Abstract
Background
Type 2 diabetes (T2D) is a chronic metabolic disorder that has a notable influence on mental well-being, contributing to elevated morbidity and mortality rates. Depression and anxiety disorders are the most common mental health concerns among patients with T2D worldwide. Therefore, the present study aimed to assess the impact of an online intensive lifestyle intervention (ILI) on mental health outcomes (depression and anxiety) in patients with T2D in India.
Materials and methods
This retrospective pre-post analysis included adult patients (aged > 18 years) diagnosed with T2D who were enrolled in a diabetes management program in India between June 2021 and June 2023. The intervention consisted of lifestyle modifications such as a customized plant-based diet, regular physical activity, psychological support through group and individual therapy, and medical management. Data were extracted from the electronic database of the clinic, including anthropometry, medical history, biochemical parameters, symptoms of depression, and anxiety (assessed using the Patient Health Questionnaire-9 (PHQ-9) and Generalized Anxiety Disorders-7 (GAD-7) scale) at the start and end of the six-month intervention period.
Results
Of the 1061 eligible patients (177 with prediabetes), 40.3% were female. The mean age, duration of diabetes, and HbA1c levels were 52 ± 10.4 years, 9.8 ± 7.8 years, and 8 ± 1.7%, respectively. The prevalence of symptoms of depression and anxiety (ranging from mild to severe) was 46% and 44.3%, respectively, which reduced to 28.7% and 29.2%, respectively, post-intervention.
Conclusion
Integrated ILI successfully improved the symptoms of anxiety and depression, highlighting the importance of a multidisciplinary approach that includes diet, physical activity, psychological support, and medical management in enhancing mental health outcomes among patients with T2D. Future prospective studies are needed to explore the long-term effects of such interventions and develop effective strategies for promoting mental health in diverse populations.
Trial registration
The study was approved by the Freedom from Diabetes Research Foundation Institutional Ethics Committee (approval number FFDRF/IEC/2024/7) and registered in the Clinical Trials Registry of India (CTRI/2024/03/064596, registered on March 21, 2024).
Keywords: Anxiety, Depression, Type 2 diabetes, Mental health, Intensive lifestyle intervention, India
Background
Mental well-being is crucial for managing various health conditions, including Type 2 diabetes (T2D) [1, 2]. T2D is a chronic metabolic disorder that affects millions of people worldwide and is associated with increased morbidity and mortality [3]. It affects not only the physical health of individuals but also their mental health, as patients often experience psychological distress, anxiety, and depression [4]. These mental health issues can impair the quality of life, self-care behaviors, and glycemic control of patients [5].
Depression and anxiety disorders are the most prevalent forms of psychological distress among T2D patients globally [6]. Further, there is a documented reciprocal relationship between T2D and depression, indicating that diabetes can contribute to depression and vice versa [7, 8]. According to the American Diabetes Association (ADA), psychological conditions can appear in people with diabetes of all ages [4]; therefore, a comprehensive medical evaluation of patients with diabetes should include an assessment of psychosocial/emotional health concerns if indicated [9, 10].
A systematic review indicated that, on a global scale, approximately 28% of individuals with T2D experience depression and 14% have anxiety disorders associated with hyperglycemia [11]. In patients with diabetes, anxiety and depression have been linked to higher medical care expenses, interference with daily life routines, poorer quality of life [12], and an increased risk of complications [13]. Effective diabetes management relies on self-care and adherence to prescribed treatment to avoid complications. Psychological distress, particularly depression and anxiety, hinders self-care routines and compliance with treatment protocols [14, 15], which may worsen the prognosis of diabetes [16]. Therefore, the importance of addressing psychological distress in individuals with diabetes cannot be overstated, as it not only affects their ability to manage their condition but can also have negative consequences on their overall health and well-being. Considering the high burden of mental health conditions in patients with T2D, there is an urgent need to implement effective interventions and treatments that can improve their mental well-being.
Several interventions have been proposed to address the psychological needs of T2D patients, such as pharmacological treatment, cognitive behavioral therapy, collaborative care, and health education [17–20]. However, these interventions may have limitations, such as side effects, cost, accessibility, and adherence [21]. Additionally, there is a scarcity of research examining the effectiveness of a multidisciplinary approach for managing mental health issues in patients with T2D, especially considering the complex and reciprocal relationship between T2D and mental health outcomes. Lifestyle changes such as modifications to diet and exercise are crucial for managing T2D, but their comprehensive impact on both T2D management and mental health remains underexplored [22]. Therefore, this study aimed to retrospectively assess the impact of an integrated intensive lifestyle intervention (ILI) (including diet, exercise, psychological support, and medical support) in alleviating symptoms of anxiety and depression in individuals with T2D.
Methods
Study design and setting
This retrospective study was carried out at the Freedom from Diabetes Clinic, which operates on a one-year subscription-based program for the online management of diabetes. The eligibility criteria included participants aged > 18 years with a confirmed diagnosis of T2D (all patients on treatment with oral hypoglycemic agents and/or Insulin or with HbA1c ≥ 6.5% without medication) or prediabetes (HbA1c between 5.7 and 6.5%) [23]. Patients with a history of medically diagnosed psychiatric illness (verified with medical records) and pregnant and lactating women were excluded.
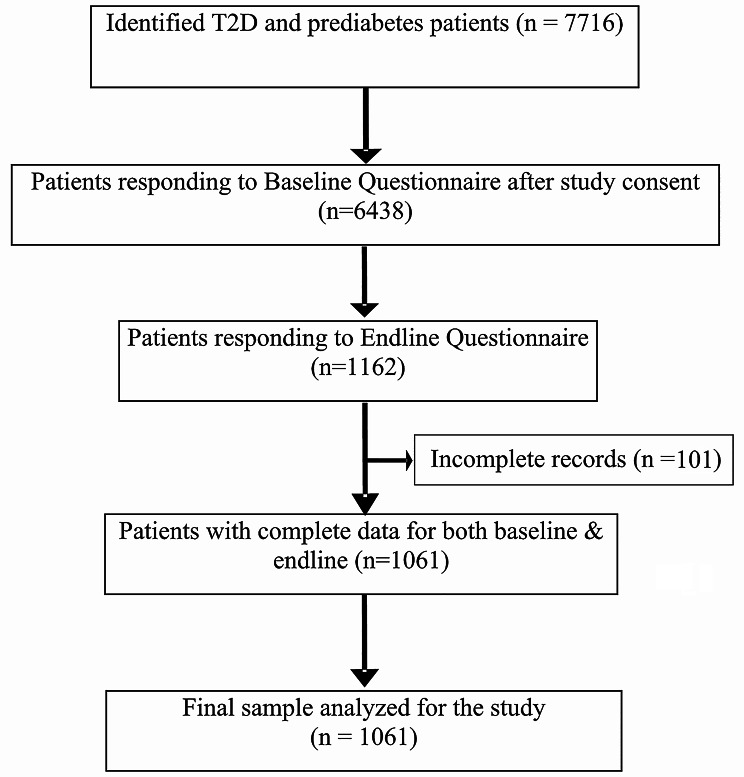
Medical records of individuals with T2D enrolled between June 2021 and June 2023 (n = 7716) were extracted from the electronic database of the Freedom from Diabetes Clinic in Pune, India. All patients (n = 1061 across 175 cities in India) with complete medical records, who met the eligibility criteria and had pre-post data on depression and anxiety scales, were included in the final analysis. The patient flow chart for this study is shown in Fig. 1.
Fig. 1.
Flowchart depicting the selection procedure of patients for the study
Ethical consideration
This retrospective study adhered to the ethical principles outlined in the Declaration of Helsinki. This study was approved by the Freedom from Diabetes Research Foundation Institutional Ethics Committee (approval number: FFDRF/IEC/2024/7). This study was registered with the Clinical Trials Registry of India (CTRI) under registration number CTRI/2024/03/064596 on March 21, 2024. Owing to the retrospective design of the study, the requirement for informed consent from participants was waived by the ethics committee.
Tools used for data collection
The de-identified data of 1061 participants were retrospectively extracted from electronic records maintained by the clinic. Collected data included sociodemographic (sex, age, marital status, education level, occupation, and family history), anthropometric (height and weight), medical history (date of diabetes detection, associated comorbidities, and medication status), and biochemical parameters (HbA1c, Fasting Blood Glucose (FBG), and postprandial blood glucose (PPBG)).
Additionally, the scores of the Patient Health Questionnaire-9 (PHQ-9) and Generalized Anxiety Disorder-7 (GAD-7) scales were included to assess depression and anxiety levels, respectively (data on the two scales were routinely collected as part of the program). Depression severity was assessed using the Patient Health Questionnaire (PHQ-9), a 9-item self-report screening tool. The PHQ-9 uses a 4-point scale ranging from 0 to 3, where 0 signifies “never,” 1 signifies “several days,” 2 signifies “more than half the time,” and 3 signifies “nearly every day.” The total score for the PHQ-9 ranges from 0 to 27, with higher scores indicating greater severity of depression symptoms. The PHQ-9 has established cutoff scores of 5 for mild depression, 10 for moderate depression, 15 for moderately severe depression, and 20 for severe depression. The PHQ-9 has demonstrated a high level of sensitivity (88%) and specificity (88%) for detecting depression [24].
The Generalized Anxiety Disorder (GAD-7), a 7-item self-report screening tool, was used to evaluate anxiety symptoms. Each item on the GAD-7 scale was rated on a 4-point scale from 0 to 3, with 0 representing “never,” 1 representing “several days,” 2 representing “more than half the time,” and 3 representing “nearly every day.” The overall score ranged from 0 to 21, with higher scores indicating greater symptom severity. Cut-offs of 5, 10, and 15 represented mild, moderate, and severe anxiety, respectively. The GAD-7 has a sensitivity of 89% and specificity of 82% for detecting anxiety [25].
Study intervention
The detailed intervention has been previously described [26]. The intervention comprised of four main components: diet, physical activity, psychological support, and medical management. Upon enrollment, each patient was assigned a team of six specialists: physician, dietician, physiotherapist (exercise expert), psychologist, mentor (former program participant who volunteered to guide new patients), and monitor (for follow-ups and reminders for lab tests, appointments, etc.). The intervention was delivered through online group sessions (educational) and individual consultations with each of the four primary experts.
The implemented dietary modifications consisted of a plant-based diet [26]. The goal of this dietary intervention was to detoxify and alkalize [27, 28] the body while facilitating weight loss through a gradual decrease in calorie intake achieved with intermittent fasting [29]. Once the target weight was achieved, the focus shifted towards building muscle through a diet with increased protein intake. This dietary approach was complemented with exercise recommendations. During the initial weight-loss period, the exercises focused on building strength, stamina, and flexibility [26]. After reaching the target weight, the focus shifted to muscle building. Overall, both the diet and exercise plans were individualized to consider the age, sex, fitness level, and comorbidities of each participant.
The psychological intervention aimed to assess participants’ stress and anxiety levels while simultaneously fostering an understanding of the mind-body connection. Each month, a team of psychologists conducted group therapy sessions with different themes. These themes ranged from guided meditations and the introduction of journaling to foster positive energy [30–32] through activities such as self-reflection and goal-setting techniques [32–34] using vision boards [35] to support personal growth and well-being. Additionally, participants who scored high on the PHQ-9 and GAD-7 at baseline (scores above 10, indicating moderate to severe anxiety and/or depression) received individual counseling from their assigned psychologist. Specialized techniques tailored to each patient’s unique circumstances were employed. These techniques include Rational Emotive Behavior Therapy (REBT) to help participants identify and challenge irrational beliefs that contribute to emotional distress [36], Clinical Hypnotherapy to access the subconscious mind and address deep-seated psychological issues [37, 38], Neuro-Linguistic Programming (NLP) techniques to facilitate positive behavior changes through language and thought patterns [39], positive affirmations to help participants reframe negative self-talk, and meditation practices to enhance mindfulness and reduce stress [34]. Participants, especially those with a high depression score, were encouraged to keep gratitude journals to foster a positive outlook on life [32]. For those with high anxiety scores, Cognitive Behavior Therapy (CBT) was employed to identify and modify distorted thinking patterns [5, 18, 40], while breathwork techniques were used to promote relaxation and reduce stress [41]. Additionally, progressive muscle relaxation was introduced to reduce physical tension and anxiety [41]. Life coaching was provided to guide participants in achieving personal goals and overcoming obstacles [42], and pranic healing was included as a complementary approach to empower participants with overall well-being [43]. This customization ensured that the treatment aligned with each patient’s specific needs and comfort level.
Medical management involved daily blood glucose monitoring, addressing nutritional deficiencies through supplements, and at least 3 medical consultations with the assigned physician.
Use of technology
The patients were given access to a dedicated ‘Freedom from Diabetes’ mobile application (https://play.google.com/store/apps/details? id=com.ffd) that allowed them to communicate with the designated team of specialists via voice and video calls and text messages throughout the intervention period. The application was designed to facilitate regular monitoring and updating of vital signs, including FBG, PPBG, weight, and blood pressure, as well as diet and exercise. The physician used the app to closely monitor blood glucose levels and blood pressure, adjusting the daily medication doses as needed. Additionally, the application provided patients with access to plant-based recipes, recorded meditation sessions, and exercise videos.
Throughout the diabetes management program, patients received counseling and motivational support to encourage adherence to the protocol (via live online video conferencing, FFD mobile application, phone calls, and WhatsApp messages). The mobile application was used to conduct monthly adherence checks.
Statistical analyses
In this retrospective analysis, all the data were thoroughly examined for completeness and accuracy. Following extraction in Microsoft Excel, the data were transferred to IBM SPSS (Statistical Package for the Social Sciences, for Windows, Version.21.0 IBM Corp., Armonk, New York, USA) for statistical analyses. Continuous variables are presented using descriptive statistics, with means and standard deviations for normally distributed variables (weight, BMI, HbA1c) and medians with interquartile ranges (IQRs) for skewed variables (anxiety and depression scores). Categorical variables are reported as frequencies and percentages. Classification of patients into mild to severe depression and/or anxiety groups is based on a cut-off score of 5 [24, 25]. To assess the effectiveness of the intervention in reducing depression and/or anxiety levels, pre-post analyses were conducted using paired t-tests for continuous variables and the McNemar test for categorical variables. R-Software was used for the violin plot to show the change in the score from the baseline to the endline. All analyses were two-tailed with a significance level of p < 0.05.
Results
The mean age and diabetes duration of patients were 52 ± 10.4 years and 9.8 ± 7.8 years, respectively. The mean baseline weight (kg), BMI (kg/m2), and HbA1c (%) levels of the patients were 73.06 ± 14.5, 26.5 ± 4.5, and 8 ± 1.7, respectively. The majority of patients were male, married, salaried, had diabetes for more than five years, had a self-reported history of stress before diabetes, and had a family history of diabetes (Table 1). The majority (88.8%) of patients were on medication for diabetes (oral hypoglycemic agents (OHAs) and/or insulin), and most reported having one or more comorbidities (Table 1).
Table 1.
Sociodemographic and biochemical characteristics of the study population
| Parameter | Frequency (N) | Percentage (%) |
|---|---|---|
| Age groups a, b | ||
| Less than 45 years | 257 | 24.2 |
| 45–55 years | 377 | 35.5 |
| 55–65 years | 320 | 30.2 |
| More than 65 years | 107 | 10.1 |
| Sex a, b | ||
| Male | 633 | 59.7 |
| Female | 428 | 40.3 |
| Marital Status b | ||
| Unmarried | 47 | 4.4 |
| Divorced/Separated | 22 | 2.1 |
| Widowed | 23 | 2.2 |
| Married | 969 | 91.3 |
| Education a, b | ||
| Below Graduation | 475 | 46.7 |
| Above Graduation | 542 | 53.3 |
| Occupation | ||
| Self Employed | 228 | 21.5 |
| Salaried | 447 | 42.1 |
| Retired | 157 | 14.8 |
| Other * | 47 | 4.4 |
| Homemaker | 182 | 17.2 |
| Stress Before Diabetes (Self-reported) a, b | ||
| No | 343 | 32.3 |
| Yes | 718 | 67.7 |
| Family History | ||
| No | 233 | 22 |
| Yes | 828 | 78 |
| BMI [44] | ||
| Normal (< 23 kg/m2) | 232 | 21.9 |
| Overweight (23–25 kg/m2) | 210 | 19.8 |
| Obese ( > = 25 kg/m2) | 619 | 58.3 |
| Duration of diabetes a | ||
| Less than 5 years | 347 | 33.5 |
| More than 5 years | 689 | 66.5 |
| Glycemic Control b | ||
| Good (HbA1c less than 7%) | 350 | 33 |
| Poor good (HbA1c more than 7%) | 711 | 67 |
| Medication Usage a, b | ||
| Insulin = Yes | 149 | 14 |
| Insulin = No | 912 | 86 |
| OHAs = Yes | 943 | 88.9 |
| OHAs = No | 118 | 11.1 |
| Comorbidities a, b | ||
| Hypertension = Yes | 441 | 41.6 |
| Hypertension = No | 620 | 58.4 |
| Dyslipidemia = Yes | 644 | 60.7 |
| Dyslipidemia = No | 417 | 39.3 |
aChi-square value significant for anxiety (p < 0.05), b Chi-square value significant for depression (p < 0.05); BMI: Body Mass Index; OHAs: Oral hypoglycemic agents; *Students/Do not wish to share
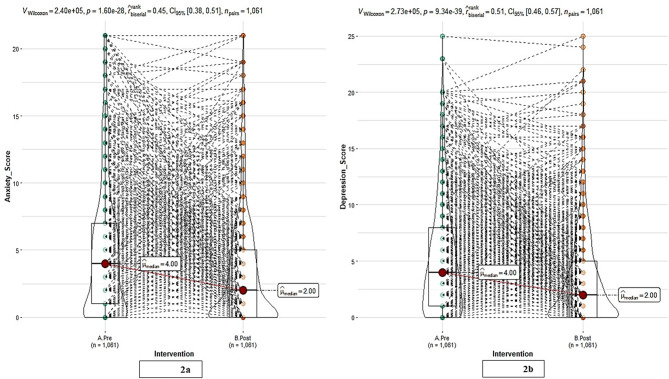
Post-intervention, a statistically significant (p < 0.001) decrease in median weight was observed from 71 kg to 66 kg corresponding to an average reduction of 4.71 kg (95% CI: 4.3 to 5.0 kg). Similarly, median HbA1c levels showed a significant improvement (7.5 to 6.5%) (p < 0.001) following the intervention, with an average decrease of 1.28 (95% CI: 1.1 to 1.3). The effect sizes for the improvements in both weight and HbA1c levels were d = 0.8, indicating that the intervention had a strong and clinically meaningful impact on both weight reduction and improvement in HbA1c levels [45], with a large effect size underscoring the substantial impact of the intervention on these health parameters. Additionally, significant (p < 0.001) improvements in FBG (123 mg/dL to 114 mg/dL) and PPBG (150 mg/dL to 137 mg/dL) were observed. The effect size for the improvements in both FBG and PPBG were d = 0.3, indicating that while the intervention produced statistically significant improvements in both fasting and postprandial blood glucose levels, the magnitude of these improvements was relatively modest compared with the other outcomes measured. A significant reduction was observed in the overall score (Fig. 2) for both anxiety (Fig. 2a) and depression (Fig. 2b) (a decrease in the median score from four to two) in the entire cohort (p < 0.001). The effect size for this improvement was d = 0.3 for anxiety and d = 0.4 for depression, which indicates a small to moderate effect according to Cohen’s conventions [45]. This suggests that the intervention produced a modest but meaningful reduction in anxiety and depression symptoms in the overall cohort.
Fig. 2.
Post-intervention changes in scores in the overall cohort (a) anxiety scores (b) depression scores
Furthermore, all patients were classified according to the severity of their anxiety and depression, ranging from mild to severe at baseline and endline (Tables 2 and 3). The prevalence of depression and anxiety symptoms (ranging from mild to severe) was 46% and 44.3% at baseline, which decreased to 28.7% and 29.2% post-intervention, respectively. The intervention notably improved the symptoms of severe anxiety and depression, with a substantial decrease in scores (8.79 and 9.08 points, respectively).
Table 2.
Change in anxiety scores based on severity
| Anxiety severity* | Pre-Intervention | Post-Intervention | Absolute Difference (95% CI) | P Value | ||
|---|---|---|---|---|---|---|
| Median (IQR) |
N
(%) |
Median (IQR) |
N
(%) |
|||
|
Minimal (Score 0–4) |
1 (0–3) | 591 (55.7) | 1 (0–3) |
751 (70.8) |
0.38 (-0.61 to 0.16) | 0.05 |
|
Mild (Score 4–9) |
6 (5–7) | 302 (28.5) | 4 (1–6) |
224 (21.1) |
2.34 (1.93 to 2.74) | < 0.001 |
|
Moderate (Score 10–14) |
12 (11–14) | 109 (10.3) | 5 (2–7.5) |
57 (5.4) |
6.07 (5.14 to 7) | < 0.001 |
|
Severe (score 15–21) |
17 (15–19) | 59 (5.6) | 8 (3–14) |
29 (2.7) |
8.79 (7.05 to 10.53) | < 0.001 |
*Represent the standard categories and the score of the GAD-7; IQR, Interquartile range; CI, Confidence interval
Table 3.
Change in depression scores based on severity
| Depression severity* | Pre-Intervention | Post-Intervention | Absolute Difference (95% CI) | P Value | ||
|---|---|---|---|---|---|---|
| Median (IQR) |
N
(%) |
Median (IQR) | N (%) | |||
|
None-minimal (Score 0–4) |
2 (0–3) |
573 (54) |
1 (0–3) | 757 (71.3) | -0.19 (-0.41 to 0.02) | 0.962 |
|
Mild (Score 5–9) |
7 (6–8) |
297 (28) |
3 (1–6) | 217 (20.5) | 2.85 (2.43 to 3.27) | < 0.001 |
|
Moderate (Score 10–14) |
12 (10–13) | 133 (12.5) | 6 (3–9) | 59 (5.6) | 5.28 (4.48 to 6.08) | < 0.001 |
|
Moderately Severe (Score 15–19) |
17 (16–18) | 46 (4.3) | 6.5 (2–13.5) | 21 (2.0) | 8.76 (6.92 to 10.6) | < 0.001 |
|
Severe (Score 20–27) |
20 (17.3–22.25) | 12 (1.1) | 10 (2.75–20.25) | 7 (0.7) | 9.08 (3.64 to 15.18) | < 0.001 |
*Represent the standard categories and the score of the PHQ-9; IQR, Interquartile range; CI, Confidence interval
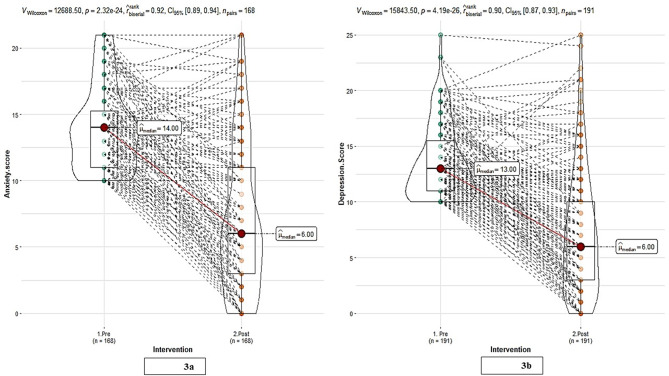
Post-intervention, changes in scores in those with moderate-to-severe symptoms at baseline were analyzed (Fig. 3). Among the 168 patients with moderate-to-severe anxiety at baseline, 69.6% demonstrated an improvement in their scores post-intervention, with the median score decreasing from 14 to 6 (Fig. 3a). Likewise, among the 191 patients with moderate-to-severe depression at baseline, 70.2% exhibited improvement in their scores following the intervention, with the median score dropping from 13 to 6 (Fig. 3b). The effect sizes were d = 1.2 and 1.1 for anxiety and depression, respectively, indicating a substantial impact of the intervention on both conditions. Effect sizes above 0.8 are regarded as large, suggesting a strong and clinically meaningful reduction in anxiety and depression in patients with moderate to severe baseline symptoms.
Fig. 3.
Post-intervention changes in scores in those with moderate to severe conditions at baseline (a) anxiety scores (b) depression scores
Individual counseling was provided to those with moderate to severe anxiety and depression. Further analysis to test the efficacy of individual counseling revealed that patients with anxiety at baseline (n = 168) showed a significant improvement in their scores, with a median decrease from 14 to 5 with counseling and 14 to 7 without counseling. Similarly, in patients with depression at baseline (n = 191), there was a significant improvement in scores; the median score decreased from 13 to 6 for those who received individual counseling and from 12 to 6.5 for those who opted not to receive counseling. The change in median scores was similar in those who received individual counseling versus those who did not (p > 0.1).
Discussion
This retrospective analysis investigated the efficacy of an online integrated ILI for diabetes management to alleviate anxiety and depression in individuals with T2D. The high prevalence of both anxiety and depression symptoms in the study cohort underscores the need for an effective intervention that we addressed through a multidisciplinary approach that showed promising results. The study outcomes revealed marked improvements in the symptoms of anxiety and depression, with the largest reductions observed in individuals experiencing moderate to severe symptoms.
Our study identified a high prevalence of mild to severe depression (46%) and anxiety (44.3%) in our cohort, which was higher than that previously reported for the Indian population [46–49]. This may be attributed to the use of a cutoff score of 5, which includes individuals with mild to severe symptoms of depression and/or anxiety [24, 25], which are often overlooked in studies using higher clinical cut-offs. With a cutoff of 10, the prevalence decreased to 18% for depression and 15.8% for anxiety at baseline which is comparable to other studies [49–51]. The higher prevalence of depression compared to anxiety aligns with previous reports [48, 52]. Post-intervention, participants experienced significant reductions in anxiety and depression scores, with a median drop of two points each. The intervention notably improved severe anxiety, with a substantial decrease of 8.79 points, consistent with the effectiveness of CBT for severe anxiety [40, 53]. For depression, the largest reductions were in the moderately severe to severe groups, with median decreases of 8.76 and 9.08 points, respectively. These findings demonstrate that the intervention was particularly effective in patients with more severe symptoms at baseline, leading to significant reductions in both anxiety and depression scores. Furthermore, the large effect sizes of 1.2 and 1.1 for anxiety and depression highlight the intervention’s substantial impact. These findings align with prior research demonstrating the efficacy of lifestyle modifications, encompassing adjustments to diet and physical activity, in reducing depressive symptoms [54].
Lifestyle interventions, including physical activity, dietary changes, and stress management, improve mental health by improving physiological and psychological well-being [55, 56]. This comprehensive approach addresses the diverse challenges of T2D affecting both physical and psychological health [4]. Previous study has reported significant improvements in anxiety, depression, weight, BMI, and HbA1c levels compared with conventional methods [54]. The efficacy of healthy lifestyle interventions in reducing stress and depression among T2D patients is well-documented [55]. Furthermore, our findings indicate that there was a significant reduction in scores for both anxiety and depression irrespective of individual counseling, suggesting that, although individual counseling contributed to positive outcomes, it may not be the sole factor driving improvement. The comprehensive ILI program, which incorporated components such as exercise, meditation, and yoga, appears to have played a more substantial role in reducing the symptoms of anxiety and depression. These components likely contribute to improved mental health through the reduction of stress hormones, enhancement of mood, and promotion of overall well-being [31, 57, 58]. Improvements in diet and eating habits are also known to enhance blood sugar control and reduce inflammation, contributing to a reduction in anxiety and depression [55]. The ILI also provides social support through group sessions, which can buffer against stress and help people cope with chronic health conditions [59–61]. The group sessions included guided meditation, journaling, and activities promoting positive energy, leading to a calmer mind-body state [62]. A focus on positive emotions through activities such as vision boards contributed to positive outcomes [35, 63]. Further, we chose an online mode for delivery of the intervention because it provides a flexible and accessible means of delivering health-related support with the potential to reach a wide audience at a lower cost. They can also enhance user engagement and self-management capabilities, which are essential for improving health outcomes. However, the implementation of such interventions must consider the associated challenges to maximize their effectiveness [64–68].
The key advantage of this research lies in its lifestyle intervention, significant sample size, and broader geographical coverage compared with earlier Indian studies. However, this study has some limitations, including the lack of a control group and the ability to assess only short-term post-intervention effects. Future prospective studies with longer follow-up periods and control group are necessary to confirm these findings, evaluate the sustainability of the intervention, and explore the mechanisms underlying the outcomes. Despite the large sample size, the retrospective design of our study may have led to a selection bias and confounding factors, which could limit the generalizability of our findings to the broader Indian population. Nevertheless, the online nature of the program allowed us to engage participants from 175 cities across India, potentially expanding the scope of our study and providing a more diverse sample. Additionally, the online program’s subscription model may limit access to those with the financial means to afford it, affecting the generalizability of the results. Furthermore, the success of the intervention depended on patient participation and adherence to lifestyle changes. Despite these limitations, this study provides valuable insights into the prevalence of anxiety and depression among individuals with diabetes in India and the effectiveness of lifestyle interventions in addressing these concerns.
Conclusion
Online lifestyle-driven multidisciplinary interventions significantly improved the symptoms of anxiety and depression in patients with T2D. Our study contributes to growing evidence that lifestyle modifications may effectively manage these mental health challenges. Future research with a robust design and long-term follow-up is essential to confirm these findings and explore the underlying mechanisms.
Acknowledgements
Not applicable.
Abbreviations
- T2D
Type 2 diabetes
- ILI
Intensive Lifestyle Intervention
- PHQ-9
Patient Health Questionnaire
- GAD-7
Generalized Anxiety Disorders
- CTRI
Clinical Trial Registry of India
- ADA
American Diabetes Association
- REBT
Rational Emotive Behavior Therapy
- NLP
Neuro-Linguistic Programming
- CBT
Cognitive Behavior Therapy
- SPSS
Statistical Package for the Social Sciences
- IQRs
Interquartile Range
- OHAs
Oral Hypoglycemic Agents
- BMI
Body Mass Index
- FBG
Fasting Blood Glucose
- PPBG
Postprandial Blood Glucose
Author contributions
PT, NK, and MG designed the study. BSh and MB analyzed the data and wrote the initial draft of the paper. NK, VG, and BS supervised the data analysis and writing of the paper. MK assisted in the data analysis. DT, TK, and AV contributed to the interpretation of the data and writing of the manuscript. All authors critically reviewed the drafts and revised the manuscript accordingly. All the authors have read and approved the final manuscript.
Funding
Not applicable.
Data availability
All data supporting our findings have been presented in the manuscript, and the datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The research was performed in accordance with the Declaration of Helsinki. Individual identities were not disclosed to protect the participants’ confidentiality. The study was approved by the Freedom from Diabetes Research Foundation - Institutional Ethics Committee (approval number: FFDRF/IEC/2024/7) and registered with the Clinical Trials Registry of India (CTRI/2024/03/064596, registered on March 21, 2024). Given the retrospective design of the study, the Ethics Committee waived the requirement for informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Moitra M, Santomauro D, Collins PY, Vos T, Whiteford H, Saxena S et al. The global gap in treatment coverage for major depressive disorder in 84 countries from 2000–2019: a systematic review and bayesian meta-regression analysis. PLoS Med. 2022;19. [DOI] [PMC free article] [PubMed]
- 2.Walker ER, McGee RE, Druss BG. Mortality in Mental disorders and Global Disease Burden implications: a systematic review and Meta-analysis. JAMA Psychiatry. 2015;72:334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dilworth L, Facey A, Omoruyi F. Diabetes Mellitus and its metabolic complications: the role of adipose tissues. Int J Mol Sci 2021. 2021;22:22:7644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Franquez RT, de Souza IM, de Cássia Bergamaschi C. Interventions for depression and anxiety among people with diabetes mellitus: review of systematic reviews. PLoS ONE. 2023;18:e0281376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sohrabi F, Sohrabi · Ahmad, Shams-Alizadeh N, Cayoun BA. Managing type 2 diabetes and depression with Mindfulness-integrated Cognitive Behavior Therapy (MiCBT). Discover Psychology 2022 2:1. 2022;2:1–23.
- 6.Depression. and Other Common Mental Disorders Global Health Estimates.
- 7.Fang T, Zhang Q, Wang Z, Liu JP. Bidirectional association between depression and diabetic nephropathy by meta-analysis. PLoS ONE. 2022;17:e0278489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lyra e Silva N, de M, Lam MP, Soares CN, Munoz DP, Milev R, De Felice FG. Insulin resistance as a shared pathogenic mechanism between depression and type 2 diabetes. Front Psychiatry. 2019;10(FEB):420372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Association AD. 4. Comprehensive Medical evaluation and Assessment of comorbidities: standards of Medical Care in Diabetes—2021. Diabetes Care. 2021;44 Supplement1:S40–52. [DOI] [PubMed] [Google Scholar]
- 10.Mental disorders. https://www.who.int/news-room/fact-sheets/detail/mental-disorders. Accessed 27 Jan 2024.
- 11.Khaledi M, Haghighatdoost F, Feizi A, Aminorroaya A. The prevalence of comorbid depression in patients with type 2 diabetes: an updated systematic review and meta-analysis on huge number of observational studies. Acta Diabetol. 2019;56. [DOI] [PubMed]
- 12.Albekairy A, Aburuz S, Alsabani B, Alshehri A, Aldebasi T, Alkatheri A, et al. Exploring factors Associated with Depression and anxiety among hospitalized patients with type 2 diabetes Mellitus. Med Princ Pract. 2017;26:547–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nouwen A, Adriaanse MC, van Dam K, Iversen MM, Viechtbauer W, Peyrot M, et al. Longitudinal associations between depression and diabetes complications: a systematic review and meta-analysis. Diabet Med. 2019;36:1562–72. [DOI] [PubMed] [Google Scholar]
- 14.Jafari A, Moshki M, Ghelichi-Ghojogh M, Nejatian M. Role of diabetes health literacy, psychological status, self-care behaviors, and life satisfaction in predicting quality of life in type 2 diabetes. Sci Rep. 2024;14. [DOI] [PMC free article] [PubMed]
- 15.Pilkington K, Wieland LS. Self-care for anxiety and depression: a comparison of evidence from Cochrane reviews and practice to inform decision-making and priority-setting. BMC Complement Med Ther. 2020;20. [DOI] [PMC free article] [PubMed]
- 16.Sartorius N. Depression and diabetes. Dialogues Clin Neurosci. 2018;20:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pot GK, Battjes-Fries MCE, Patijn ON, Van Der Zijl N, Pijl H, Voshol P. Lifestyle medicine for type 2 diabetes: practice-based evidence for long-term efficacy of a multicomponent lifestyle intervention (reverse Diabetes2 now). BMJ Nutr Prev Health. 2020;3:bmjnph–2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang X, Li Z, Sun J. Effects of cognitive behavioral therapy–based intervention on improving glycaemic, psychological, and physiological outcomes in adult patients with diabetes Mellitus: a Meta-analysis of Randomized controlled trials. Front Psychiatry. 2020;11:711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pamungkas RA, Chamroonsawasdi K, Vatanasomboon PA, Systematic Review. Family Support Integrated with Diabetes Self-Management among Uncontrolled Type II Diabetes Mellitus Patients. Behavioral Sciences 2017, Vol 7, Page 62. 2017;7:62. [DOI] [PMC free article] [PubMed]
- 20.Richards DA, Hill JJ, Gask L, Lovell K, Chew-Graham C, Bower P et al. Clinical effectiveness of collaborative care for depression in UK primary care (CADET): cluster randomised controlled trial. BMJ. 2013;347. [DOI] [PMC free article] [PubMed]
- 21.Liu S, Leone M, Ludvigsson JF, Lichtenstein P, Gudbjörnsdottir S, Landen M, et al. Early-onset type 2 diabetes and Mood, anxiety, and stress-related disorders: a genetically informative Register-based Cohort Study. Diabetes Care. 2022;45:2950–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.MacDonald CS, Nielsen SM, Bjørner J, Johansen MY, Christensen R, Vaag A, et al. One-year intensive lifestyle intervention and improvements in health-related quality of life and mental health in persons with type 2 diabetes: a secondary analysis of the U-TURN randomized controlled trial. BMJ Open Diabetes Res Care. 2021;9:e001840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Diabetes D. & Tests | ADA. https://diabetes.org/about-diabetes/diagnosis. Accessed 17 Jul 2024.
- 24.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief Depression Severity measure. J Gen Intern Med. 2001;16:606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–7. [DOI] [PubMed] [Google Scholar]
- 26.Tripathi P, Kadam N, Tiwari D, Kathrikolly T, Vyawahare A, Sharma B, et al. The diabetes remission in India (DiRemI) study: protocol for a prospective matched-control trial. PLoS ONE. 2024;19:e0306394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Adair KE, Bowden RG. Ameliorating Chronic Kidney Disease Using a Whole Food Plant-Based Diet. Nutrients 2020, Vol 12, Page 1007. 2020;12:1007. [DOI] [PMC free article] [PubMed]
- 28.Storz MA, Ronco AL, Hannibal L. Observational and clinical evidence that plant-based nutrition reduces dietary acid load. J Nutr Sci. 2022;11:e93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rynders CA, Thomas EA, Zaman A, Pan Z, Catenacci VA, Melanson EL. Effectiveness of intermittent fasting and time-restricted feeding compared to Continuous Energy Restriction for Weight Loss. Nutrients. 2019;11. [DOI] [PMC free article] [PubMed]
- 30.Dixon LJ, Hornsey MJ, Hartley N. The secret to success? The psychology of belief in Manifestation. https://doi.org/101177/01461672231181162. 2023. https://doi.org/10.1177/01461672231181162. [DOI] [PMC free article] [PubMed]
- 31.Marmarosh CL, Sandage S, Wade N, Captari LE, Crabtree S. New horizons in group psychotherapy research and practice from third wave positive psychology: a practice-friendly review. Res Psychotherapy: Psychopathol Process Outcome. 2022;25:258–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smyth JM, Johnson JA, Auer BJ, Lehman E, Talamo G, Sciamanna CN. Online positive affect Journaling in the improvement of Mental Distress and Well-being in General Medical patients with elevated anxiety symptoms: a preliminary Randomized Controlled Trial. JMIR Ment Health. 2018;5. [DOI] [PMC free article] [PubMed]
- 33.Kulbaş E, Özabacı N. The effects of the Positive Psychology-Based Online Group Counselling Program on Mothers having children with intellectual disabilities. J Happiness Stud. 2022;23:1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lindsay EK, Chin B, Greco CM, Young S, Brown KW, Wright AGC, et al. How mindfulness training promotes positive emotions: dismantling acceptance skills training in two randomized controlled trials. J Pers Soc Psychol. 2018;115:944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alyami M, Serlachius A, Law M, Murphy R, Almigbal TH, Lyndon M et al. Utility and acceptability of a brief type 2 diabetes visual animation: mixed methods feasibility study. JMIR Form Res. 2022;6. [DOI] [PMC free article] [PubMed]
- 36.Turner MJ. Rational Emotive Behavior Therapy (REBT), Irrational and Rational Beliefs, and the Mental Health of Athletes. Front Psychol. 2016;7 SEP. [DOI] [PMC free article] [PubMed]
- 37.Peter B. Hypnosis in psychotherapy, psychosomatics and medicine. A brief overview. Front Psychol. 2024;15. [DOI] [PMC free article] [PubMed]
- 38.Pereira M. Da G. changing the mind: hypnosis and diabetes. Rev Lat Am Enfermagem. 2017;25:e2868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Doğan A, Doğan R, Menekli T, Berktaş HB. Effect of neuro-linguistic programming on COVID-19 fear in kidney transplant patients: a randomized controlled study. Complement Ther Clin Pract. 2022;49:101638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Curtiss JE, Levine DS, Ander I, Baker AW. Cognitive-Behavioral Treatments for Anxiety and Stress-Related Disorders. https://doi.org/101176/appi.focus20200045. 2021;19:184–9. [DOI] [PMC free article] [PubMed]
- 41.Yadav A, Kaushik RM, Kaushik R. Effects of diaphragmatic breathing and systematic relaxation on Depression, anxiety, stress, and Glycemic Control in type 2 diabetes Mellitus. Int J Yoga Th. 2021;31. [DOI] [PubMed]
- 42.van Zyl LE, Roll LC, Stander MW, Richter S. Positive psychological coaching definitions and models: a systematic literature review. Front Psychol. 2020;11:793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nittur A, Pavan B, Ganapathy R, Dorai VK, Singhal S. Pranic Healing as a complementary therapy in Diabetic Foot Ulcer Management: a randomised, controlled, double-blind trial. Global Adv Integr Med Health. 2023;12. [DOI] [PMC free article] [PubMed]
- 44.(PDF). Consensus Statement for Diagnosis of Obesity, Abdominal Obesity and the Metabolic Syndrome for Asian Indians and Recommendations for Physical Activity, Medical and Surgical Management. https://www.researchgate.net/publication/26652681_Consensus_Statement_for_Diagnosis_of_Obesity_Abdominal_Obesity_and_the_Metabolic_Syndrome_for_Asian_Indians_and_Recommendations_for_Physical_Activity_Medical_and_Surgical_Management#fullTextFileContent. Accessed 16 Mar 2024. [PubMed]
- 45.Sullivan GM, Feinn R. Using effect size—or why the P value is not enough. J Grad Med Educ. 2012;4:279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Karpha K, Biswas J, Nath S, Dhali A, Sarkhel S, Dhali GK. Factors affecting depression and anxiety in diabetic patients: a cross sectional study from a tertiary care hospital in Eastern India. Annals Med Surg. 2022;84:104945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Khullar S, Dhillon H, Kaur G, Sharma R, Mehta K, Aggarwal R, et al. The prevalence and predictors of Depression in Type 2 Diabetic Population of Punjab. Community Ment Health J. 2016;52:479–83. [DOI] [PubMed] [Google Scholar]
- 48.Hussain S, Habib A, Singh A, Akhtar M, Najmi AK. Prevalence of depression among type 2 diabetes mellitus patients in India: a meta-analysis. Psychiatry Res. 2018;270:264–73. [DOI] [PubMed] [Google Scholar]
- 49.Paudel S, Khanal SP, Gautam S, Chalise A, Koirala TN, Marahatta SB. Original research: anxiety and depression among people with type 2 diabetes visiting diabetes clinics of Pokhara Metropolitan, Nepal: a cross-sectional study. BMJ Open. 2023;13:64490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sharma K, Dhungana G, Adhikari S, Bista Pandey A, Sharma M. Depression and Anxiety among Patients with Type II Diabetes Mellitus in Chitwan Medical College Teaching Hospital, Nepal. Nurs Res Pract. 2021;2021. [DOI] [PMC free article] [PubMed]
- 51.Aga IZ, Khurram SS, Karim M, Muzzamil M, Hashmi S, Shafique K. Authors authors employing telepsychiatry services to assess the prevalence and identify mental health disorders using the PHQ-9 and GAD-7 in resource-constrained regions of Dadar Mansehra, Pakistan: an observational cross-sectional study. BMJ Open. 2023;13:78976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Badillo N, Khatib M, Kahar P, Khanna D. Correlation between body Mass Index and Depression/Depression-Like symptoms among different genders and races. Cureus. 2022;14. [DOI] [PMC free article] [PubMed]
- 53.Li J, Cai Z, Li X, Du R, Shi Z, Hua Q, et al. Mindfulness-based therapy versus cognitive behavioral therapy for people with anxiety symptoms: a systematic review and meta-analysis of random controlled trials. Ann Palliat Med. 2021;10:7596612–7612. [DOI] [PubMed] [Google Scholar]
- 54.Aguilar-Latorre A, Pérez Algorta G, Navarro-Guzmán C, Serrano-Ripoll MJ, Oliván-Blázquez B. Effectiveness of a lifestyle modification programme in the treatment of depression symptoms in primary care. Front Med (Lausanne). 2022;9. [DOI] [PMC free article] [PubMed]
- 55.Bradley T, Campbell E, Dray J, Bartlem K, Wye P, Hanly G, et al. Systematic review of lifestyle interventions to improve weight, physical activity and diet among people with a mental health condition. Syst Rev. 2022;11:198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Levine GN, Cohen BE, Commodore-Mensah Y, Fleury J, Huffman JC, Khalid U, et al. Psychological Health, Well-Being, and the mind-heart-body connection: a Scientific Statement from the American Heart Association. Circulation. 2021;143:E763–83. [DOI] [PubMed] [Google Scholar]
- 57.Priya G, Kalra S. Mind–body interactions and mindfulness meditation in diabetes. Eur Endocrinol. 2018;14:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Raveendran AV, Deshpandae A, Joshi SR. Therapeutic role of yoga in type 2 diabetes. Endocrinol Metab. 2018;33:307–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Parviniannasab AM, Faramarzian Z, Hosseini SA, Hamidizadeh S, Bijani M. The effect of social support, diabetes management self-efficacy, and diabetes distress on resilience among patients with type 2 diabetes: a moderated mediation analysis. BMC Public Health. 2024;24:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Beverly EA, Ritholz MD, Dhanyamraju K. The buffering effect of social support on diabetes distress and depressive symptoms in adults with type 1 and type 2 diabetes. Diabet Med. 2021;38:e14472. [DOI] [PubMed] [Google Scholar]
- 61.Hempler NF, Joensen LE, Willaing I. Relationship between social network, social support and health behaviour in people with type 1 and type 2 diabetes: cross-sectional studies. BMC Public Health. 2016;16:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dong Y, Zhang X, Zhao R, Cao L, Kuang X, Yao J. The effects of mind-body exercise on anxiety and depression in older adults: a systematic review and network meta-analysis. Front Psychiatry. 2024;15. [DOI] [PMC free article] [PubMed]
- 63.Burton L, Lent J. The use of vision boards as a therapeutic intervention. J Creat Ment Health. 2016;11:52–65. [Google Scholar]
- 64.Jiang S. Talk to your doctors online: an internet-based intervention in China. Health Commun. 2021;36:405–11. [DOI] [PubMed] [Google Scholar]
- 65.Solomon M, Wagner SL, Goes J. Effects of a web-based intervention for adults with chronic conditions on patient activation: online randomized controlled trial. J Med Internet Res. 2012;14:e1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.View of Meta-Analysis. Effectiveness of Web-Based Intervention to Increase Physical Activity in Older People. https://thejhpb.com/index.php/thejhpb/article/view/350/213. Accessed 26 Aug 2024.
- 67.Im EO, Chang SJ. Web-based interventions in nursing. CIN - Computers Inf Nurs. 2013;31:94–102. [DOI] [PubMed] [Google Scholar]
- 68.Colvin J, Chenoweth L, Bold M, Harding C. Caregivers of older adults: advantages and disadvantages of internet-based Social Support*. Fam Relat. 2004;53:49–57. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data supporting our findings have been presented in the manuscript, and the datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.