Abstract
Background
Intestinal tuberculosis is a rare disease in western countries, affecting mainly immigrants and immunocompromised patients. Intestinal tuberculosis is a diagnostic challenge, especially when active pulmonary infection is absent. It may mimic many other abdominal diseases.
Case presentation
Here, we report a case of isolated colonic tuberculosis where the initial diagnostic workup was suggestive of Crohn's disease. Computed tomography findings however, raised the possibility of colonic tuberculosis and the detection of acid-fast bacilli in biopsy specimens confirmed the diagnosis.
Conclusions
In conclusion, this case highlights the need for awareness of intestinal tuberculosis in the differential diagnosis of chronic intestinal disease
Background
Intestinal tuberculosis (TB) is rarely seen in western countries, affecting mainly immigrants and immunocompromised patients [1-5]. However, the incidence of abdominal TB has been steadily increasing for the past 20 years [4,6-8] and a reported 2–3% of patients with abdominal TB have isolated colonic involvement [5]. Intestinal TB is usually a diagnostic challenge, particularly in the absence of active pulmonary infection. It may mimic many other abdominal diseases, such as other infectious processes, tumors, periappendiceal abscess, and Crohn's disease (CD) [7]. Several cases of intestinal TB have so far been described [1-5,9] including a few reports of intestinal TB mimicking CD [10,11]. The differential diagnosis between TB and CD is important because if TB is suspected, empiric treatment with antituberculous drugs should be considered, especially if an immunosuppresive treatment for CD is to be initiated.
In this report we present a case of isolated colonic TB in which the initial diagnostic workup suggested CD. It highlights the need for awareness of intestinal TB in the differential diagnosis of chronic intestinal disease.
Case presentation
A 61-yr-old man, born and raised in Crete, was admitted to our hospital with a 6-month history of diarrhea, weight loss of 7 kg, weakness, anorexia, low grade fever, and episodes of pain in the right lower abdominal quadrant. He did not reported arthralgias, rash, cough, or the presence of blood in his stools. There was no family history of inflammatory bowel disease or colon cancer. His past medical history included a diagnosis of hypothyoidism under treatment with thyroxine 100 mcg/d, and an episode of haemoptysis five years ago attributed to bronchiectasis. The patient had no past history of TB and was not aware of any TB exposure. He had been drinking alcohol (50–60 g/d) for 25 years, but stopped drinking five years ago. He did not smoke and worked as auxiliary staff in a community mental clinic.
Physical examination revealed mild abdominal tenderness, mostly confined to the right lower quadrant. The remainder of the examination was unremarkable. The laboratory workup showed a mild anaemia (Hb 11.5 g/dl, Hct 35.8%, MCV 68.1 fl), a serum ferritin of 7.71 (normal, 12–237 ng/ml) and a serum folate of 4.2 ng/ml (normal, 5.3–14.4 ng/ml). Liver biochemistries, total cholesterol, serum proteins, prothrombin time and thyroid hormones were within normal range. Serologic testing for HIV, Yersinia and E. histolytica were negative. Stool samples were negative for infectious organisms. A chest x-ray examination presented no significant findings.
Colonoscopy revealed a tumorous lesion in the ascending colon near the caecum. The colonoscope could not be introduced beyond the lesion. Initial endoscopic diagnosis was that of a malignant lesion, and multiple biopsies were obtained. Histology showed chronic inflammatory changes and noncaseating epithelioid granulomas, a pattern consistent with Crohn's disease. Esophagogastroduodenoscopy showed an axial hiatal hernia and a diffusely erythematous gastric mucosa. A small bowel series was normal. A tentative diagnosis of Crohn's disease was made and a treatment with Budesonide 9 mg/d and Mesalamine 3 g/d was initiated. However, no improvement was noticed and the diarrhea and fever rather deteriorated in the next days.
A CT-scan examination was performed to rule out an abdominal or pelvic abscess. The CT scan revealed a concentric wall thickening confined to the caecal-ascending colon border, luminal stenosis, extensive thickening of the mesenteric folds, the peritoneum and great omentum, small mesenteric lymph nodes, and a small amount of high density peritoneal fluid (Figures 1 and 2). CT findings were not consistent with Crohn's disease and raised the possibility of TB involvement. Tuberculin test was negative. A thoracic CT revealed nodular and fibrotic changes in the apical segments of the upper lobes, a pattern consistent with past TB exposure. Bronchoscopy was normal and acid-fast bacilli were not detected in the sputum, bronchoalveolar lavage or gastric aspirate. In view of our failure to confirm the diagnosis of colonic TB, a second colonoscopy was planned to obtain new biopsy specimens for culture and PCR analysis. When however the biopsies from the tumorous lesion were reevaluated and appropriately stained to look for acid-fast rods, several tubercle bacilli were identified upon Zielh-Neelsen staining. The patient was treated with Rifampicin (10 mg/kg/d), Isoniazid (5 mg/kg/d), Pyrazinamide (30 mg/kg/d) and Ethambutol (15 mg/kg/d). Over the next 10 days, the patient became afebrile, the stools were formed, at a frequency of 2–3 times per day, and he was subsequently discharged from the hospital in good condition. The patient was seen 2 months after discharge at which time he had gained weight and he was asymptomatic. Colonoscopy revealed a normal appearing caecal mucosa. Currently, six months after diagnosis, the patient is free of symptoms and is continuing the anti-tuberculous treatment.
Figure 1.

Colonic wall thickening with irregular outer margins. Note the thickening of the mesenteric folds.
Figure 2.
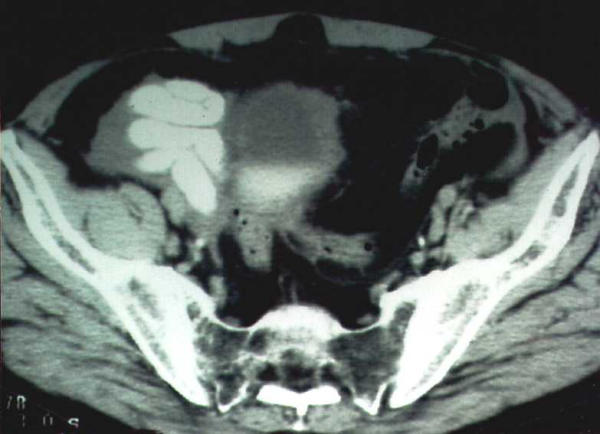
High density peritoneal fluid, peritoneal thickening and extensive mesenteric infiltration in the pelvis.
Discussion
The ileo-caecal area is reported to be the area most commonly involved in colonic tuberculosis [1,3,4,7,12-15]. The apparent affinity of the tubercle bacillus for lymphoid tissue and areas of physiologic stasis facilitating prolonged contact between the bacilli and the mucosa may be the reasons for the ileum and cecum being the most common sites of disease. Other areas of the colon besides the ileocaecal area represent the next more common site of tuberculous involvement of the GI tract, usually manifested as segmental colitis involving the ascending and transverse colon [1,15]. Colonic TB may present as an inflammatory stricture, hypertrophic lesions resembling polyps or tumors, segmental ulcers and colitis or rarely, diffuse tuberculous colitis [7]. The diagnosis can be quite difficult since there are no specific clinical symptoms of large bowel TB and only a quarter of patients have chest radiographs showing evidence of active or healed pulmonary infection [1,15,16]. The clinical, radiological and endoscopic picture is most likely to be confused with neoplasms or Crohn's disease, and infrequently with other considerations including amoeboma, Yersinia infection, GI histoplasmosis, and periappendiceal abscess [7].
The diagnostic procedure of choice is colonoscopy and biopsy [17]. Apart from routine histology looking for caseating granulomas, appropriately stained slides should be prepared to look for acid-fast rods and biopsies should also be sent for culture [7]. Biopsies should be taken preferably from the margins of ulcerations because granulomas are often submucosal [7]. However, granulomas with or without caseation are usually seen in less than 50% of patients [1,7,15], while clusters of epithelioid cells without well formed granulomas have been reported to occur in 20–30% of the biopsies obtained [1,15]. Similarly, in a considerable number of cases the biopsies have features of chronic inflammation but no granulomas, caseation or clusters of epithelioid cells [1,15]. Only 35–60% of cases can be rapidly diagnosed by the finding of acid-fast rods [7], however there are reports indicating no detection of tubercle bacilli in the biopsies [1]. Culture of the biopsy material may increase the diagnostic yield [7], however disappointing results with 0% detection of acid-fast bacilli have also been reported [1]. Polymerase chain reaction analysis of biopsy specimens obtained endoscopically has been shown to be more sensitive than culture and acid-fast stains in diagnosing intestinal TB [18]. Other studies have suggested that an enzyme-linked immunosorbent assay using mycobacterial saline-extracted antigen may increase the yield of correct diagnosis of colonic TB [19]. Extensive infiltration of the peritoneum, omentum and mesentery – in the form of peritoneal folds thickening – and the coexistence of high density peritoneal fluid are CT findings favoring the diagnosis of TB involvement [20]. Small bowel series and barium enema most often reveal a high-riding cecum with or without a string-like lesion of the terminal ileum [7]. The preferred treatment of GI TB is with antituberculous drugs, with surgery reserved primarily for complications [7].
Our case illustrates not only a typical manifestation of isolated colonicTB, but also a case mimicking CD. Colonoscopic differentiation between TB and Crohn's colitis can be difficult taking into account that both entities may present themselves with mucosal ulcerations and nodularity, apthous ulcers, oedematous mucosal folds, strictures and pseudopolyps and luminal narrowing [21]. Although in our case endoscopic appearance was suggestive of a neoplasm, histology showed chronic inflammatory changes and noncaseating epithelioid granulomas, a pattern consistent with CD. CT scan was helpful revealing an infiltrative pattern suggesting TB. This is in accordance with other reports where it was found that CT scan was useful for the diagnosis avoiding unnecessary exploratory laparotomy [22]. Finally with the detection of acid-fast bacilli in our biopsy specimens we were able to set the correct diagnosis. It then became obvious that despite normal appearing chest x-ray the previously mentioned episode of haemoptysis was probably due to active pulmonary TB. Correct diagnosis in such patients is extremely important taking into account that steroid treatment may have potentially disastrous effects.
In conclusion colonic TB should be considered as a differential diagnosis in patients suspected of having a tumourous lesion on colonoscopy and in patients suspected of having Crohn's disease.
List of abbrevations
CD, Crohn's disease; CT, computer tomography; GI, gastrointestinal; TB, tuberculosis
Competing interests
None declared
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
Written consent was obtained from the patient for publication of the patient's details
Contributor Information
Constantinos Chatzicostas, Email: matrix01gr@yahoo.gr.
Ioannis E Koutroubakis, Email: ktjohn@her.forthnet.gr.
Maria Tzardi, Email: tzardi_maria@yahoo.co.uk.
Maria Roussomoustakaki, Email: rousso@med.uoc.gr.
Panagiotis Prassopoulos, Email: gournick@med.uoc.gr.
Elias A Kouroumalis, Email: kouroum@med.uoc.gr.
References
- Singh V, Kumar P, Kamal J, Prakash V, Vaiphei K, Singh K. Clinicocolonoscopic profile of colonic tuberculosis. Am J Gastroenterol. 1996;91:565–568. [PubMed] [Google Scholar]
- Probert CSJ, Jayanti V, Wicks AC, Carr-Locke DL, Mayberry JF. Epidemiological study of abdominal tuberculosis among Indian migrants and the indigenous population of Leicester, 1972–1989. Gut. 1992;33:1085–1088. doi: 10.1136/gut.33.8.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen WS, Leu SY, Hsu H, Lin JK, Lin TC. Trend of large bowel tuberculosis and the relation with pulmonary tuberculosis. Dis Colon Rectum. 1992;35:189–192. doi: 10.1007/BF02050677. [DOI] [PubMed] [Google Scholar]
- Guth A, Kim U. The reappearence of abdominal tuberculosis. Surg Gynecol Obstet. 1991;172:432–436. [PubMed] [Google Scholar]
- Palmer KB, Patil DH, Basran GS, Riordan JF, Silk DB. Abdominal tuberculosis in urban Britain. A common disease. Gut. 1985;26:1296–1305. doi: 10.1136/gut.26.12.1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson JM, Gill ON. HIV infection and tuberculosis: Br Med J. 1990;300:63–65. doi: 10.1136/bmj.300.6717.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall JB. Tuberculosis of the gastrointestinal tract and peritoneum. Am J Gastroenterol. 1993;88:989–999. [PubMed] [Google Scholar]
- Snider Jr DE, Roper WL. The new tuberculosis. N Eng J Med. 1992;326:703–705. doi: 10.1056/NEJM199203053261011. [DOI] [PubMed] [Google Scholar]
- McGee GS, Williams LF, Potts J, Barnwell S, Sawyers JL. Gastrointestinal tuberculosis: resurgence of an old pathogen. Am Surg. 1989;55:16–20. [PubMed] [Google Scholar]
- Arnold C, Moradpour D, Blum HE. Tuberculous colitis mimicking Crohn's disease. Am J Gastroenterol. 1998;11:2294–2296. doi: 10.1016/S0002-9270(98)00525-5. [DOI] [PubMed] [Google Scholar]
- Kaushik SP, Bassett ML, McDonald C, Lin BP, Bokey EL. Case report: gastrointestinal tuberculosis simulating Crohn's disease. J Gastroenterol Hepatol. 1996;11:532–534. doi: 10.1111/j.1440-1746.1996.tb01697.x. [DOI] [PubMed] [Google Scholar]
- Klimach OE, Ormerod LP. Gastrointestinal tuberculosis: A retrospective review of 109 cases in a district general hospital. Q J Med. 1985;56:569–78. [PubMed] [Google Scholar]
- Sherman S, Rohwedder JJ, Ravikrishann KP, Weg JG. Tuberculous enteritis and peritonitis. Report of 36 general hospital cases. Arch Intern Med. 1980;140:506–508. doi: 10.1001/archinte.140.4.506. [DOI] [PubMed] [Google Scholar]
- Jakubowski A, Elwood RK, Enarson DA. Clinical features of abdominal tuberculosis. J Infect Dis. 1988;158:687–692. doi: 10.1093/infdis/158.4.687. [DOI] [PubMed] [Google Scholar]
- Shah S, Thomas V, Mathan M, Chacko A, Chandy G, Ramakrishna BS, Rolston DDK. Colonoscopic study of 50 patients with colonic tuberculosis. Gut. 1992;33:347–351. doi: 10.1136/gut.33.3.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Karawi MA, Mohamed AE, Yasawy ML, Graham DY, Shariq S, Ahmed AM, Al Jumah A, Ghandour Z. Protean manifestations of gastrointestinal tuberculosis. Report of 130 patients. J Clin Gastroenterol. 1995;20:225–232. doi: 10.1097/00004836-199504000-00013. [DOI] [PubMed] [Google Scholar]
- Misra SP, Misra V, Dwivedi M, Gupta SC. Colonic tuberculosis: clinical features, endoscopic appearance and management. J Gastroenterol Hepatol. 1999;14:723–729. doi: 10.1046/j.1440-1746.1999.01940.x. [DOI] [PubMed] [Google Scholar]
- Anand BS, Schneider FE, El-Zaatari FAK, Shawar RM, Clarridge JE, Graham DY. Diagnosis of intestinal tuberculosis by polymerase chain reaction on endoscopic biopsy specimens. Am J Gastroenterol. 1994;89:2248–2249. [PubMed] [Google Scholar]
- Bhargava DK, Dasarathy S, Shriniwas MD, Kushwaha AK, Duphare H, Kapur BM. Evaluation of enzyme-linked immunosorbent assay using mycobacterial saline-extracted antigen for the serodiagnosis of abdominal tuberculosis. Am J Gastroenterol. 1992;87:105–108. [PubMed] [Google Scholar]
- Balthazar EJ, Gordon R, Hulnick D. Ileocecal tuberculosis: CT and radiologic evaluation. Am J Roentgenol. 1990;154:499–503. doi: 10.2214/ajr.154.3.2106212. [DOI] [PubMed] [Google Scholar]
- Ferentzi CV, Sieck JO, Ali MA. Colonoscopic diagnosis and medical treatment of ten patients with colonic tuberculosis. Endoscopy. 1988;20:62–65. doi: 10.1055/s-2007-1018132. [DOI] [PubMed] [Google Scholar]
- Boudiaf M, Zidi SH, Soyer P, Lavergne-Slove A, Kardache M, Logeay O, Rymer R. Tuberculous colitis mimicking Crohn's disease: utility of computed tomography in the differentiation. Eur Radiol. 1998;8:1221–1223. doi: 10.1007/s003300050539. [DOI] [PubMed] [Google Scholar]


