Abstract
Introduction:
Early operative intervention in orthopaedic injuries is associated with decreased morbidity and mortality. Relevant process measures (e.g. femoral shaft fixation <24 hours) are used in trauma quality improvement programs to evaluate performance. Currently, there is no mechanism to account for patients who are unable to undergo surgical intervention (i.e. physiologically unstable). We characterized the factors associated with patients who did not meet these orthopaedic process measures.
Methods:
A retrospective cohort study of patients from 35 ACS-COT verified Level 1 and Level 2 trauma centers was performed utilizing quality collaborative data (2017-2022). Inclusion criteria were adult patients (≥18 years), ISS ≥5, and a closed femoral shaft or open tibial shaft fracture classified via the Abbreviated Injury Scale version 2005 (AIS2005). Relevant factors (e.g. physiologic) associated with a procedural delay >24 hours were identified through a multivariable logistic regression and the effect of delay on inpatient outcomes was assessed. A sub-analysis characterized the rate of delay in “healthy patients”
Results:
We identified 5,199 patients with a femoral shaft fracture and 87.5% had a fixation procedure, of which 31.8% had a delay, and 47.1% of those delayed were “healthy.” There were 1,291 patients with an open tibial shaft fracture, 92.2% had fixation, 50.5% had an irrigation and debridement and 11.2% and 18.7% were delayed, respectively. High ISS, older age and multiple medical comorbidities were associated with a delay in femur fixation, and those delayed had a higher incidence of complications.
Conclusions:
There is a substantial incidence of surgical delays in some orthopaedic trauma process measures that are predicted by certain patient characteristics, and this is associated with an increased rate of complications. Understanding these factors associated with a surgical delay, and effectively accounting for them, is key if these process measures are to be used appropriately in quality improvement programs.
Level of Evidence:
Level III; Therapeutic/Care Management
Keywords: orthopaedic, process measures, quality improvement, trauma outcomes
INTRODUCTION
Early operative intervention of orthopaedic injuries has been proven to result in decreased mortality,1–6 reduced complication rates,2,7,8 and lower total healthcare related costs.9–11 Subsequently, appropriate orthopaedic process measures have been incorporated into both the American College of Surgeons Trauma Quality Improvement Program (ACS TQIP)12,13 and the ACS Committee on Trauma verification process.14 Currently there are seven orthopaedic process measures, including three that are assessed within 24 hours of patient arrival: 1) fixation of mid-shaft femur fractures, 2) fixation of open tibia shaft fractures and 3) operative irrigation and debridement of open tibia fractures. ACS TQIP performance reports are generated and fed back to the participating trauma centers so that local stakeholders can know where they stand in relation to their peers as well as identify and understand outlier patients that did not receive a timely operative intervention at their own institution. To accomplish these measures, it is essential to have the coordination of multiple stakeholders (e.g. trauma surgeons, anesthesiologists, orthopaedic surgeons, etc.) along with robust systems in place (e.g. operating room availability, surgical staff, etc.).9,15 As orthopaedic outcomes are currently not measured by ACS TQIP, measurement of care processes represents the best alternative means to evaluate quality, in line with the Donabedian16–18 model.
However, current reporting of orthopaedic process measures does not account for patients that are physiologically unstable or who have other extenuating issues (e.g. hemorrhagic shock, subarachnoid hemorrhage) that could preclude operative intervention within 24 hours. While the presence of resources (e.g. the availability of appropriate surgeons, operating rooms) can be addressed through performance improvement (PI) mechanisms, the existing health status of the patient at the time of injury is something that cannot be modified. As a goal of ACS TQIP is to provide credible reports with actionable information for all relevant stakeholders, it is unclear how individual centers respond to these outlier patients in their reports, especially those that might have been deemed “too unstable” for surgery. Additionally, these metrics are also utilized during trauma center verification site visits to evaluate the overall orthopaedic care provided. Interestingly, when evaluating the door-to-balloon time in patients with a myocardial infarction, the issue of which patients to include, and exclude, in this process measure has been discussed and treating centers are allowed some leeway in their patient selection.19,20 Subsequently, it might be appropriate to have a more nuanced approach to how we measure these orthopaedic process measures (e.g. times to operative interventions) in these patients and possibly consider the relevant factors that might delay care and that are beyond the control of the treating center and care team.
The goal of this study is to characterize trauma patients undergoing operative intervention (e.g., fixation, irrigation and debridement) of either closed femoral or open tibia shaft fractures and determine if there are factors (e.g. demographic, physiologic, injury) associated with delays in care. These injuries were chosen because they are each associated with substantial complications (e.g., femoral shaft fracture: mortality, ARDS; open tibia shaft fracture: infection, nonunion) and their subsequent process measures are associated with these outcomes. The secondary goal is to assess whether patients who have a delay to surgery have an increased rate of complications. Using ACS TQIP criteria, we will examine patients in a state-wide trauma collaborative to answer these two questions. We hypothesize that there are patient factors (e.g. higher injury severity, increased age) associated with delays in care. Our aim is to frame the conversation towards “risk-adjusting” of these process measures to acknowledge the heterogeneity of these patients and design an evaluation system that accounts for non-modifiable factors beyond the control of the trauma center.
METHODS
Study design and setting
This is a retrospective cohort study of trauma patients treated at 35 American College of Surgeons Committee on Trauma verified level 1 and level 2 trauma centers participating in the YYYYYYYY ABC Program (XXXXX). XXXXX is a collaborative quality initiative, funded by the Blue Cross Blue Shield of YYYYYYYY (BCBSY), which utilizes enhanced trauma registry data collection.21 In addition to standard trauma registry data, XXXXX collects additional information on outcomes, processes of care, and employs a robust data validation program.22
Data and participants
Patients with a closed femoral shaft or open tibial shaft fracture were identified using Abbreviated Injury Scale version 2005 (AIS05) codes described in the Fall 2022 ACS TQIP reporting code set. Associated fixation and irrigation and debridement procedures were based on International Classification of Diseases, Tenth Revision, Procedure Coding System (ICD-10-PCS) codes also defined in the same reporting codes set (Supplemental Digital Content 1). Patients aged ≥ 18 years with an injury severity score (ISS) of ≥ 5 who presented to a XXXXX participant trauma center between January 2017 through October 2022 with a relevant fracture were included in the study. Patients were excluded if they had been entered into the database prior to the center enrolling in XXXXX. Patients with burns, with no signs of life at initial evaluation in the Emergency Department (ED) (Systolic Blood Pressure (SBP) = 0, Pulse = 0, Glasgow Coma Scale Score (GCS) = 3), patients who died in the ED or died during their hospital admission, those who were not admitted, and those who were transferred from another hospital were excluded.23 Additionally, patients with a hospital length of stay less than 12 hours were also excluded.
Data collection and data definitions
Data collection was performed using the existing trauma registry at participating hospitals with a modular add-on for XXXXX specific data. XXXXX publishes a data definitions dictionary, based upon the National Trauma Data Standard (NTDS), which is available online and updated annually. Trauma registrars and data abstractors from participating centers undergo training in XXXXX and NTDS data definitions. Data are transmitted to the coordinating center at two-month intervals. Each XXXXX center undergoes an annual data validation audit.22
Analysis
The primary outcome of this study was the proportion of patients who had a delay of a relevant orthopaedic procedure (e.g., fixation or irrigation and debridement) greater than 24 hours. For each linked diagnosis-surgery group (e.g., mid-shaft femur fractures-fixation) the time to surgery was calculated based on the patient’s arrival at the emergency department to the start of surgery. Patients that had both a femur fracture and an open tibia fracture were analyzed separately in each appropriate category. A univariate analysis was performed to describe differences between the delay and non-delayed groups. A multivariable logistic regression was used to evaluate any relevant factors that were associated with a delay to surgery. This model included 25 co-variates: age, sex, race, insurance, admission during weekend, trauma center level, admitting service, Injury Severity Score, AIS regions, ED systolic blood pressure, ED heart rate, GCS Motor, intubation, smoking status, hypertension, anti-coagulant usage, functionally dependent health status, pre-hospital cardiac arrest, disseminated cancer, blood transfusion and chronic renal failure. The variables for the regression were chosen after we analyzed the univariate analyses and used a forward stepwise selection process with the variables that were potentially correlated with delay (p<0.2). We then added co-variates that are clinically and demographically important that could be expected to be on the causal pathway. These covariates chosen are consistent with the stated hypothesis and are consistent with other trauma outcomes studies.4,24–30
A sub-analysis was also performed to assess the proportion of patients delayed to surgery who were deemed to be “healthy,” i.e. patients who were physiologically stable and likely able to undergo an operative intervention. This sub-analysis was designed to capture patients that were presumably delayed due to trauma center structural issues, e.g. surgeon staffing, OR availability, etc. These patients were defined as being non-hypotensive (Emergency Department Systolic Blood Pressure> 90 mmHg), lacking serious head injury (Head AIS < 3), ISS < 15, no pre-injury use of anti-coagulant medication, no procedures within first 24 hours, and no ICU stay.
The secondary outcome was to determine if the patients who had a delay to surgery had a higher rate of complications (e.g., Pneumonia, Acute Respiratory Distress Syndrome, Deep Vein Thrombosis, Pulmonary Embolism, Stroke/Cerebral Vascular Accident, Ventilator Associated Pneumonia, Unplanned return to ICU, Unplanned Intubation) or overall hospital length of stay compared to those who were not delayed.
Average values were expressed as the mean ± standard deviation. All statistical tests were two-sided. Statistical significance was defined as a p-value of less than 0.05. Statistical analyses were performed using Stata 15.1 (StataCorp, College Station, TX).
This study was submitted to the University of YYYYYYYY Medical School Institutional Review Board and given a determination of “not regulated” status as secondary use of existing data from a quality assurance and quality improvement clinical activity. Secondary use of XXXXX data has been approved by the YYYYYYYY Medicine IRB under application HUM00041947. We followed the STROBE guidelines in this retrospective, cross-sectional study utilizing observational cohort data.31
RESULTS
There were 467,435 trauma patients in the XXXXX database and after inclusion/exclusion criteria were applied, 6,375 patients were left for the final analysis. We identified 5,199 patients with a femoral shaft fracture and 1,291 patients with an open tibial shaft fracture (some patients had both injuries) (Figure 1). Of the patients with a femoral shaft fracture, 4,550 (87.5%) had a fixation procedure, and of those who underwent surgery, 1,445 (31.8%) had an operative delay > 24 hours (Table 1). Of the patients that had a surgical delay, 681 (47.1%) were deemed to be “healthy” by our criteria. Of the patients with an open tibial shaft fracture, 1,190 (92.2%) had a fixation procedure and 652 (50.5%) had an irrigation and debridement, and of those who underwent surgery, 133 (11.2%) and 122 (18.7%) had an operative delay > 24 hours of their respective procedures. Of the open tibia fracture patients that had a surgical delay, 27 (20.3%) fixation and 13 (10.7%) irrigation and debridement were deemed to be “healthy” by our criteria.
Figure 1.
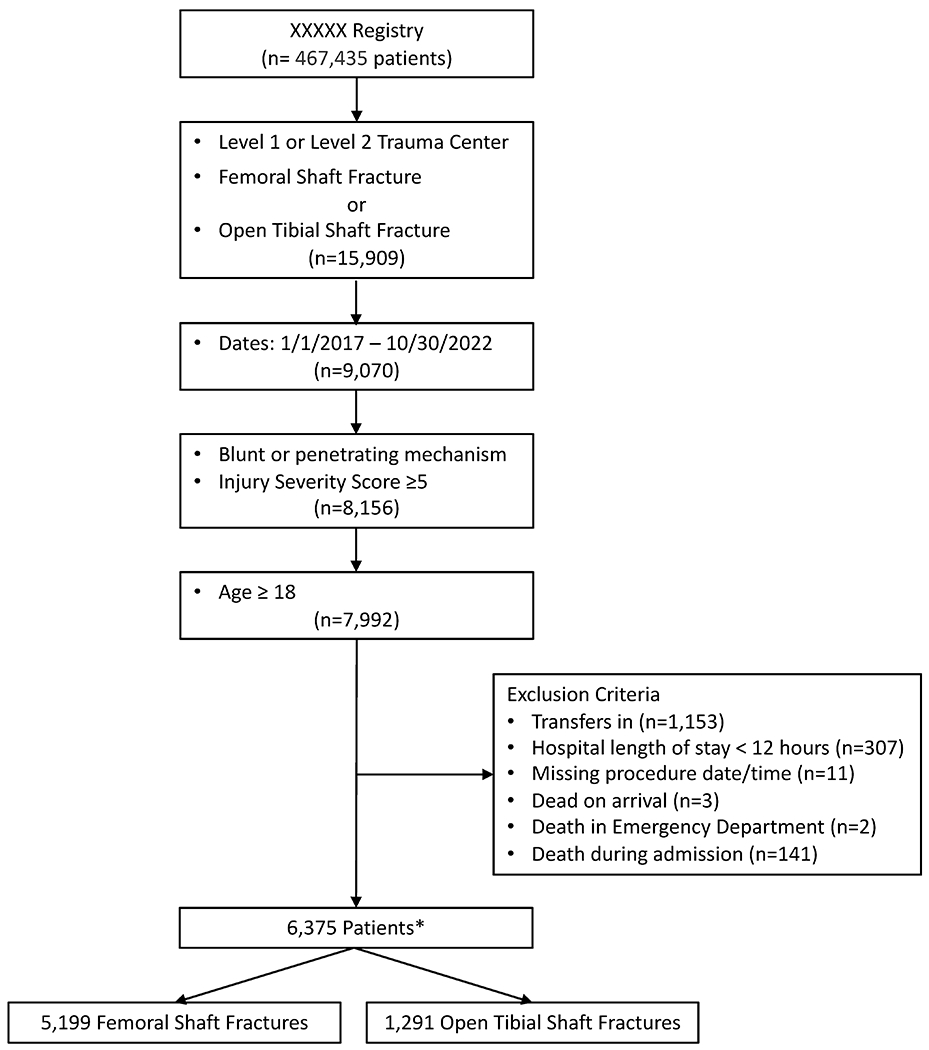
Patient Cohort Inclusion and Exclusion Criteria
XXXXX, YYYYYYYY ABC Program
Some patients had both types of fractures
Table 1.
Orthopaedic Procedures Performed and Surgical Delays
| Total Injuries (n) and Associated Procedures | Total Procedures Performed, n (%) | Surgical Patients with Delay > 24 Hours, n (% of Total Procedures) | “Healthy” Surgical Patients with Delay > 24 Hours, n (% of Delayed Patients) |
|---|---|---|---|
| Femoral Shaft Fracture (5,199) | |||
| Operative Stabilization | 4,550 (87.5) | 1,445 (31.8) | 681 (47.1) |
| Open Tibial Shaft Fracture (1,291) | |||
| Operative Stabilization | 1,190 (92.2) | 133 (11.2) | 27 (20.3) |
| Irrigation and Debridement | 652 (50.5) | 122 (18.7) | 13 (10.7) |
In a univariate analysis of patients with a femur fracture who had a surgical delay > 24 hours, patients tended to be older, female, white, insured, intubated and have a significant head or neck injury along with more medical comorbidities compared to those who did not have a surgical delay (Table 2). For patients with open tibia fractures, patients who had a surgical delay tended to have higher ISS scores, be intubated but largely did not show a difference in medical comorbidities compared to those without a surgical delay (Table 3).
Table 2.
Femoral Shaft Fracture Patients Undergoing Surgical Fixation (n=4,550)
| Variable | Patients without Surgical Delay (n=3,105) | Patients with Surgical Delay > 24 hrs (n=1,445) | p-value |
|---|---|---|---|
| Mean Age (SD) | 51.4 (24.7) | 66.9 (22.4) | <0.001 |
| Age (%) | <0.001 | ||
| 18-25y | 19.2 | 7.3 | |
| 26-45y | 28.2 | 13.0 | |
| 46-65y | 17.7 | 16.6 | |
| 65-75y | 11.8 | 17.8 | |
| >75y | 23.1 | 45.3 | |
| Male (%) | 53.5 | 41.5 | <0.001 |
| Race (%) | <0.001 | ||
| White | 69.5 | 80.9 | |
| Black | 25.9 | 15.9 | |
| Other | 4.6 | 3.2 | |
| Uninsured (%) | 6.4 | 3.2 | <0.001 |
| Trauma Center Level (%) | <0.001 | ||
| 1 | 44.5 | 38.0 | |
| 2 | 55.5 | 62.0 | |
| Injury Severity Score (%) | <0.001 | ||
| 5-15 | 81.5 | 85.8 | |
| 15-24 | 11.9 | 5.8 | |
| 24-35 | 5.2 | 5.1 | |
| >35 | 1.4 | 3.3 | |
| AIS Head/neck>2 (%) | 4.1 | 5.5 | 0.038 |
| AIS Face>2 (%) | 0.3 | 0.6 | 0.12 |
| AIS Chest>2 (%) | 10.2 | 8.9 | 0.19 |
| AIS Abdomen>2 (%) | 3.9 | 4.2 | 0.64 |
| AIS Extremity>2 (%) | 100.0 | 100.0 | |
| AIS External>2 (%) | 0.2 | 0.2 | 0.73 |
| ED Heart Rate (%) | 0.002 | ||
| 51-120, bpm | 90.8 | 88.9 | |
| > 120 | 5.9 | 5.3 | |
| 0-50 | 0.7 | 1.2 | |
| Missing | 2.6 | 4.6 | |
| ED Systolic Blood Pressure (%) | <0.001 | ||
| > 90, mmHg | 93.7 | 91.2 | |
| 61-90 | 3.3 | 3.3 | |
| ≤ 60 | 0.5 | 0.4 | |
| Missing | 2.5 | 5.1 | |
| Glasgow Coma Scale Motor (%) | <0.001 | ||
| 1 | 1.1 | 2.3 | |
| 2-5 | 3.0 | 3.5 | |
| 6 | 90.5 | 84.8 | |
| Missing | 5.4 | 9.4 | |
| Intubated (%) | 4.5 | 6.9 | <0.001 |
| Comorbid diseases (%) | |||
| Active chemotherapy | 0.5 | 1.2 | 0.003 |
| Advanced directive limiting care | 3.3 | 7.5 | <0.001 |
| Alcohol use disorder | 6.1 | 6.0 | 0.83 |
| Angina | 0.3 | 1.0 | 0.005 |
| Bleeding risk | 8.2 | 21.5 | <0.001 |
| Cerebrovascular accident | 1.8 | 4.2 | <0.001 |
| COPD | 5.5 | 9.1 | <0.001 |
| Chronic renal failure | 0.5 | 2.2 | <0.001 |
| Congestive heart failure | 4.1 | 11.1 | <0.001 |
| Current smoker | 26.6 | 16.3 | <0.001 |
| Dementia | 7.3 | 15.3 | <0.001 |
| Diabetes mellitus | 10.2 | 17.6 | <0.001 |
| Disseminated cancer | 0.5 | 1.8 | <0.001 |
| Drug use disorder | 26.0 | 14.6 | <0.001 |
| Functionally dependent health status | 18.7 | 40.4 | <0.001 |
| History of myocardial infarction | 0.4 | 0.8 | 0.065 |
| Hypertension requiring medication | 31.1 | 55.1 | <0.001 |
| Liver disease | 0.6 | 0.7 | 0.75 |
| Major psychiatric illness | 22.5 | 24.4 | 0.16 |
| Obesity | 2.4 | 1.8 | 0.17 |
| Peripheral vascular disease | 1.8 | 3.7 | <0.001 |
| Steroid use | 2.0 | 3.5 | 0.004 |
AIS, Abbreviated Injury Scale; ED, Emergency Department; COPD, Chronic Obstructive Pulmonary Disease
Table 3.
Open Tibia Shaft Fracture Patients Undergoing Surgical Fixation (n=1,190) or Irrigation and Debridement (n=652)
| Variable | Surgical Fixation (n=1,190) | p-value | Irrigation and Debridement (n=652) | p-value | ||
|---|---|---|---|---|---|---|
| Patients without Surgical Delay (n=1,057) |
Patients with Surgical Delay > 24 hrs (n=133) |
Patients without Surgical Delay (n=530) |
Patients with Surgical Delay > 24 hrs (n=122) |
|||
| Mean Age (SD) | 41.3 (17.4) | 42.6 (18.4) | 0.45 | 41.7 (18.1) | 42.9 (16.1) | 0.50 |
| Age (%) | 0.083 | 0.25 | ||||
| 18-25y | 20.7 | 16.5 | 21.9 | 13.9 | ||
| 26-45y | 41.5 | 45.1 | 39.2 | 46.7 | ||
| 46-65y | 28.4 | 23.3 | 27.9 | 27.9 | ||
| 65-75y | 4.7 | 9.8 | 5.5 | 7.4 | ||
| >75y | 4.6 | 5.3 | 5.5 | 4.1 | ||
| Male (%) | 72.3 | 70.7 | 0.70 | 70.4 | 79.5 | 0.043 |
| Race (%) | 0.19 | 0.36 | ||||
| White | 62.9 | 54.9 | 59.4 | 54.1 | ||
| Black | 32.6 | 39.1 | 35.1 | 41.8 | ||
| Other | 4.4 | 6.0 | 5.5 | 4.1 | ||
| Uninsured (%) | 11.0 | 8.3 | 0.34 | 10.2 | 9.0 | 0.70 |
| Trauma Center Level (%) | 0.046 | 0.34 | ||||
| 1 | 48.7 | 57.9 | 59.2 | 63.9 | ||
| 2 | 51.3 | 42.1 | 40.8 | 36.1 | ||
| Injury Severity Score (%) | 0.002 | 0.014 | ||||
| 5-15 | 78.1 | 66.2 | 74.0 | 61.5 | ||
| 15-24 | 14.1 | 16.5 | 17.2 | 20.5 | ||
| 24-35 | 5.4 | 12.0 | 5.7 | 11.5 | ||
| >35 | 2.4 | 5.3 | 3.2 | 6.6 | ||
| AIS Head/neck>2 (%) | 7.0 | 16.5 | <0.001 | 8.5 | 14.8 | 0.035 |
| AIS Face>2 (%) | 0.2 | 1.5 | 0.014 | 0.4 | 0.8 | 0.52 |
| AIS Chest>2 (%) | 12.0 | 17.3 | 0.084 | 14.3 | 23.0 | 0.019 |
| AIS Abdomen>2 (%) | 4.2 | 6.8 | 0.17 | 4.9 | 7.4 | 0.27 |
| AIS Extremity>2 (%) | 100.0 | 100.0 | 100.0 | 100.0 | ||
| AIS External>2 (%) | 0.3 | 0.0 | 0.54 | 0.4 | 0.8 | 0.52 |
| ED Heart Rate (%) | 0.16 | 0.12 | ||||
| 51-120, bpm | 89.3 | 82.7 | 88.7 | 82.0 | ||
| > 120 | 8.7 | 14.3 | 9.1 | 16.4 | ||
| 0-50 | 0.9 | 1.5 | 1.1 | 0.8 | ||
| Missing | 1.1 | 1.5 | 1.1 | 0.8 | ||
| ED Systolic Blood Pressure (%) | 0.40 | 0.95 | ||||
| > 90, mmHg | 93.8 | 94.7 | 92.6 | 93.4 | ||
| 61-90 | 4.6 | 3.0 | 5.5 | 4.9 | ||
| ≤ 60 | 0.6 | 0.0 | 0.6 | 0.8 | ||
| Missing | 1.0 | 2.3 | 1.3 | 0.8 | ||
| Glasgow Coma Scale Motor (%) | 0.050 | 0.43 | ||||
| 1 | 1.8 | 5.3 | 2.3 | 4.9 | ||
| 2-5 | 3.5 | 3.8 | 4.5 | 4.9 | ||
| 6 | 91.8 | 86.5 | 90.4 | 86.9 | ||
| Missing | 2.9 | 4.5 | 2.8 | 3.3 | ||
| Intubated (%) | 7.8 | 15.8 | 0.002 | 9.6 | 16.4 | 0.030 |
| Comorbid diseases (%) | ||||||
| Active chemotherapy | 0.1 | 0.8 | 0.081 | 0.2 | 0.8 | 0.26 |
| Advanced directive limiting care | 0.2 | 2.3 | <0.001 | 0.6 | 0.8 | 0.75 |
| Alcohol use disorder | 10.9 | 15.0 | 0.15 | 11.1 | 11.5 | 0.91 |
| Angina | 0.3 | 0.0 | 0.54 | 0.0 | 0.8 | 0.037 |
| Bleeding risk | 3.8 | 5.3 | 0.41 | 4.5 | 4.9 | 0.85 |
| Cerebrovascular accident | 0.5 | 0.8 | 0.67 | 0.8 | 1.6 | 0.36 |
| COPD | 4.0 | 3.0 | 0.59 | 3.2 | 4.9 | 0.36 |
| Chronic renal failure | 0.6 | 0.0 | 0.38 | 0.4 | 0.0 | 0.50 |
| Congestive heart failure | 2.6 | 2.3 | 0.79 | 2.8 | 4.1 | 0.46 |
| Current smoker | 37.7 | 38.3 | 0.88 | 35.7 | 41.8 | 0.20 |
| Dementia | 0.7 | 0.8 | 0.91 | 0.6 | 0.0 | 0.40 |
| Diabetes mellitus | 7.1 | 6.0 | 0.64 | 5.8 | 9.8 | 0.11 |
| Disseminated cancer | 0.0 | 0.8 | 0.005 | 0.0 | 0.8 | 0.037 |
| Drug use disorder | 36.2 | 45.1 | 0.046 | 36.4 | 47.5 | 0.023 |
| Functionally dependent health status | 4.8 | 7.5 | 0.18 | 4.7 | 7.4 | 0.23 |
| History of myocardial infarction | 0.2 | 0.0 | 0.62 | 0.4 | 0.0 | 0.50 |
| Hypertension requiring medication | 17.4 | 18.0 | 0.86 | 18.5 | 19.7 | 0.76 |
| Liver disease | 0.7 | 0.0 | 0.35 | 0.9 | 0.8 | 0.90 |
| Major psychiatric illness | 19.9 | 18.0 | 0.62 | 18.1 | 23.0 | 0.22 |
| Obesity | 2.8 | 2.3 | 0.70 | 3.8 | 4.1 | 0.87 |
| Peripheral vascular disease | 1.7 | 1.5 | 0.87 | 1.9 | 1.6 | 0.85 |
| Steroid use | 1.3 | 0.0 | 0.18 | 0.8 | 0.8 | 0.94 |
AIS, Abbreviated Injury Scale; ED, Emergency Department; COPD, Chronic Obstructive Pulmonary Disease
The multivariable analysis of patients with a femoral shaft fracture yielded a C-statistic of 0.73 and identified characteristics associated with a delay to surgery (Table 4). Having an ISS of >35 [OR 2.64, p=0.012] and being intubated [OR 2.59, p<0.001] was associated with having a surgical delay, while an ISS below 35 was not a significant factor. In patients older than 45, there was a significant risk of a delayed surgery with odds increasing from 2.32 (p<0.001) (46-65 years old) to 3.37 (p<0.001) (>75 years old). Multiple medical comorbidities were also relative factors in patients with a delay, including hypertension, anti-coagulant use, functionally dependent health status, cancer and chronic renal failure. Interestingly, receiving a blood transfusion was more likely in patients who did not have a delay in their femur fixation surgery.
Table 4.
Characteristics of femoral shaft fracture patients with a surgical fixation delay
| Variable | Odds Ratio and 95% CI | p-value |
|---|---|---|
| Age | ||
| 18-25y | (reference) | |
| 26-45y | 1.32 (0.93-1.85) | 0.117 |
| 46-65y | 2.32 (1.64-3.28) | <0.001 |
| 65-75y | 3.14 (2.24-4.40) | <0.001 |
| >75y | 3.37 (2.23-5.10) | <0.001 |
| Male | 1.07 (0.93-1.24) | 0.328 |
| Race | ||
| White | (reference) | |
| Black | 0.90 (0.73-1.10) | 0.293 |
| Other | 0.86 (0.55-1.35) | 0.522 |
| Uninsured | 0.77 (0.51-1.17) | 0.225 |
| Trauma Center Level | ||
| 1 | (reference) | |
| 2 | 0.98 (0.69-1.39) | 0.903 |
| Admitting Service | ||
| Trauma | (reference) | |
| Orthopedics | 0.67 (0.44-1.02) | 0.064 |
| Other | 1.32 (0.95-1.84) | 0.104 |
| Weekend Admission | 0.95 (0.80-1.13) | 0.568 |
| Injury Severity Score | ||
| 5-15 | (reference) | |
| 15-24 | 0.80 (0.54-1.18) | 0.252 |
| 24-35 | 1.30 (0.72-2.35) | 0.392 |
| >35 | 2.64 (1.24-5.61) | 0.012 |
| AIS Head/neck>2 | 1.27 (0.81-1.98) | 0.304 |
| AIS Face>2 | 0.98 (0.41-2.38) | 0.970 |
| AIS Chest>2 | 1.00 (0.65-1.54) | 0.983 |
| AIS Abdomen>2 | 1.53 (0.96-2.42) | 0.073 |
| AIS External>2 | 1.55 (0.22-11.00) | 0.659 |
| ED Systolic Blood Pressure | ||
| > 90, mmHg | (reference) | |
| 61-90 | 1.07 (0.78-1.47) | 0.679 |
| ≤ 60 | 0.90 (0.30-2.69) | 0.846 |
| Missing | 1.89 (0.78-4.57) | 0.156 |
| ED Heart Rate | ||
| 51-120, bpm | (reference) | |
| > 120 | 1.26 (0.92-1.71) | 0.150 |
| 0-50 | 1.28 (0.68-2.41) | 0.442 |
| Missing | 0.63 (0.30-1.31) | 0.217 |
| Glasgow Coma Scale Motor (%) | ||
| 1 | (reference) | |
| 2-5 | 0.65 (0.38-1.11) | 0.114 |
| 6 | 0.69 (0.40-1.20) | 0.192 |
| Missing | 0.76 (0.41-1.40) | 0.375 |
| Intubated | 2.59 (1.72-3.90) | <0.001 |
| Current smoker | 0.88 (0.71-1.08) | 0.212 |
| Hypertension requiring medication | 1.32 (1.10-1.58) | 0.003 |
| Anti-coagulant Use | 1.70 (1.39-2.07) | <0.001 |
| Functionally dependent health status | 1.59 (1.34-1.88) | <0.001 |
| Pre-hospital cardiac arrest | 3.30 (0.41-26.41) | 0.260 |
| Disseminated cancer | 2.13 (1.19-3.83) | 0.011 |
| Blood transfusion | 0.54 (0.41-0.72) | <0.001 |
| Chronic renal failure | 2.43 (1.09-5.41) | 0.029 |
AIS, abbreviated injury scale; ED, emergency department.
In the multivariable analysis of patients with an open tibia fracture, those that were 65-75 years old, other race and had received a blood transfusion were associated with delays to fixation, while those that were uninsured were less likely to have a delay to surgery. In open tibia patients undergoing a debridement, ages (26-45 and 65-75), male sex, receiving a blood transfusion and having functionally dependent health status were associated with a delay to surgery. The C-statistic of these models were 0.66 and 0.72 respectively (Supplemental Digital Content 2).
In patients with a femur fracture, those that had a delay in care had more complications (Table 5). Compared to those without a delay, these patients had a significantly higher rate of pneumonia (3.5% vs 1.5%, p<0.001), ventilator assisted pneumonia (2.1% vs. 0.9%, p<0.001), unplanned ICU admission (4.2% vs. 2.1%, p<0.001) and a longer length of stay (8.4 days vs. 6.7 days, p<0.001). While femur fracture fixation patients with a delay did have a higher complication rate of Acute Respiratory Distress Syndrome (ARDS), venothromboembolic events, stroke and unplanned intubation, these differences were not statistically significant.
Table 5.
Complications in Patients with a Femoral Shaft Fracture
| Complication, n (%) | Patients with Surgical Delay > 24 hours (n=1445) | Patients without Surgical Delay > 24 hours (n=3105) | p-value |
|---|---|---|---|
| Pneumonia | 51 (3.5) | 47 (1.5) | <0.001 |
| ARDS | 11 (0.8) | 11 (0.4) | 0.065 |
| DVT/PE | 29 (2.0) | 39 (1.3) | 0.052 |
| Stroke/CVA | 8 (0.6) | 13 (0.4) | 0.53 |
| VAP | 31 (2.1) | 27 (0.9) | <0.001 |
| Return to ICU | 61 (4.2) | 66 (2.1) | <0.001 |
| Unplanned Intubation | 13 (0.9) | 17 (0.5) | 0.17 |
| Outcome | |||
| Hospital LOS, mean days (SD) | 8.4 (7.5) | 6.7 (6.7) | <0.001 |
ARDS, Acute Respiratory Distress Syndrome; DVT, Deep Vein Thrombosis; PE, Pulmonary Embolism; VAP, Ventilator Assisted Pneumonia; ICU, Intensive Care Unit
DISCUSSION
In this study, we found that a substantial portion of patients (31.8%) with a femur fracture had a delay to surgical fixation of greater than 24 hours. Of those that had a surgical delay, almost half of them were deemed to be “healthy,” or otherwise should have been able to undergo a fixation procedure. Highly injured patients, older age and multiple medical comorbidities were factors predictive of femur fracture patients not undergoing surgical fixation within 24 hours. In open tibia fracture patients, having an older age receiving a blood transfusion were the common factors that predicted a delay in either operative fixation or a formal irrigation and debridement procedure. Patients with a delay to surgery were also more likely to develop some serious complications and have a longer hospital length of stay.
The ACS TQIP orthopaedic process measures were designed to evaluate major orthopaedic injuries based on widely accepted interventions and their respective timeframes. Multiple studies have shown that the early fixation (within 24 hours) of a femoral shaft fracture results in decreased mortality.1,5,8,32 and fewer complications.2,7,8 In this study, almost one-third of patients with a femur fracture did not have surgery within a day, and those with a delay also had a higher rate of complications. While only half of the patients with an open tibia fracture had a documented irrigation and debridement of their injury, it is possible that this procedure was performed during the fixation surgery, but not coded. It should also be noted that newer evidence is shifting more towards the importance of early antibiotic administration and less on urgent irrigation and debridement,33–35 however the majority of these patients were not delayed in their procedures. Nevertheless, it is essential that we understand the reasons for these delays if we are to improve the care that is delivered.
Based on the multivariable analysis, we can characterize a phenotype of a femur fracture patient (e.g. older, high ISS, medical comorbidities) that is likely to have a delay in surgical fixation. Subsequently, it might be reasonable to assume that these patients were deemed “too sick to operate,” even for a temporizing damage control type procedure (e.g. external fixator).3,32,36,37 Including these patients in the reporting for this measure, together with those who are stable for surgery, is problematic as it creates a heterogeneous group for the analysis. This issue has been acknowledged in myocardial infarction patients receiving a percutaneous coronary intervention (PCI) within 90 minutes, as some patients are excluded from the denominator of this process measure based on their risk factors.19,20 It might be reasonable to have a similar approach to trauma process measures and exclude the patients who are known to not be candidates for timely operative intervention. Also, by defining a homogenous cohort from the start, this might encourage more stakeholder buy-in and lessen the risk of creating a set-up-to-fail situation where the vested parties are asked to do something beyond their control (i.e. operate on a patient who cannot tolerate surgery).38
The limitations of this study should be acknowledged. This was a retrospective review of previously collected trauma registry data. It is unclear why all femoral shaft fractures did not receive a fixation procedure as this injury is almost never treated non-operatively. It is possible that some of these patients were coded as a shaft fracture, however they might have had some involvement of either the proximal or distal component, such that the coded operative procedure pertained to the non-shaft portion of the injury. While a small proportion of open tibia fractures did not have an associated fixation procedure, it is reasonable that some of these fractures were treated without surgical fixation. It is also reasonable to believe that the reason that roughly half of open tibia fractures did not have a formal irrigation and debridement coded, is because that happened in conjunction with the fixation procedure. We also did not assess complications in the open tibia group (e.g. infections, nonunions) as these outcomes almost always occur after discharge and are not captured in the current trauma registry structure. We were also limited by the granularity of the data, and thus there could be other factors not included in the trauma registry data that could have better delineated a “healthy” patient. Lastly, while mortality is an important outcome, we excluded patients who died during their admission from the analysis as we felt that we would be unable to discern whether their injuries or other confounding factors influenced non-operative or delayed treatment.
A strength of this study is that it utilizes the diagnosis and procedure codes that are used by ACS TQIP so that these results should be similar to the reports that are fed back to participating trauma centers and should describe the patients captured in these process measures. Also, this data is from 35 level 1 and level 2 ACS COT verified trauma centers that represent multiple health systems across a state and are dispersed across rural and urban environments in both academic and non-academic practice settings. Further, these two diagnoses, and their respective treatments, are both very common and relevant orthopaedic conditions that often affect the cadence of the patient’s care and their length of stay. However, it is reasonable that some of these patients simply will not be medically stable or able to tolerate these procedures within the first 24 hours of their admission. Thus, if we are to include all patients (stable and unstable) in these process measures, we are creating a situation whereby centers and their respective care teams are being evaluated and scored based on factors outside their control, i.e. including patients who cannot have a procedure within 24 hours. Further, as some entities are beginning to use process measures in pay-for-performance initiatives, this might be another reason to consider which patients are included in the denominator of these calculations. We should also examine mechanisms to adjudicate the reasons when patients do not meet these timed measures and potentially further elucidate a trauma patient phenotype that is too sick to include.
In conclusion, this study showed that a substantial proportion of patients with a femoral shaft fracture had a delay to fixation beyond 24 hours and had an increased rate of complications. A high ISS, increasing age and medical comorbidities were predictive factors for a patient having a delay to surgery with the first day, however we also found a substantial number of patients who did not have discernable reason for their delay, likely indicating a local system issue at the trauma center that could be addressed through PI audit mechanisms. As we continue to use process measures to evaluate the quality of orthopaedic care delivered at trauma centers, we should pause and evaluate which patients we include in the denominator of this calculation.
Supplementary Material
SDC 3. STROBE Checklist
SDC 1. Fall 2022 ACS TQIP Reporting Code Set
SDC 2. Characteristics of Open Tibia Shaft Fracture Patients with a Surgical Fixation or Irrigation and Debridement Delay
Social Media.
Media summary: We should understand the reasons why some trauma patients don’t meet orthopaedic process measures if we are going to use these metrics to benchmark centers. Are the patients too sick, or is it something else?
Hashtags: #orthotwitter, #processmeasure, #trauma
Social Media Handles:
Center for Healthcare Outcomes & Policy - @UMichCHOPFellow
Institute for Healthcare Policy and Innovation - @UM_IHPI
Anna Miller - @AnnaMillerMD
Molly Jarman - @MollyJarman
John W. Scott - @DrJohnScott
Bryant W. Oliphant - @BonezNQuality
Funding:
Bryant W. Oliphant and this study were supported by a National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health grant K23-AR079565. John W. Scott was supported by grants K08-HS028672 and R01-HS027788 from the Agency for Healthcare Research and Quality. Mark R. Hemmila was supported by a Blue Cross Blue Shield of Michigan and Blue Care Network Collaborative Quality Initiatives grant and a Michigan Department of Health and Human Services to administer the Michigan Trauma Quality Improvement Program.
The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest: All Journal of Trauma and Acute Care Surgery disclosure forms have been supplied and are provided as supplemental digital content.
This paper will be an oral presentation at the 37th EAST Annual Scientific Assembly on January 12, 2024 in Orlando, Florida. It has not been submitted for publication elsewhere.
REFERENCES
- 1.Bone LB, McNamara K, Shine B, et al. Mortality in multiple trauma patients with fractures. The Journal of Trauma: Injury, Infection, and Critical Care 1994; 37: 262 4-discussion 264-5. [DOI] [PubMed] [Google Scholar]
- 2.Pincus D, Ravi B, Wasserstein D, et al. Association Between Wait Time and 30-Day Mortality in Adults Undergoing Hip Fracture Surgery. Jama 2017; 318: 1994 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giannoudis PV, Pape HC. Damage control orthopaedics in unstable pelvic ring injuries. Inj 2004; 35: 671 677. [DOI] [PubMed] [Google Scholar]
- 4.deMeireles AJ, Gerhardinger L, Oliphant BW, et al. Factors associated with optimal patient outcomes after operative repair of isolated hip fractures in the elderly. Trauma Surg Acute Care Open 2020; 5: e000630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cantu RV, Graves SC, Spratt KF. In-hospital mortality from femoral shaft fracture depends on the initial delay to fracture fixation and Injury Severity Score: a retrospective cohort study from the NTDB 2002-2006. J Trauma Acute Care 2014; 76: 1433 1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nyholm AM, Gromov K, Palm H, et al. Time to Surgery Is Associated with Thirty-Day and Ninety-Day Mortality After Proximal Femoral Fracture: A Retrospective Observational Study on Prospectively Collected Data from the Danish Fracture Database Collaborators. J Bone Jt Surg 2015; 97: 1333 1339. [DOI] [PubMed] [Google Scholar]
- 7.Forsythe RM, Peitzman AB, DeCato T, et al. Early lower extremity fracture fixation and the risk of early pulmonary embolus: filter before fixation? J Trauma Inj Infect Critical Care 2011; 70: 1381 1388. [DOI] [PubMed] [Google Scholar]
- 8.Lefaivre KA, Starr AJ, Stahel PF, et al. Prediction of pulmonary morbidity and mortality in patients with femur fracture. J Trauma 2010; 69: 1527 35; discussion 1535-6. [DOI] [PubMed] [Google Scholar]
- 9.Childs BR, Vallier HA. Cost savings associated with a multidisciplinary protocol that expedites definitive fracture care. American journal of orthopedics (Belle Mead, NJ) 2014; 43: 309 315. [PubMed] [Google Scholar]
- 10.Vallier HA, Dolenc AJ, Moore TA. Early Appropriate Care: A Protocol to Standardize Resuscitation Assessment and to Expedite Fracture Care Reduces Hospital Stay and Enhances Revenue. J Orthop Trauma 2016; 30: 306–311. [DOI] [PubMed] [Google Scholar]
- 11.Bone LB, Johnson KD, Weigelt J, et al. Early versus delayed stabilization of femoral fractures. A prospective randomized study. J bone Jt Surg Am Vol 1989; 71: 336–40. [PubMed] [Google Scholar]
- 12.Nathens AB, Cryer HG, Fildes J. The American College of Surgeons Trauma Quality Improvement Program. Surg Clin North Am 2012; 92: 441–54, x–xi. [DOI] [PubMed] [Google Scholar]
- 13.Hemmila MR, Nathens AB, Shafi S, et al. The Trauma Quality Improvement Program: pilot study and initial demonstration of feasibility. J Trauma 2010; 68: 253–62. [DOI] [PubMed] [Google Scholar]
- 14.Trauma AC of SC on. Resources for Optimal Care of the Injured Patient. 2014. [Google Scholar]
- 15.Langford JR, Burgess AR, Liporace FA, et al. Pelvic fractures: Part 1. Evaluation, classification, and resuscitation. J Am Acad Orthop Sur 2013; 21: 448–457. [DOI] [PubMed] [Google Scholar]
- 16.Moore L, Lavoie A, Bourgeois G, et al. Donabedian’s structure-process-outcome quality of care model. J Trauma Acute Care 2015; 78: 1168–1175. [DOI] [PubMed] [Google Scholar]
- 17.Ayanian JZ, Markel H. Donabedian’s Lasting Framework for Health Care Quality. New Engl J Medicine 2016; 375: 205–7. [DOI] [PubMed] [Google Scholar]
- 18.Donabedian A. Evaluating the quality of medical care. 1966. Blackwell Publishing, Inc., 2005. Epub ahead of print 2005. DOI: 10.1111/j.1468-0009.2005.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mheen PJM de, Nallamothu BK. Exclusions in the denominators of process-based quality measures: the missing link in understanding performance or ecological fallacy? BMJ Qual Saf 2017; 26: 169. [DOI] [PubMed] [Google Scholar]
- 20.Bruckel J, Liu X, Hohmann SF, et al. The denominator problem: national hospital quality measures for acute myocardial infarction. BMJ Qual Saf 2017; 26: 189. [DOI] [PubMed] [Google Scholar]
- 21.Hemmila MR, Jakubus JL, Cain-Nielsen AH, et al. The Michigan Trauma Quality Improvement Program: Results from a collaborative quality initiative. J Trauma Acute Care 2017; 82: 867–876. [DOI] [PubMed] [Google Scholar]
- 22.Jakubus JL, Pasquo SLD, Mikhail JN, et al. Pull back the curtain: External data validation is an essential element of quality improvement benchmark reporting. J Trauma Acute Care 2020; 89: 199–207. [DOI] [PubMed] [Google Scholar]
- 23.Calland JF, Nathens AB, Young JS, et al. The effect of dead-on-arrival and emergency department death classification on risk-adjusted performance in the American College of Surgeons Trauma Quality Improvement Program. J Trauma Acute Care 2012; 73: 1086–1092. [DOI] [PubMed] [Google Scholar]
- 24.Perl VJU, Leroux B, Cook MR, et al. Damage-control resuscitation and emergency laparotomy. J Trauma Acute Care Surg 2016; 80: 568–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coimbra R, Allison-Aipa T, Zachary B, et al. A comprehensive analysis of 30-day readmissions after emergency general surgery procedures: Are risk factors modifiable? J Trauma Acute Care Surg 2023; 94: 61–67. [DOI] [PubMed] [Google Scholar]
- 26.Oliphant BW, Tignanelli CJ, Napolitano LM, et al. American College of Surgeons Committee on Trauma verification level affects trauma center management of pelvic ring injuries and patient mortality. J Trauma Acute Care 2019; 86: 1–10. [DOI] [PubMed] [Google Scholar]
- 27.Tignanelli CJ, Joseph B, Jakubus JL, et al. Variability in management of blunt liver trauma and contribution of level of American College of Surgeons Committee on Trauma verification status on mortality. J Trauma Acute Care 2018; 84: 273–279. [DOI] [PubMed] [Google Scholar]
- 28.Haas B, Gomez D, Hemmila MR, et al. Prevention of complications and successful rescue of patients with serious complications: characteristics of high-performing trauma centers. J Trauma Inj Infect Critical Care 2011; 70: 575–582. [DOI] [PubMed] [Google Scholar]
- 29.Hemmila MR, Cain-Nielsen AH, Jakubus JL, et al. Association of Hospital Participation in a Regional Trauma Quality Improvement Collaborative With Patient Outcomes. Jama Surg 2018; 153: 747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Newgard CD, Fildes JJ, Wu L, et al. Methodology and Analytic Rationale for the American College of Surgeons Trauma Quality Improvement Program. J Am Coll Surg 2013; 216: 147–157. [DOI] [PubMed] [Google Scholar]
- 31.Vandenbroucke JP, Elm E von, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. PLoS Med 2007; 4: e297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Morshed S, Miclau T, Bembom O, et al. Delayed internal fixation of femoral shaft fracture reduces mortality among patients with multisystem trauma. J Bone Jt Surg 2009; 91: 3–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lack WD, Karunakar MA, Angerame MR, et al. Type III Open Tibia Fractures. J Orthop Trauma 2015; 29: 1–6. [DOI] [PubMed] [Google Scholar]
- 34.Rozell JC, Connolly KP, Mehta S. Timing of Operative Debridement in Open Fractures. Orthop Clin N Am 2017; 48: 25–34. [DOI] [PubMed] [Google Scholar]
- 35.Pollak AN, Jones AL, Castillo RC, et al. The Relationship Between Time to Surgical Débridement and Incidence of Infection After Open High-Energy Lower Extremity Trauma. J Bone Jt Surg 2010; 92: 7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scalea TM, Boswell SA, Scott JD, et al. External fixation as a bridge to intramedullary nailing for patients with multiple injuries and with femur fractures: damage control orthopedics. The Journal of Trauma: Injury, Infection, and Critical Care 2000; 48: 613 21-discussion 621-3. [DOI] [PubMed] [Google Scholar]
- 37.Rixen D, Grass G, Sauerland S, et al. Evaluation of criteria for temporary external fixation in risk-adapted damage control orthopedic surgery of femur shaft fractures in multiple trauma patients: “evidence-based medicine” versus “reality” in the trauma registry of the German Trauma Society. The Journal of trauma 2005; 59: 1375 94-discussion 1394-5. [DOI] [PubMed] [Google Scholar]
- 38.Manzoni J-F, Barsoux J-L. The Set-Up-To-Fail Syndrome. Harvard Business Review, 1998 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SDC 3. STROBE Checklist
SDC 1. Fall 2022 ACS TQIP Reporting Code Set
SDC 2. Characteristics of Open Tibia Shaft Fracture Patients with a Surgical Fixation or Irrigation and Debridement Delay


