac bone was used. (A) Class IIb defect of the maxilla. (B) Chimeric SCIP flap with the iliac bone pointed with a red arrow. (C) Placement of the flap with the iliac bone pointed with a white arrow. (D) Three-dimensional reconstruction of postoperative CT. (E) Postoperative panoramic image
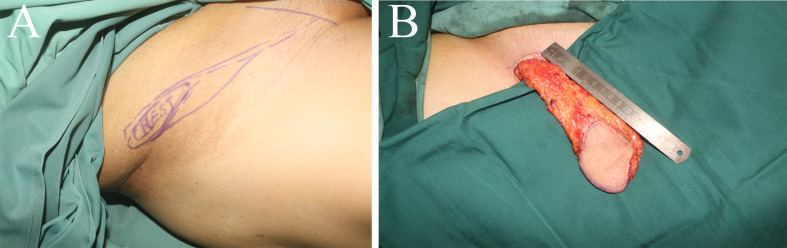
Fig. 2.
Design and surgical outcome of the distal flap design and de-epidermis technique for the SCIP flap. (A) The locations of the femoral artery and iliac crest were identified during surgery via palpation. (B) The available pedicle length could reach 10 cm with the help of the pedicle elongation technique
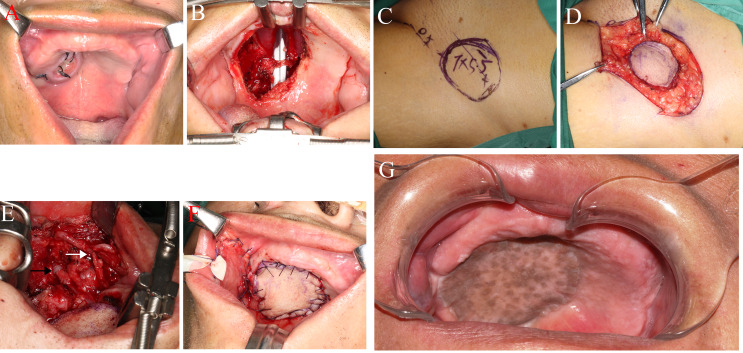
The flap arteries were anastomosed based on the pedicel length, neck management, and patient willingness. For the artery, intraoral anastomosis with the trunk of a facial artery or branch such as a superior labial artery (Fig. 3) or a traditional neck incision with the branch of an external carotid artery such as the superior thyroid artery was used. On the vein, the flap veins were correspondingly anastomosed with accompanying veins via the intraoral anastomosis technique or the branches of the internal jugular vein through a neck incision. The size, operative time, pedicel length, and vessel inner caliber of the flap were recorded.
Fig. 3.
Surgical procedure and postoperative imaging of Patient No. 3, in which a simple SCIP flap with intraoral anastomosis was used. (A) Tumor; (B) Class IIa defect of the maxilla; (C) Design of the SCIP flap; (D) Harvest of the SCIP flap; (E) Intraoral anastomosis of this case with a white arrow and a black arrow pointing at the anastomosis area of the artery and vein, respectively; (F) End of the surgery. (G) Three months after surgery
Follow-up
Complications, such as systematic and surgical area complications such as infection, dehiscence, and fistula at either the donor or recipient site, were recorded during the follow-up.
Results
A total of 12 patients who underwent reconstruction of the maxilla via an SCIP flap or a chimeric SCIP flap with an iliac bone at Peking University School of Stomatology from June 2020 to December 2022 were included. Among these, there were 3 males and 9 females, with a median age of 45 years ranging from 14 to 74 years. None of the patients were treated previously. Ten cases originated from the palatal area, and the other 2 originated from the upper gingiva. The primary causes were squamous cell carcinoma in 2 patients, adenoid cystic carcinoma in 2 patients, mucoepidermoid carcinoma in 6 patients, pleomorphic adenoma in 1 patient, and postoperative palate fistula in 1 patient. According to the Brown classification, the defects and flap types are listed in Table 1.
Table 1.
Information on the flaps
| No. | Flap Type | Defect Site | Defect Type | Size | Pedicle Length | Recipient Artery | Recipient Vein |
|---|---|---|---|---|---|---|---|
| 1 | Left SCIP* | Left maxilla | IIb | 5 cm×8 cm | 10 cm | Facial | Branch of the internal jugular |
| 2 | Left SCIP | Middle palatal | IIa | 4 cm×6 cm | 6 cm | Superior labial | Superior labial |
| 3 | Left SCIP | Left palatal | IIa | 6 cm×8 cm | 6 cm | Facial | Facial |
| 4 | Left SCIP | Left maxilla | IIb | 3 cm×6 cm | 4 cm | Superior labial | Superior labial |
| 5 | Right SCIP | Left palatal | IIa | 3.5 cm×4.5 cm | 4 cm | Superior labial | Superior labial |
| 6 | Left SCIP | Right maxilla | IIb | 5 cm×7 cm | 6 cm | Facial | Facial |
| 7 | Left SCIP | Right maxilla | IIb | 4.5 cm×5 cm | 6 cm | Facial | Facial |
| 8 | Left SCIP | Right maxilla | IIb | 4 cm×6 cm | 5 cm | Superior labial | Superior labial |
| 9 | Right chimeric SCIP with iliac bone | Right maxilla | IIb | 5 cm×6 cm for skin peddle and 1.5 cm×4 cm for bone | 8 cm | Superior thyroid | Branches of the internal jugular |
| 10 | Left SCIP | Right palatal | IIa | 3 cm×4 cm | 8 cm | Superior thyroid | Branch of the internal jugular |
| 11 | Left chimeric SCIP with iliac bone | Left maxilla | IIb | 4.5 cm×6 cm for skin peddle and 1.5 cm×4 cm for bone | 12 cm | Facial | Branch of the internal jugular |
| 12 | Left SCIP | Right palatal | IIa | 3 cm×4.5 cm | 8 cm | Superior thyroid | Branch of the internal jugular |
*SCIP is short for superficial circumflex iliac perforator flap
All 12 flaps were harvested successfully. The flap sizes, recipient vessels and pedicle lengths are listed in Table 1. The inner caliber of the arteries ranged from 0.7 mm to 2 mm, with a median of 1 mm, and the veins ranged from 1.5 mm to 4 mm, with a median of 2.5 mm. The flap harvesting and donor site closure times were 60 to 180 min, with a median of 85 min. The total operation time was 180 to 450 min, with a median of 250 min. Intraoral anastomosis and super-microsurgery technique were employed in 6 patients without a neck incision, and pedicle elongation and super-microsurgery technique were applied in 6 patients because of the need for a neck approach. All the flaps survived without any systematic or surgical complications. All patients were satisfied with the outcome of function and aesthetic restoration.
Discussion
Defects in the maxilla require rehabilitation for a series of functions, which makes the maxilla the most complicated area in head and neck reconstructive surgery [1, 2]. Free flaps, including the radial forearm, anterolateral thigh, and fibula flaps, remain the main choices for satisfactory outcomes for function and aesthetics [10]. However, morbidity from donor sites of these flaps still affects patients’ postoperative quality of life and urges clinicians to search for the optimal flap [7]. The superficial circumflex iliac perforator flap (SCIP) is best but is limited by vascular conditions for maxillary defects. With developing intraoral anastomosis, pedicle elongation, and super-microsurgery, SCIP seems feasible for maxillary reconstruction. Therefore, this study evaluated the feasibility and safety of SCIP for maxillary defects.
The advantages of SCIP are quite attractive. The remaining scar is inconspicuous and can be covered by underwear [16], meeting more patients’ desires than anterolateral thigh flaps do for scar concealment, and can satisfy the development requirements of higher postoperative quality of life. The thickness is easily adjustable by harvesting the superficial branch alone to obtain a thin flap or harvesting both the superficial and deep branches for a thicker and broader flap [19]. The sacrifice of tissue and function is minimal after modification of the groin flap, as there is no need for muscle and nerve dissection, which also results in minimal morbidity, such as lymph leakage [10, 17]. The surgery can be performed with two teams simultaneously, and a shorter operative time has been proven [10]. Moreover, the SCIP can also be harvested accompanied by an iliac bone supplied by the superficial circumflex iliac artery [9, 20]. All the advantages described above seem to lead SCIP to use a workhorse flap instead of the forearm, anterolateral thigh, or fibula flaps for maxillary defect reconstruction, but the present condition is the opposite because of the anatomic-based shortcomings of SCIP described below.
The study of anatomical stability in cadavers of the SCIP revealed that the perforator was always found while the length and caliber of the perforator varied [19, 21]. In addition, the mean outer caliber of the perforator in cadavers does not exceed 2 mm, and the available pedicle length is approximately 4 cm [19]. The results implied that simple SCIP might not be suitable for maxillary defects, as the path to the neck vessels is much longer, not to mention the small caliber. In this study, the inner caliber of the artery in 5 patients was less than 0.8 mm, necessitating intervention via the super-microsurgical technique [22]. The lengths of the 6 cases were less than 6 cm, as they were harvested and were regarded as a failure for maxillary defects with traditional approaches.
An angiography study revealed that the deep branch provided a longer pedicle than the superficial branch, and a relevant technique was used to lengthen the pedicle [17, 21]. In addition, using deep and transverse branches for reverse-flow elongation or enhancement can help the pedicle reach even 12 cm [16]. The third choice for pedicle elongation is the distal flap design and de-epidermis technique, which can help the pedicle reach 10 cm [20, 23] and offer soft tissue to fill the defect after neck dissection. Considering all the above, 6 patients in this study with neck incisions benefited from the third pedicle elongation technique.
Another technique used to overcome the shortcomings of SCIP is the intraoral anastomosis technique. Since Gaggl first introduced the intraoral anastomosis technique in 2009 [14], it has been well accepted and developed by many clinicians for its advantages, such as scarless incisions, solutions for short pedicles, and protection of the facial nerve [14, 15, 24, 25]. Therefore, the intraoral anastomosis technique is the “perfect partner” for SCIP with the same aesthetic theory and complementary characteristics. In addition, the variation of the perforators sometimes makes dissection technically demanding and pedicle elongation impossible. Even with comprehensive evaluation, such as CTA and Doppler mapping, in some situations, the pedicle length might be as low as 6 cm [13] or even 4 cm in this cohort, which is relatively insufficient for anastomosis in the neck region. In this study, if there was no neck incision intended for tumor cure or unable to achieve sufficient pedicle length, patients could benefit from the intraoral anastomosis technique, with 6 flaps surviving.
The limitations of this study mainly include the lack of comparisons, the prospective design, the objective evaluation of function and aesthetics, and the solution for technique sensitivity. The former three, due to clinical difficulty, are expected to be solved in future research, but the latter might need to wait until the mature form of the surgical robot system [26], which can overcome the visual depth in the head and neck, appears.
Patients suffering from maxillary defects with or without the need for bony rehabilitation were proven to safely benefit from the advantages of SCIP via intraoral anastomosis, pedicle elongation, and super-microsurgery techniques by an experienced surgical team.
Acknowledgements
None.
Author contributions
WW collected and analyzed the data, and drafted the manuscript. ZJ and RCWW critically revised the manuscript. LXM, ZYW and SY collected and analyzed the data, and critically revised the manuscript. ZL conceptualized and designed the study, performed statistical analysis, participated in the data collection, and critically revised the manuscript. And all authors have read and approved the final manuscript.
Funding
This study was supported by the Project of National Clinical Key Department Construction of Peking University School and Hospital of Stomatology (PKUSSNKP-202120) and the Program for New Clinical Techniques and Therapies of Peking University School and Hospital of Stomatology (PKUSSNCT-22A13).
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethical approval
This study was approved by the Ethics Committee of Peking University School and Hospital of Stomatology (IRB number: PKUSSIRB-202167124).
Consent for publication
Consent for publication was obtained from the included patients.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Brown JS, Shaw RJ. Reconstruction of the maxilla and midface: introducing a new classification. Lancet Oncol. 2010;11(10):1001–8. [DOI] [PubMed] [Google Scholar]
- 2.Lenox ND, Kim DD. Maxillary reconstruction. Oral Maxillofac Surg Clin North Am. 2013;25(2):215–22. [DOI] [PubMed] [Google Scholar]
- 3.Aldelaimi TN, Khalil AA. Maxillary Sinus Augmentation J Craniofac Surg. 2016;27(6):e557–9. [DOI] [PubMed] [Google Scholar]
- 4.Aldelaimi TN, Khalil AA. Reconstruction of Facial defect using Deltopectoral Flap. J Craniofac Surg. 2015;26(8):e786–8. [DOI] [PubMed] [Google Scholar]
- 5.Aldelaimi AA, et al. Tumors of Craniofacial Region in Iraq (Clinicopathological Study). J Res Med Dent Sci. 2021;9(1):66–71. [Google Scholar]
- 6.Chang YM, et al. Maxillary reconstruction with a fibula osteoseptocutaneous free flap and simultaneous insertion of osseointegrated dental implants. Plast Reconstr Surg. 2004;113(4):1140–5. [DOI] [PubMed] [Google Scholar]
- 7.Ma C, et al. Superficial circumflex iliac artery perforator flap for tongue reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;121(4):373–80. [DOI] [PubMed] [Google Scholar]
- 8.Hong JP. The superficial Circumflex Iliac Artery Perforator Flap in Lower Extremity Reconstruction. Clin Plast Surg. 2021;48(2):225–33. [DOI] [PubMed] [Google Scholar]
- 9.Sakata Y, Nishioka T, Asamura S. Application of free iliac bone flap based on superficial Circumflex Iliac Perforators in Mandibular Reconstruction. J Craniofac Surg. 2022;33(3):e253–5. [DOI] [PubMed] [Google Scholar]
- 10.Papanikolas MJ, et al. Anterolateral thigh, radial forearm and superficial circumflex iliac perforator flaps in oral reconstruction: a comparative analysis. ANZ J Surg; 2023. [DOI] [PubMed]
- 11.Green R, et al. The superficial circumflex iliac artery perforator flap in intra-oral reconstruction. J Plast Reconstr Aesthet Surg. 2013;66(12):1683–7. [DOI] [PubMed] [Google Scholar]
- 12.Goh TLH, et al. The search for the ideal thin skin flap: superficial circumflex iliac artery perforator flap–a review of 210 cases. Plast Reconstr Surg. 2015;135(2):592–601. [DOI] [PubMed] [Google Scholar]
- 13.Scaglioni MF, et al. Head and neck reconstruction with the superficial circumflex iliac artery perforator (SCIP) free flap: lessons learned after 73 cases. Head Neck. 2024;46(6):1428–38. [DOI] [PubMed] [Google Scholar]
- 14.Gaggl A, et al. An intraoral anastomosing technique for microvascular bone flaps in alveolar ridge reconstruction: first clinical results. Int J Oral Maxillofac Surg. 2009;38(9):921–7. [DOI] [PubMed] [Google Scholar]
- 15.Zheng L, et al. Intraoral anastomosis of a vascularized iliac-crest flap in maxillofacial reconstruction. J Plast Reconstr Aesthet Surg. 2019;72(5):744–50. [DOI] [PubMed] [Google Scholar]
- 16.Yoshimatsu H, Yamamoto T, Iida T. Pedicle elongation technique of superficial circumflex iliac artery perforator flap. J Plast Reconstr Aesthet Surg. 2015;68(3):e61–2. [DOI] [PubMed] [Google Scholar]
- 17.Fernandez-Garrido M, et al. The extended SCIP flap: an anatomical and clinical study of a new SCIP flap design. J Plast Reconstr Aesthet Surg. 2022;75(9):3217–25. [DOI] [PubMed] [Google Scholar]
- 18.Koshima I, et al. Perforator flaps and supermicrosurgery. Clin Plast Surg. 2010;37(4):683–9. vii-iii. [DOI] [PubMed] [Google Scholar]
- 19.Zubler C, et al. The anatomical reliability of the superficial circumflex iliac artery perforator (SCIP) flap. Ann Anat. 2021;234:151624. [DOI] [PubMed] [Google Scholar]
- 20.Yoshimatsu H, et al. Superficial Circumflex Iliac artery-based iliac bone flap transfer for Reconstruction of Bony defects. J Reconstr Microsurg. 2018;34(9):719–28. [DOI] [PubMed] [Google Scholar]
- 21.Gandolfi S, et al. Vascularization of the superficial circumflex iliac perforator flap (SCIP flap): an anatomical study. Surg Radiol Anat. 2020;42(4):473–81. [DOI] [PubMed] [Google Scholar]
- 22.Masia J, et al. Barcelona consensus on supermicrosurgery. J Reconstr Microsurg. 2014;30(1):53–8. [DOI] [PubMed] [Google Scholar]
- 23.Chao WN, et al. Freestyle groin flaps: the real axial flap design and clinical application. Ann Plast Surg. 2015;74(Suppl 2):S75–9. [DOI] [PubMed] [Google Scholar]
- 24.Jie B, et al. New series of surgical design for anterior maxillary reconstruction with deep circumflex iliac artery flap. Head Neck. 2020;42(11):3438–45. [DOI] [PubMed] [Google Scholar]
- 25.Zhang G, Zhu H, Zheng L. Management of Palatal Fistula using superficial Circumflex Iliac Artery Perforator Flap with Intraoral Anastomosis and Supermicrosurgery techniques. J Craniofac Surg. 2022;33(5):e474–6. [DOI] [PubMed] [Google Scholar]
- 26.Barbon C, et al. Exploring the learning curve of a new robotic microsurgical system for microsurgery. JPRAS Open. 2022;34:126–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.