Abstract
Background
Prenatal care provides pregnant women with repeated opportunities for prevention, screening and diagnosis that have no current extension to future fathers. It also contributes to women’s general better access to health. The goal of PARTAGE study was to evaluate the level and determinants of adherence to a prenatal prevention consultation dedicated to men.
Methods
Between January 2021 and April 2022, we conducted a monocentric interventional study in Montreuil hospital. We assessed the acceptance of a prenatal prevention consultation newly offered to every future father, through their pregnant partner’s prior consent to provide their contact details.
Results
Three thousand thirty-eight women provided contact information used to reach the fathers; effective contact was established with 2,516 men, of whom 1,333 (53%) came for prenatal prevention consultation. Immigrant men were more likely to come than French-born men (56% versus 49%, p < 0·001), and the more they faced social hardship, the more likely they were to accept the offer. In multivariate analysis, men born in Subsaharan Africa and Asia were twice as likely to attend the consultation as those born in Europe or North America.
Conclusion
Acceptance of this new offer was high. Moreover, this consultation was perceived by vulnerable immigrant men as an opportunity to integrate a healthcare system they would have otherwise remained deprived of.
Trial registration
Registry: ClinicalTrials.gov, US National Library of Medicine https://classic.clinicaltrials.gov/ct2/show/NCT05085717
Clinical Trial number: NCT05085717.
Date of registration: 20/10/2021.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-20388-x.
Keywords: Social inequalities in health, Migrants health, Prenatal health, Gender inequalities, HIV, Sexually transmitted infections, Vaccination, Health insurance coverage
Introduction
Gynecological care: an opportunity for prevention, screening and health improvement
Worldwide, men have less contact with the healthcare system [1] and seek primary care less offen than women [2–4]. One reason is that gynecological care (contraception, pregnancy, cervical cancer prevention) makes women used to meeting healthcare professionals regularly, even in absence of any disease [5].
Most countries recommend regular medical check-ups and biological monitoring during pregnancy. When the father’s health is taken into the picture, this is to avoid genetic or infectious transmission rather than keeping the father himself in good health [6]. Even then, infectious diseases are poorly screened in the second parent: HIV diagnosis is delayed in heterosexual men compared to women, because male partner uptake of HIV testing during antenatal care remains scarce [7], despite numerous initiatives to promote it [8–12].
Prenatal visits are also used to encourage behavioral changes in pregnant women, such as smoking and alcoholic withdrawal, promoting physical exercise and combating obesity [13, 14]. To date, men do not have such opportunities. Yet, involving their partner supports behavioral changes in pregnant women [15]. In addition, important health needs were identified in a cohort of future fathers [16] and fatherhood is a high-risk period for depression in men [17, 18].
Expecting a child could therefore be an opportunity to offer men a consultation designed to protect the mother and the foetus from transmissible diseases, but also to improve or preserve their own health [19].
The French context and the Seine Saint Denis specific situation
In France, seven medical visits are scheduled during pregnancy. The prenatal HIV screening strategy is highly effective in women, with at least 97% of them tested at every pregnancy [20]. Systematic HIV screening is also recommended for fathers [21], yet not performed: between 2017 and 2020, among 567 fathers surveyed, only 3% knew a man who had been tested for HIV in connection with his partner’s pregnancy [22].
The French health insurance scheme mentions the possibility of a medical examination for the father. However, there are no guidelines for reimbursing this consultation or the biological tests that would be prescribed during it: paternal prenatal consultation is therefore not currently practiced.
Seine Saint-Denis (population; 1.6 million inhabitants), located in the northeastern suburbs of Paris (Ile de France region), is the department with the highest rates of immigration and poverty in mainland France [23]. As elsewhere in Europe, most immigrants arrive in better health than the general population (“healthy immigrant effect”), before their health deteriorates faster and more than the natives’ one throughout their stay (“unhealthy convergent effect”) [24]. Although access to healthcare is theoretically universal in France, with a system called Aide Médicale de l’Etat (State Medical Aid) allowing illegal immigrants with proof of a continuous presence of at least three months in the country to access the healthcare system, nearly half of illegal migrants don’t get this health coverage due to lack of adequate information, with a lower rate of take-up among men [25]. Immigrants are also disproportionately affected by social vulnerability, especially in the years following their arrival: the median time to obtain a basic security package (residence permit, housing, income-generating activity) for immigrants from sub-Saharan Africa was estimated to 7 years in Paris area [26]. Lack of housing or residence permit is associated to deteriorated health, and to exposition to sexual risks and infections [27]. Recent French recommendations on vaccination catch up [28] and on health check-up [29] for newly arrived immigrants should be fully implemented in our setting, which raises the question of how to reach those populations effectively.
Montreuil (111 000 inhabitants) hospital maternity ward provides prenatal care for some 3,500 women every year. In 2020–2021, 4·6% of women who gave birth in Montreuil were immigrants with < 12 months’ residence in France [30]. Among all women who delivered in Montreuil hospital over the same period, 52% were later identified as socially vulnerable, 41% of them being born in Subsaharan Africa and 11% in Asia [31].
In this maternity where poverty and immigration prevail, a Personalized Pregnancy Follow Up Unit has been implemented so that the most vulnerable pregnant women receive early reinforced multidisciplinary care [31]. However, their partners, and adult men in general, hardly ever get targetted by interventions aimed at reducing social inequalities in health. We seized the symbolic opportunity of parenthood to offer future fathers a free prenatal consultation. PARTAGE was an interventional study: intervention consisted in a prenatal consultation dedicated to the male partners of all women attending antenatal care in our clinic. Acceptability of this intervention was assessed, with the final aim of transferring it to routine practice. The primary endpoint of PARTAGE study was the proportion of men contacted who actually attended the prenatal consultation offered to them. The results presented in this article focus on this main objective: the acceptance rate and the socio-demographic factors associated with this acceptance.
Methods
PARTAGE (« Prévention, Accès aux droits, Rattrapage vaccinal, Traitement des Affections pendant la Grossesse et pour l’Enfant») was a monocentric interventional research without control arm assesssing for 15 months (January 2021-April 2022) the acceptability of a new prenatal prevention consultation offered through the pregnant women to all future fathers in Montreuil’s hospital.
Study population
Eligible women were 18 and older pregnant women attending a first prenatal consultation at Montreuil hospital during the study period, reporting a male partner positively involved in the pregnancy.
Eligible men were those designated by the participating woman as the father, provided they lived in Ile-de-France region. To make it simple, « men», « partners» or « fathers» all refer to them.
Intervention
The interview was integrated into the women’s maternity trajectory. Trained interviewers offered eligible women to respond to a face-to-face questionnaire that included their sociodemographic and marital characteristics (maternal questionnaire, MQ, Additional file 1). Women were asked to provide the future father’s contact details. When the father was present, the project was presented directly to the couple and the consultation appointment could be made immediately. Several time slots were open for unscheduled consultations: if the couple met the interviewers during those slots, the father could choose to attend the prenatal consultation straight away.
An information letter was given to all eligible pregnant women. An e-mail was sent to men for whom an e-mail address was provided, with an online appointment platform link and dedicated phone-line and e-mail address to schedule consultation. Fathers who did not reply were called by a research midwife and offered an appointment either during the day or in the evening, on weekdays or Saturday, at the hospital or in the city center, within easy reach of public transportation.
Fathers received a text reminder before appointment. If they failed to attend, they were systematically called again and given the option of either refusing the consultation (their reason for refusal was then collected and they were not called again) or rescheduling and being called again in case of another missed appointment.
Fathers were seen by a doctor or midwife. Blood pressure was measured, clinical examination was carried out if needed, biological tests were adapted to individual’s exposure and medical history. Vaccines were updated; fathers lacking health insurance coverage met a social worker to obtain it. Test results were delivered face to face, by telephone or by e-mail, according to men’s choice. Depending on their needs, men were referred to a health mediator, a psychologist, a general practioner or any hospital specialist. The full protocol and details on the study are available [32, 33].
Ethics
The French Data Protection Authority (CNIL, registration number 921135) and the French Personnal Data Protection Comittee (Comite de Protection des Personnes, registation number 21.01.19.44753 amended by 21.05022.944753 decision, allowing and increased number of inclusions and additional data collection) gave full ethical approval.
Statistical analysis
Women’s own sociodemographic characteristics, their partners’ ones as well as data on the couple (length of relationship, previous children, type of union, communication about sexually transmitted infections and previous screening) were collected in maternal questionnaire. In addition to the general sociodemographic data; variables exclusively or particularly related to immigrant status were collected (main reason for women’s migration, length of stay, permit of residence, housing conditions, health insurance coverage).
Data were compared between fathers who attended the prenatal prevention consultation and those who did not, using Chi [2] or Fisher exact tests for categorical variables and Student’s or Wilcoxon rank sum tests for quantitative variables, as appropriate. All tests were two-sided with p-values < 0·05 defined as statistically significant. Multivariate logistic regression models were built to identify the factors associated with men’s take-up of this offer, based on their own characteristics on one hand, and on their pregnant partner’s as well as the couple’s characteristics on the other hand, in the general study population, and then in the sub-groups of immigrant men and women. Backward elimination procedures were used to determine the final models. Given the limited number of missing data, no imputation was performed, in order to avoid introducing bias. Incomplete observations were removed from the multivariate models. Analyses were performed in Stata SE 17 (Stata Corporation, College Station, TX, USA).
Results
Acceptance rate and characteristics of the studied population
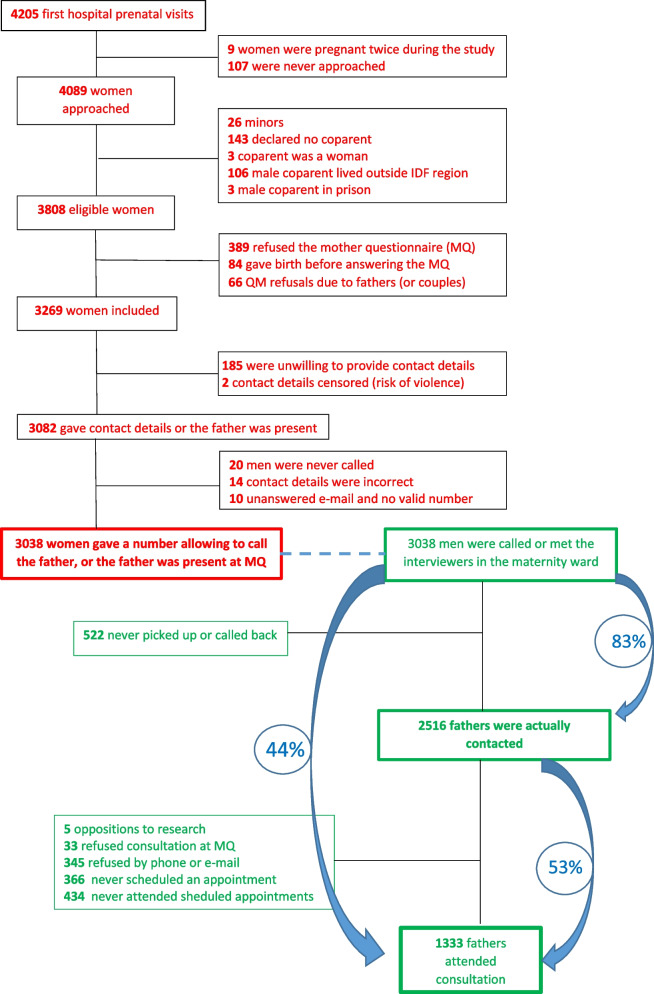
Among 4205 women with first hospital prenatal visit during the study period, 3808 were eligible, 3038 provided effective contact details wich enabled the research team to contact their partner. Contact was actually made (face-to-face, by phone or via message exchange) with 2516 men (83%), of whom 1333 (53%) eventually attended father’s prenatal prevention consultation (FPPC) (Fig. 1).
Fig. 1.
Study flow chart, Montreuil (France) 2021–2022
Regarding women: their median age was 31 years, interquartile range 28–35 years. One third was expecting a first child; 49% had a university degree, whereas 46% were unemployed prior to current pregnancy; 13% believed they had never been tested for HIV, while 15% identified their ongoing pregnancy serology as their first. Only 36% recalled a couple’s discussion about HIV or sexually transmitted infections (STIs), and 56% didn’t know if their partner had ever been tested for HIV. 78% predicted that the future father would attend the prenatal consultation he would be offered.
Fifty-two percent were immigrants, most often from Subsaharan Africa (20%), North Africa or the Middle East (18%). Among the immigrant women (N = 1590): 51% had been in France for less than 7 years, the median time to achieve a basic level of installation [26]; 9% had no residence permit and 9% no health insurance coverage. Two-thirds had come to France to join either their husbands (43%) or a family member (26%), while 17% had come to seek a better life, 8% to study, 6% to escape threats or violence, and only 0.7% for health reasons.
Regarding men: Their median age was 35 (IQR30-40 years); 35% had been to university, 14% were unemployed. Fifty-nine percent of those with whom contact had been established were immigrants (N = 1490): 25% came from Subsaharan Africa, 19% from North Africa or the Middle East. Only 29% had been in France for less than 7 years, 18% had no residence permit, and 11% had no health insurance coverage. Only 11% have themselves taken the step of making an appointment, while 78% responded to requests from the research team, generally (57%) midwives’ phone calls. The use of unscheduled consultations remained marginal (1.6%) (Table 1).
Table 1.
Characteristics of the study population, Montreuil (France) 2021-2022
| Women who gave effective contact information | Men who were actually contacted | |||
|---|---|---|---|---|
| N | % or [IQR] | N | % or [IQR] | |
| Sociodemographic characteristics | ||||
| Population size | 3038 | 100% | 2516 | 100% |
| Of which foreign-born | 1590 | 52·3% | 1490 | 59·2% |
| Age (years) | 31 | [28-35] | 35 | [30-40] |
| [18-24] | 345 | 11·3% | 116 | 4·6% |
| [25-29] | 897 | 29·5% | 391 | 15·5% |
| [30-34] | 1029 | 33·9% | 744 | 29·6% |
| [35-39] | 604 | 19·9% | 609 | 24·2% |
| 40 and over | 163 | 5·4% | 656 | 26·1% |
| Region of birth | ||||
| Mainland France | 1401 | 46·1% | 986 | 39·2% |
| French overseas departments and territories | 47 | 1·5% | 40 | 1·6% |
| European Union and United Kingdom (EU-UK) | 126 | 4·1% | 95 | 3·8% |
| Subsaharan Africa | 603 | 19·9% | 633 | 25·1% |
| Asia | 143 | 4·7% | 152 | 6·0% |
| North Africa and Middle East | 555 | 18·3% | 480 | 19·1% |
| Latin America and the Caribbean | 70 | 2·3% | 60 | 2·4% |
| Non EU-UK Europe, North America, Australia | 93 | 3·1% | 70 | 2·8% |
| Length of residence in France (for foreign-born)a | ||||
| < 7 years | 818 | 51·5% | 413 | 28·7% |
| >=7 years | 769 | 48·5% | 1024 | 71·3% |
| Main reason for coming to France (in foreign-born)b,c | ||||
| Find a job, seek a better life | 263 | 16·6% | ||
| Join her husband | 678 | 42·8% | ||
| Join another member of the family | 412 | 26·0% | ||
| Study | 129 | 8·1% | ||
| Threatened in her country | 92 | 5·8% | ||
| Disease | 11 | 0·7% | ||
| Education leveld | ||||
| None/Primary or koranic school | 272 | 9·0% | 283 | 11·6% |
| Secondary | 1274 | 42·0% | 1301 | 53·1% |
| University | 1483 | 49·0% | 864 | 35·3% |
| Living conditions | ||||
| Administrative statuse | ||||
| French nationality | 1713 | 56·4% | 1350 | 53·7% |
| Regular EU status | 182 | 6·0% | 158 | 6·3% |
| 10 years residence card | 420 | 13·8% | 439 | 17·5% |
| >= 1 year residence permit | 314 | 10·3% | 256 | 10·2% |
| < 1 year residence permit or receipt | 103 | 3·4% | 40 | 1·6% |
| No residence permit | 306 | 10·1% | 270 | 10·7% |
| Health insurance coveragef | ||||
| No | 145 | 4·8% | 161 | 6·5% |
| State Medical Assistance (SMA) | 200 | 6·6% | 124 | 5·0% |
| Basic Health Insurance | 262 | 8·6% | 278 | 11·1% |
| Complete Health Insurance | 2431 | 80·0% | 1933 | 77·4% |
| Housing conditionsb,g | ||||
| Personal housing (owner or tenant, including social lease) | 2573 | 84·8% | ||
| Hosted by family | 324 | 10·7% | ||
| Hosted by associations | 19 | 0·6% | ||
| Hosted in residence for asylum seekers or migrant hostel | 25 | 0·8% | ||
| No housing or overnight stay in social hostel | 95 | 3·1% | ||
| Employment status (excluding the pregnancy period for women)h | ||||
| Non-precarious employment | 1376 | 45·3% | 1664 | 66·9% |
| Precarious employment | 147 | 4·8% | 433 | 17·4% |
| Education or training | 90 | 3·0% | 30 | 1·2% |
| Parental leave | 39 | 1·3% | 0 | 0% |
| Unemployment | 1385 | 45·6% | 360 | 14·5% |
| Couple’s characteristics | ||||
| Marital statusi | ||||
| No formal union | 842 | 27·8% | ||
| Civil, religious or traditional formal union | 2190 | 72·2% | ||
| Cohabitationj | ||||
| No or not really | 271 | 8·9% | ||
| Yes | 2763 | 91·1% | ||
| Couple durationk | ||||
| Not really together | 27 | 0·9% | ||
| < 1 year | 120 | 4·0% | ||
| 1-3 years | 622 | 20·6% | ||
| 4-10 years | 1445 | 48·0% | ||
| Over 10 years | 799 | 26·5% | ||
| Children already born | ||||
| Woman’s first child | 1016 | 33·4% | ||
| The woman has children but only with other father(s) | 190 | 6·3% | ||
| The couple already have children | 1832 | 60·3% | ||
| Couple discussion about HIV and STIsl | ||||
| Never, or the mother doesn't remember | 1933 | 64·2% | ||
| Yes | 1076 | 35·8% | ||
| Woman's knowledge of having been screened for HIVm | ||||
| Never screened or doesn't know | 397 | 13·2% | ||
| Screened before current pregnancy | 2167 | 71·8% | ||
| First screening during this pregnancy | 452 | 15·0% | ||
| Woman’s knowledge of father's possible HIV testn | ||||
| Never screened or doesn't know | 1686 | 55·9% | ||
| Already screened | 1330 | 44·1% | ||
| Woman's prognosis of father's attendanceo | ||||
| Thinks he won’t attend FPPC | 166 | 5·5% | ||
| Doesn't know if he will | 490 | 16·2% | ||
| Thinks he will attend | 2376 | 78·4% | ||
Data are n (%) or median [interquartile range]
aData missing for 3 women and 53 men
bData only collected for women
cData missing for 5 women
dData missing for 9 women and 68 men
eData missing for 3 men
fData missing for 20 men
gData missing for 2 women
hData missing for 1 woman and 29 men
iData missing for 6 couples
jData missing for 4 couples
kData missing for 25 couples
lData missing for 29 couples
m22 women did not respond
n22 women did not respond
o6 women did not respond
Characteristics of women whose partner accepted the offer
Comparison of women whose partner came to the consultation with women whose partner did not
Partners of primipara were more likely to come than those of women who were already mothers, especially if the couple already had children together (53% versus 38%, p < 0.001).
Partners of women born in Subsaharan Africa, Asia and Latin America-Haiti took up the offer better than those born in France (56%, 62% and 50%, respectively, versus 38%%, p < 0.001).
Partners of women in precarious situations (homeless, with SMA or no health insurance coverage) came more often than those of women living in their own homes or registered with the general health insurance scheme.
Partners of women declaring a first HIV serology during the current pregnancy were more likely to take up the offer than those of women who were unaware of having been tested, and those who had been tested prior to the current pregnancy (50% versus 46% and 42%, respectively, p = 0,004).
Half of men whose partner predicted they would take up the offer actually came, versus 22% of those whose partner were uncertain, and 13% of those whose partner predicted that refusal (p < 0.001, Table 2).
Table 2.
Women’s characteristics by partner's attendance to father prenatal prevention consultation, Montreuil (France) 2021-2022 (N = 3038 partners called or met)
| Women whose partner came (N = 1333) | Women whose partner did not come (N = 1705) | P-value | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Agea | |||||
| [18-24 years] | 153 | 44·3% | 192 | 55·7% | 0·531 |
| [25-29 years] | 376 | 41·9% | 521 | 58·1% | |
| [30-34 years] | 456 | 44·3% | 573 | 55·7% | |
| 35 and over | 348 | 45·4 % | 419 | 54·6% | |
| Region of birth | |||||
| France | 557 | 38·5% | 891 | 61·5% | <0·001 |
| UE 27-UK | 54 | 42·9% | 72 | 57·1% | |
| Europe non-EU 27-UK, North America, Australia | 39 | 41·9% | 54 | 58·1% | |
| North Africa and Middle East | 221 | 39.8% | 334 | 60.2% | |
| Subsaharan Africa | 338 | 56.0% | 265 | 44.0% | |
| Asia | 89 | 62.2% | 54 | 37.8% | |
| Latin America and the Caribbean | 35 | 50.0% | 35 | 50.0% | |
| Length of residence in Franceb | |||||
| < 7 years | 443 | 54·2% | 374 | 45·8% | <0·001 |
| >= 7 years | 331 | 43·1% | 437 | 56·9% | |
| Born in France | 557 | 38·5% | 891 | 61·5% | |
| Main reason for migration | |||||
| Not applicable (born in France) | 557 | 38·5% | 890 | 61·5% | <0·001 |
| Find a job, seek a better life | 150 | 57·0% | 113 | 43·0% | |
| Join someone (family, husband) or study | 553 | 45·3% | 667 | 54·7% | |
| Disease or threated in her country | 71 | 68·9% | 32 | 31·1% | |
| Education level | |||||
| None/ Primary or koranic school | 153 | 56·2% | 119 | 43·8% | <0.001 |
| Secondary | 497 | 39·0% | 777 | 61·0% | |
| University | 679 | 45·8% | 804 | 54·2% | |
| Administrative status | |||||
| French nationality | 674 | 39·3% | 1039 | 60·7% | <0·001 |
| Regular EU status | 83 | 45·6% | 99 | 54·4% | |
| 10-year residence card | 185 | 44·0% | 235 | 56·0% | |
| Residence permit 1 year or more | 156 | 49·7% | 158 | 30·3% | |
| < 1 year residence permit or receipt | 52 | 50·5% | 51 | 49·5% | |
| No residence permit | 183 | 59·8% | 123 | 40·2% | |
| Health insurance coverage | |||||
| No | 79 | 54·5% | 66 | 45·5% | <0·001 |
| State Medical Assistance | 116 | 58·0% | 84 | 42·0% | |
| Basic Health Insurance only | 96 | 36·6% | 166 | 63·4% | |
| Complete Health Insurance | 1042 | 42·9% | 1389 | 57·1% | |
| Employment status (excluding the pregnancy period) | |||||
| Precarious employment, student, in training | 123 | 51·2% | 117 | 48·8% | 0·056 |
| Non-precarious employment | 598 | 43·5% | 778 | 56·5% | |
| Unemployment or on parental leave | 612 | 43·1% | 809 | 56·9% | |
| Housing conditions | |||||
| Personal housing | 1090 | 42·4% | 1483 | 57·6% | <0·001 |
| Hosted (family, association) | 173 | 47·0% | 195 | 53·0% | |
| No housing or overnight stay in social hostel | 70 | 73·7% | 25 | 26·3% | |
| Couple duration | |||||
| Not really together | 10 | 37·0% | 17 | 63·0% | <0·001 |
| < 1 year | 67 | 55·8% | 53 | 44·2% | |
| 1-3 years | 306 | 49·2% | 316 | 50·8% | |
| 4-10 years | 638 | 44·1% | 807 | 55·9% | |
| Over 10 years | 312 | 39·0% | 487 | 91·0% | |
| Children already born | |||||
| No | 536 | 52·8% | 480 | 47·2% | <0·001 |
| Yes, including children with the same father | 703 | 38·4% | 1129 | 61·6% | |
| Yes, but only with other father(s) | 94 | 49·5% | 96 | 50·5% | |
| Have you had an HIV test? | |||||
| No or I don't think so | 182 | 45·8% | 215 | 54·2% | 0·004 |
| Yes, even before the current pregnancy | 914 | 42·2% | 1253 | 57·8% | |
| Yes, only during this pregnancy | 228 | 50·4% | 224 | 49·6% | |
| Have you ever talked about HIV/STIs with your partner? | |||||
| No or I don't know | 858 | 44·4% | 1075 | 55·6% | 0·472 |
| Yes | 463 | 43·0% | 613 | 57·0% | |
| Do you think he will accept FPPC? | |||||
| No | 22 | 13·2% | 144 | 86·8% | <0·001 |
| I don't know | 108 | 22·0% | 382 | 78·0% | |
| Yes | 1200 | 50·5% | 1176 | 49·5% | |
aCohabitation with the father, marital status, women’s knowledge of father’s HIV status and of any HIV performed by the father were also analyzed, with no difference between groups. A complete comparison of women's characteristics is provided as additional file 2
bWhen the sum of the category headcounts does not correspond to the total headcount, there are missing data (see Table 1)
Women’s characteristics associated with their partners’ attendance
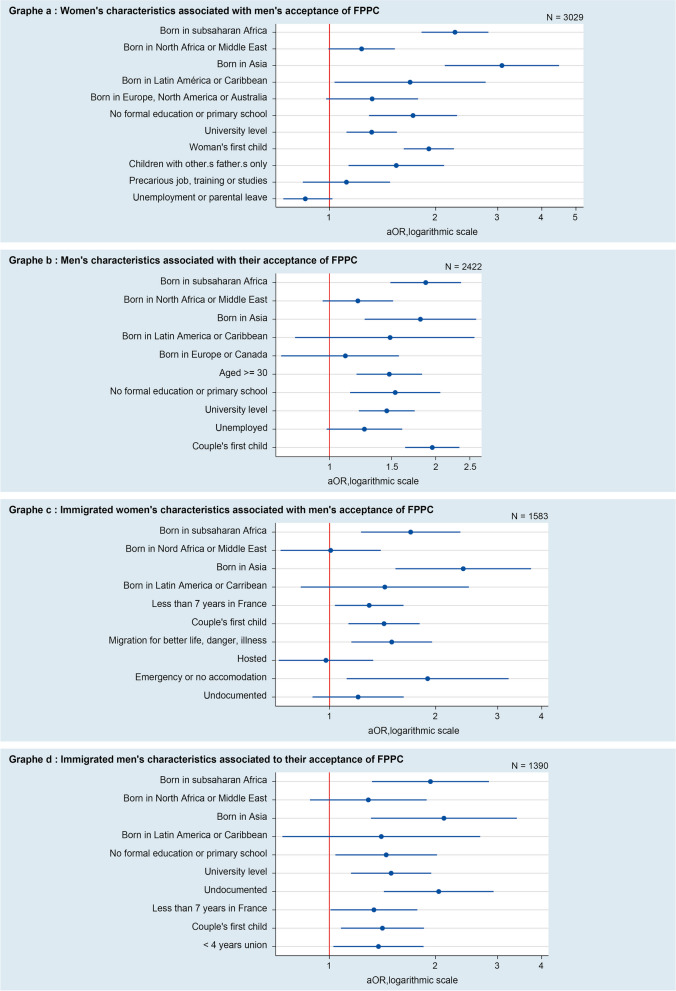
After adjusting for other women’s characteristics, those born in Subsaharan Africa (OR 2.23 [1.79–2.78]), Asia (OR 3.14 [2.15–4.59]) or Latin America-Haiti (OR 1.71 [1.04–2.82]) were more likely to have their partner attending than those born in France. Women’s level of education remained associated with their partners’ attendance: partners of women with a low level of formal education (no or only elementary school) or, on the contrary, a high level of formal education (university degree) came more often than those of women with a high school level (Fig. 2, graph a).
Fig. 2.
Women’s and men’s characteristics associated with men’s acceptance of Father’s Prenatal Prevention Consultation (FPPC), Montreuil (France), 2021–20221
1Reference groups in graph a are: France for region of birth, secondary school for education level, couple with children for parity, non precarious job for employment; graph b: France for region of birth, secondary school for education level, <30 for age, any job for employment, couple with children for parity, >= 4 years for union’s duration; graph c: Europe/North America/Australia for region of birth, secondary school for education level, >= 7 years for length of stay, study/join someone for main reason for coming to France, regular situation for administrative status, personal house for housing conditions, couple with children for parity; graph d: Europe/North America for region of birth, secondary school for education level, >= 7 years for length of stay, regular situation for administrative status, couple with children for parity. For logistic regressions, see Additional file 3
Characteristics of the immigrant women sub-population associated with their partner's attendance
In multivariate analysis, partners of women born Subsaharan Africa and Asia made greater use of this new consultation than those of women from Europe, USA or Australia, even after adjustment for length of stay, reason for migration, housing, administrative status and parenthood (OR 1.61 [1.16–2.23] and OR 2.35 [1.50–3.68], respectively). Homelessness, migration for their own safety or to seek a better life, and a residence period of less than seven years were independently associated with the partner’s attendance (Fig. 2, graph c).
Characteristics of men who took up the offer
Comparison of men who came to the consultation versus those who did not
Participation was higher among men aged 30 and over than among younger ones, and among Subsaharan African, Asian and Latin American-Haitian immigrants than among French-born men (49% versus 61%, 63% and 53% respectively). Immigrants present for less than 7 years came more often than those who had been in France for longer (66% versus 55%, p < 0.001). As for women, men with social vulnerabilities (no residence permit, no affiliation to the general health insurance scheme) made greater use of consultations than less precarious ones. The uptake rate was lower among men with a secondary level of education than among men with a lower or higher level of education (49% versus 63% and 59%, respectively, p < 0.001), and a similar trend was observed with regard to women’s level of education. Finally, the proportion of adherence was similar whether or not men had any medical follow-up (53% versus 47%, p = 609, Table 3).
Table 3.
Men’s characteristics by attendance to father prenatal prevention consultation, Montreuil (France) 2021-2022 (N = 2516 men actually contacted)
|
Men who attended (N = 1333) |
Men who did not attend despite effective contact (N = 1183) |
P-value | |||
|---|---|---|---|---|---|
| Agea | |||||
| [18-29 years] | 238 | 46·9% | 269 | 53·1% | 0·009 |
| [30-34 years] | 402 | 54·0% | 342 | 46·0% | |
| 35 and over | 693 | 54·8% | 571 | 45·2% | |
| Region of birth | |||||
| France | 500 | 48·7% | 526 | 51·3% | <0·001 |
| EU 27 | 42 | 44·2% | 53 | 55·6% | |
| Non-EU 27 Europe, Canada | 32 | 45·7% | 38 | 54·3% | |
| North Africa and Middle East | 245 | 51·0% | 235 | 49·0% | |
| Subsaharan Africa | 386 | 61·0% | 247 | 39·0% | |
| Asia | 96 | 63·2% | 56 | 36·8% | |
| Latin America and the Caribbean | 32 | 53·3% | 28 | 46·7% | |
| Length of residence in France | |||||
| < 7 years | 274 | 66·3% | 139 | 33·7% | <0·001 |
| >= 7 years | 559 | 54·6% | 465 | 45·4% | |
| Born in France | 500 | 48·7% | 526 | 51·3% | |
| Administrative status | |||||
| French nationality | 679 | 50·3% | 671 | 49·7% | <0·001 |
| Regular EU status | 75 | 47·5% | 83 | 52·5% | |
| 10-year residence card | 217 | 49·4% | 222 | 50·6% | |
| >= 1 year residence permit | 143 | 55·9% | 113 | 44·1% | |
| Residence permit < 1 year or receipt | 23 | 57·5% | 17 | 42·5% | |
| No residence permit | 196 | 72·6% | 74 | 27·4% | |
| Health insurance coverage | |||||
| No | 106 | 65·8% | 55 | 34·2% | <0·001 |
| State Medical Assistance (SMA) | 88 | 71·0% | 36 | 29·0% | |
| Basic Health Insurance | 118 | 42·5% | 160 | 57·5% | |
| Complete Health Insurance | 1021 | 52·8% | 912 | 47·2% | |
| Employment status | |||||
| Precarious employment, student, in training | 247 | 53·4% | 216 | 46·6% | 0·052 |
| Non-precarious employment | 872 | 52·4% | 792 | 47·6% | |
| Unemployment | 214 | 59·4% | 146 | 40·6% | |
| Level of education | |||||
| None, primary or koranic school | 179 | 63·3% | 104 | 36·7% | <0·001 |
| Secondary | 641 | 49·3% | 660 | 50·7% | |
| University | 512 | 59·3% | 352 | 40·7% | |
| Other children with the same mother | |||||
| No | 629 | 60·7% | 407 | 39·3% | <0·001 |
| Yes | 704 | 47·6% | 776 | 52·4% | |
| Integration into the healthcare system | |||||
| Rarely or never in contact with a physician | 458 | 53·8% | 394 | 46·2% | 0·609 |
| Has a primary care physician or chronic disease follow-up | 875 | 52·7% | 786 | 47·3% | |
aWhen the sum of the category headcounts does not correspond to the total headcount, there is missing data (see Table 1)
Men’s characteristics associated with their attendance
After adjustment for other men’s characteristrics, father attendance remained strongly associated with the couple’s expecting a first child (odds Ratio [OR] 2.00 95% confidence interval [95% CI] 1·67–2·40, p < 0·001) and with the father’s being born abroad (Subsaharan Africa OR 1·83 95% CI 1·45–2·31, Asia OR 1·82 95% IC 1·26–2·63, Fig. 2, graph a).
Men aged 30 and over remained more receptive to the offer than younger men. The same U-shaped curve was observed for educational level: men with little or no schooling and men with higher education were more likely to seek advice than men who had studied up to secondary school. In the overall study population, compliance was higher in men aged 30 and over than in younger ones (Fig. 2, graph b).
Immigrated men’s characteristics associated with their attendance
In multivariate analysis, immigrants from Subsaharan Africa and Asia attended more than those from Europe or North America (OR 1.96 [1.33–2.88] and OR 2.06 [1.28–3.34], respectively), while paternal age was no longer associated with the acceptance rate. Immigrant men involved in a recent relationship came more often than those in a longer relationship (Fig. 2, graph d).
After adjustment for other precariousness criteria including country of origin, healthcare coverage, length of stay and employment, undocumented fathers remained more likely to attend than fathers with residence permit (OR 2·41, 95% CI 1·80–3·22 in the complete multivariate model and OR 1·93, 95% CI 1·34–2·77 in the final model, additional file 3).
Discussion
Our main findings were a high level of acceptance by men, though lower than the women’s predictions (78% thought their partner would come). Acceptance was higher among immigrants, especially the most precarious ones.
A high participation rate, based on a proactive approach
The participation rate was 44% based on the target population and 53% based on the men who actually had a contact with the research team. We did not find any similar published initiatives to compare our participation rates with. In 2011–2012, a British team offered HIV and Sexually Transmitted Infection (STI) testing to expectant fathers during obstetric ultrasounds examinations. The initiative led to an acceptance rate of 35%, but the coverage rate (18%) was limited by the study design, focusing the offer on the men attending ultrasounds with their partners [10]. While a letter given by PARTAGE interviewers to participating women, and a subsequent e-mail, instructed men on how to easily book their own appointments, the proactive approach of calling each eligible father one or more times or offering immediate appointment when they were present at the maternal questionnaire has been the main mode of recruitment for male consultation (78%). Earlier, proactive interventions also proved efficient in promoting HIV testing in future fathers, in different Subsaharan African settings: randomized controlled trials showed higher HIV test rates in future fathers when men received an invitation letter to attend the clinic [12], sometimes with an appointment already booked [34]. The highest recourse rates were obtained by caregivers’ home visits for immediate couple counselling and testing [35].
In an other field, that of cancer in high-income countries, as screening had been showed to be lower in immigrated and socially disvantaged populations [36, 37], proactive interventions have been built and assessed towards those publics: “Health navigators “call theirs targets on the phone, explain the screening, schedule appointments, assess lack of transportation, financial and insurance barriers [38]. The effectiveness of such programs in increasing screening rates has been demonstrated [39].
Overall, the proactive approach has been positively received by PARTAGE targeted men, particularly by immigrants in precarious situations, who have largely taken up the offer. However, we have always sought consent from pregnant women before contacting their partners, in order not to disempower them [40].
Although the association did not remain significant after adjustment, the partners of women who reported a first HIV test during the current pregnancy were more likely to come than those of women who were unaware of having been tested, and than those of women who had been tested previously. This finding supports the promotion of couple-oriented screening. However, using the symbolic occasion of childbirth to incite fathers to care for their own health would probably not be sufficient without this active outreach, as long as the social norm on both parent’s duties remains unchanged, with a gendered distribution of responsibilities that places women as guardians of children’s health [41, 42].
Immigrants were the most receptive to the offer, especially those with social vulnerabilities
Immigrant men took up the offer better than French-born men, particularly those from Subsaharan Africa and Asia. This differential acceptance persisted after adjustment to men’s social vulnerabilities. Therefore, the most precarious immigrants are the ones who came to the FPPC the most.
Yet the reduced flexibility of working hours for fathers in precarious employment has been identified as a potential obstacle to their attendance at classic antenatal visits [43], the availability issue was less frequently raised by socially vulnerable men than by well established ones (unshown data: reasons given by eligible fathers when refusing the offer). However, consultation schedules were deliberately extended to include evenings and weekends.
One possible explanation for immigrants’ greater attendance is their need to be helped in opening up health insurance rights: 7% of men had no health insurance coverage when surveyed, although French system theoretically covers nearly everyone. Another explanation could be greater uncovered healthcare needs in immigrants [44].
Surprisingly, while lack of health insurance coverage was associated with the use of consultations, having a medical follow-up was not. Number of French-born men with no social vulnerability did not have any medical follow up and did not attend FPPC. We may hypothesize that the reason why well-integrated men do not take up the offer is that they have the social skills to access the healthcare system, should a health problem occur. This hypothesis is supported by the finding of inequitable access to the healthcare system for immigrants in various European countries, including France [45].
Strengths and limitations
While most of the research published in the field has emphasised the importance of involving men in prenatal care in order to improve the health of the mother and the development of the child, this is, to our knowledge, the first structured healthcare intervention built in the perspective of improving fathers’ own health.
This survey has several limitations: research team’s outreach efforts towards the fathers, free and easy access to a multidisciplinary team, may not be replicable in routine clinical practice. Moreover, monocentric design limits the generalizability of the results. Given our context, marked by social insecurity and immigration, we reached men who may not have the same needs as the general population of fathers. We can, however, project that in areas where poverty prevails, the most disadvantaged men would seize a routine prenatal consultation as a point of entry into the health system.
Lastly, broader needs emerged during the study, including systematic mental health assessment. Another challenge is to adress men with preventive messages on various topics regarding child and family health: risk of domestic violence, overexposure to screens, diet, substance abuse. The burden of transmitting and applying those recommendations currently devolves largely onto women and could therefore be better shared. A male prenatal consultation including these new components is currently being implemented and assessed throughout Montreuil municipality (PARTAGE 2 project).
Conclusion
Although a prenatal consultation with biological tests is theoretically possible in France, it is not yet implemented. This study has shown that such consultation is well accepted when, for the first time, it is actually organized and offered. The men who make most use of it are immigrants with social vulnerabilities, and those who have been in France for less time. This consultation therefore appears as an opportunity for men facing administrative obstacles, or who do not have the social codes of the country they live in, to integrate into the healthcare system. Scaling up this intervention might thus reduce social inequalities in health. Consideration now needs to be given on how to make it available and free of charge in current practice.
Supplementary Information
Additional file 1. Maternal Questionnaire.
Additional file 2. Women's complete characteristics by partner's attendance.
Acknowledgements
The authors would like to thank all the people who participated in the study. The PARTAGE Study Group included, in addition to the authors: Anne-Laurence Doho, Patricia Obergfell, Djamila Gherbi, Emilie Daumergue, Anne Simon, Miguel de Sousa Mendes, Naima Osmani, Sandrine Dekens, Oumar Sissoko (ARCAT Association), Virginie Supervie, France Lert, Stéphanie Demarest, Ngone Diop.
We thank Christophe Michon, Nathalie Lydié, Joanna Orne-Gliemann, Laurent Mandelbrot, Corinne Taeron, Nicolas Derche, Gwenaelle Morvan, Bernadette Rwegera, Mélanie Jaunay, Ruth Foundje Notemi, Elisa Wardzala, Caroline Regnier, Paul Chalvin, Perrine Bonnefoy, Priscillia Ribouchon, Neima Sghiouar, Abdelkrim Imechket, Pauline Aubry, Francis Bouvier, David Benhammou, Andrainolo Ravalihasy, Karna Coulibaly, Guy Nielsen, the Montreuil Municipality, the Seine Saint Denis Departmental Council.
Abbreviations
- MQ
Maternal Questionnaire
- SMA
State Medical Assistance (Aide Médicale de l’Etat in French)
- FPPC
Father’s Prenatal Prevention Consultation
- CI
Confidence Interval
- OR
Odd Ratio
- GP
General Practitioner
Authors’ contributions
Conceptualization: PP, ADL, GJ, AG, TP. Data curation: PP, TP, RH, AG, GJ, CT, VAL. Formal analysis: PP, ADL. Funding Acquisition: PP, PEM. Investigation: VAL, CT, GJ, AG Methodology: PP, ADL. Project administration: PP, GJ, AG, PEM, BR.Software: TP. Supervision: ADL. Writing-original draft: PP, ADL. Manuscript revisions: PP, ADL
Funding
PARTAGE study was financed by the French Agency for research on AIDS, viral hepatitis, tuberculosis and emerging infectious diseases (ANRS-MIE) (research team’s salaries) and by the French Society against AIDS (SFLS), to implement and evaluate a Saturday consultation outside hospital walls. Montreuil’s hospital also received a donation from Gilead Sciences, Inc. to develop PARTAGE’s communication and IT tools.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
The French Data Protection Authority (CNIL, registration number 921135) and the French Personnal Data Protection Comittee (Comite de Protection des Personnes, registation number 21.01.19.44753 amended by 21.05022.944753 decision, allowing and increased number of inclusions and additional data collection) gave full ethical approval. Pregnant women and fathers-to-be included in the study gave their consent after being fully informed.
Consent for publication
Participants consent to publication is not required, as no identifying information is provided. All co-authors have reviewed and approved the submitted manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Pauline Penot, Email: pauline.penot@ght-gpne.fr.
the Partage Study Group:
Anne-Laurence Doho, Patricia Obergfell, Djamila Gherbi, Emilie Daumergue, Anne Simon, Miguel de Sousa Mendes, Naima Osmani, Sandrine Dekens, Oumar Sissoko, Virginie Supervie, France Lert, Stéphanie Demarest, and Ngone Diop
References
- 1.Greig A, Kimmel M, Lang J. Men, Masculinities & Development: Broadening Our Work Towards Gender Equality.2000.p. 22. (Gender in development monograph series). Report No.: 10. https://www.researchgate.net/publication/246771572_Men_Masculinities_Development_Broadening_Our_Work_Towards_Gender_Equality/link/572ad85708ae057b0a0797cd/download. Accessed 21 Aug 2023.
- 2.Institut national de la statistique et des études économiques, éditeur. Femmes et hommes, l’égalité en question. Éd. 2022. Montrouge: INSEE; 2022. (INSEE Références).
- 3.Sandman D, Simantov E, An C. Out of touch: American men and the health care system - Commonwealth Fund Men’s and Women’s Health Survey Findings. USA: The Commonwealth Fund; 2000. [Google Scholar]
- 4.Bertakis KD, Azari R, Helms LJ, Callahan EJ, Robbins JA. Gender differences in the utilization of health care services. J Fam Pract. 2000;49(2):147–52. [PubMed] [Google Scholar]
- 5.Koechlin A. La norme gynécologique: ce que la médecine fait au corps des femmes. Paris: Éditions Amsterdam; 2022. p. 305. [Google Scholar]
- 6.World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: World Health Organization; 2016. 152p. https://apps.who.int/iris/handle/10665/250796. Accessed 22 Aug 2023. [PubMed]
- 7.Dahl CM, Miller ES, Leziak K, Jackson J, Yee LM. Short Communication: Communication Between Pregnant Women and Male Partners About HIV Testing in the United States. AIDS Res Hum Retroviruses. 2021;37(9):683–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Desgrées-Du-Loû A, Brou H, Djohan G, Becquet R, Ekouevi DK, Zanou B, et al. Beneficial Effects of Offering Prenatal HIV Counselling and Testing on Developing a HIV Preventive Attitude among Couples. Abidjan, 2002–2005. AIDS Behav. 2009;13(2):348–55. [DOI] [PubMed] [Google Scholar]
- 9.Orne-Gliemann J, Balestre E, Tchendjou P, Miric M, Darak S, Butsashvili M, et al. Increasing HIV testing among male partners. AIDS Lond Engl. 2013;27(7):1167–77. [DOI] [PubMed] [Google Scholar]
- 10.Dhairyawan R, Creighton S, Sivyour L, Anderson J. Testing the fathers: carrying out HIV and STI tests on partners of pregnant women. Sex Transm Infect. 2012;88(3):184–6. [DOI] [PubMed] [Google Scholar]
- 11.Chanyalew H, Girma E, Birhane T, Chanie MG. Male partner involvement in HIV testing and counseling among partners of pregnant women in the Delanta District, Ethiopia. PLoS ONE. 2021;16(3): e0248436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mohlala BKF, Boily MC, Gregson S. The forgotten half of the equation: randomized controlled trial of a male invitation to attend couple voluntary counselling and testing. AIDS Lond Engl. 2011;25(12):1535–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McCloud MB. Health Behavior Change in Pregnant Women With Obesity. Nurs Womens Health. 2018;22(6):471–80. [DOI] [PubMed] [Google Scholar]
- 14.Anderson AE, Hure AJ, Powers JR, Kay-Lambkin FJ, Loxton DJ. Determinants of pregnant women’s compliance with alcohol guidelines: a prospective cohort study. BMC Public Health. 2012;12:777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martin LT, McNamara MJ, Milot AS, Halle T, Hair EC. The effects of father involvement during pregnancy on receipt of prenatal care and maternal smoking. Matern Child Health J. 2007;11(6):595–602. [DOI] [PubMed] [Google Scholar]
- 16.Kotelchuck M, Levy RA, Nadel HM. Voices of Fathers During Pregnancy: The MGH Prenatal Care Obstetrics Fatherhood Study Methods and Results. Matern Child Health J. 2022;26(8):1603–12. [DOI] [PubMed] [Google Scholar]
- 17.Gedzyk-Nieman SA. Postpartum and Paternal Postnatal Depression: Identification, Risks, and Resources. Nurs Clin North Am. 2021;56(3):325–43. [DOI] [PubMed] [Google Scholar]
- 18.Smythe KL, Petersen I, Schartau P. Prevalence of Perinatal Depression and Anxiety in Both Parents: A Systematic Review and Meta-analysis. JAMA Netw Open. 2022;5(6): e2218969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grau Grau M, Las Heras Maestro M, Riley Bowles H. Engaged fatherhood for men, families and gender equality: healthcare, social policy, and work perspectives. Springer Nature; 2022. 325 p. https://library.oapen.org/handle/20.500.12657/50717. Accessed 11 Aug 2023.
- 20.Tran TC, Pillonel J, Cazein F, Sommen C, Bonnet C, Blondel B, et al. Antenatal HIV screening: results from the National Perinatal Survey, France, 2016. Euro Surveill. 2019;24(40):pii=1800573. 10.2807/1560-7917.ES.2019.24.40.1800573 [DOI] [PMC free article] [PubMed]
- 21.Réévaluation de la stratégie de dépistage de l’infection à VIH en France. Haute Autorité de Santé; 2017.305 p. https://www.has-sante.fr/upload/docs/application/pdf/2017-03/dir2/reevaluation_de_la_strategie_depistage_vih_-_recommandation.pdf. Accessed 23 Aug 2023.
- 22.Penot P. [Acceptabilité et faisabilité d’une consultation prénatale masculine de Prévention, Accès aux droits, Rattrapage vaccinal, Traitement des Affections pendant la Grossesse et pour l’Enfant]. 23rd French AIDS society (SFLS) conference: Plenary session « Beyond gender boundaries »; 2022; Paris.
- 23.Chevrot J, Khelladi I, Omont L, Wolber O, Bikun Bi Nkott F, Fourré C, et al. La Seine-Saint-Denis : entre dynamisme économique et difficultés sociales persistantes . INSEE; 2020. https://www.insee.fr/fr/statistiques/4308516. Accessed 8 June 2023.
- 24.Bousmah MAQ, Combes JBS, Abu-Zaineh M. Health differentials between citizens and immigrants in Europe: A heterogeneous convergence. Health Policy Amst Neth. 2019;123(2):235–43. [DOI] [PubMed] [Google Scholar]
- 25.Dourgnon P, Jusot F, Marsaudon A, Sarhiri J, Wittwer J. Just a question of time? Explaining non-take-up of a public health insurance program designed for undocumented immigrants living in France. Health Econ Policy Law. 2023;18(1):32–48. [DOI] [PubMed] [Google Scholar]
- 26.Gosselin A, Desgrées du Loû A, Lelièvre E, Lert F, Dray-Spira R, Lydié N, et al. Understanding Settlement Pathways of African Immigrants in France Through a Capability Approach: Do Pre-migratory Characteristics Matter? Eur J Popul Rev Eur Demogr. 2018;34(5):849–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Desgrees-du-Lou A, Pannetier J, Ravalihasy A, Le Guen M, Gosselin A, Panjo H, et al. Is hardship during migration a determinant of HIV infection? Results from the ANRS PARCOURS study of sub-Saharan African migrants in France. AIDS Lond Engl. 2016;30(4):645–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haute Autorité de Santé. Catch-up vaccination for newly arrived migrants In the event of unknown, incomplete or incompletely known immunisation status. 2019. 9 p. https://www.has-sante.fr/upload/docs/application/pdf/2020-05/in_the_event_of_unknown_incomplete_or_incompletely_known_immunisation_status.pdf. Accessed 6 Sept 2024.
- 29.Société de Pathologie Infectieuse de Langue Française, Société Française de Pédiatrie, Société Française de Lutte contre le Sida. Bilan de santé à réaliser chez toute personne migrante primo-arrivante (adulte et enfant) 2024. 253 pages. https://www.infectiologie.com/UserFiles/File/migrants/recommandations/recommandation-bilan-de-sante-vfinale-2.pdf. Accessed 6 Sept 2024.
- 30.Crequit S, Chatzistergiou K, Bierry G, Bouali S, La Tour AD, Sgihouar N, et al. Association between social vulnerability profiles, prenatal care use and pregnancy outcomes. BMC Pregnancy Childbirth. 2023;23(1):465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Crequit S, Bierry G, Maria P, Bouali S, La Tour AD, Sgihouar N, et al. Use of pregnancy personalised follow-up in case of maternal social vulnerability to reduce prematurity and neonatal morbidity. BMC Pregnancy Childbirth. 2023;23(1):289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.United States Clinical Trials database. https://classic.clinicaltrials.gov/ct2/show/NCT05085717. Accessed 01 Sept 2024.
- 33.PARTAGE website. https://www.ceped.org/fr/Projets/Projets-Axe-1/article/partage-prevention-acces-aux. Accessed 01 Sept 2024.
- 34.Byamugisha R, Åstrøm AN, Ndeezi G, Karamagi CAS, Tylleskär T, Tumwine JK. Male partner antenatal attendance and HIV testing in eastern Uganda: a randomized facility-based intervention trial. J Int AIDS Soc. 2011;14:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Osoti AO, John-Stewart G, Kiarie J, Richardson B, Kinuthia J, Krakowiak D, et al. Home visits during pregnancy enhance male partner HIV counselling and testing in Kenya: a randomized clinical trial. AIDS Lond Engl. 2014;28(1):95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hoeck S, Van Roy K, Willems S. Barriers and facilitators to participate in the colorectal cancer screening programme in Flanders (Belgium): a focus group study. Acta Clin Belg. 2022;77(1):37–44. [DOI] [PubMed] [Google Scholar]
- 37.Rondet C, Lapostolle A, Soler M, Grillo F, Parizot I, Chauvin P. Are immigrants and nationals born to immigrants at higher risk for delayed or no lifetime breast and cervical cancer screening? The results from a population-based survey in Paris metropolitan area in 2010. PLoS ONE. 2014;9(1): e87046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Freeman HP. The history, principles, and future of patient navigation: commentary. Semin Oncol Nurs. 2013;29(2):72–5. [DOI] [PubMed] [Google Scholar]
- 39.Mosquera I, Todd A, Balaj M, Zhang L, Benitez Majano S, Mensah K, et al. Components and effectiveness of patient navigation programmes to increase participation to breast, cervical and colorectal cancer screening: A systematic review. Cancer Med. 2023;12(13):14584–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tokhi M, Comrie-Thomson L, Davis J, Portela A, Chersich M, Luchters S. Involving men to improve maternal and newborn health: A systematic review of the effectiveness of interventions. PLoS One. 2018;13(1): e0191620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Haile F, Brhan Y. Male partner involvements in PMTCT: a cross sectional study, Mekelle. Northern Ethiopia BMC Pregnancy Childbirth. 2014;14:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roudsari RL, Sharifi F, Goudarzi F. Barriers to the participation of men in reproductive health care: a systematic review and meta-synthesis. BMC Public Health. 2023;23(1):818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gerstel N, Clawson D. Control Over Time: Employers, Workers, and Families Shaping Work Schedules. Annu Rev Sociol. 2018;44:77–97. [Google Scholar]
- 44.Berchet C, Jusot F. État de santé et recours aux soins des immigrés en France : une revue de la littérature. Bull Epidémiologique Hebd-BEH. 2012;(2–3‑4):17‑21.
- 45.Lebano A, Hamed S, Bradby H, Gil-Salmerón A, Durá-Ferrandis E, Garcés-Ferrer J, et al. Migrants’ and refugees’ health status and healthcare in Europe: a scoping literature review. BMC Public Health. 2020;20(1):1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Maternal Questionnaire.
Additional file 2. Women's complete characteristics by partner's attendance.
Data Availability Statement
No datasets were generated or analysed during the current study.