Abstract
Background
On October 7, 2023, Hamas carried out an unprecedented attack on the State of Israel and kidnapped 251 people into captivity to the Gaza Strip. Several months later, as part of a humanitarian exchange deal, 105 hostages were released in five phases and admitted to one of six hospitals throughout the country for treatment. Shamir Medical Center (SMC) was one of these facilities. This study aims to describe the structure, process and outcomes of establishing a comprehensive, multi-step, operational protocol for receiving hostages returning from captivity.
Method
The process of preparing SMC as a receiving center, the establishment of procedures for implementation of the medical protocol, and the assessment of multi-disciplinary team preparedness and implementation and outcomes in an institutional protocol are described.
Results
24 returning hostages were received at SMC. Social workers, dietitians and translators were used by 100% of the majority group of returning hostages from the same country of origin and the sole individual from the other country of origin utilized a dietitian, social worker, ENT consultations, and a hearing test. Among the majority group, orthopedic and dermatological consultations were utilized by 17.4% and 13% received an ENT consultation. Of the administered imaging, 13% received a chest X-ray, 8.7% received a limb X-ray, 17.4% received a head CT scan, and 4.3% received an abdominal CT. In addition, 21.7% were provided antibiotic therapy. Protocol efficacy was measured by assessing time to various operational aspects of protocol implementation and medical procedures such as mean hours to room assignment, primary physician evaluation and social worker session. No correlation between age and operational variables was found.
Conclusion
This novel operational protocol was successfully implemented and may serve as a framework for managing similar unpredictable sensitive events in the case of future need.
Keywords: Hostages, Captives, Captivity, Terror attack, POW
Background
In the early morning of October 7, 2023, approximately 3000 Hamas terrorists invaded Southern Israel from the Gaza Strip, while firing thousands of rockets in what became the largest terror attack in the country’s history [1]. People of all ages were kidnapped to the Gaza Strip [2]. To date, the official Israeli government casualty figures state that 1438 individuals were killed, 11,549 were wounded, and 251 people were kidnapped to Gaza that day [3].
On November 24, 2023, a long-awaited first hostage exchange agreement was made between Israel and Hamas. During the period of Nov 24-Dec 1, 105 hostages were released to Israeli authorities via the Red Cross, and transported to six different medical centers throughout Israel [4]. Twenty-four hostages arrived at the Shamir Medical Center (SMC), an academic medical facility with the fourth largest governmental hospital in Israel throughout that week.
In preparation for the release and return of the hostages from captivity, SMC’s management team created a comprehensive protocol based on scientific evidence, clinical experience, and official guidelines from the local Ministry of Health (MOH). The aim of this paper is to describe the process of preparing the medical facility as a receiving center for hostages returning from captivity, and the assessment of the multi-disciplinary team’s preparedness and implementation of the protocol in real-time as well as a reflection of the experience and efficacy. To our knowledge, this is the first paper to describe an operational protocol for receiving hostages released from captivity. A protocol component checklist for future use is included in the tables section. (Table 1)
Table 1.
Protocol components and reasoning
| Selecting the team |
| Selecting building to house the receiving ward |
| Preparation of inpatient rooms |
| Preparation of urgent care ward |
| Establishing security |
| Parking and transportation |
| Management of media |
| Preparing the protocol |
| Preparation and training of medical staff for admission of hostages |
| Simulation and readiness assessment |
| Calling up/Alerting the medical team |
| Returning hostage arrival at helicopter landing pad and initial triage |
| Reunion with families |
| Admission to receiving ward/documentation of injuries and wounds/sexual assault |
| Mental health support |
| Foreign citizens needs |
| Discharge from hospital |
Existing studies, primarily on the health and functioning of former prisoners of war (POWs), depict the serious psychological consequences that ensue after release from captivity, where captives often undergo extreme and inhumane conditions, as well as psychological and physical abuse [5–8]. Despite the data on the severe health effects of captivity, both clinical and psychosocial, our search identified only one publication detailing operational and clinical approaches to receiving released hostages [9].
Methods
Study design
This is a descriptive-narrative study of the structure, process and outcomes of establishing a comprehensive operational protocol for receiving returning hostages from captivity. The multi-step protocol includes.
Preparation of the operational protocol.
Preparation of the receiving facility.
Establishment of a medical workup/laboratory testing protocol (described in a separate paper).
Preparation and training of medical staff for admission of released hostages.
Simulation and readiness assessment.
Metrics of the protocol efficacy from an operational perspective were also evaluated.
Participants
24 released hostages returning from captivity in the Gaza Strip.
Setting
Shamir Medical Center is a 904-bed academic medical facility in Israel’s central region. The emergency medicine department is the 4th largest in Israel.
Preparing the facility
On November 24, 2023, the management team of SMC was alerted of the possibility of a hostage release deal and asked to prepare to receive hostages released from captivity (the exact number was not known in advance). The preparation of both the facility and its staff for the event is described.
Selecting the team
One of the first steps taken by the hospital management was to select the clinical team to receive and treat the returned hostages and the following members were selected:
Operational manager
A physician member of hospital management involved with the building of the protocol would serve as the operational manager for the site and would review all certifications and permits.
Floor manager physician
An emergency medicine specialist would serve as emergency department (ED) manager, oversee the clinical site and select the case management teams.
Emergency medicine physician for triage
In the case of hostage arrival, an emergency medicine specialist was to wait on the helipad to meet the air ambulances, receive a summary from the care team, greet the hostages and conduct initial triage to assess if urgent care would be required. Those requiring urgent care would be transported to the urgent care ward.
Case management teams for each patient
The official guidelines of the MOH for the six hospitals selected to receive hostages returning from captivity stated that patient medical teams would be required to include an ED physician or an internist and an ED nurse. Based upon this guideline, a triad concept for case management teams was formulated at Shamir, in which each patient would be provided a personal medical team, including an ED physician/internist, an ED nurse, a social worker and if needed, a translator.
The team social worker would be tasked with the responsibility for requesting any required psychological and psychiatric care, although final decisions were to be made in collaboration with the team physician. The social worker would also accompany the patient (and their family) from arrival until discharge and be responsible for establishing and overseeing continuing treatment in the community setting, after the patient’s return home. It was decided that the inpatient team would remain consistent and permanent throughout the patient’s entire stay, except for any required specialists who might be added as consultants, at the discretion of the team physician and managing physician. All team members were required to have schedule flexibility and availability, access to transportation as well as a developed sense of compassion and sensitivity. The staff was also trained to prepare for language barriers and to recognize and respect potential cultural differences, such as preferences for personal physical space. Every staff member responsible for cleaning, sanitation, and maintenance was also trained for the event and would be required to receive permission at every shift to enter the admission ward to carry out their job duties.
Preference for female team members
The protocol emphasized a preference for female physicians and team members due to evidence supporting a strong likelihood of sexual assault and violence being perpetrated in captivity. Various experts in the field had recommended that a predominance of female staff might be less of a trigger for the female returning hostages and that a greater presence of women would serve as an added differentiator between the hospital/inpatient experience and that of captivity. Ultimately, the choice of physician gender was left to the patients themselves.
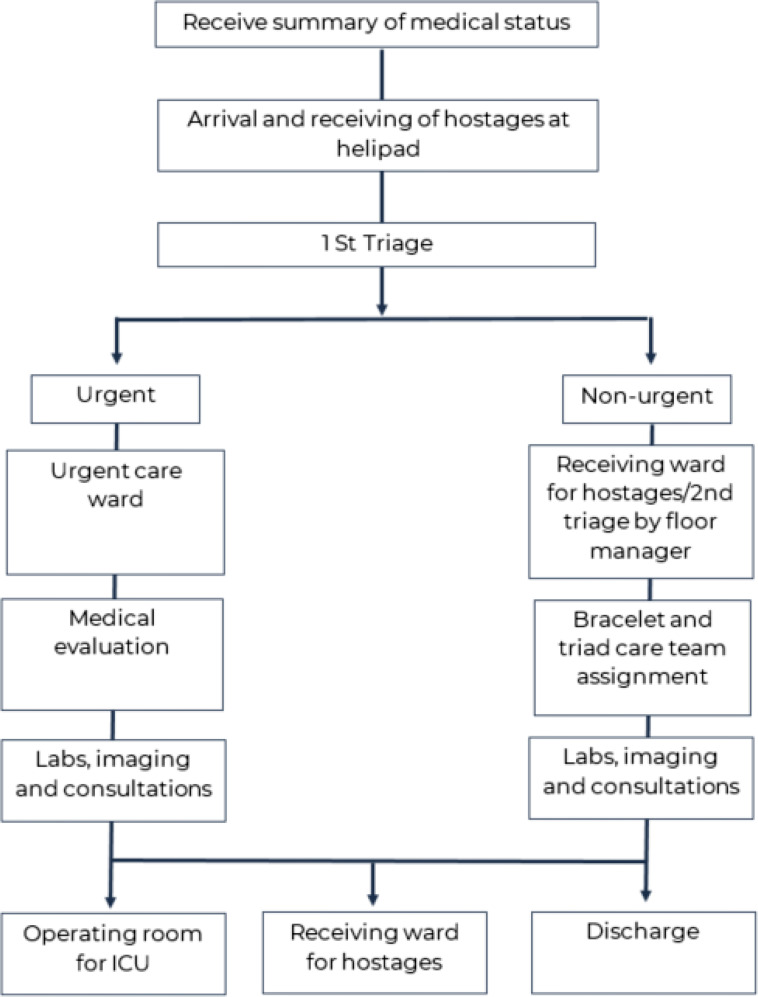
Medical specialists
Physicians and nurses from every area of specialty were also included in the team to ensure comprehensive care. The multi-disciplinary team included an ED doctor, a pediatric ED doctor, an internal medicine doctor, a surgeon, an orthopedist, a pediatrician, an infectious disease specialist, a psychiatrist and a gynecologist (specializing in sexual assault). (Fig. 1)
Fig. 1.
Hospital flowchart for receiving returned hostages
Choosing the building to house the admission ward
The building chosen to serve as the receiving facility was large enough to accommodate many patients and was located at ground level at the campus periphery, far from access to potential onlookers, the media and hospital staff. It was decided that entry to the ward would be permitted exclusively to approved staff and MOH representatives and others given prior management approval. Those with permission to enter would be given a colored wristband and a name tag for identification purposes.
The building also included offices that could be utilized by administrative and support staff and for storage of supplies; it was also located within walking distance of approved visitor parking. Since this site was a regular internal ward, carts with additional medical supplies needed for urgent care treatment such as wound care, blood draws, EKG, and ultrasound machines would be made available there, in case of need.
Preparation of inpatient rooms
One of the main priorities was to impart a strong sense of warmth, hospitality and comfort upon arrival at the facility. Signs with the name of the returning hostage, and flags of Israel and of their home country (in the case of foreign citizens) were placed on room doors before their arrival. Each room was to be furnished with a comfortable bed, a TV, armchairs, a robe and towels, flip-flops, soap/toiletries, infant formula and diapers. Light refreshments were to be offered after receiving the approval of the dietitian that there was no risk of refeeding syndrome.
The courtyard of the building included a garden with benches, and the halls of the ward were to be furnished with additional benches and extra couches. It was requested that all mirrors be removed from the hallways, in order to prevent a potentially traumatic experience of inadvertently viewing dramatic changes in appearance that may have occurred during an extended time in captivity [10].
The admission ward was also to include a fully furnished family room with child-appropriate refreshments. Children’s rooms were to be equipped with a child-size bed, soft dolls, and toys, based upon the social workers’ recommendation. Shade umbrellas, tables with refreshments and patio chairs were also to be made available for use by patients and their families.
Special rooms were prepared for use by the translators, staff from the National Insurance Institute, staff from the Ministry of Foreign Affairs, representatives from the local police and other government representatives, as was a seminar room for routine updates and team meetings to discuss patient status.
Any required imaging, blood and urine tests would be performed in the admission ward, with priority status. A medication room, a crash cart, an EKG cart, oxygen tanks, a portable X-ray machine, an ultrasound machine and an exam table for gynecological exams were all to be made available in the ward.
Urgent care ward
Patients requiring urgent care were to be taken to a separate fully stocked ward that had been previously established, close to the ED and not currently in use. In the case that a need for this ward was to arise, the security team was prepared to perform a full security lockdown, and a case manager triad (a physician, nurse, social worker plus translator) for each patient was to be called in. The urgent care ward had the benefits of the availability of advanced radiology, CT (computed tomography) scans, a facility for urgent medical procedures, and the availability of resources such as a stocked medicine room and blood for transfusions.
Establishing facility security
The most significant security concern for the hospital by far was the presence of local onlookers who might try to enter the facility, as well as the presence of local and international media. Consequently, the hospital had an extensive plan to ensure the highest levels of security, 24 h a day. The admission ward area was to be blocked off entirely and the security team would assume responsibility for maintaining the privacy of the returned hostages within the Medical Center campus. Curtains/blinds would be installed in the inpatient rooms, such that no one could see through the windows. In addition, all cameras and video cameras were to be disconnected. Entry to the facility was in the form of a “one-directional flow” and all exits were to be closed off, with the exception of emergency exits which were to be left available for use. Access to patient rooms was to be given to the patient’s personal medical team only.
Security and cars that transported patients from the helipad to the ward were also staffed with a security member. As a general rule, every effort was to be made to keep all advisors/physicians “in-house,” and to prevent unnecessary exits from the ward.
Parking and transportation
Families and approved representatives were to be given use of and unlimited access to a designated parking lot. Upon receiving notice of the imminent arrival of the returning hostages to the hospital (with advance notice of four hours), the security team would be notified of the closest parking lot to the admission ward, clear the parked vehicles and assign a security person to manage traffic flow.
Media management
It was decided that no contact or interviews would be permitted between members of the media and the returning hostages, their families or hospital staff. A special site was created for the use of media members at the site normally used for covering mass casualty events including an outside area for cameras and live broadcasts or interviews. The location provided a view of the urgent care ward and the helipad (only ambulances were visible). The outside area included electrical outlets for cameras, podiums flags and rollups for interviews to encourage members of the media to remain stationed in their designated area. Full cooperation was maintained with the army, the Ministry of Foreign Affairs and the hospital spokesperson.
Preparing the operational protocol
Calling up/alerting the medical team
Upon receiving word of the released hostages’ imminent arrival, the hospital manager would immediately contact the medical team such that they would all be ready within four hours. Management/team contact was maintained using an instant messaging app. Demographic details about the hostages were to be provided to the hospital management by the MOH and all of this information was to be shared with the team.
Returning hostage arrival and initial triage
An emergency medicine specialist was to be available to receive and greet them on the helipad, carry out an initial evaluation and triage after receiving a brief summary from the air ambulance team, and determine who required immediate medical attention. Ambulances and minibuses would be made available to securely transport every returning hostage to the appropriate ward. Critically ill patients requiring immediate treatment would be transported directly to the urgent care ward in an ambulance, where an initial medical evaluation would be conducted by the specially trained urgent care team. In the case of a child and parent arriving together, they were to be transferred to the admission ward as quickly as possible and kept together. Medical charts would be opened and established by urgent care admissions. Patients who did not require urgent care were to be transported directly to the admission ward in secured minibuses.
Reunion with family members
The security team was to be responsible for receiving and accompanying any family members arriving via helicopter or car to their relatives in the admission ward. Family members were given a brief training as to how to interact with the hostages upon their return and were encouraged to stay in the ward in order to accompany returning hostages throughout their hospitalization to all tests and evaluations. Every family would be assigned their team social worker while waiting to be admitted. In the case of the arrival of children, a family member was to be assigned to accompany the child according to the social worker’s recommendation.
Admission to the receiving ward
After being transported by minibus to the receiving ward, non-urgent patients were to enter the building via an area adjacent to the staff lounge area in a gradual and single-file manner, which allowed for the utmost privacy. Upon entering their room, each was to be given the time they required to bathe and dress in a calm and quiet environment. In the case that a returning hostage did not have relatives to support them, they were to be given the option of sharing a room with another returning hostage for emotional support throughout their stay. Only after reuniting with family members and settling into their rooms would patients receive a complete explanation of the medical evaluation process and together with their families or companions, undergo a more extensive in-room evaluation. A family member or companion could be present during all laboratory testing or examinations upon the request and full consent of the patient.
Any patient requiring a second or follow-up evaluation outside of their ward was to be accompanied by a security person, a family member or companion and a hospital staff member. Patients leaving the ward were to be accompanied by a security person, a hospital staff member, and stretcher-bearers, if needed.
Documentation of medical and forensic records
Patient charts were to be opened using the regular hospital electronic medical record system (EMR), but to be stored in a confidential section for the files of returning hostages; only those with permission would be allowed access to these files. All evidence of physical injury that might represent evidence of war crimes and/or sexual assault was to be documented and reported to the MOH and forensic team. Specialists in forensic records and a special legal medical team were made available to collect testimonies and photos as evidence in such cases. In the case of evidence of sexual assault, special testing and prophylactic medication were to be made available as needed.
Discharge from hospital
The decision to discharge was to be made by the case manager, in collaboration with the social worker and in coordination with the MOH. The social worker was to remain responsible for communicating with their local health maintenance organization (HMO) regarding the continuation of treatment in the community setting. Any returning hostage who wanted to remain in the hospital for additional days would have the option to do so.
Preparation and training of medical staff for admission of hostages
The medical staff was trained and prepared to impart a sense of “coming home” to all of the returning hostages. In general, the team was educated about the importance of wording and communication that was sensitive, respectful and also encouraging in order to give returning hostages back control over their lives. In addition, team members were instructed to avoid provocative questioning about events that may have occurred in captivity. All social workers underwent simulations of working with released hostages. The staff was also trained to prepare for language barriers, as well as to recognize and respect potential cultural differences, such as preferences for personal physical space. Psychologists and psychiatrists were also made available to consult as needed.
Simulation/readiness assessment
Two simulations involving the entire team were carried out as the final stage of the protocol preparation. Actors were brought in to play the role of returning hostages and every team member walked through their role in greeting and receiving them, speaking with them, from their arrival at the landing pad until admission. Upon terminating the simulation, the social workers and various subject matter experts provided important feedback for fine-tuning and assessing team readiness.
Statistical analysis
Participant data was analyzed separately based on country of origin to maintain group homogeneity and due to the difference in the use of hospital resources from the remainder of the participants which also impacted length of stay. Frequencies for categorical variables were tested using SPSS 29.0 software. Descriptive statistics were calculated for continuous variables including the mean, standard deviation, median, interquartile range, and range. The correlations between independent continuous variables were assessed using the Spearman correlation coefficient. Two-tailed P < 0.05 was considered statistically significant.
Results
A total of 24 returning hostages arrived at SMC; 23 male and one female, and all were foreign workers. 23 of the hostages were from the same country of origin (Table 2). The hostages arrived in phases between November 24 and November 30, 2023. Throughout that week, the phases of arrival were as follows: 11 hostages arrived on November 24, seven on November 26th, two hostages on November 28th, and four on November 30th.
Table 2.
Demographic data - group
| Frequency | Percentage | Mean + SD | Median (25-75%) | Range | ||
|---|---|---|---|---|---|---|
| Group | Total | 23 | 100% | |||
| Gender (male) | 22 | 95.7% | ||||
| Age | 35 + 6.5 | 35 (29–40) | 25–49 | |||
| Individual from other country of origin | Gender (male) | 1 | ||||
| Age | 33 |
Operational outcomes
For the majority group, the mean number of days spent hospitalized was 5 ± 1 (median 6; range 4–6) and for the participant from the other country of origin, the mean number of days spent hospitalized was 3.
Protocol efficacy was measured in part by assessing the time it took to various operational aspects of protocol implementation and medical procedures. The mean number of hours from admission to room assignment was 1.04 + 0.88 and a mean of 3 + 0.79 h passed from admission until the primary physician evaluation. A mean of 2.99 + 3.14 h passed from admission to when vital signs were taken, and a mean of 10.99 + 7.71 h passed from admission to the first assessment/measure of pain intensity. The mean time from admission to the first social worker session was 4.89 + 3.01 h and the mean time from admission to receipt of blood count results was 2.89 + 1.46 h (Table 3).
Table 3.
Measures of operational/implementation times
| Group N = 23 (100%) |
Mean + SD | Median (25-75%) | Range | Mean + SD |
|---|---|---|---|---|
| Individual from other country of origin | ||||
| Hours from admission to room assignment | 1.04 + 0.88 | 0.57 (0.38–1.99) | 0.01–0.11 | 39 min |
| Hours from admission until 1st physician evaluation | 3 + 0.79 | 3.03 (2.76–3.43) | 0.05–0.19 | 2.45 h |
| Hours from admission to receipt of ID bracelet | 4.88 + 2.17 | 5.58 (2.76–6.2) | 0.09–0.44 | 6.15 h |
| Hours from admission to measure of vital signs | 2.99 + 3.14 | 2.33 (2.18–2.63) | 0.05–0.72 | 1.53 h |
| Hours from admission to assessment of pain intensity (VAS) | 10.99 + 7.71 | 5.53 (3.81–18.73) | 0.09–0.8 | 19.25 h |
| Hours from admission to taking body measurements | 2.39 + 0.59 | 2.37 (2.18–2.66) | 0.05–0.16 | 1.54 h |
| Hours from admission to 1st social worker session | 4.89 + 3.01 | 3.07 (2.73–7.23) | 0.08–0.43 | 2.44 h |
| Hours from admission to placement of Venflon | 11.19 + 8.28 | 18.50 (2.54–18.75) | 0.08–0.81 | 19.26 h |
| Hours from admission to receipt of blood count results | 2.89 + 1.46 | 2.63 (2.28–2.84) | 0.07–0.38 | 2.12 h |
For the participant from the other country of origin, the mean time from admission to room assignment was 39 min. A mean of 2.45 h passed from admission until the primary physician evaluation. A mean of 1.53 h passed from admission to when vital signs were taken, and a mean of 19.25 h passed from admission to the first assessment/measure of pain intensity. The mean time from admission to the first social worker session was 2.44 h and the mean time from admission to receipt of blood count results was 2.12 h (Table 3).
Utilization of resources
Among the group of 23 returning hostages from the same origin, various consultations were utilized. Consults with social workers and dietitians, as well as translators and COVID-19 tests, were used by 100% (23) of the returning hostages and 95.7% (22) received testing for Q-fever, Hepatitis B and HIV. Urine toxicology testing was used by 73.9% of participants. Psychiatrist consultation was utilized by 8.7%. Orthopedic and dermatological consultations were utilized by 17.4% of the patients and 13% received an ear nose and throat (ENT) consultation.
Various types of imaging were used by the group. Of the 23, 13% received hearing tests and chest X-rays, 8.7% received a limb X-ray, 17.4% received a head CT scan, and 4.3% received an abdominal CT. 8.7% required a consultation with a neurosurgeon. In addition, 21.7% were provided antibiotics. The remaining available consultations and tests (ophthalmologist, hearing test, mouth and jaw, occupational therapists, hematologist, cardiologist, surgeon consult, continuous vital signs monitoring, EKG, ECG, B-Hcg test) were utilized by between 4.3 − 21.7% of the individuals (Table 4).
Table 4.
Patient use of resources/consultations
| Total | Frequency | Percentage | Frequency |
|---|---|---|---|
| 23 | 100% | Individual from other country of origin | |
| Consultations | |||
| Translator | 23 | 100% | 0 |
| Social worker | 23 | 100% | 1 |
| Ophthalmologist | 3 | 13% | 0 |
| Dermatologist | 4 | 17.4% | 0 |
| Ear nose and throat | 3 | 13% | 1 |
| Hearing test | 3 | 13% | 1 |
| Dietitian | 23 | 100% | 1 |
| Mouth and jaw | 1 | 4.3% | 0 |
| Orthopedist | 4 | 17.4% | 0 |
| Occupational therapist | 2 | 8.7% | 0 |
| Hematologist | 1 | 4.3% | 0 |
| Cardiologist | 1 | 4.3% | 0 |
| 0 | |||
| Surgeon consult | 2 | 8.7% | 0 |
| Psychiatrist | 2 | 8.7% | 0 |
| Neurosurgeon | 2 | 8.7% | 0 |
| Imaging | |||
| Chest X-ray | 3 | 13% | 0 |
| Limb X-ray | 2 | 8.7% | 0 |
| Head CT | 4 | 17.4% | 0 |
| Abdominal CT | 1 | 4.3% | 0 |
| Monitoring | |||
| Continuous vital signs monitoring | 1 | 4.3% | 0 |
| EKG | 1 | 4.3% | 0 |
| ECG | 1 | 4.3% | 0 |
| Laboratory testing | |||
| Covid-19 test | 23 | 100% | 1 |
| Q fever test | 22 | 95.7% | 1 |
| HIV test | 22 | 95.7% | 1 |
| Hepatitis B test | 22 | 95.7% | 1 |
| Urine toxicology test | 17 | 73.9% | 1 |
| B-Hcg test | 1 | 4.3% | 0 |
| Medication | |||
| Antibiotics | 5 | 21.7% | 0 |
The individual from the other country of origin utilized dietitian, social worker and ENT consultations, a hearing test and COVID-19, Q fever, HIV, Hepatitis B, and Urine toxicology tests (Table 4).
Finally, the Spearman test was used to assess the correlation of numerous variables related to operational aspects of protocol implementation with patient age, however, these results did not have clinical significance (Table 5).
Table 5.
Spearman correlation – age correlation with variables
| Variable | Spearman’s rho to age | P value |
|---|---|---|
|
Weight change N = 19 |
-0.227 | 0.350 |
|
Hours to room N = 23 |
-0.144 | 0.514 |
|
Hours to primary physician N = 23 |
-0.267 | 0.218 |
|
Hours to bracelet N = 19 |
0.339 | 0.156 |
|
Hours to vital signs N = 23 |
0.144 | 0.511 |
|
Hours to pain evaluation N = 19 |
0.300 | 0.212 |
|
Hours to anthropometric data collection N = 23 |
0.096 | 0.664 |
|
Hours to social worker N = 23 |
-0.167 | 0.445 |
|
Hours Venflon N = 19 |
0.281 | 0.244 |
|
Hours to CBC N = 23 |
0.293 | 0.174 |
Discussion
This paper sought to describe the establishment of a novel, operational protocol for the preparation of a medical facility to receive hostages released from captivity, and to describe the outcomes of its implementation.
From an operational perspective, the protocol was effective when implemented in real-time. The hospital management, patient teams and staff collaborated effectively, and there were no unexpected events or lack of critical staff or equipment identified. Of all the team members, the importance of social workers’ presence throughout the patient journey was evident, particularly during more sensitive moments.
The study outcomes did reveal that the mean times from admission to room assignment, taking of vital signs, first primary physician visit, first social worker visit, blood draw and measure of pain intensity, were all slightly longer than would be expected under normal circumstances in a routine setting. However, these findings did not come as a surprise, as we had previously noted the length of time the returning hostages spent bathing and tending to personal hygiene after their arrival (over 1.5 h), a natural need after the extensive time these individuals spent in captivity in underground tunnels. The urgent care ward was not needed or utilized.
A typical number of visitors came to the ward, with numerous visits paid by concerned family members of other hostages who were and still remain in captivity, who were eager to inquire about the state of their loved ones. There was also a consistent presence of representatives from various government offices. As a result, there was a need for additional sleeping quarters, additional secure parking and primarily, additional translators, for consultations and conversations and the translation of medical charts and documents.
Due to a stringent protocol, the building choice for the admission ward and the hermetic closure of the facility, the security team was able to successfully prevent access and entry to curious onlookers, one of the most important operational aspects of the protocol. In addition, this event required a significant shift for the hospital that normally functions as an independent entity in order to support a widespread collaboration with government entities such as the MOH and other governmental bodies, such as foreign embassies, which was achieved with success despite a lack of certainty, even on part of the management.
Limitations and points for future consideration
This protocol was comprised of a vast body of knowledge from numerous hospital operational protocols, including staff management, medication management, imaging, and security. This hostage protocol was built using these methods together with the oversight of the MOH and the military regarding the process and protocol. Therefore, to our knowledge, nothing significant was missing.
As previously mentioned, the data was analyzed separately based on country of origin which was intended to maintain the homogeneity of the large group and since country of origin affected variables such as length of stay and use of resources (such as translators).
In expectation of special requests, rooms were stocked in advance with an array of toiletries and self-care items, including hygiene, perfume and tobacco products normally not stocked on-site. In addition, due to the length of time spent in captivity, the majority of returning hostages requested a haircut, so a volunteer barber was brought in to address grooming needs. Future protocols should consider such factors and prepare for various types of non-medical requests.
Another issue that arose in real time that was not addressed in the original protocol was the religious needs of the returning hostages. Once it was understood that the majority of the hostages that were received at SMC were practicing Buddhists, meetings with members of academia were arranged in order to educate the staff, and arrangements were made to prepare a suitable place of worship in the ward. Future protocols should address the potential religious and spiritual needs of returning hostages (i.e. having available various religious texts), another essential aspect of support after release from captivity.
Finally, even though the majority of the hostages were eligible to be discharged after two days, the majority stayed in the hospital for a maximum of five days. While the original protocol assumed that returning hostages would have the presence of strong family support, hostages who were foreign citizens employed in the agricultural sector did not have the privilege of the presence or support of family members nearby. Stays were lengthened for a variety of reasons that also included the feeling of safety, warmth and support provided at the hospital, particularly from the team social worker. The possibility of a lengthier stay and its effect on hospital resources should be taken into account in the case that similar events arise.
Conclusion
This novel protocol for the operational management of returning hostages was planned and successfully implemented during the first phase of hostage release from Gaza in November and December of 2023. The real-time implementation specifically highlighted the unique and complex needs of released hostages, particularly when also foreign citizens, as well as the importance of multi-disciplinary teamwork, and the seamless continuation of psychosocial and medical treatment in the community setting. It is highly recommended to prepare facilities as far in advance of arrival as possible since most hospitals are not set up to accommodate such a sensitive event. This protocol may be used as a framework for other institutions and facilities in case of future need. Further research is needed, particularly as related to the needs of hostages who are foreign citizens.
Acknowledgements
Not applicable.
Abbreviations
- SMC
Shamir Medical Center
- ENT
Ear, nose, and throat
- MOH
Ministry of Health
- POW
Prisoner of war
- ED
Emergency department
- HMO
Health maintenance organization
Author contributions
DT was involved with conceptualization, visualization, methodology; data curation, formal analysis, project administration, drafting the manuscript, reviewing and editing the manuscript; IS was involved with reviewing and editing the manuscript; RK was involved with methodology, data curation reviewing and editing the manuscript; OT was involved with methodology, data curation reviewing and editing the manuscript; GP was involved with methodology, data curation reviewing and editing the manuscript; GG was involved with methodology, data curation reviewing and editing the manuscript; KO was involved with methodology, data curation reviewing and editing the manuscript; MA was involved with data curation reviewing and editing the manuscript; RZ was involved with methodology, data curation reviewing and editing the manuscript; MB was involved with data curation reviewing and editing the manuscript; BB was involved with data curation reviewing and editing the manuscript; REV was involved with drafting, reviewing and editing the manuscript; IH was involved with methodology, data curation reviewing and editing the manuscript; MA was involved with methodology, data curation reviewing and editing the manuscript; VS was involved with methodology, data curation reviewing and editing the manuscript; AA was involved with methodology, data curation reviewing and editing the manuscript; OLK was involved with supervision, methodology, data curation reviewing and editing the manuscript.
Funding
This trial received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data availability
Raw Data were generated at Shamir Medical Center. Derived data supporting the findings of this study are available from the corresponding author DT on request.
Declarations
Ethics approval and consent to participate
Ethical approval was sought and approved by the Shamir Medical Center Helsinki committee, reference 0027 − 24. The Helsinki committee waived the requirement for written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.News Y. 2023; https://www.ynetnews.com/article/bkjkxweqp, 2024.
- 2.Ministry of Foreign Affairs I. 2023; https://www.gov.il/en/departments/news/swords-of-iron-war-in-the-south-7-oct-2023, 2024.
- 3.Shabak.gov. 2023 Year End Report. Shabak.gov;2024.
- 4.Ministry of Foreign Affairs.gov. Swords of Iron: Hostages and Missing Persons Report. Swords of Iron: Hostages and Missing Persons Report Ministry of Foreign Affairs (www.gov.il); June 25, 2024.
- 5.Jukić M, Malenica L, Đuričić V et al. Long-Term Consequences of War Captivity in Military Veterans. Healthcare (Basel, Switzerland). 2023;11(14). [DOI] [PMC free article] [PubMed]
- 6.Fletcher K. The management of released hostages. Adv Psychiatr Treat. 1996;2(6):232–40. [Google Scholar]
- 7.Turnbull G, Hostage, Retrieval. J R Soc Med. 1997;90(9):478–83. 10.1177/014107689709000904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Basoglu M. Rehabilitation of traumatised refugees and survivors of torture. BMJ. 2006;333(7581):1230–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de la Fontaine N, Silberg T, Fegert JM, Tsafrir S, Weisman H, Rubin N, Ashkenazi M, Nacasch N, Polliack ML, Chen W, Herman-Raz M, Wachsberg-Lachmanovich R, Pessach-Gelblum L, Ziv A, Moshkovitz A, Shilo N, Frenkel-Nir Y, Gothelf D, Pessach IM. Acute response to the October 7th hostage release: rapid development and evaluation of the novel ReSPOND protocol implementation within a children’s hospital. Child Adolesc Psychiatry Ment Health. 2024;18(1):76. 10.1186/s13034-024-00767-3. PMID: 38902765; PMCID: PMC11191208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Freysteinson WM. Demystifying the mirror taboo: a neurocognitive model of viewing self in the mirror. Nurs Inq. 2020;27(4):e12351. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Raw Data were generated at Shamir Medical Center. Derived data supporting the findings of this study are available from the corresponding author DT on request.