Abstract
Objective
China has a serious burden of Postpartum depression (PPD). In order to improve the current situation of high burden of PPD, this study explores the factors affecting PPD from the multidimensional perspectives with physiology, family support and social support covering the full-time chain of pre-pregnancy–pregnancy–postpartum.
Methods
A follow-up survey was conducted in the Qujing First People’s Hospital of Yunnan Province from 2020 to 2022, and a total of 4838 pregnant women who underwent antenatal checkups in the hospital were enrolled as study subjects. Mothers were assessed for PPD using the Edinburgh Postnatal Depression Scale (EPDS), and logistic regression was used to analyse the level of mothers’ postnatal depression and identify vulnerability characteristics.
Results
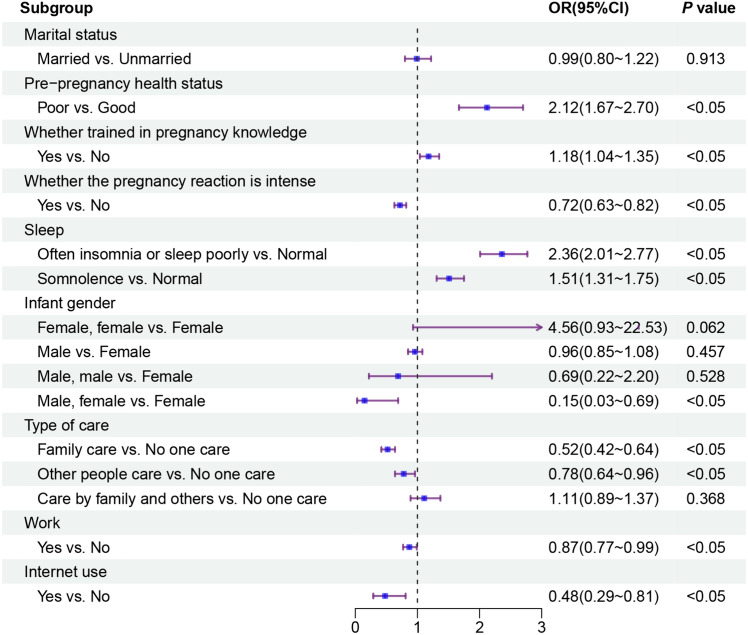
The prevalence of mothers’ PPD was 46.05%, with a higher prevalence among those who had poor pre-pregnancy health, had sleep problems during pregnancy, and only had a single female fetus. In the family support dimension, only family care (OR = 0.52, 95% CI 0.42–0.64) and only other people care(OR = 0.78, 95% CI 0.64–0.96) were the protective factors of PPD. The experience risk of PPD was higher among mothers who did not work or use internet.
Conclusion
The PPD level in Yunnan Province was significantly higher than the global and Chinese average levels. Factors affecting mothers’ PPD exist in all time stages throughout pregnancy, and the influence of family support and social support on PPD shouldn’t be ignored. There is an urgent need to extend the time chain of PPD, move its prevention and treatment forward and broaden the dimensions of its intervention.
Keywords: Postpartum depression, Risk factors, Family support, Social support
Introduction
Postpartum depression (PPD) is caused by a combination of factors in the pre-pregnancy, pregnancy, and postpartum periods. It is one of the most prevalent and disabling but most underappreciated complications in women of childbearing age [1]. PPD not only leads to mothers’ morbidity in forms of guilt, fatigue, loss of appetite and sleep disorder. It also adversely affects the health and well-being of the newborn, partners and other family members, disrupting infant care and family dynamics [2]. PPD is experienced by women around the world, making it an important public health issue [3]. Globally, about 10–15% of the mothers suffered PPD in the postpartum period, while the prevalence of PPD was about 9.4% to 27.4% in China [4]. PPD is not only affected by physiological factors such as changes in hormone and immune levels but also affected by traditional Chinese fertility culture [5]. Chinese mothers are subject to higher levels of family and social intervention. Moreover, 40% of women who have experienced PPD will experience depression again in their lifetime; nearly 50% will experience PPD again in subsequent pregnancies [6].
Mothers are vulnerable to depression due to a combination of psychological and social attributes [7, 8]. In the case of depression, mothers’ treatment options are limited by the potential adverse effects of medications on the baby [9]. Therefore, early preconception identification, intervention and elimination of risk factors for PPD are particularly important for both mothers and newborns. However, previous studies have mostly focused on capturing risk factors for mothers’ depression during pregnancy and postpartum [10–13], without fully considering the time-cumulative characteristics of PPD, lacking analyses of factors such as pre-pregnancy health and pre-pregnancy preparation, and the nodes of concern have not covered the full chain of the pregnancy cycle. It was also found that previous studies have explicitly explored the mechanism of physiological factors influencing PPD [14, 15], and although some studies have also paid attention to the impact of multidimensional factors such as family support and social risk on PPD [16, 17], the mechanisms of influence remain unclear.
Generally, this study takes pre-pregnancy, pregnancy and post-pregnancy as analysis nodes to identify the vulnerability gap of PPD in the whole-time chain, comprehensively considers the multi-attribute characteristics of the disease, and explores the influencing mechanism of PPD based on multiple dimensions of socio-demographic, family support and social support.
Methods
Study sample
The study subjects were pregnant women undergoing prenatal care at Qujing First People’s Hospital Inclusion Criteria: have reading comprehension and communication skills, voluntarily participate in the survey and complete the questionnaire. Exclusion criteria: stillbirth, birth defects, miscarriage, lack of information, etc. The total of 4838 participants were included in this study after deleting missing values and abnormal values.
Questionnaire and content
A self-designed questionnaire was used to collect demographic data on pregnant women and information on depression during postpartum. The demographic data of pregnant women include: residence, marital status, pre-pregnancy health status, whether trained in pregnancy knowledge, whether the pregnancy reaction is intense, single or double fetus, sleep, gestational weeks of childbirth, depression score, infant gender, infant birth weight, type of care, work, and Internet use.
Screening tools for PPD
Depressive symptoms are assessed using the EPDS, which is widely used to screen for PPD. The scale assesses the intensity of depressive symptoms in the past 7 days, and contains a total of 10 items, each of which is divided into “never”, “occasionally”, “often”, and “always” according to the intensity of depressive symptoms, corresponding to “0 points”, “1 point”, “2 points”, and “3 points”. The total score ranges from 0 to 30 points, and the higher the score, the more severe the depressive symptoms. In this study, participants were divided into depressive (≥ 12) and non-depressive (< 12) groups using 12 points as cut-off values.
Model variable
The dependent variable in this study was PPD.
The covariates included in this study were socio-demographic factors (residence and marital status), pre-pregnancy factors (pre-pregnancy health status and whether trained in pregnancy knowledge), pregnancy factors (whether the pregnancy reaction is intense, single or double fetus, sleep, and gestational weeks of childbirth), postpartum factors (gender of the infant, birth weight of the infant), family support factors (type of care), and social support factors (work and internet use).
Statistical analysis
The study used SPSS 22.0 for descriptive statistics analysis. Firstly, each risk factor was individually tested for variability. Secondly, using logistic regression model, all significant risk factors were subjected to multivariate logistic regression, in order to assess the risk factors for PPD. The results of the study were expressed as odds ratio (OR) and 95% confidence interval (CI). A p-value of less than 5% was considered statistically significant in all tests.
Results
Sample characteristics
Table 1 presents the basic information of all participants. More than half of the participants lived in the city (67.16%); participants’ marital status was mostly married (88.90%). 92.35% of the participants reported having good pre-pregnancy health conditions; the percentage of attending pregnancy knowledge training was relatively balanced, with 58.60% of participants attending and 41.40% not attending. In the pregnancy period, about one-third of the participants reported that they had severe pregnancy reactions (34.15%); only a small percentage of the mothers gave birth to double fetuses (1.84%); the percentage of the participants who had normal sleep was 59.1%, while 18.44% often insomnia or sleep poorly and 22.53% somnolence; and the majority of the mothers gave birth at full term (93.12%). In the postpartum period, the prevalence of PPD was 46.05%, single fetus only with the gender of the infant was female or male was more prevalent in the variable of the infant gender, their values respectively were 47.15% and 52.07%, and the majority of the newborns weighed from 2.5 to 4.5 kg (90.51%). In the family support and social support dimensions, the types of care were more prevalent in the type only by family members and only by other people, at 32.68% and 32.74% respectively; about half of the participants went to work (56.24%); and 98.51% of the participants reported going online.
Table 1.
Basic information of the participants in this study
| Dimension | Variables | Frequency | Component ratio (%) | |
|---|---|---|---|---|
| Demographic characteristics | Residence | Rural | 1589 | 32.84 |
| Urban | 3249 | 67.16 | ||
| Marital status | Unmarried | 537 | 11.10 | |
| Married | 4301 | 88.90 | ||
| Pre-pregnancy | Pre-pregnancy health status | Good | 4468 | 92.35 |
| Poor | 370 | 7.65 | ||
| Whether trained in pregnancy knowledge | No | 2003 | 41.40 | |
| Yes | 2835 | 58.60 | ||
| Pregnancy | Whether the pregnancy reaction is intense | No | 3186 | 65.85 |
| Yes | 1652 | 34.15 | ||
| Single or double fetus | Single fetus | 4749 | 98.16 | |
| double fetus | 89 | 1.84 | ||
| Sleep | Normal | 2856 | 59.03 | |
| Often insomnia or sleep poorly | 892 | 18.44 | ||
| Somnolence | 1090 | 22.53 | ||
| Gestational weeks of childbirth | Term birth | 4505 | 93.12 | |
| Preterm birth | 310 | 6.41 | ||
| Post-term birth | 23 | 0.47 | ||
| Postpartum | Depression | No | 2610 | 53.95 |
| Yes | 2228 | 46.05 | ||
| Infant gender | Female | 2281 | 47.15 | |
| Female, female | 10 | 0.20 | ||
| Male | 2519 | 52.07 | ||
| Male, male | 13 | 0.27 | ||
| Male, female | 15 | 0.31 | ||
| Infant birth weight | Normal weight | 4379 | 90.51 | |
| Low birth weight | 337 | 6.97 | ||
| Overweight | 122 | 2.52 | ||
| Family support | Type of care | No one care | 517 | 10.69 |
| Family care | 1581 | 32.68 | ||
| Other people care | 1584 | 32.74 | ||
| Care by family and others | 1156 | 23.89 | ||
| Social support | Work | No | 2117 | 43.76 |
| Yes | 2721 | 56.24 | ||
| Internet use | No | 72 | 1.49 | |
| Yes | 4766 | 98.51 | ||
Postpartum depression profiles
In the total sample (n = 4838), 2610 (53.95%) mothers had an EPDS score of < 12 and 2228 (46.05%) had an EPDS score ≥ 12. Therefore, the prevalence of PPD was 46.05%.
Table 2 presents the association of sociodemographic, family support and social support dimensions factors with PPD. Grouped by marital status, the prevalence of PPD was 51.40% in the unmarried group and 45.38% in the married group. The prevalence of PPD was higher in women with excessively low and excessively high family support, women cared by only family members and only others were relatively less affected by PPD. Women with low social support experienced higher levels of PPD and those who had social support experienced less depression, this is related to the shift from family to society of women’s attention.
Table 2.
Conditions of PPD in different dimensions of sociodemographic–family support–social support (N = 4838)
| Variable | Non-postpartum depression | Postpartum depression | P |
|---|---|---|---|
| N (%) | N (%) | ||
| Residence | |||
| Rural | 877 (55.19) | 712 (44.81) | 0.225 |
| Urban | 1733 (53.34) | 1516 (46.66) | |
| Marital status | |||
| Unmarried | 261 (48.60) | 276 (51.40) | P < 0.05 |
| Married | 2349 (54.62) | 1952 (45.38) | |
| Type of care | |||
| No one care | 235 (45.45) | 282 (54.55) | P < 0.05 |
| Family care | 1017 (64.33) | 564 (35.67) | |
| Other people care | 844 (53.28) | 740 (46.72) | |
| Care by family and others | 514 (44.46) | 642 (55.54) | |
| Work | |||
| No | 1090 (51.49) | 1027 (48.51) | P < 0.05 |
| Yes | 1520 (55.86) | 1201 (44.14) | |
| Internet use | |||
| No | 22 (30.56) | 50 (69.44) | P < 0.05 |
| Yes | 2588 (54.30) | 2178 (45.70) | |
Table 3 presents the relationship between factors and PPD throughout pregnancy. The PPD prevalence of the women with good pre-pregnancy health was 44.49% and it was 64.86% of those with poor pre-pregnancy health; the prevalence of PPD was higher in women with pregnancy knowledge training (48.71%), compared with that in those without training. The experience risk of PPD was lower in women with severe pregnancy reactions (43.04%) than in women with normal pregnancy reactions (47.61%); and it was lower in women with normal sleep, relative to those with frequent insomnia or poor sleep (61.32%), and somnolence (51.74%). In infant gender, the prevalence of PPD was particularly high among women with double fetuses that both infant gender were female (80.00%).
Table 3.
Conditions of PPD throughout the entire pregnancy period (N = 4838)
| Variable | Non-postpartum depression | Postpartum depression | P |
|---|---|---|---|
| N (%) | N (%) | ||
| Pre-pregnancy health status | |||
| Good | 2480 (55.51) | 1988 (44.49) | P < 0.05 |
| Poor | 130 (35.14) | 240 (64.86) | |
| Whether trained in pregnancy knowledge | |||
| No | 1156 (57.71) | 847 (42.29) | P < 0.05 |
| Yes | 1454 (51.29) | 1381 (48.71) | |
| Whether the pregnancy reaction is intense | |||
| No | 1669 (52.39) | 1517 (47.61) | P < 0.05 |
| Yes | 941 (56.96) | 711 (43.04) | |
| Single or double fetus | |||
| Single fetus | 2561 (53.93) | 2188 (46.07) | 0.832 |
| Double fetuses | 49 (55.06) | 40 (44.94) | |
| Sleep | |||
| Normal | 1739 (60.89) | 1117 (39.11) | P < 0.05 |
| Often insomnia or sleep poorly | 345 (38.68) | 547 (61.32) | |
| Somnolence | 526 (48.26) | 564 (51.74) | |
| Gestational weeks of childbirth | |||
| Term birth | 2435 (54.05) | 2070 (45.95) | 0.778 |
| Preterm birth | 164 (52.90) | 146 (47.10) | |
| Post-term birth | 11 (47.83) | 12 (52.17) | |
| Infant gender | |||
| Female | 1225 (53.70) | 1056 (46.30) | P < 0.05 |
| Female, female | 2 (20.00) | 8 (80.00) | |
| Male | 1362 (54.10) | 1157 (45.93) | |
| Male, male | 8 (61.54) | 5 (38.46) | |
| Male, female | 13 (86.67) | 2 (13.33) | |
| Infant birth weight | |||
| Normal weight | 2364 (53.98) | 2015 (46.02) | 0.124 |
| Low birth weight | 171 (50.74) | 166 (49.26) | |
| Overweight | 75 (61.48) | 47 (38.52) | |
Binary logistic regression analysis of influencing factors of PPD
Figure 1 shows the results of binary logistic regression analysis of socio-demographic, whole pregnancy, family support, and social support dimensions with PPD. In the sociodemographic dimension, the marital status of married and unmarried did not show a significant difference. In the pre-pregnancy period, women with poor pre-pregnancy health were 2.12 times more likely to experience PPD than the reference category (good pre-pregnancy health); women who received pregnancy knowledge training (OR = 1.18, 95% CI 1.04–1.35) had a higher experience risk of PPD compared to the reference group. In the pregnancy period, intense pregnancy reactions were a protective factor against PPD for women; having normal sleep was important in protecting women from depression. Compared to the experience risk of PPD in women with normal sleep, those who had often insomnia or sleep poorly were 2.36 times more likely to occur, and those who had somnolence were 1.51 times more likely to occur. In the postpartum period, the variable of infant gender showed a significant difference between only single female fetus and double fetuses with one male and one female infant, double fetuses with one male and one female infant (OR = 0.15, 95% CI 0.03–0.69) was a protective factor against mothers’ PPD compared to single fetus with female infant. In the family support dimension, being cared only by family members (OR = 0.52, 95% CI 0.42–0.64) and being cared only by other people (OR = 0.78, 95% CI 0.64–0.96) were protective factors for PPD compared to being cared by no one, and women cared by no one were more susceptible to the effects of PPD. The variables in the social support dimension were all significantly different, the women who lack social support were more likely to be affected by PPD, and going to work (OR = 0.87, 95% CI 0.77–0.99), going online (OR = 0.48, 95% CI 0.29–0.81) were protective factors for women’s PPD.
Fig. 1.
Risk factor analysis for PPD in sociodemography–whole pregnancy–family support–social support dimension
Discussion
We assessed the prevalence of PPD in Yunnan Province, China, and explored the associations between the full-time chain of pre-pregnancy–pregnancy–postpartum, sociodemographic–family support–social support, and PPD. We also expanded the time chain of PPD research, breaking through the causal mechanism of PPD occurrence beyond just physiological or social dimension. We realised the dynamic capture of PPD under the full-time chain, and mapped the vulnerability characteristics atlas of PPD from a multidimensional perspective. The study revealed a high prevalence of 46.1% for PPD in Yunnan Province, which is significantly higher than global (17.22%) and Chinese regional (21.4%) averages [18, 19]. Similar trends were observed when side-by-side comparing with cities such as Shanghai (23.2%) and Guangzhou (27.37%) [20, 21]. Traditional Chinese cultural beliefs regarding unique family dynamics and gender roles may lead to increased family conflicts and closed social networks [22], while China’s rapid economic growth has escalated life stress and elongated work hours [23]. Yunnan Province’s economy is relatively underdeveloped and the scarcity of healthcare resources led to mental health issues being easily neglected. In this study, the average age of childbearing for women was 34 years old. Considering the higher age of childbearing, concerns over medical risks contribute to an increased psychological burden [24]. These factors all contributed to the severe situation of PPD in Yunnan Province. Based on the full-time chain perspective, the PPD prevalence was higher among mothers with poor pre-pregnancy health (64.86%) and sleep problems during pregnancy (often insomnia, sleep poorly: 61.32%; somnolence: 51.74%); and mothers with double fetuses of one male and one female infant had better mental health status after giving birth. In the multidimensional analysis, only family care and only other people care were positive factors for PPD in the family support dimension; going to work or going online had a protective effect on mothers’ health.
Prevention and treatment of PPD should focus on the whole pre-pregnancy–pregnancy–postpartum period and extend the intervention chain.
The PPD experience risk of women with poor pre-pregnancy health was (2.12 times) higher than women with good. This result is consistent with the findings of Michael W. O'Hara et al. [25]. In the pre-pregnancy period, mothers had a previous depression history or possible comorbidities such as hypertension, diabetes, gynecological disorders, with a low physical health level [26, 27]; and in the postpartum period, they suffered from fatigue, pain in wounds, and weakness [28, 29]. The multiple discomforts superimposition makes mothers more prone to postpartum psychiatric problems, such as anxiety, depression, and despondency. Notably, mothers with pregnancy knowledge training were more likely to experience PPD. The possible reason is the mothers with pregnancy knowledge training were more aware of the psychological and physiological changes, that occur during pregnancy and the postpartum period, and they were more likely to think what may cause unnecessary tension, anxiety, and uneasiness [30, 31]. And this increased the PPD experience risk. During the pregnancy period, often insomnia or sleep poorly/somnolence hurt mothers; Some studies have indicated that mothers who sleep 6 h or less were more likely to experience PPD, and sleeping more than 8 h did not significantly decrease the PPD prevalence [32]. The major neurotransmitter systems in the brain involved in regulating sleep have been linked to the development of psychiatric disorders [33]. Therefore, neurotransmitter imbalances can lead to PPD increase. In the postpartum period, twin births of a male and a female infant were a protective factor compared to having only single female infant. In the context of traditional Chinese fertility culture, family members may show some negative reactions to female infants’ birth, that may result in less support for mothers giving birth to a female fetus; whereas a preference for male fetus may be communicated to mothers, and ease their postpartum stress [34]. Additionally, lower marital satisfaction following the birth of female fetus may explain for the increased risk of PPD among the mothers with female fetus. Family members should be well-informed about pregnancy-related matters and offer psychological support to pregnant women. mothers need to maintain a healthy lifestyle and engage in activities that alleviate stress. After childbirth, the focus should shift from solely preventing PPD to prevention and treatment. Nursing interventions are provided to mothers without PPD. Receiving prompt follow-up visits and developing personalized treatment plans is crucial for individuals who have suffered from PPD.
The prevention and treatment of PPD are inseparable from the dual support of family and society, with social support playing an increasingly prominent role.
In terms of family support, only family care and only other care were protective factors of PPD. Family care is the main resource of family support [35]. Family not only provides tangible support such as material and financial support, but also offer mental support from family members, especially husbands, which greatly enhances mothers’ self-esteem and self-confidence, alleviating tension and stress during various pregnancy stages. In addition to family members, medical personnel, friends and colleagues also influence mothers by providing information support, emotional accompaniment and value recognition [36, 37]. In terms of social support, going to work or going online can reduce the risk of PPD, it not only increases mothers’ self-efficacy, but also provides the understanding and appreciation they need as they transition to motherhood [38]. The social climate in social networks reflects a stigma associated with mental health problems, which acts as a barrier to seeking professional help for mothers. However, positive social behaviours can enhance cognitive abilities of mental health problems, overcome perceptual barriers and help-seeking intentions, and reduce the stigma of mental illness [39]. Family support for mothers should encompass emotional, informational, material, and interactive aspects, focusing on recognizing emotional shifts, providing comfort, sharing childcare knowledge, and ensuring effective communication. Communities ought to deliver holistic primary health care, including early detection, education, and postpartum support. The government should consider establishing childcare allowances and creating job opportunities to facilitate mothers’ societal reintegration post-birth.
Acknowledgements
Each author contributed to the concept, design, research, data analysis, drafting of the article. I have obtained written permission from all authors.
Author contributions
Conceptualization: Dingyun You and Ye Li; Analysis and interpretation of data: Mengmei Liu and Min Li; Statistical analysis: Ping Chen and Xinwei Liu; Writing - Original Draft: Yiyun Zhang; Critical revision of the manuscript for important intellectual content: Dingyun You; Funding acquisition: Dingyun You; Visualization and Acquisition of data: Guanghong Yan and Qingyan Ma.All authors reviewed the manuscript.
Funding
This study was supported by National Natural Science Foundation of China (Grant Nos. 82073569, 81960592), Outstanding Youth Science Foundation of Yunnan Basic Research Project (Grant No. 202001AW070021), Reserve Talent Project for Young and Middle-aged Academic and Technical Leaders (Grant No. 2012005AC160023), Key Science Foundation of Yunnan Basic Research (Grant No. 202101AS070040).
Data availability
The data that support the findings of this study are available on request from the corresponding author.
Declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethics approval and consent to participate
This study was approved by the Medical Ethics Committee of Kunming Medical University (protocol number: KMMU2020MEC056). All participants received the informed consent form for this study, including a detailed explanation of the research.
Footnotes
Dingyun You is the first corresponding author of this study and Ye Li is the second corresponding author of this study.
Contributor Information
Ye Li, Email: liye8459@163.com.
Dingyun You, Email: youdingyun@qq.com.
References
- 1.Guo P, Xu D, Liew Z et al (2021) Adherence to traditional Chinese postpartum practices and postpartum depression: a cross-sectional study in Hunan, China. Front Psychiatry 12:649972. 10.3389/fpsyt.2021.649972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang W, Li G, Wang D et al (2023) Postpartum depression literacy in Chinese perinatal women: a cross-sectional study. Front Psychiatry 14:1117332. 10.3389/fpsyt.2023.1117332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lanjewar S, Nimkar S, Jungari S (2021) Depressed motherhood: prevalence and covariates of maternal postpartum depression among urban mothers in India. Asian J Psychiatry 57:102567. 10.1016/j.ajp.2021.102567 [DOI] [PubMed] [Google Scholar]
- 4.Stewart DE, Robertson E, Phil M et al (2003) Postpartum depression: literature review of risk factors and interventions. University Health Network Women’s Health Program for Toronto Public Health, Toronto [Google Scholar]
- 5.Hendrick V, Altshuler LL, Suri R (1998) Hormonal changes in the postpartum and implications for postpartum depression. Psychosomatics 39:93–101. 10.1016/S0033-3182(98)71355-6 [DOI] [PubMed] [Google Scholar]
- 6.Tebeka S, Strat YL, Higgons ADP et al (2021) Prevalence and incidence of postpartum depression and environmental factors: the IGEDEPP cohort. J Psychiatr Res 138:366–374. 10.1016/j.jpsychires.2021.04.004 [DOI] [PubMed] [Google Scholar]
- 7.Huang S, Xiao M, Hu Y et al (2023) Attitudes toward seeking professional psychological help among Chinese pregnant women: a cross-sectional study. J Affect Disord 322:163–172. 10.1016/j.jad.2022.11.034 [DOI] [PubMed] [Google Scholar]
- 8.Zhou X, Liu H, Li X, Zhang S (2021) Fear of childbirth and associated risk factors in healthy pregnant women in northwest of China: a cross-sectional study. Psychol Res Behav Manag 14:731–741. 10.2147/PRBM.S309889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davanzo R, Copertino M, De Cunto A et al (2011) Antidepressant drugs and breastfeeding: a review of the literature. Breastfeed Med 6:89–98. 10.1089/bfm.2010.0019 [DOI] [PubMed] [Google Scholar]
- 10.Wu M, Li X, Feng B et al (2014) Poor sleep quality of third-trimester pregnancy is a risk factor for postpartum depression. Med Sci Monitor 20:2740–2745. 10.12659/MSM.891222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stickel S, Eickhoff SB, Habel U et al (2021) Endocrine stress response in pregnancy and 12 weeks postpartum—exploring risk factors for postpartum depression. Psychoneuroendocrinology 125:105122. 10.1016/j.psyneuen.2020.105122 [DOI] [PubMed] [Google Scholar]
- 12.Min W, Nie W, Song S et al (2020) Associations between maternal and infant illness and the risk of postpartum depression in rural China: a cross-sectional observational study. Int J Environ Res Public Health 17:9489. 10.3390/ijerph17249489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee L-C, Hung C-H (2022) Women’s trajectories of postpartum depression and social support: a repeated-measures study with implications for evidence-based practice. Worldviews Evid-Based Nurs 19:121–129. 10.1111/wvn.12559 [DOI] [PubMed] [Google Scholar]
- 14.Markhus MW, Skotheim S, Graff IE et al (2013) Low Omega-3 index in pregnancy is a possible biological risk factor for postpartum depression. PLoS ONE 8:e67617. 10.1371/journal.pone.0067617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mikoteit T, Von Felten N, Hoesli I et al (2020) P.355 delayed increase of perinatally downregulated serum brain-derived neurotrophic factor concentrations may be a risk factor of postpartum depression. Eur Neuropsychopharmacol 40:S207. 10.1016/j.euroneuro.2020.09.270 [Google Scholar]
- 16.Angley M, Divney A, Magriples U, Kershaw T (2015) Social support, family functioning and parenting competence in adolescent parents. Matern Child Health J 19:67–73. 10.1007/s10995-014-1496-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cho H, Lee K, Choi E et al (2022) Association between social support and postpartum depression. Sci Rep 12:3128. 10.1038/s41598-022-07248-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Z, Liu J, Shuai H et al (2021) Mapping global prevalence of depression among postpartum women. Transl Psychiatry 11:1–13. 10.1038/s41398-021-01663-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu X, Wang S, Wang G (2022) Prevalence and risk factors of postpartum depression in women: a systematic review and meta-analysis. J Clin Nurs 31:2665–2677. 10.1111/jocn.16121 [DOI] [PubMed] [Google Scholar]
- 20.Deng A-W, Xiong R-B, Jiang T-T et al (2014) Prevalence and risk factors of postpartum depression in a population-based sample of women in Tangxia Community, Guangzhou. Asian Pac J Trop Med 7:244–249. 10.1016/S1995-7645(14)60030-4 [DOI] [PubMed] [Google Scholar]
- 21.Liu Y, Guo N, Li T et al (2020) Prevalence and associated factors of postpartum anxiety and depression symptoms among women in Shanghai, China. J Affect Disord 274:848–856. 10.1016/j.jad.2020.05.028 [DOI] [PubMed] [Google Scholar]
- 22.Tang L, Zhu R, Zhang X (2016) Postpartum depression and social support in China: a cultural perspective. J Health Commun 21:1055–1061. 10.1080/10810730.2016.1204384 [DOI] [PubMed] [Google Scholar]
- 23.Nie P, Otterbach S, Sousa-Poza A (2015) Long work hours and health in China. China Econ Rev 33:212–229. 10.1016/j.chieco.2015.02.004 [Google Scholar]
- 24.Xiong R, Deng A (2020) Incidence and risk factors associated with postpartum depression among women of advanced maternal age from Guangzhou, China. Perspect Psychiatr Care 56:316–320. 10.1111/ppc.12430 [DOI] [PubMed] [Google Scholar]
- 25.O’Hara MW, McCabe JE (2013) Postpartum depression: current status and future directions. Annu Rev Clin Psychol 9:379–407. 10.1146/annurev-clinpsy-050212-185612 [DOI] [PubMed] [Google Scholar]
- 26.Miller ES, Peri MR, Gossett DR (2016) The association between diabetes and postpartum depression. Arch Womens Ment Health 19:183–186. 10.1007/s00737-015-0544-x [DOI] [PubMed] [Google Scholar]
- 27.Riggin L (2020) Association between gestational diabetes and mental illness. Can J Diabetes 44:566. 10.1016/j.jcjd.2020.06.014 [DOI] [PubMed] [Google Scholar]
- 28.McCarter-Spaulding D, Shea S (2016) Effectiveness of discharge education on postpartum depression. MCN Am J Matern-Child Nurs 41:168–172. 10.1097/NMC.0000000000000236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schaffir J, Kunkler A, Lynch CD et al (2018) Association between postpartum physical symptoms and mood. J Psychosomat Res 107:33–37. 10.1016/j.jpsychores.2018.02.003 [DOI] [PubMed] [Google Scholar]
- 30.Shimizu A, Nishiumi H, Okumura Y, Watanabe K (2015) Depressive symptoms and changes in physiological and social factors 1 week to 4 months postpartum in Japan. J Affect Disord 179:175–182. 10.1016/j.jad.2015.03.036 [DOI] [PubMed] [Google Scholar]
- 31.Yu C-Y, Hung C-H, Huang M-C, Chan T-F (2016) Predictors of hyperglycemic women’s perinatal health status. Worldviews Evid-Based Nurs 13:445–453. 10.1111/wvn.12173 [DOI] [PubMed] [Google Scholar]
- 32.Ding G, Niu L, Vinturache A et al (2020) “Doing the month” and postpartum depression among Chinese women: a Shanghai prospective cohort study. Women Birth 33:E151–E158. 10.1016/j.wombi.2019.04.004 [DOI] [PubMed] [Google Scholar]
- 33.Ross LE, Murray BJ, Steiner M (2005) Sleep and perinatal mood disorders: a critical review. J Psychiatry Neurosci 30:247–256 [PMC free article] [PubMed] [Google Scholar]
- 34.Xie R-H, He G, Liu A et al (2007) Fetal gender and postpartum depression in a cohort of Chinese women. Soc Sci Med 65:680–684. 10.1016/j.socscimed.2007.04.003 [DOI] [PubMed] [Google Scholar]
- 35.Qi W, Liu Y, Lv H et al (2022) Effects of family relationship and social support on the mental health of Chinese postpartum women. BMC Pregnancy Childbirth 22:65. 10.1186/s12884-022-04392-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chrzan-Detkos M, Murawska N, Walczak-Kozlowska T (2022) “Next Stop: Mum”: evaluation of a postpartum depression prevention strategy in Poland. Int J Environ Res Public Health 19:11731. 10.3390/ijerph191811731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tsuno K, Okawa S, Matsushima M et al (2022) The effect of social restrictions, loss of social support, and loss of maternal autonomy on postpartum depression in 1 to 12-months postpartum women during the COVID-19 pandemic. J Affect Disord 307:206–214. 10.1016/j.jad.2022.03.056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li K, Lu J, Pang Y et al (2023) Maternal postpartum depression literacy subtypes: a latent profile analysis. Heliyon 9:e20957. 10.1016/j.heliyon.2023.e20957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Branquinho M, Canavarro MC, Fonseca A (2019) Knowledge and attitudes about postpartum depression in the Portuguese general population. Midwifery 77:86–94. 10.1016/j.midw.2019.06.016 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.