ABSTRACT
Background:
Thoracoscopic surgery is an increasingly popular surgical technique for the repair of congenital diaphragmatic hernias. We performed a meta-analysis to compare the efficacy, safety of thoracoscopic surgery and the conventional open surgical approach for congenital diaphragmatic hernia in neonates.
Materials and Methods:
A systematic search of electronic databases such as PubMed, Google, and Web of Science was performed to identify studies comparing thoracoscopic surgery and open surgery for congenital diaphragmatic hernia. A total of 6 studies with 3348 patients were found. Parameters such as operation time, hospital stay, recurrence rate, postoperative mortality, and postoperative complications were pooled and compared by meta-analysis.
Results:
Of the 3348 children with congenital diaphragmatic hernia included in the 6 studies, 615 underwent thoracoscopic surgery and 2733 underwent open surgery. All studies were nonrandomized controlled trials. The operation times were shorter for thoracoscopic surgery than for open surgery in three studies, but there was no significant difference (standard mean difference = 1.25, confidence interval [CI] = [−0.48–2.98], P = 0.16). In the thoracoscopic surgery group, the rate of postoperative deaths was significantly lower (95% CI = 1.24–2.75), but the occurrence of recurrences was more frequent (95% CI = 0.08–0.23). The hospital stay varied significantly across studies. There was a statistically significant difference (standard mean difference = −1.47, CI = [−2.24–−0.70], P < 0.001) in the overall effect between the groups. The complication rate was significantly lower with thoracoscopic surgery compared to open surgery (odds ratio = 0.26, CI = [0.10–0.66], P = 0.004) for the overall effect between the groups. The thoracoscopic procedure, however, was planned for milder and stable cases.
Conclusion:
Thoracoscopic repair of congenital diaphragmatic hernia in neonates is associated with a shorter length of hospital stay, fewer complications, and less postoperative mortality than traditional open repair. However, the rate of recurrence was found to be higher in those who underwent thoracoscopic surgery.
KEYWORDS: Congenital diaphragmatic hernia, minimally invasive surgery, mortality, neonates, recurrence
INTRODUCTION
A congenital diaphragmatic hernia is a birth anomaly in which the abdominal organs protrude into the chest cavity due to incomplete development of the diaphragm, a muscle that separates the chest and abdomen. Congenital diaphragmatic hernias occur with an approximate frequency of 1:2500–1:5000,[1] and 40%–60% of cases are fatal,[2,3] which can impede lung growth and lead to respiratory problems. To diagnose a congenital diaphragmatic hernia, a prenatal ultrasound scan is usually performed. As part of the treatment, surgical correction is performed to realign the organs and fix the diaphragm. Despite improvements in medical care, congenital diaphragmatic hernias remain a difficult condition with unpredictable results. Congenital diaphragmatic hernias in newborns may require extensive medical care, including assisted breathing. The long-term prognosis depends on how severe the defect is and how many complications occur.
Different surgical procedures are used for congenital diaphragmatic hernias because of their phenotypic and clinical implications. The diaphragmatic defect must be addressed by open or minimally invasive surgery (MIS) at this point.
For open repair of the diaphragmatic defect, a laparotomy is usually performed. In the past 20 years, thoracic surgery has been used to treat congenital diaphragmatic hernias as MIS has rapidly evolved. The first report on thoracoscopy for congenital diaphragmatic hernia was published in 1995 by Silen et al.[4] Theoretically, thoracoscopic surgery offers the advantages of fewer postoperative complications, better cosmesis, and faster recovery. According to related studies, children undergoing MIS have shorter recovery times, shorter hospital stays, shorter recovery times after mechanical ventilation, and lower postoperative analgesic consumption than patients undergoing open surgery; however, MIS may increase the risk of hypoxia and hypercapnia.[5] In addition, the recurrence rate after MIS is higher.[6] In this study, we performed a meta-analysis of all published clinical trials to compare the efficacy, safety, and effectiveness of thoracoscopic surgery and the conventional open surgical approach for congenital diaphragmatic hernia in neonates.
MATERIALS AND METHODS
Setting and study design
This meta-analysis study was conducted in the Department of Paediatric Surgery at a government tertiary teaching institute in Northern India.
Identification and procedure: Literature search and study selection
The researchers independently searched PubMed, Google, and Web of Science for articles on thoracoscopic surgery and the conventional open surgical approach for congenital diaphragmatic hernia in neonates. The following search terms were used: (thoracoscopic surgery OR conventional open surgery) AND (operative time OR length of hospital stay) AND (recurrence OR survival rate OR mortality rate OR complications). In addition, a manual search of all article and journal references was performed to find further relevant studies.
The results were limited to congenital diaphragmatic hernias in neonates and to operation duration, length of hospital stay, recurrence, survival rate, mortality rate, and complications. The search results from PubMed, Google, and Web of Science yielded a total of 158 articles. (1) Multinational study, retrospective study, and prospective study; (2) thoracoscopic surgery and conventional open surgery; (3) published articles; (4) full article in English; and (5) human studies and articles published after 2016 were included, while unpublished articles, animal studies, and articles not published in English were excluded. These were the inclusion criteria for the selection and inclusion of studies. The primary consideration in the selection of studies was the evaluation of operative time, length of hospital stay, recurrence, survival, mortality, and complications associated with thoracoscopic surgery and conventional open surgery for congenital diaphragmatic hernia in neonates.
Data collection
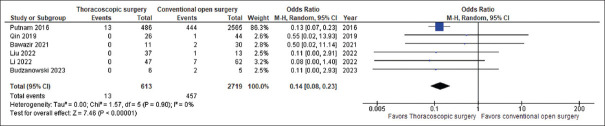
Data were extracted individually by the authors from the text, figures, or tables of each published article. The above information was extracted from each study, including operation time, length of hospital stay, recurrence, survival rate, mortality rate, and complications of thoracoscopic surgery and conventional open surgery [Figure 1].
Figure 1.
Flow diagram of article searching, screening, eligibility, and included or selection process
Synthesis of the data
The following data were collected for each study: article title, lead author name, journal name, date of publication, nation name, and type of surgery.
Statistical analysis
Statistical analysis was performed using Review Manager 5.3 (RevMan 5.3) from the Cochrane Collaboration based in London, United Kingdom. The parameters were measured using mean, standard deviation, number, and percentage. The heterogeneity of the study was assessed using the Q (2) test and the I2 statistic. Assuming significant heterogeneity, the effect size was calculated using the random effects model. In addition, a sensitivity analysis was performed to investigate the reasons for the heterogeneity. p<0.05 was considered statistically significant for the effect sizes.
RESULTS
Search results
Figure 1 shows the search results for published articles. A total of 158 published articles were initially looked up and obtained. A total of 20 articles were removed due to duplicate. A total of 138 literature references were reviewed for relevance to the topic, duplicate works, and review articles before being excluded from this meta-analysis. A total of 123 articles were removed due to irrelevant data. This was done based on the titles and abstracts of the papers. After the abstract and title review, 15 articles were selected for full-text review. Due to the case report and the lack of sufficient data, 9 articles were excluded. Therefore, a total of 6 studies were included in the meta-analysis, which included 615 patients in the thoracoscopic surgery group and 3133 patients in the conventional open surgery group. Six publications[7,8,9,10,11,12] were finally considered for the meta-analysis [Figure 1 and Table 1].
Table 1.
Characteristics/information of the studies included in the meta-analysis
| Studies | Surgery | Measures | Groups (n): Surgical technique |
|---|---|---|---|
| Putnam et al.[7] | Congenital diaphragmatic hernia | Duration of surgery, mechanical ventilation, hospital stay, complications, mortality, recurrence | Minimally invasive approach (n=488) Open repair (n=2579) |
| Qin et al.[8] | Congenital diaphragmatic hernia | Intraoperative bleeding, incision length, operation duration, complications, mortality, recurrence | Thoracoscopic repair (n=26) Open repair (n=44) |
| Bawazir and Bawazir[9] | Congenital diaphragmatic hernia | Duration of surgery, mechanical ventilation, hospital stay, complications, mortality, recurrence | Thoracoscopic repair (n=11) Open repair (n=30) |
| Liu et al.[10] | Congenital diaphragmatic hernia | Duration of surgery, mechanical ventilation, hospital stay, shorter time to reach optimal feeding, complications, mortality, recurrence | Thoracoscopic repair (n=37) Open repair (n=13) |
| Li et al.[11] | Congenital diaphragmatic hernia | Operation time, intraoperative blood loss, postoperative mechanical ventilation time, postoperative hospital stay, postoperative CCU admission time, complications, mortality, recurrence | Thoracoscopic repair (n=47) Open repair (n=62) |
| Budzanowski et al.[12] | Congenital diaphragmatic hernia | Mortality, recurrence | Thoracoscopic repair (n=6) Open repair (n=5) |
CCU: Coronary care unit
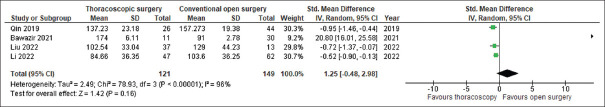
Operation time
Assessment of the operation time was performed in 4 studies, including 121 patients in the thoracoscopic surgery group and 149 patients in the conventional open surgery group. For the thoracoscopic and conventional open surgery groups, the operation time was recorded. There was significant heterogeneity between studies (P < 0.00001, I2 = 96%). The operation time varied significantly across studies. There was no significant difference (standard mean difference = 1.25, confidence interval [CI] = [−0.48–2.98], P = 0.16) in the overall effect between the groups [Figure 2].
Figure 2.
Forest plots of the association of operative time between the thoracoscopic surgery group and the conventional open surgery group for congenital diaphragmatic hernia in neonates. SD: Standard deviation, CI: Confidence interval
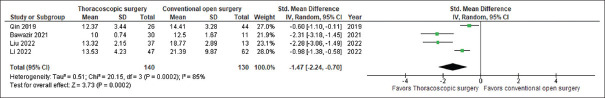
Hospital stay
Assessment of the hospital stay was performed in four studies, including 140 patients in the thoracoscopic surgery group and 130 patients in the conventional open surgery group. For the thoracoscopic and conventional open surgery groups, the hospital stay was recorded in each included study. There was significant heterogeneity between studies (P = 0.0002, I2 = 85%). The hospital stay varied significantly across studies. There was a statistically significant difference (standard mean difference = −1.47, CI [−2.24–−0.70], P < 0.001) in the overall effect between the groups [Figure 3].
Figure 3.
Forest plots of the association of hospital stay between the thoracoscopic surgery group and the conventional open surgery group for congenital diaphragmatic hernia in neonates. SD: Standard deviation, CI: Confidence interval
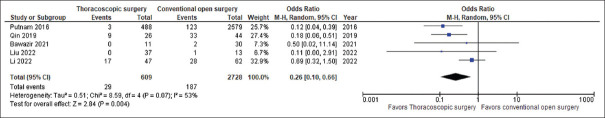
Complications
Assessment of the complications was performed in 5 studies, including 609 patients in the thoracoscopic surgery group and 2728 patients in the conventional open surgery group. For the thoracoscopic and conventional open surgery groups, the complications were recorded in each included study. The complication rate was not significant heterogeneity between studies (P = 0.07, I2 = 53%). The complication rate not varied significantly across studies. There was a statistically significant difference (odds ratio = 0.26, CI = [0.10–0.66], P = 0.004) in the overall effect between the groups [Figure 4].
Figure 4.
Forest plots of the comparison of complication rate between the thoracoscopic surgery group and the conventional open surgery group for congenital diaphragmatic hernia in neonates. CI: Confidence interval
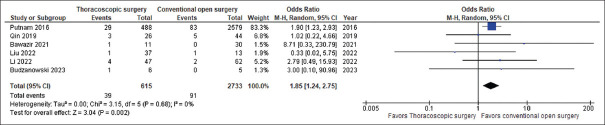
Recurrence
Assessment of the recurrence was performed in 6 studies, including 615 patients in the thoracoscopic surgery group and 2733 patients in the conventional open surgery group. For thoracoscopic and conventional open surgery groups, the recurrence was recorded in each included study. The recurrence rate was not significant heterogeneity between studies (P = 0.68, I2 = 0%). The recurrence rate not varied significantly across studies. There was a statistically significant difference (odds ratio = 1.85, CI = [1.24–2.75], P = 0.002) in the overall effect between the groups [Figure 5].
Figure 5.
Forest plots of the comparison of recurrence rate between the thoracoscopic surgery group and the conventional open surgery group for congenital diaphragmatic hernia in neonates. CI: Confidence interval
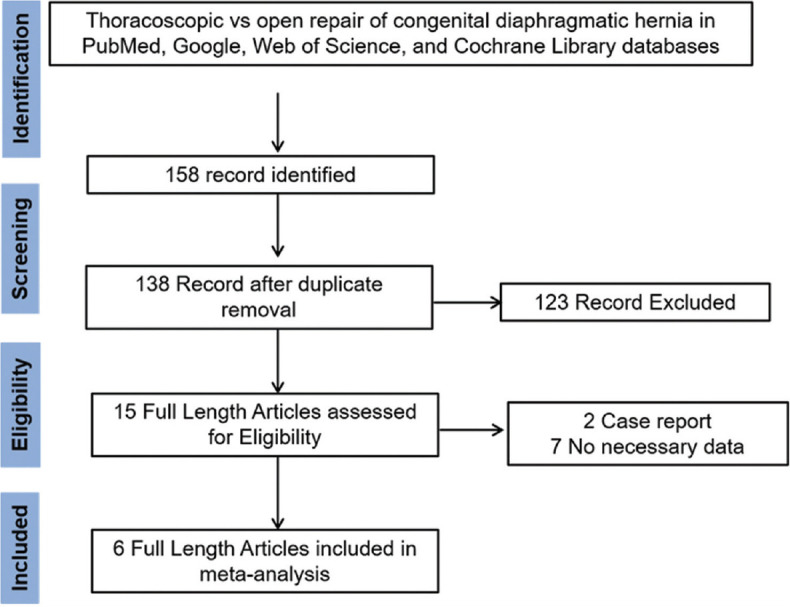
Mortality
Assessment of the mortality was performed in 6 studies, including 613 patients in the thoracoscopic surgery group and 2719 patients in the conventional open surgery group. For the thoracoscopic and conventional open surgery groups, the mortality was recorded in each included study. The mortality rate was not significant heterogeneity between studies (P = 0.90, I2 = 0%). The mortality rate not varied significantly across studies. There was a statistically significant difference (odds ratio = 0.14, CI = [0.08–0.23], P < 0.001) in the overall effect between the groups [Figure 6].
Figure 6.
Forest plots of the comparison of mortality rate between the thoracoscopic surgery group and the conventional open surgery group for congenital diaphragmatic hernia in neonates. CI: Confidence interval
DISCUSSION
The use of thoracoscopic procedures in pediatrics has increased due to recent advances in MIS. Thoracoscopic repair, first reported in 1995, is considered a new strategy for the treatment of congenital diaphragmatic hernias. Compared to open surgery, the thoracoscopic approach offers better cosmetic results and a shorter recovery time.[13,14,15] However, thoracoscopic correction of congenital diaphragmatic hernia is still controversial. Not only is the recurrence rate higher with this procedure, but also there is a risk of hypercapnia and severe acidosis due to CO2 insufflation in thoracoscopically operated patients. Therefore, the use of thoracoscopic surgery for the treatment of congenital diaphragmatic hernia must be carefully evaluated. We performed a meta-analysis of six included published papers, to evaluate the safety and efficacy of thoracoscopic surgery for congenital diaphragmatic hernia.
Meta-analysis is an effective analytical tool for compiling data from studies with low power. This meta-analysis shows that thoracoscopic surgery and conventional open surgery were compared for congenital diaphragmatic hernias in newborns. The results show that thoracoscopic surgery significantly reduces length of hospital stay, mortality, and complications while improving survival. These results indicate that thoracoscopic surgery is a relatively safe and successful surgical treatment for congenital diaphragmatic hernias. However, the meta-analysis showed that the group that underwent thoracoscopic surgery had more recurrences. Of most of the papers we analyzed, only one study showed a lower recurrence rate after thoracoscopic surgery.
Death is one of the most important potential problems after surgery. Compared to traditional open surgery, our meta-analysis shows a significantly lower rate of postoperative deaths with thoracoscopic surgery. The results we obtained were consistent with the results of a previous meta-analysis.[13,16]
In this study, total 4 of the six trials showed a significantly higher recurrence rate in the thoracoscopic surgery group. According to the pooled data, recurrences occurred in 6.34% (39 of 615) of patients who underwent thoracoscopic surgery and in 3.33% (91 of 2733) of patients who underwent open surgery. This clinical outcome may be influenced by other factors. As mentioned above, learning curves are inevitable in surgeons with insufficient experience in clinical practice. Jancelewicz et al.,[17] reported that there was a trend towards a decreased recurrence rate from 50% prior to 2008 to 25% after 2008 (P=0.26). The use of prosthetic patches also had an effect on the recurrence rate after surgery. So far, however, none of these variables has proven to be predictive of recurrence. Increased recurrence rates have been associated with thoracic repair of diaphragmatic hernias.[18,19] The International Congenital Diaphragmatic Hernia Registry has shown that patients who underwent patching had a higher risk of recurrence than patients who underwent open repair with patching.[19]
The limitations of the study were that all included studies had selection bias and no randomized studies were included. Therefore, prospective, multicentric and randomized controlled trials are required for a final judgment. The reporting and overall methodological quality of some studies were poor. In addition, the laparoscopic experience reported in the included studies could vary, and several of the included studies had relatively small sample sizes. Finally, there were significant statistical differences in the length of hospital stay and the duration of surgery.
CONCLUSION
This meta-analysis showed that thoracoscopic surgery was associated with a shorter length of hospital stay, fewer complications, and less mortality compared to standard open surgery for congenital diaphragmatic hernias in neonates. It should be noted that the thoracoscopic surgery group had a higher recurrence rate than the open surgery group. Therefore, further high-quality prospective, multicenter, randomized, and controlled studies are needed to evaluate these two surgical approaches.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.de Buys Roessingh AS, Dinh-Xuan AT. Congenital diaphragmatic hernia: Current status and review of the literature. Eur J Pediatr. 2009;168:393–406. doi: 10.1007/s00431-008-0904-x. [DOI] [PubMed] [Google Scholar]
- 2.Beresford MW, Shaw NJ. Outcome of congenital diaphragmatic hernia. Pediatr Pulmonol. 2000;30:249–56. doi: 10.1002/1099-0496(200009)30:3<249::aid-ppul9>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 3.Brownlee EM, Howatson AG, Davis CF, Sabharwal AJ. The hidden mortality of congenital diaphragmatic hernia: A 20-year review. J Pediatr Surg. 2009;44:317–20. doi: 10.1016/j.jpedsurg.2008.10.076. [DOI] [PubMed] [Google Scholar]
- 4.Silen ML, Canvasser DA, Kurkchubasche AG, Andrus CH, Naunheim KS. Video-assisted thoracic surgical repair of a foramen of Bochdalek hernia. Ann Thorac Surg. 1995;60:448–50. doi: 10.1016/0003-4975(95)00100-y. [DOI] [PubMed] [Google Scholar]
- 5.Bishay M, Giacomello L, Retrosi G, Thyoka M, Garriboli M, Brierley J, et al. Hypercapnia and acidosis during open and thoracoscopic repair of congenital diaphragmatic hernia and esophageal atresia: Results of a pilot randomized controlled trial. Ann Surg. 2013;258:895–900. doi: 10.1097/SLA.0b013e31828fab55. [DOI] [PubMed] [Google Scholar]
- 6.Putnam LR, Gupta V, Tsao K, Davis CF, Lally PA, Lally KP, et al. Factors associated with early recurrence after congenital diaphragmatic hernia repair. J Pediatr Surg. 2017;52:928–32. doi: 10.1016/j.jpedsurg.2017.03.011. [DOI] [PubMed] [Google Scholar]
- 7.Putnam LR, Tsao K, Lally KP, Blakely ML, Jancelewicz T, Lally PA, et al. Minimally invasive versus open congenital diaphragmatic hernia repair: Is there a superior approach? J Am Coll Surg. 2017;224:416–22. doi: 10.1016/j.jamcollsurg.2016.12.050. [DOI] [PubMed] [Google Scholar]
- 8.Qin J, Ren Y, Ma D. A comparative study of thoracoscopic and open surgery of congenital diaphragmatic hernia in neonates. J Cardiothorac Surg. 2019;14:118. doi: 10.1186/s13019-019-0938-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bawazir OA, Bawazir A. Congenital diaphragmatic hernia in neonates: Open versus thoracoscopic repair. Afr J Paediatr Surg. 2021;18:18–23. doi: 10.4103/ajps.AJPS_76_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu R, Zheng Z, Tang C, Zhang K, Du Q, Gong Y, et al. Thoracoscopic surgery for congenital diaphragmatic hernia in neonates: Should it be the first choice? Front Pediatr. 2022;10:1–7. doi: 10.3389/fped.2022.1020062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li H, Zhao S, Wu C, Pan Z, Wang G, Dai J. Surgical treatment of congenital diaphragmatic hernia in a single institution. J Cardiothorac Surg. 2022;17:344. doi: 10.1186/s13019-022-02098-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Budzanowski A, Loukogeorgakis S, Mullassery D, Blackburn S, Curry J, Ioannou I, et al. Thoracoscopic versus open repair of congenital diaphragmatic hernia after extracorporeal membrane oxygenation: A comparison of intra-operative data. Pediatr Surg Int. 2023;39:82. doi: 10.1007/s00383-022-05312-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tyson AF, Sola R, Jr, Arnold MR, Cosper GH, Schulman AM. Thoracoscopic versus open congenital diaphragmatic hernia repair: Single tertiary center review. J Laparoendosc Adv Surg Tech A. 2017;27:1209–16. doi: 10.1089/lap.2017.0298. [DOI] [PubMed] [Google Scholar]
- 14.Goldschlager T, Frawley G, Crameri J, Taylor R, Auldist A, Stokes K. Comparison of thoracoscopic drainage with open thoracotomy for treatment of paediatric parapneumonic empyema. Pediatr Surg Int. 2005;21:599–603. doi: 10.1007/s00383-005-1423-8. [DOI] [PubMed] [Google Scholar]
- 15.Kishan S, Bastrom T, Betz RR, Lenke LG, Lowe TG, Clements D, et al. Thoracoscopic scoliosis surgery affects pulmonary function less than thoracotomy at 2 years postsurgery. Spine (Phila Pa 1976) 2007;32:453–8. doi: 10.1097/01.brs.0000255025.78745.e6. [DOI] [PubMed] [Google Scholar]
- 16.Terui K, Nagata K, Ito M, Yamoto M, Shiraishi M, Taguchi T, et al. Surgical approaches for neonatal congenital diaphragmatic hernia: A systematic review and meta-analysis. Pediatr Surg Int. 2015;31:891–7. doi: 10.1007/s00383-015-3765-1. [DOI] [PubMed] [Google Scholar]
- 17.Jancelewicz T, Langer JC, Chiang M, Bonnard A, Zamakhshary M, Chiu PP. Thoracoscopic repair of neonatal congenital diaphragmatic hernia (CDH): Outcomes after a systematic quality improvement process. J Pediatr Surg. 2013;48:321–5. doi: 10.1016/j.jpedsurg.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 18.Schlager A, Arps K, Siddharthan R, Glenn I, Hill SJ, Wulkan ML, et al. Thoracoscopic repair of congenital diaphragmatic hernia after extracorporeal membrane oxygenation: Feasibility and outcomes. J Laparoendosc Adv Surg Tech A. 2018;28:774–9. doi: 10.1089/lap.2016.0583. [DOI] [PubMed] [Google Scholar]
- 19.Tsao K, Lally PA, Lally KP Congenital Diaphragmatic Hernia Study Group. Minimally invasive repair of congenital diaphragmatic hernia. J Pediatr Surg. 2011;46:1158–64. doi: 10.1016/j.jpedsurg.2011.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]