Abstract
Photon-counting CT has a completely different detector mechanism than conventional energy-integrating CT. In the photon-counting detector, X-rays are directly converted into electrons and received as electrical signals. Photon-counting CT provides virtual monochromatic images with a high contrast-to-noise ratio for abdominal CT imaging and may improve the ability to visualize small or low-contrast lesions. In addition, photon-counting CT may offer the possibility of reducing radiation dose. This review provides an overview of the actual clinical operation of photon-counting CT and its diagnostic utility in abdominal imaging. We also describe the clinical implications of photon-counting CT including imaging of hepatocellular carcinoma, liver metastases, hepatic steatosis, pancreatic cancer, intraductal mucinous neoplasm of the pancreas, and thrombus.
Graphical Abstract
Keywords: Photon-counting CT, Abdomen, Liver, Pancreas, Metabolic dysfunction-associated steatohepatitis (MASH), Iron overload
Introduction
In abdominal imaging, CT has played a very important role in various diseases and conditions. In the field of oncology, CT has been used for detection, staging and preoperative planning of various tumors [1, 2]. In chronic diseases, CT has also been used to evaluate substances present in the organs, such as fatty deposition in the liver in metabolic dysfunction-associated steatohepatitis or hepatic iron deposition in iron overload condition [3].
Since the introduction of clinical CT in the early 1970s, CT have has advanced rapidly [4, 5]. One of the milestones in the history of CT was the advent of multidetector CT, which allowed for improved spatial resolution and wider image coverage, both of which contributed greatly to tumor imaging, including hepatocellular carcinoma and pancreatic neoplasia in many aspects [6, 7]. In addition, the advent of dual-energy CT made it possible to accurately quantify substances in organs, such as lipids [8]. On the other hand, virtual monochromatic imaging with dual-energy CT has improved image contrast, which has also contributed to improved tumor detection [9].
More recently, photon-counting detector technology has been introduced into clinical CT [10]. Designed to overcome the contrast and spatial resolution limitations of conventional CT and to reduce radiation dose, this technology represents one of the most significant innovations in CT equipment to date. The photon-counting detector can measure the number of photons and the energy of each photon, allowing the acquisition of images with high spatial resolution and virtual monochromatic contrast [11]. Thus, photon-counting CT has tremendous potential, but it has only been clinically available for a short time, and studies of its diagnostic ability and clinical utility for abdominal lesions are limited at this time, and further research and experience are needed before its benefits can be understood.
We offer here a review of the actual clinical operation of photon-counting CT and its diagnostic utility in abdominal imaging.
Technical overview of photon-counting detector
Photon-counting CT has a detector with a completely different mechanism than conventional CT. Conventional CT detectors convert X-rays into light, and then this light is converted into electrical signals using a photodiode, but photon-counting detectors can convert X-rays directly into electrons (charge cloud) and receive them as electrical signals [11].
Photon-counting CT has two major advantages over conventional CT equipped with energy-integrating detectors. One is better dose efficiency, and the other is better spatial resolution.
Photon-counting CT does not require a detector septum, thus increasing the aperture area [11]. There is no electrical noise because subthreshold electrical signals are eliminated in photon-counting CT [12]. In addition, there is no "energy weighting effect" in photon-counting CT, i.e. the scintillation light in an energy-integrating detector becomes stronger and the output increases in proportion to the energy of the X-ray photon, but in photon-counting detector the output is constant regardless of the energy of the X-ray photon [13]. As a result, sensitivity is relatively high in the low energy range, resulting in improved soft tissue contrast in photon-counting CT [14]. These characteristics of the photon-counting detector contribute to improved dose efficiency [15].
Each detector pixel of the photon-counting detector is smaller than that of conventional detectors [12]. In addition, the higher resolution results in increased image noise, but this effect can be reduced by improving dose efficiency. For these reasons, photon-counting CT can improve the spatial resolution of CT images [16].
Radiation dose reduction opportunities
Because photon-counting detectors have no detector septum, no electrical noise, and no “energy weighting effect”, they are inherently more dose efficient. Therefore, photon-counting CT can achieve the same spatial resolution and image noise as conventional CT at a lower radiation dose (Fig. 1, 2). Photon-counting CT provides a significant dose reduction (approximately 32%) in contrast-enhanced abdominal CT while maintaining image quality similar to that of second-generation dual-source CT [17]. Decker et al. reported that image noise was significantly lower, and iodine signal-to-noise ratio was significantly higher, and subjective image quality was higher and conspicuity was better for the renal pelvis, ureters, and mesenteric vessels with low-dose photon-counting CT (mean CTDIvol 1.61 mGy) compared with low-dose second-generation dual-source CT (mean CTDIvol 1.45 mGy) [18].
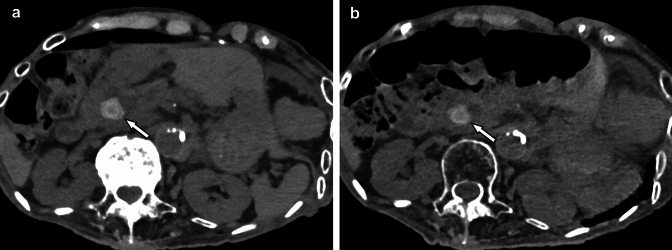
Fig. 1.
Non-contrast abdominal CT images of a patient with choledocholithiasis scanned with photon-counting CT (A) and conventional dual-source CT (single-energy mode) (B) on different days. Image noise was apparently lower with photon-counting CT than with conventional CT, even though the radiation dose was lower with photon-counting CT (CTDIvol: 7.5 mGy) than with conventional CT (11.9 mGy). The layered calcified stone in the common bile duct (arrows) is visualized more precisely with photon-counting CT
Fig. 2.
Contrast-enhanced dynamic CT images during the arterial dominant phase (A, B) and the equilibrium phase (C, D) of the liver scanned with photon-counting CT (A, C) and conventional dual-source CT (single-energy mode) (B, D) on different days. A small hemangioma is seen under the capsule of the right lobe of the liver (arrows). Although the radiation dose of the photon-counting CT (CTDIvol: 4.6 mGy) was coincidently half of that of the conventional CT (9.2 mGy), the image quality remained comparable
Photon-counting CT is also advantageous for imaging patients with large body habitus. When dual-energy imaging is performed on obese patients with conventional detector CT, the overall image quality is reduced due to the lack of photons at low kVp acquisition [19]. Hagen et al. reported that contrast-enhanced abdominal CT using photon-counting CT in obese patients achieved similar or improved image quality and significant dose reduction compared with conventional single-energy CT [20].
Iodine contrast dose reduction opportunities
Improved contrast-to-noise ratio in photon-counting CT may provide an opportunity to reduce the contrast dose required for abdominal imaging. In the phantom study, a 30–37% improvement in the iodine contrast-to-noise ratio was observed, suggesting that there is room for a reduction in the contrast dose used [21]. Hagen et al. reported that photon-counting CT (non-spectral images at 120 kVp) allows a significant 27% contrast dose reduction with a comparable contrast-to-noise ratio, in addition to a radiation dose reduction of up to 34% compared to conventional CT at 120 kVp (single energy mode) in obese patients [22].
Scan modes
The currently available clinical photon-counting CT has three main scan modes, including ultra-high resolution (UHR) mode, multi-energy mode, and dual-source mode. The UHR mode provides the highest spatial resolution images. The UHR mode uses 120 rows with a slice thickness of 0.2 mm, resulting in a total width of 24 mm. Multi-energy mode is the imaging method capable of producing virtual monochromatic images at standard scan speeds. The use of dual-source mode allows for a very fast scan speed. Dual-source mode uses two detectors, each with 144 rows and a slice thickness of 0.4 mm. This results in a total width of 115.2 mm. Each imaging mode should be used according to the purpose of the examination. Of these, the multi-energy mode is frequently used for abdominal scanning because of the many potential applications of spectral imaging with this mode, including the ability to generate different levels of monoenergetic images [22, 23]. Meanwhile, the use of the dual-source mode, which allows for very fast scanning, can be considered for patients who have difficulty holding their breath. High-speed scans can reduce motion artifacts associated with respiratory motion.
Image reconstruction
The photon-counting CT scanner is equipped with a wide variety of reconstruction kernels (Table 1). In general, the body regular (Br) kernel is used for abdominal CT images [24]. The numbers in the kernel indicate the index numbers. The larger the resolution index number, the higher the resolution, but the image noise increases. Therefore, it is necessary to select an appropriate value, while taking into account the degradation of image quality due to increased image noise. However, image noise may also be affected by the Quantum Iterative Reconstruction (QIR) algorithm condition settings described below, so both the kernel and QIR algorithm settings need to be considered together (Fig. 3). For CT angiography, the Body Vascular (Bv) kernel is recommended because it reduces blooming artifacts caused by objects with very high attenuation. Spectral analysis requires images reconstructed using the Quantitative Regular (Qr) kernel. For the evaluation of hepatocellular carcinoma in photon-counting CT, softer reconstruction kernels are superior in terms of noise and image quality, but no significant differences in image contrast and lesion conspicuity are found between the different reconstruction kernels [25].
Table 1.
The list of image reconstruction kernels at photon-counting CT
| Kernel Family & Kernel Group | ||||||||
|---|---|---|---|---|---|---|---|---|
| Body (B) | Head (H) | Quantitative (Q) | ||||||
| l (lung) | r (regular) | v (vascular) | c (crisp) | r (regular) | v (vascular) | r (regular) | ||
| Resolution | 36 | Br36 | Bv36 | Hr36 | Hv36 | Qr36 | ||
| Index | 40 | Br40 | Bv40 | Hc40 | Hr40 | Hv40 | Qr40 | |
| 44 | Br44 | Bv44 | Hc44 | Hr44 | Hv44 | Qr44 | ||
| 48 | Br48 | Bv48 | Hr48 | Hv48 | Qr48 | |||
| 56 | Bl56 | Br56 | Bv56 | Hr56 | Hv56 | Qr56 | ||
| 60 | Bl60 | Br60 | Bv60 | Hr60 | Hv60 | Qr60 | ||
| 64 | Bl64 | Br64 | Bv64 | Hr64 | Hv64 | Qr64 | ||
| 68 | Br68 | Bv68 | Hr68 | Hv68 | Qr68 | |||
| 72 | Br72 | Bv72 | Hr72 | Hv72 | Qr72 | |||
| 76 | Br76 | Bv76 | Hr76 | Hv76 | Qr76 | |||
| 80 | Br80 | Bv80 | Hr80 | Hv80 | Qr80 | |||
| 84 | Br84 | Bv84 | Hr84 | Hv84 | Qr84 | |||
| 89 | Br89 | Bv89 | Hr89 | Hv89 | Qr89 | |||
| 92 | Br92 | Hr92 | ||||||
| 96 | Br96 | Hr96 | ||||||
| 98 | Br98 | Hr98 | ||||||
Note: Kernels with a resolution index of 80 or higher can only be used in UHR mode
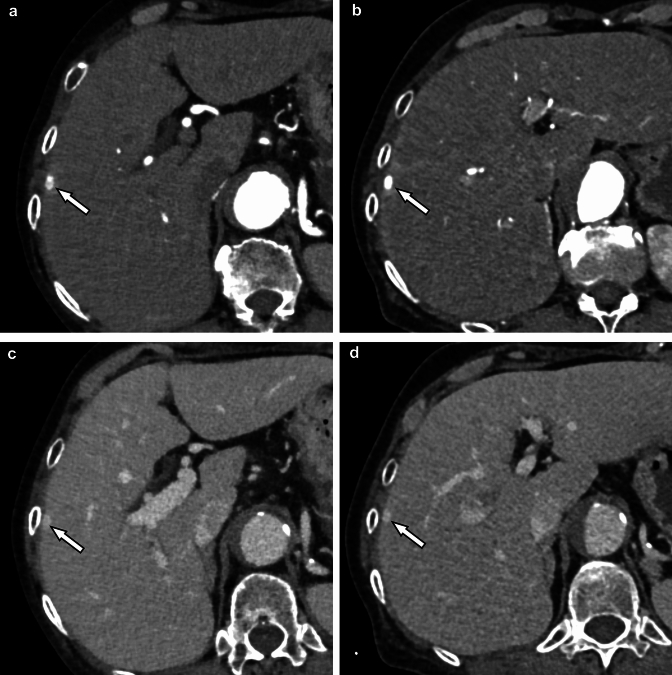
Fig. 3.
Photon-counting CT images with different reconstruction settings are shown aligned. The higher the resolution index (Br36, Br40, Br44), the higher the resolution, but the higher the image noise. The higher the level of the Quantum Iterative Reconstruction (QIR) algorithm, the lower the image noise
Although photon-counting CT has excellent dose efficiency, a denoising algorithm may be essential for abdominal CT imaging. A high-intensity iterative reconstruction algorithm improves image quality by reducing image noise in abdominal photon-counting CT [23]. There are four levels of QIR strength, where level 1 is the weakest and level 4 is the strongest [23]. A high strength level corresponds to level 3 or 4. Especially in images with thin slice thickness, image noise is significant, so the iterative reconstruction algorithm at the highest strength level is very effective in reducing image noise. The currently available clinical photon-counting CT scanner is equipped with an iterative reconstruction algorithm (QIR), but deep learning image reconstruction techniques are not yet installed.
Virtual monochromatic imaging
One of the major advantages of photon-counting CT in abdominal examinations is that it provides virtual monochromatic images with high image quality. The photon-counting detector is able to determine the energy intensity of the photons, making it possible to generate virtual monochromatic images from single-energy acquisition data at, for example, 120 kVp (Fig. 4). The minimum and maximum energy level settings for virtual monochromatic images in this CT system are 40 and 190 keV, respectively [24, 26]. The low-keV virtual monochromatic images with the photon-counting CT can provide superior performance over conventional single-energy (non-spectral) CT in arterial phase imaging, including significantly higher contrast-to-noise ratio, better image quality, and lesion conspicuity [27]. The low-keV virtual monochromatic images with the photon-counting CT have a significantly higher contrast-to-noise ratio with similar subjective image quality as compared to conventional single-energy dual-source CT at identical radiation dose [24].
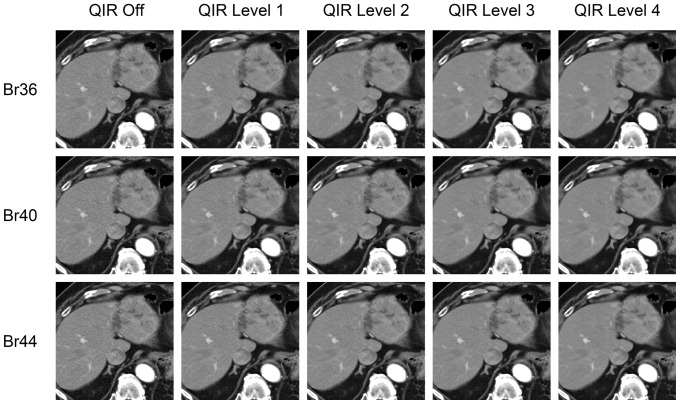
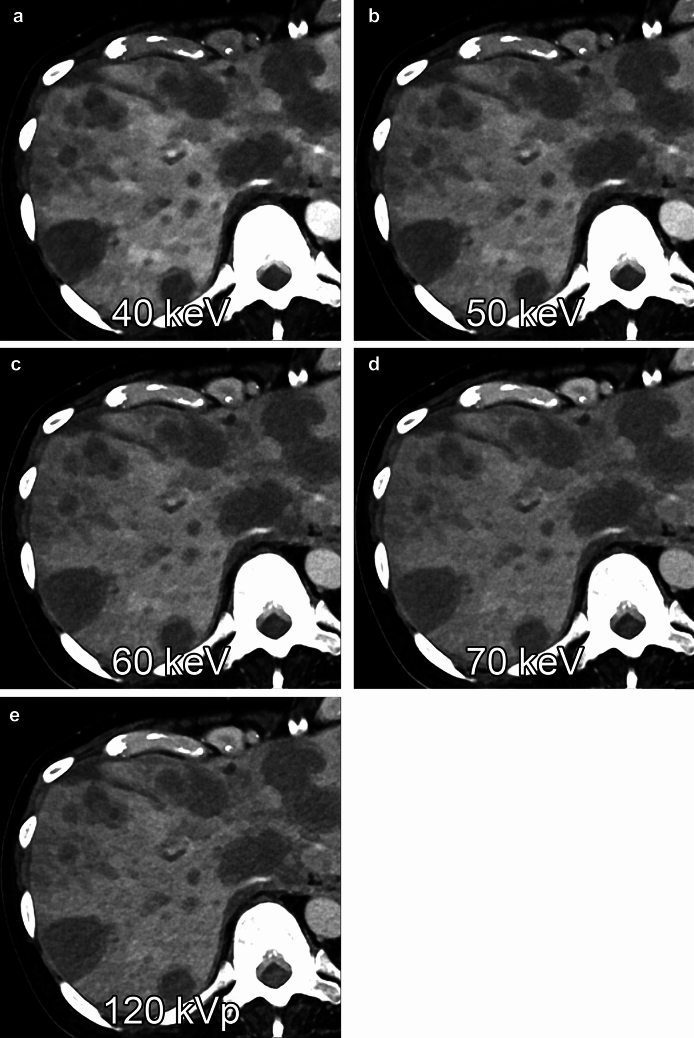
Fig. 4.
Using a photon counting detector, virtual monochromatic images of any energy level from 40 to 190 keV can be generated from 120kVp single-energy raw data. The lower the keV setting of the virtual monochromatic image, the higher the contrast between the liver lesion and the liver parenchyma
The mainstream of conventional dual-energy CT is to scan with two different energy X-ray beams, for example 80 kVp and 140 kVp, and analyze the data to generate virtual monochromatic images [28]. Therefore, prior to scanning, a decision had to be made whether to perform dual-energy imaging or normal single-energy imaging. The design of the photon-counting detector allows virtual monochromatic images to be reconstructed from single-energy data acquired at 120 kVp or 140 kVp. There is no need to decide on the type of acquisition before scanning, considering whether the virtual monochromatic imaging is needed or not [19]. For the virtual monochromatic images at energies below 60 keV, the contrast-to-noise ratio of the photon-counting CT images was generally higher than that of the corresponding energy-integrating detectors dual-energy CT images [29].
High spatial resolution
Photon-counting CT can improve spatial resolution due to the nature of its detector structure. When scanning in UHR mode, images with a thickness of 0.2 mm can be obtained. The image matrix size can also be output at 1024 × 1024, and when the field-of-view is reduced to 20 cm, it is also possible to generate 0.2 mm isotropic voxel image data. For high-contrast structures such as the lungs and temporal bones, the extremely high spatial resolution allows fine structures to be visualized in detail. In abdominal CT, the high spatial resolution characteristic of photon-counting CT can be exploited in CT angiography generated from early arterial phase images. Additional applications, such as the detection and staging of pancreatic cancer and cystic pancreatic lesions (i.e., intraductal papillary mucinous neoplasms), could potentially benefit from this new capability [19]. Photon-counting CT also has the potential to improve the detection and determination of the composition of small urolithiasis [30]. This diagnosis might be important for patients with renal stones, as detection of these small stones could allow for early clinical intervention [30].
Scanning protocols optimized for the abdominal diseases
Virtual monochromatic images are available with acquisition at 120 kVp or 140 kVp of X-ray tube voltage. Because acquisition at 140 kVp provides the best possible spectral separation at the detector level [31], Schwartz et al. acquire all adult abdominal CT images at 140 kVp [19]. When performing abdominal photon-counting CT, many radiologists are concerned with determining which keV setting of virtual monochromatic image reconstruction is optimal for diagnosis. The 40 keV images have the best contrast-to-noise ratio for abdominal organs, vascular structures, and hypovascular liver metastases [24, 26]. However, CT image quality may be affected by factors other than the contrast-to-noise ratio. Racine et al. reported that the highest detectability was found at 65 and 70 keV for both hypoattenuating and hyperattenuating objects, regardless of phantom size and radiation dose, in the phantom study, which was performed assuming the detection of hepatocellular carcinoma [32]. Higashigaito et al. reported that the overall image quality of abdominal CT tended to be higher at 50 keV and 60 keV compared with energy-integrating detector CT, whereas the overall image quality was lower at 40 keV compared with energy-integrating detector CT in the clinical study [24]. Further studies may be needed to determine the optimal keV setting for diagnostic abdominal CT using photon-counting CT in clinical practice.
Abdominopelvic CT is usually performed in a single breath hold. Acquisition of abdominopelvic CT with the thinnest collimation (0.2 mm × 120 rows, UHR mode) is more difficult due to longer scan times, so it is generally performed with routine collimation (0.4 mm × 144 rows) [33]. However, when acquired with this setting, the minimum slice thickness of the images is 0.4 mm.
An example of the acquisition and reconstruction parameters for a scan of the abdomen using photon counting CT is shown in Table 2.
Table 2.
Example of acquisition and reconstruction parameters for abdominal scan using photon-counting CT
| Parameters | |
|---|---|
| Voltage (kVp) | 120 or 140 |
| Collimation (mm) | 144 × 0.4 or 120 × 0.2 |
| Pitch | 0.8 |
| Rotation time (s) | 0.5 |
| Kernel | Br40 or Br44* |
| QIR level | 2 or 3 |
| Energy level (keV) | 70 (and 50) |
| Matrix | 512 × 512 |
Note: * For spectral post processing, the images reconstructed with the kernels Qr (quantum regular) are needed
Clinical implications for the diagnosis of abdominal diseases
Virtual monochromatic imaging technique on a photon-counting CT scanner achieves higher image contrast and lower image noise, allowing precise delineation of lesions and has the potential to improve detection of liver and pancreatic tumors and peritoneal lesions. As mentioned above, virtual monochromatic images with photon-counting CT are expected to improve CNR compared to virtual monochromatic images with conventional CT [29]. In the phantom study, photon-counting CT significantly improved the detection of focal liver lesions smaller than 1 cm, especially at low radiation dose, compared to conventional dual-energy CT [32]. The high spatial resolution and high contrast images with photon-counting CT are also effective for CT angiography to delineate small visceral arteries.
Virtual noncontrast imaging based on the spectral data from a photon-counting detector is also a valuable technique in the abdominal CT. Virtual noncontrast images with photon-counting CT have similar CT attenuation accuracy to true noncontrast images [34]. Importantly, the photon-counting CT significantly outperformed conventional dual-energy CT in terms of quantification accuracy, even after adjusting for confounding variables such as radiation dose and patient size [34]. In addition, Mergen et al. demonstrated that the CT attenuation difference was within 10 H.U. in 95% of the measurements [35].
Liver imaging
Hepatocellular carcinoma
Hepatocellular carcinoma is the most common primary liver cancer [36] and one of the most malignant cancers with high morbidity and mortality [37]. In the diagnostic imaging of hepatocellular carcinoma, detailed evaluation of contrast enhancement on dynamic contrast-enhanced CT, such as early enhancement during the arterial phase and washout pattern during the equilibrium phase, provides very important clues [38]. The high contrast-to-noise ratio of the photon-counting CT makes it possible to clearly visualize subtle differences in contrast, which might contribute to improved diagnostic performance when evaluated in the future (Fig. 5).
Fig. 5.
Contrast-enhanced photon-counting CT images during arterial dominant phase (A, B) and equilibrium phase (C, D) at 70 (A, C) and 50 keV (B, D). Arterial enhancement and washout pattern of HCC are better visualized on 50 keV images (B, D) than on 70 keV images (A, C) in the arterial and equilibrium phases, respectively (arrows). The hypovascular nodule (arrowheads: suspected dysplastic nodule) is also more clearly delineated on the 50 keV image (B) than on the 70 keV image (D)
Liver metastases
Liver metastasis is the most common type of liver cancer, and most cases have hypovascular characteristics. Virtual monochromatic images with photon-counting CT show reduced image noise compared to conventional single-energy CT and improved conspicuity of hypovascular liver metastases at lower keV levels, and patients with a high body mass index benefit especially from photon-counting CT compared to conventional CT [26] (Fig. 6).
Fig. 6.
Multiple metastatic liver tumors from pancreatic cancer were shown on virtual monochromatic images at 40 (A), 50 (B), 60 (C), and 70 keV (D) and polychromatic image (i.e., T3D) acquired with photon-counting CT at 120 kVp (E) during the portal venous dominant phase. The contrast-to-noise ratios between the liver metastasis and the liver parenchyma are 14.6, 11.9, 9.8, 8.5, and 7.4, respectively
Hepatic steatosis
Hepatic steatosis, including metabolic dysfunction-associated fatty liver disease and metabolic dysfunction-associated steatohepatitis, is a serious pathological condition of the liver that can progress to cirrhosis and hepatocellular carcinoma [39]. Estimation of intrahepatic fat is essential for the diagnosis of hepatic steatosis [40]. Photon-counting CT has been shown to be accurate for index-based liver fat estimation from virtual non-contrast images [41] and has the potential to increase the likelihood of incidental detection of liver steatosis on contrast-enhanced abdominal CT scans (Fig. 7). In addition, photon-counting CT can quantify intrahepatic fat even in the presence of iron overload [42].
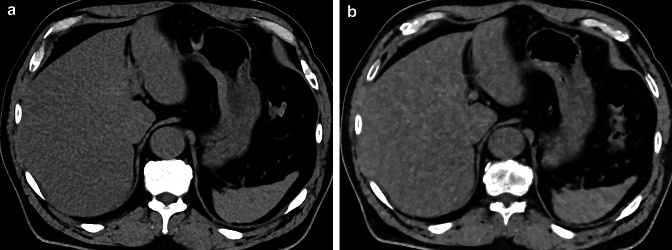
Fig. 7.
A true noncontrast CT image (A) and a virtual noncontrast CT image obtained from contrast-enhanced image data (B) acquired with photon-counting CT. Virtual noncontrast images with photon-counting CT have similar CT attenuation accuracy to true noncontrast images. In both images, the liver parenchyma is less attenuated than the spleen, indicating hepatic steatosis
Pancreas imaging
Pancreatic cancer
Pancreatic cancer has a significantly poor prognosis among various cancers, and early detection is critical for patient survival [43]. Pancreatic cancer usually presents as a hypovascular mass, but in the early stages it is often difficult to detect with diagnostic imaging, CT or MRI, due to its small size and poor contrast [44]. Virtual monochromatic images with 70 keV or less in photon-counting CT significantly improves conspicuity of pancreatic cancer in both, pancreatic and portal venous phase, compared to energy-integrating detector CT [45] (Fig. 8). In addition, pancreatic cancer is a highly invasive tumor [46], and it is important to determine the extent of its invasion on the images before treatment. The high spatial resolution of photon-counting CT may also be useful in evaluating tumor invasion [47].
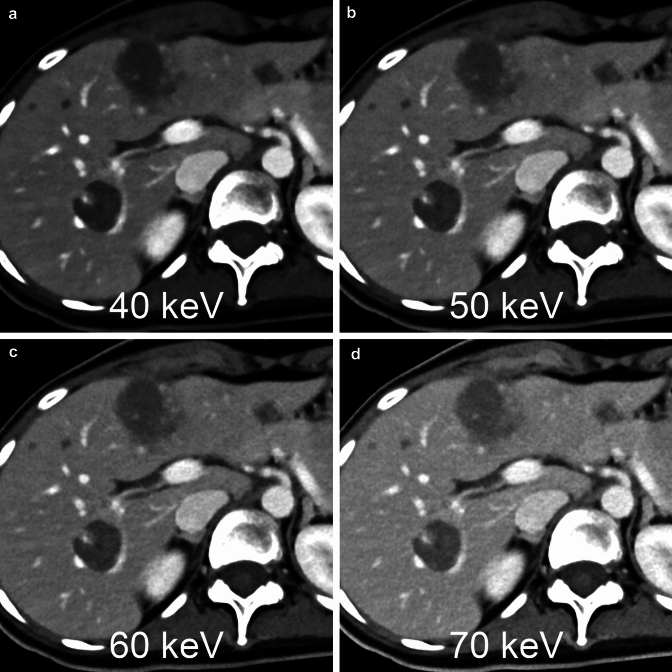
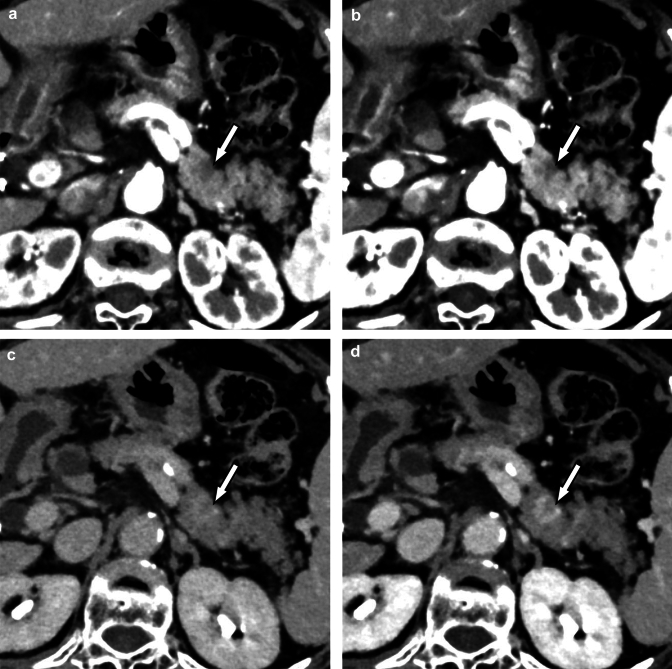
Fig. 8.
Pancreatic cancer is shown as a small hypovascular nodule in the tail of the pancreas (arrows) on the pancreatic parenchymal phase (arterial phase) photon-counting CT images at 70 (A) and 50 keV (B). Meanwhile, enhancement of the tumor (arrows) is shown during the equilibrium phase at 70 (C) and 50 keV (D). The delayed enhancement is more evident in the 50 keV image (D) than in the 70 keV image (C). Small pancreatic cancers are often not visualized in the pancreatic parenchymal phase but are visualized as delayed-enhancement lesions only in the equilibrium phase. Low-keV images obtained with photon-counting CT may help in the early detection of pancreatic cancer
Intraductal papillary mucinous neoplasm
Intraductal papillary mucinous neoplasm is the most common cystic neoplasm of the pancreas [48]. The increased attention to intraductal papillary mucinous neoplasm is due to its unique features of malignant progression [49]. Photon-counting CT can detect more pancreatic cysts than conventional energy-integrating detector CT [50]. The Fukuoka consensus proposes two-tiered criteria for predicting malignancy in intraductal papillary mucinous neoplasm, "high-risk stigmata" and "worrisome features" [51]. For patients with "high-risk stigmata" consisting of obstructive jaundice, enhancing mural nodules, and main duct dilatation ≥ 10 mm, immediate surgical resection is recommended [51]. Therefore, accurate evaluation of these findings on imaging is necessary. Imaging with photon-counting CT may be particularly helpful in the accurate evaluation of small structures such as enhancing mural nodules (Fig. 9).
Fig. 9.
A cystic lesion with a mural nodule (arrows) is seen in the tail of the pancreas on the pancreatic parenchymal phase (arterial phase) photon-counting CT images at 70 (A) and 50 keV (B). The cystic lesion is consistent with an intraductal papillary mucinous neoplasm. The 50 keV image (B) shows the enhancement of the mural nodule more clearly than the 70 keV image (A). Such a nodule is a sign of malignancy (i.e., high-risk stigmata)
Vascular imaging
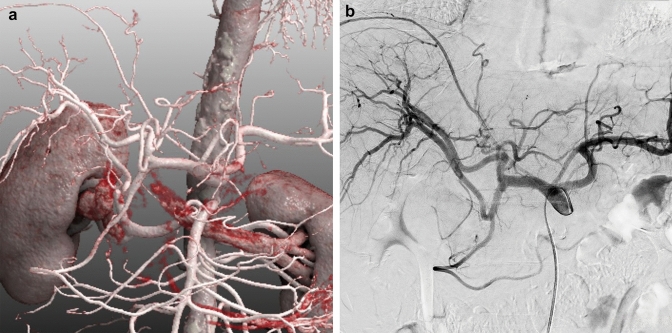
Vascular anatomy evaluation
When performing laparoscopic surgery, the surgeon must have extensive preoperative information about the vascular anatomy to plan the procedure [52]. Visualization of vascular variants on preoperative imaging such as CT angiography can help identify these vessels and prevent fatal vascular injury [53]. Assessment of vascular anatomy by CT angiography is also useful in the preprocedural evaluation of arterial embolization procedures. Photon-counting CT shows considerable improvements in several aspects of vascular imaging [54] (Fig. 10). Dillinger et al. reported that virtual monochromatic images at 60–70 keV provide the best objective and subjective image quality in terms of vessel contrast [55].
Fig. 10.
Photon-counting CT is also excellent for CT angiography (A) because of its superior spatial resolution. In this case, hepatocellular carcinoma was treated by transarterial chemoembolization, and celiac angiography was also performed during the procedure (B). CT angiography adequately delineated the hepatic artery to the periphery, which may facilitate selective catheter insertion into the hepatic artery branches
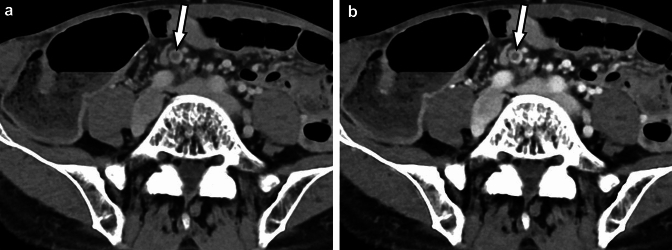
Thrombosis
Contrast-enhanced CT is also useful in the diagnosis of thrombosis. With photon-counting CT, even small thrombi can be clearly visualized, contributing to an accurate diagnosis [56] (Fig. 11).
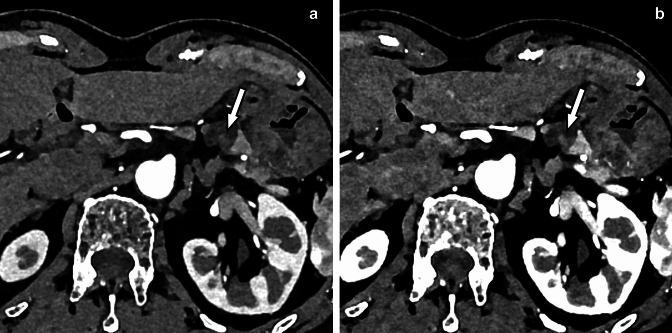
Fig. 11.
A small thrombus in the mesenteric vein (arrows) is visualized on the photon-counting CT images at 70 (A) and 50 keV (B). The 50 keV image (B) shows the thrombus with higher contrast than the 70 keV image (A). Photon-counting CT is excellent for visualization of venous thrombus
Challenges
Investigation on the diagnosis of abdominal disease using photon-counting CT is still in its early stages and several challenges have been identified.
One of these may be the determination of optimal imaging parameters for the diagnosis of abdominal lesions. Since the type of image to be obtained depends on the purpose of the examination, it may be necessary to consider optimal settings for different clinical situations. The situations may be divided into pre-treatment examination, routine examination, and examination of patients with renal failure. Each of these situations requires improved diagnostic performance, lower radiation doses, and lower contrast doses, respectively. The large variety of parameters (e.g., radiation dose, reconstruction kernel, level of iterative reconstruction, energy level of VMI) also complicates the problem. These factors need to be properly organized to define reasonable imaging conditions.
Another issue may be the lack of evidence to show whether photon-counting CT significantly improves the ability to detect and diagnose disease, especially when compared to conventional CT systems. In such cases, due attention should be paid to whether the conventional CT being compared is spectral images similar to that of photon-counting CT or non-spectral images.
Further investigations will be needed to resolve these issues.
Conclusion
Photon-counting CT provides a high contrast-to-noise ratio for abdominal CT imaging and may improve the ability to visualize small or low-contrast lesions. In addition, photon-counting CT may offer the opportunity of reducing radiation exposure dose.
Acknowledgements
We acknowledge the invaluable work of our CT technologist team at our institution. This work was supported by JSPS KAKENHI Grant Number 23K07179.
Funding
Open Access funding provided by Osaka University.
Declarations
Conflict of interest
The authors declare no conflicts of interest associated with this manuscript.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zeman RK, Fox SH, Silverman PM, et al. Helical (spiral) CT of the abdomen. AJR Am J Roentgenol. 1993 Apr;160(4):719-25. [DOI] [PubMed] [Google Scholar]
- 2.Agrawal MD, Pinho DF, Kulkarni NM, Hahn PF, Guimaraes AR, Sahani DV. Oncologic applications of dual-energy CT in the abdomen. Radiographics. 2014 May-Jun;34(3):589–612. [DOI] [PubMed]
- 3.Elbanna KY, Mansoori B, Mileto A, Rogalla P, S Guimarães L. Dual-energy CT in diffuse liver disease: is there a role? Abdom Radiol (NY). 2020 Nov;45(11):3413–3424. [DOI] [PubMed]
- 4.Wildberger JE, Prokop M. Hounsfield’s Legacy. Investig Radiol 2020; 55:556–558. [DOI] [PubMed] [Google Scholar]
- 5.Hsieh J, Flohr T. Computed tomography recent history and future perspectives. J Med Imaging 2021; 8:052109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murakami T, Kim T, Hori M, Federle MP. Double arterial phase multi-detector row helical CT for detection of hypervascular hepatocellular carcinoma. Radiology. 2003 Dec;229(3):931-2. [DOI] [PubMed] [Google Scholar]
- 7.Nino-Murcia M, Tamm EP, Charnsangavej C, Jeffrey RB Jr. Multidetector-row helical CT and advanced postprocessing techniques for the evaluation of pancreatic neoplasms. Abdom Imaging. 2003 May-Jun;28(3):366–77. [DOI] [PubMed]
- 8.Hyodo T, Yada N, Hori M, et al. Multimaterial Decomposition Algorithm for the Quantification of Liver Fat Content by Using Fast-Kilovolt-Peak Switching Dual-Energy CT: Clinical Evaluation. Radiology. 2017 Apr;283(1):108-118. [DOI] [PubMed] [Google Scholar]
- 9.Okada M, Kim T, Murakami T. Hepatocellular nodules in liver cirrhosis: state of the art CT evaluation (perfusion CT/volume helical shuttle scan/dual-energy CT, etc.). Abdom Imaging. 2011 Jun;36(3):273–81. [DOI] [PubMed]
- 10.Douek PC, Boccalini S, Oei EHG, et al. Clinical Applications of Photon-counting CT: A Review of Pioneer Studies and a Glimpse into the Future. Radiology 2023; 309(1):e222432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Willemink MJ, Persson M, Pourmorteza A, et al. Photon-counting CT: technical principles and clinical prospects. Radiology. 2018;289:293–312. [DOI] [PubMed] [Google Scholar]
- 12.DanielssonM, Persson M, Sjölin M. Photon-counting x-ray detectors for CT. Phys Med Biol. 2021;66:03tr1. [DOI] [PubMed]
- 13.Flohr T, Petersilka M, Henning A, Ulzheimer S, Ferda J, Schmidt B. Photon-Counting CT review. Phys Med 2020; 79: S1120–1797(20)30273–8:126–36: [DOI] [PubMed]
- 14.Pourmorteza A, Symons R, Reich DS, et al. Photon-Counting CT of the Brain: In Vivo Human Results and Image-Quality Assessment. AJNR Am J Neuroradiol. 2017 Dec;38(12):2257–2263. [DOI] [PMC free article] [PubMed]
- 15.Symons R, Reich DS, Bagheri M, et al. Photon-Counting Computed Tomography for Vascular Imaging of the Head and Neck: First In Vivo Human Results. Invest Radiol. 2018 Mar;53(3):135-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCollough, C.H., Rajendran, K., Leng, S. et al. The technical development of photon-counting detector CT. Eur Radiol 33, 5321–5330 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wrazidlo R, Walder L, Estler A, et al. Radiation Dose Reduction in Contrast-Enhanced Abdominal CT: Comparison of Photon-Counting Detector CT with 2nd Generation Dual-Source Dual-Energy CT in an oncologic cohort. Acad Radiol. 2023 May;30(5):855-862. [DOI] [PubMed] [Google Scholar]
- 18.Decker JA, Bette S, Lubina N, et al. Low-dose CT of the abdomen: Initial experience on a novel photon-counting detector CT and comparison with energy-integrating detector CT. Eur J Radiol. 2022 Mar;148:110181. [DOI] [PubMed] [Google Scholar]
- 19.Schwartz FR, Samei E, Marin D. Exploiting the Potential of Photon-Counting CT in Abdominal Imaging. Invest Radiol. 2023 Jul 1;58(7):488-498. [DOI] [PubMed] [Google Scholar]
- 20.Hagen F, Hofmann J, Wrazidlo R, et al. Image quality and dose exposure of contrast-enhanced abdominal CT on a 1st generation clinical dual-source photon-counting detector CT in obese patients vs. a 2nd generation dual-source dual energy integrating detector CT. Eur J Radiol. 2022 Jun;151:110325. [DOI] [PubMed]
- 21.Sawall S, Klein L, Amato C, et al. Iodine contrast-to-noise ratio improvement at unit dose and contrast media volume reduction in whole-body photon-counting CT. Eur J Radiol. 2020 May;126:108909. [DOI] [PubMed] [Google Scholar]
- 22.Hagen F, Estler A, Hofmann J, et al. Reduced versus standard dose contrast volume for contrast-enhanced abdominal CT in overweight and obese patients using photon counting detector technology vs. second-generation dual-source energy integrating detector CT. Eur J Radiol. 2023 Dec;169:111153. [DOI] [PubMed]
- 23.Sartoretti T, Landsmann A, Nakhostin D, et al. Quantum Iterative Reconstruction for Abdominal Photon-counting Detector CT Improves Image Quality. Radiology. 2022 May;303(2):339-348. [DOI] [PubMed] [Google Scholar]
- 24.Higashigaito K, Euler A, Eberhard M, Flohr TG, Schmidt B, Alkadhi H. Contrast-Enhanced Abdominal CT with Clinical Photon-Counting Detector CT: Assessment of Image Quality and Comparison with Energy-Integrating Detector CT. Acad Radiol. 2022 May;29(5):689-697. [DOI] [PubMed] [Google Scholar]
- 25.Graafen D, Müller L, Halfmann MC, et al. Soft Reconstruction Kernels Improve HCC Imaging on a Photon-Counting Detector CT. Acad Radiol. 2023 Sep;30 Suppl 1:S143-S154. [DOI] [PubMed] [Google Scholar]
- 26.Bette S, Decker JA, Braun FM, et al. Optimal Conspicuity of Liver Metastases in Virtual Monochromatic Imaging Reconstructions on a Novel Photon-Counting Detector CT-Effect of keV Settings and BMI. Diagnostics (Basel). 2022;12(5):1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Graafen D, Müller L, Halfmann M, Düber C, Hahn F, Yang Y, Emrich T, Kloeckner R. Photon-counting detector CT improves quality of arterial phase abdominal scans: A head-to-head comparison with energy-integrating CT. Eur J Radiol. 2022;156:110514. [DOI] [PubMed] [Google Scholar]
- 28.McCollough CH, Leng S,Yu L, et al. Dual- andmulti-energy CT: principles, technical approaches, and clinical applications. Radiology. 2015;276:637–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Booij R, van der Werf NR, Dijkshoorn ML, van der Lugt A, van Straten M. Assessment of Iodine Contrast-To-Noise Ratio in Virtual Monoenergetic Images Reconstructed from Dual-Source Energy-Integrating CT and Photon-Counting CT Data. Diagnostics (Basel). 2022;12(6):1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marcus RP, Fletcher JG, Ferrero A, et al. Detection and Characterization of Renal Stones by Using Photon-Counting-based CT. Radiology. 2018;289(2):436-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sawall S, Klein L, Wehrse E, Rotkopf LT, Amato C, Maier J, Schlemmer HP, Ziener CH, Heinze S, Kachelrieß M. Threshold-dependent iodine imaging and spectral separation in a whole-body photon-counting CT system. Eur Radiol. 2021 Sep;31(9):6631-6639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Racine D, Mergen V, Viry A, Frauenfelder T, Alkadhi H, Vitzthum V, Euler A. Photon-Counting Detector CT for Liver Lesion Detection-Optimal Virtual Monoenergetic Energy for Different Simulated Patient Sizes and Radiation Doses. Invest Radiol. 2024 Jan 9. [DOI] [PubMed]
- 33.McCollough CH, Rajendran K, Baffour FI, et al. Clinical applications of photon counting detector CT. Eur Radiol. 2023 Aug;33(8):5309-5320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sartoretti T, Mergen V, Higashigaito K, Eberhard M, Alkadhi H, Euler A. Virtual Noncontrast Imaging of the Liver Using Photon-Counting Detector Computed Tomography: A Systematic Phantom and Patient Study. Invest Radiol. 2022 Jul 1;57(7):488-493. [DOI] [PubMed] [Google Scholar]
- 35.Mergen V, Racine D, Jungblut L, et al. Virtual Noncontrast Abdominal Imaging with Photon-counting Detector CT. Radiology. 2022 Oct;305(1):107-115. [DOI] [PubMed] [Google Scholar]
- 36.Burkhart RA, Pawlik TM. Staging and Prognostic Models for Hepatocellular Carcinoma and Intrahepatic Cholangiocarcinoma. Cancer Control. 2017 Jul-Sep;24(3):1073274817729235. [DOI] [PMC free article] [PubMed]
- 37.Brown ZJ, Tsilimigras DI, Ruff SM, et al. Management of Hepatocellular Carcinoma: A Review. JAMA Surg. 2023 Apr 1;158(4):410-420. [DOI] [PubMed] [Google Scholar]
- 38.Onishi H, Kim T, Imai Y, et al. Hypervascular hepatocellular carcinomas: detection with gadoxetate disodium-enhanced MR imaging and multiphasic multidetector CT. Eur Radiol. 2012 Apr;22(4):845-54. [DOI] [PubMed] [Google Scholar]
- 39.Kuchay MS, Choudhary NS, Mishra SK. Pathophysiological mechanisms underlying MAFLD. Diabetes Metab Syndr. 2020 Nov-Dec;14(6):1875–1887. [DOI] [PubMed]
- 40.Hyodo T, Hori M, Lamb P, et al. Multimaterial Decomposition Algorithm for the Quantification of Liver Fat Content by Using Fast-Kilovolt-Peak Switching Dual-Energy CT: Experimental Validation. Radiology. 2017;282(2):381-389. [DOI] [PubMed] [Google Scholar]
- 41.Niehoff JH, Woeltjen MM, Saeed S, et al. Assessment of hepatic steatosis based on virtual non-contrast computed tomography: Initial experiences with a photon counting scanner approved for clinical use. Eur J Radiol. 2022 Apr;149:110185. [DOI] [PubMed] [Google Scholar]
- 42.Hollý S, Chmelík M, Suchá S, et al. Photon-counting CT using multi-material decomposition algorithm enables fat quantification in the presence of iron deposits. Phys Med. 2024 Feb;118:103210. [DOI] [PubMed] [Google Scholar]
- 43.Cai J, Chen H, Lu M, et al. Advances in the epidemiology of pancreatic cancer: Trends, risk factors, screening, and prognosis. Cancer Lett. 2021 Nov 1;520:1-11. [DOI] [PubMed] [Google Scholar]
- 44.Gandhi NS, Feldman MK, Le O, et al. Imaging mimics of pancreatic ductal adenocarcinoma. Abdom Radiol (NY). 2018;43:273–284. [DOI] [PubMed] [Google Scholar]
- 45.Decker JA, Becker J, Härting M, et al. Optimal conspicuity of pancreatic ductal adenocarcinoma in virtual monochromatic imaging reconstructions on a photon-counting detector CT: comparison to conventional MDCT. Abdom Radiol (NY). 2024 Jan;49(1):103-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vincent A, Herman J, Schulick R, et al. Pancreatic cancer. Lancet. 2011 Aug 13;378(9791):607-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim J, Mabud T, Huang C, et al. Inter-reader agreement of pancreatic adenocarcinoma resectability assessment with photon counting versus energy integrating detector CT. Abdom Radiol (NY). 2024 Apr 17. [DOI] [PubMed]
- 48.Werner J, Fritz S, Buchler MW. Intraductal papillary mucinous neoplasms of the pancreas: a surgical disease. Nat Rev Gastroenterol Hepatol. 2012; 9:253–259. [DOI] [PubMed] [Google Scholar]
- 49.Tanaka M. Clinical Management and Surgical Decision-Making of IPMN of the Pancreas. Methods Mol Biol. 2019;1882:9-22. [DOI] [PubMed] [Google Scholar]
- 50.Dane B, Kim J, Qian K, Megibow A. Pancreatic cyst prevalence and detection with photon counting CT compared with conventional energy integrating detector CT. Eur J Radiol. 2024 Mar 20;175:111437. [DOI] [PubMed] [Google Scholar]
- 51.Tanaka M, Fernandez del Castillo C, Adsay V et al (2012) International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology 12:183–197 [DOI] [PubMed] [Google Scholar]
- 52.Raman SS, Pojchamarnwiputh S, Muangsomboon K, et al. Utility of 16-MDCT angiography for comprehensive preoperative vascular evaluation of laparoscopic renal donors. AJR Am J Roentgenol 2006;186:1630–1638. [DOI] [PubMed] [Google Scholar]
- 53.Kumar S, Neyaz Z, Gupta A. The utility of 64 channel multidetector CT angiography for evaluating the renal vascular anatomy and possible variations: a pictorial essay. Korean J Radiol. 2010 May-Jun;11(3):346–54. [DOI] [PMC free article] [PubMed]
- 54.Wildberger JE, Alkadhi H. New Horizons in Vascular Imaging with Photon-Counting Detector CT. Invest Radiol. 2023 Jul 1;58(7):499-504. [DOI] [PubMed] [Google Scholar]
- 55.Dillinger D, Overhoff D, Booz C, et al. Diagnostics (Basel). 2023 Mar 1;13(5):938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kisohara M, Kitera N, Itoh T, et al. Radiol Case Rep. 2024 Jan 16;19(4):1404-1408. [DOI] [PMC free article] [PubMed] [Google Scholar]