Abstract
Background
Turnaround time is an integral component of primary healthcare and is a key performance indicator of healthcare delivery. It is defined as the time patients spend during a healthcare facility visit. In this study, turnaround time is defined as the time elapsed from registration to the end of consultation.
Objectives
This study aimed to determine the turnaround time of consults in the primary care system in a rural site in the Philippines, and compare turnaround time during the pre-pandemic and COVID-19 pandemic periods.
Methods
This is a retrospective cohort study of patients seen at the primary care facility under the Philippine Primary Care Studies (PPCS) rural site from April 2019 to March 2021. Patients included in this study were chosen through random sampling. Electronic medical records (EMR) of these patients were reviewed. Turnaround time was computed electronically from time of registration to end of consultation. Descriptive statistics was used to summarize data and report turnaround time. The turnaround time before and during the pandemic was compared using an independent sample t-test (if normally distributed) or Mann Whitney U test (if not normally distributed). A p-value of <0.05 was considered statistically significant.
Results
A random sample of 342 patients out of the total 45,501 patient consults seen at the rural primary healthcare facility from April 2019 to March 2021 were included in this study. The median turnaround time was 29.0 minutes (interquartile range [IQR] 68.3), with range of 0.9 to 437.2 minutes. During the pre-pandemic period, the median turnaround time of consults is 29.3 minutes (IQR 70.4) which is 1.8 minutes longer than the pandemic period which showed median turnaround time of 27.5 minutes (IQR 72.7). The difference between the two time periods was not statistically significant (P = 0.39).
Conclusion
The study showed that the median turnaround time of medical consults was 29.0 minutes, which was shorter by 80 minutes compared to other published Philippine studies. The turnaround time did not differ significantly in the pandemic and pre-pandemic period, despite new policies and systems that were implemented during the pandemic.
Keywords: turnaround time, primary care, electronic medical records, pandemic, Philippines
INTRODUCTION
A strong primary healthcare system improves the capacity of a country to provide high quality and cost-effective health services. An ineffective primary care system forces individuals to rely on the resources of potentially understaffed emergency departments.1 In the past years, the Philippines had faced several challenges in primary care, including inequity in health access, shortage of primary care providers, and inadequate skill mix.2
The Philippine Primary Care Studies (PPCS) was launched in 2016 as a pilot health system research in line with the country’s goal towards universal healthcare. This research aimed to strengthen primary care facilities by engaging dedicated primary care providers supported by a centralized electronic database. A rural, urban, and remote site were chosen for the PPCS pilot study. An important component of the PPCS program is the utilization of an Electronic Medical Records (EMR) system. The EMR contains patient information such as demographic data, consult time, diagnoses, laboratory results, treatment, and health expenditures. It provides a more efficient system of tracking patient visits, provider workloads, and health-related expenses. In the rural PPCS pilot site, the primary care system was established through a service delivery network (SDN) composed of the rural health unit (RHU) and 14 barangay health stations (BHS). The health human resources in the RHU consists of two physicians, 2-3 nurses and 1-2 midwives per day, while one midwife is available for each BHS. The EMR system was introduced in April 2019, which led to accurate documentation of patient visits and monitoring of healthcare delivery.3
The effectiveness of a primary healthcare system is evaluated through its impact on healthcare delivery, quality, and access. Turnaround time is an integral component of primary care practice and is a key performance indicator of healthcare delivery. It is defined as the time patients spend during a healthcare facility visit. It may be evaluated in terms of its components – waiting time and consultation time.
Waiting time is measured from the time of patient's entry to the care facility until the actual consultation time. This includes registration and pre-consultation assessment. A study done to assess patient satisfaction to ambulatory care services showed that waiting time is one of the biggest contributors to patient satisfaction and influences adherence to management and follow up.4 Long waiting time is perceived by patients as a barrier to health services.5 Studies done in the primary care setting in Nigeria used a standard of 30 minutes waiting time as recommended by the Institute of Medicine.6,7
Consultation time is measured as the time between the first greeting and the dismissal of a patient from the consultation room.8 It is an integral component of primary care practice and a central factor in medical practice. It is during this time that the patient-doctor relationship is initiated, actual health needs are identified, and therapeutic plans are established. The duration of face time with a physician is considered to be an important indicator of high-quality health care.9 In a systematic review of 67 countries, the average primary care physician consultation length ranged from as short as 48 seconds in Bangladesh to 22.5 minutes in Sweden. Alarmingly, short consultation lengths were more likely to adversely affect patient healthcare.10 Another study evaluated the strength of primary care in Europe and showed that patient satisfaction is higher among those with longer consultation time, since it allows more time for the physician to discuss treatment goals and options.11 Similarly, a study done at a general practice clinic in Nigeria showed that for every unit increase in consultation time, there was a corresponding increase in patient satisfaction level.6 It is generally concluded that longer consultation times in primary care is linked with better quality of care and improved health-related outcomes.12 A study done by Aytona and colleagues in 2022 used consultation time as a variable in computing workload indicators for staffing needs, highlighting its importance in determining staffing standards for primary care services.2
In the PPCS, turnaround time includes both patient waiting time and consultation time, and is considered a measure of administrative efficiency.3 Several studies have been conducted to evaluate waiting times and consultation times in many countries, including neighboring Southeast Asian countries. Local studies are limited.1
No actual value has been established as the standard or acceptable turnaround time in primary care settings. This can be attributed to marked differences in structural characteristics of health systems as well as in the sociodemographic characteristics of patients and physicians across countries. A 2017 study that assessed patient waiting and consultation time in a primary healthcare clinic in Malaysia based its standards and target criteria according to the recommendation of the Malaysian Ministry of Health.13
A survey conducted by the British Medical Association showed that 95 percent of general physicians perceive that 10 minutes is insufficient for primary care consultations and that at least 15 minutes should be spent in appointments.14
Several factors affect consultation time. Physician factors included sex, age, and specialization. Physicians engaged in general practice and mental health care had longer turnaround times.8,15 Patient factors included sex, age, ethnicity, and educational attainment. Patients coming in for initial consult, those with multiple health problems, and those with complaints related to behavioral or psychiatric conditions required longer consultation times.16 In the present time when technological advancements are in place, patients are more engaged in their management. This is evidenced by the longer duration of primary consultation care documented over the years, compared to the earliest study conducted by Fry and Watts in 1952 which showed an average consultation time of 5 to 7.2 minutes.8
OBJECTIVES
This study aimed to determine the turnaround time of consults in the primary care system in a rural site in the Philippines, and compare turnaround time during the pre-pandemic and COVID-19 pandemic period. The results of this study can aid in the development of policies for workforce planning and achieving cost-effective turnaround times, and provide information on strengths and gaps in primary care practice in order to strengthen existing systems.
METHODS
Study Design
This was a retrospective cohort study utilizing a review of time-stamped EMRs of patients seen at the primary care system under the PPCS rural site from April 2019 to March 2021.
Study Population
This study included all adult and pediatric patients at the PPCS rural site primary care system via face-to-face consult from April 2019 to March 2021. Age restrictions were not imposed; thus, patients from all ages, from newborns to elderly patients were included. The study excluded patients whose turnaround times are reflected in the EMR as “8 hours or more” and “zero”, since this was attributed to technical difficulties and bugs in the EMR. Both initial and follow-up consults were included.
The pre-pandemic period was defined in this study from April 2019 to March 2020, since March 15, 2020 was the first day that lockdowns were instituted in the country. The COVID-19 pandemic period was defined as the period from April 2020 to March 2021.
Sample Size Calculation
The sample size was computed using a formula to compare means from two independent groups. Values were derived in reference to two Philippine studies. A study by Cenizal et al. in 2020 conducted in the pre-pandemic time showed mean turnaround time of 117 minutes with a standard deviation of 51.5 minutes.17 Another study by Laviña et al. during the pandemic in 2021 showed a mean turnaround time of 109 minutes with a standard deviation of 39.2 minutes.18 Using the difference between mean turnaround time in the two studies of 8 minutes, the computed sample size for this study is 342 participants divided equally into the pre-pandemic and pandemic period (171 participants each).
Description of Study Procedure
Data Collection
Data was retrieved from the EMR of the PPCS rural site primary care system. The flow of a patient’s movement during a primary care visit is described in Figure 1. Upon arrival at the healthcare facility, patients were seen at the triage and those deemed as emergency cases were immediately sent to a tertiary hospital via an online referral system. Patients for consultation were directed to the registration area. First-time consults were registered into the EMR. Records of patients on follow-up consults were retrieved from the EMR using a unique patient number. This timepoint was recorded as start of consult. The end of consult timepoint was recorded upon pressing of the “End Visit” button by the physician after the consultation. Time elapsed is automatically recorded in the system as the time from start of consult to the end of consult, and is regarded as the turnaround time in this study. Due to the limitations in the EMR configuration, separate analysis for the waiting time and consultation time could not be conducted. Thus, for the purpose of this study, turnaround time is defined as the total time (in minutes) from registration to the end of consultation, and encompasses both waiting time and consult time.
Figure 1.
Flow chart showing patient’s movement in the primary care system from arrival to departure.
Encoding and Processing
Raw data was encoded and tallied in a password-protected Microsoft Excel file. Each patient was assigned a code to ensure confidentiality of data. Data was stored in the principal investigator's laptop which was secured by a password accessible to the principal investigator only.
Statistical Analysis
Descriptive statistics was used to summarize data on turnaround time. Patient details included sociodemographic characteristics (age, sex, and place of residence) and clinical information (primary diagnosis and type of consult). Categorical data was reported in frequencies and percentages. Continuous variables were reported as mean and standard deviation for normally distributed data, and median and interquartile range (IQR) for data that did not follow normal distribution. Missing data were reported as “no data” in the results section and excluded in the analysis. The turnaround time before and during the pandemic was compared using an independent sample t-test (if normally distributed) or Mann Whitney U test (if not normally distributed). A p-value of <0.05 was considered statistically significant.
Ethical Considerations
The study was done through the provision of PPCS as one of the performance indicators for administrative efficiency. The study is exempted from the University of the Philippines Manila Research Board (UPMREB) with study protocol code number UPMREB 20-15-489-01. Given that aggregate data and no personally identifying information was used, informed consent was not required. The study was conducted in compliance with the Data Privacy Act of 2012. All records were anonymized.
RESULTS
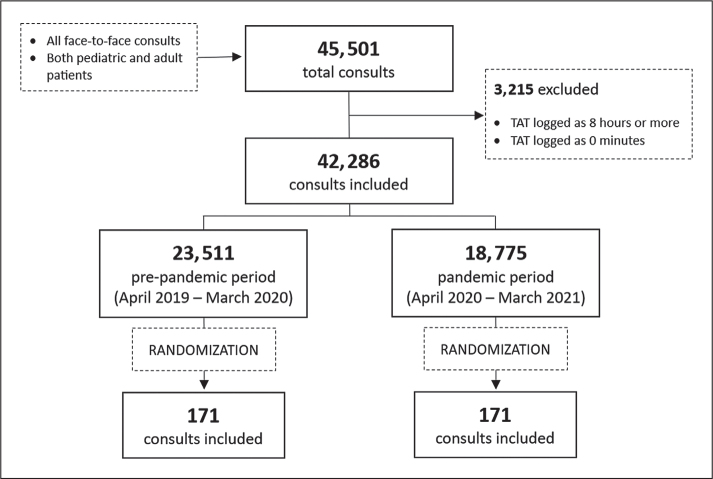
A total of 45,501 consults were logged at the rural primary care system from April 2019 to March 2021. We excluded 3,200 consults whose turnaround time were logged as “8 hours or more” and 15 consults erroneously logged as zero. A total of 23,511 consults were logged during the pre-pandemic period from April 2019 to March 2020. There were 18,775 consults logged during the COVID-19 pandemic period from April 2020 to March 2021. A total of 171 participants were randomly selected from the pre-pandemic period and the pandemic period, with a total sample size of 342 participants for this study (Figure 2).
Figure 2.
Flow diagram of study participants.
Sociodemographic characteristics of patients seen in the primary care system
Table 1 outlines the sociodemographic characteristics of the 342 study participants. In the pre-pandemic period (n = 171), 43% were pediatric patients while 57% were adults. The participants’ ages ranged from newborn to 97 years old. Majority of patients (60%) were females. Sixty percent of consultations came from lowland barangays.
Table 1.
Sociodemographic Characteristics of Patients Seen at the PPCS Rural Site Primary Care Health System before and during the COVID-19 Pandemic
| Pre-pandemic n=171 (%) | Pandemic n=171 (%) | Total n=342 (%) | |
|---|---|---|---|
| Age Group | |||
| Newborn | 10 (5.9) | 7 (4.1) | 17 (5.0) |
| Under 5 years | 26 (15.2) | 13 (7.6) | 39 (11.4) |
| 5 to <19 years | 37 (21.6) | 13 (7.6) | 50 (14.6) |
| 19 to <60 years | 64 (37.4) | 110 (64.3) | 174 (50.9) |
| Senior Citizen | 34 (19.9) | 28 (16.4) | 62 (18.1) |
|
| |||
| Sex | |||
| Male | 68 (39.8) | 82 (48.0) | 150 (43.9) |
| Female | 103 (60.2) | 89 (52.0) | 192 (56.1) |
|
| |||
| Place of Residence | |||
| Upland barangay | 32 (18.7) | 45 (26.3) | 77 (22.5) |
| Lowland barangay | 102 (59.7) | 119 (69.6) | 221 (64.6) |
| No data | 37 (21.6) | 7 (4.1) | 44 (12.8) |
|
| |||
| Employment | |||
| Private employee | 8 (4.7) | 24 (14.0) | 32 (9.4) |
| Government employee | 2 (1.7) | 7 (4.1) | 9 (2.8) |
| Student | 33 (19.3) | 18 (10.5) | 51 (14.9) |
| Others (not specified)* | 30 (17.5) | 59 (34.5) | 89 (26.0) |
| No data | 98 (57.3) | 63 (36.8) | 161 (47.1) |
|
| |||
| Special Populations | |||
| Indigent | 2 (1.2) | 0 (0) | 2 (0.6) |
| 4Ps** member | 4 (2.4) | 1 (0.6) | 5 (1.5) |
| Persons with Disabilities | 5 (2.9) | 1 (0.6) | 6 (1.8) |
| Pregnant | 16 (9.4) | 7 (4.1) | 23 (6.7) |
Recorded as “Others” in the EMR but no details provided
4Ps – Pantawid Pamilyang Pilipino Program
During the pandemic period (n = 171), there was a marked decrease in the pediatric consults, with the majority of consults (81%) belonging to the adult population. Female patients accounted for 52% of consults. Majority of patients (70%) came from lowland barangays.
Turnaround time of medical consults
The turnaround time is reported in Table 2. Overall, the median turnaround time in the primary care system is 29.0 minutes (IQR 68.3). There is no significant difference in the median turnaround time of consults between the pre-pandemic and the pandemic periods (P = 0.39).
Table 2.
Turnaround Time of Patients Seen at the PPCS Rural Site Primary Care Health System before and during the COVID-19 Pandemic
| Time Period | Median (IQR) in minutes | Range in minutes |
|---|---|---|
| Pre-pandemic | 29.3 (70.4) | 1.7-370.8 |
| Pandemic | 27.5 (72.7) | 0.9-437.2 |
| Overall | 29.0 (68.3) | 0.9-437.2 |
DISCUSSION
The PPCS rural site primary care system serves as a catchment area with a population of 38,302.19 Healthcare services are provided through the primary care system composed of the rural health unit (RHU) and its 14 barangay health stations (BHS). Review of EMR showed that 45,501 face-to-face consults were recorded over two years. Turnaround time ranged from as short as 0.9 minutes to as long as 437.2 minutes.
Turnaround time in the primary care system
In this study, the median turnaround time of consults in the primary care system is 29.0 minutes (IQR 68.3). This result is almost one-fourth of that reported in two local studies. A study by Cenizal et al. in 2020 set in the pre-pandemic time showed mean turnaround time of 117 minutes while another study done during the pandemic by Laviña et al. in 2019 showed a mean turnaround time of 109 minutes.17,18 This may be attributed to differences in setup, system processes, and variances among physicians and patients. In our study, maintenance medication refills, requests for medical certification, and interpretation of laboratories were the usual reasons for consults with shorter turnaround times. Consults for chief complaints such as respiratory symptoms and abdominal pain had longer turnaround times, which is likely due to the need for more thorough history taking and physical examination.
Comparison to a study done in another Southeast Asian country showed that this study has a shorter turnaround time. A study by Ahmad et al. in a primary healthcare clinic in Malaysia showed an average of 59.3 minutes – broken down into 41.1 minutes waiting time and 18.2 minutes consultation time. It also showed that the turnaround time varied from as short as 0.6 minutes to as long as 477.6 minutes. This primary healthcare clinic in Malaysia was situated in a large district that catered to 682,996 people, whereas the rural site in this study catered to 35,298 residents across 14 barangays. Moreover, the Malaysian study identified that the long waiting time was due to long queues in registration due to inadequate staff, where only one staff was in charge of both registration and provision of follow-up appointments.13 In contrast, one of the strategies implemented by the PPCS to improve healthcare services was to augment healthcare providers. The rural primary care facility had three physicians, 16 nurses, 20 midwives, and 100 community health workers. Registration at the BHS was handled by the midwives.20
Turnaround time in the primary care system during the pandemic
The primary care system saw a decrease in face-to-face consults by 20% in the pandemic period. This is consistent with findings in a study by Tu et al. across nine countries which compared the patient visit volume in the pandemic period to the pre-pandemic period, showing a decrease in patient visits by 26% among the Asian countries included.21 Another study in the primary care setting in Germany also showed a dramatic reduction in the number of consultations by 49%. This drop was independent of age, sex, and practice location.22 The decrease in the number of consults is attributed to the implementation of protocols aimed to reduce viral transmission. In the German study, the decrease in in-person visits coincided with the shift to virtual consults, which is likewise seen in our study setting. The PPCS primary care system opened an online consultation in April 2021 to continue addressing community health needs. This service began with an average of 15 to 20 patients per day and gradually increased over the course of the pandemic.23
There is no significant difference in the median turnaround times before and during the pandemic in this study. During the pandemic, new protocols had to be instituted to ensure patient and healthcare personnel safety. For example, healthcare workers had to don appropriate personal protective equipment (PPE) prior to seeing patients. The whole system also saw a change in the process flows such as patient pathways and physical set-up. Despite the new protocols, there was no significant change in turnaround time from pre-pandemic to pandemic times. This finding contrasts to the results of several studies which report that the COVID-19 pandemic affected health service delivery. The impact of the pandemic was wide-reaching, with changes in physical set-up of the clinics, human resource allocation, and process flows to accommodate influx of patients and enforce infection control measures.18 Such changes influence turnaround times of consults. A study done in a general practice clinic in Nigeria showed that any changes to the patient flow can increase waiting time, thus affecting the overall turnaround time.6 The pandemic turnaround time of 27.5 minutes is shorter compared to a similar study done at the UP Health Service (UPHS) setting of the Philippine General Hospital (PGH) which showed an average of 108.68 minutes. This may be attributed to additional service areas in the UPHS setting such as swabbing booths and screening tests which were included in their reported turnaround time.18
Limitations
The study was conducted in one rural setting in the Philippines hence it may be limited in terms of generalizability and applicability to other healthcare settings. The study only included a random sample of records (342 out of 45,501 records). Records with turnaround time of “8 hours or more” and “zero” were excluded, since they were likely due to technical bugs in the EMR.” Data is also limited to retrievable information in the electronic medical records. Instances of technological challenges such as internet and electricity disruptions on the field may have affected the accuracy of documentation of turnaround times.
Another limitation is that the turnaround time was measured as the sum of both waiting time and consultation time. As seen in related literature, longer waiting time is perceived as a barrier to health service, while longer consultation time is actually linked to better quality of care. In this study, both waiting time and consultation time were considered together as turnaround time as a measure of administrative efficiency. Future studies that can investigate the individual components of waiting time and consultation time are needed.
Another limitation is that the current EMR does not provide information on the type of consultation, whether initial or follow-up consult. This is a possible effect modifier that may affect turnaround time. We also could not compare if the proportion of initial and follow-up consults were similar for the pre-pandemic and pandemic periods. Other possible effect modifiers, such as age of patient, severity of symptoms, presence of co-morbidities, were also not explored since this is beyond the scope of the study.
CONCLUSION AND RECOMMENDATIONS
This study showed a median turnaround time of 29.0 minutes, which is shorter by 80 minutes compared to other local studies. This study can aid in workforce planning in primary care facilities with similar settings, and provide information for policies that aim to optimize turnaround times. Evaluation of systems should be done to target optimal allocation of workforce according to facility burden. Quality improvement studies are needed to decrease wait times and increase consult times. The turnaround time did not differ significantly in the pandemic and pre-pandemic period, despite new policies and systems that were implemented during the pandemic.
Further studies are recommended to analyze determinants of turnaround time including physician and patient factors. Studies focusing on outcomes such as patient satisfaction, treatment adherence, and health outcomes may also be explored. The EMR can be improved by allowing healthcare workers to log waiting time separately from consult time so that further studies can be done to analyze these variables independently. Policies may be developed to target reduction in waiting time to improve efficiency of service delivery. This includes proper allocation and augmentation of human resources. The development of a scheduling system for patient visits may help improve process flow and patient management. Addition of a field in the EMR to identify the type of consult as initial or follow-up is recommended to improve data gathering and analysis.
Statement of Authorship
All authors certified fulfillment of ICMJE authorship criteria.
Author Disclosure
All authors declared no conflicts of interest.
REFERENCES
- 1.Ansell D, Crispo JAG, Simard B, Bjerre LM. Interventions to reduce wait times for primary care appointments: a systematic review. BMC Health Serv Res. 2017. Apr;17(1):295. doi: 10.1186/s12913-017-2219-y. PMID: 28427444; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aytona MG, Politico MR, McManus L, Ronquillo K, Okech M. Determining staffing standards for primary care services using workload indicators of staffing needs in the Philippines. Hum Resour Health. 2022. Jan;19(Suppl 1):129. doi: 10.1186/s12960-021-00670-4. PMID: 35090487; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Philippine Primary Care Studies . Philippine Primary Care Studies - Program description & Method overview v1.4. Philippine Primary Care Studies. 2019. [Google Scholar]
- 4.Ali MAS, Amirthalingam P, Alatawi Y, Aljabri A. Patient satisfaction of ambulatory care pharmacy services. J Patient Exp. 2022. Jul;9:23743735221112631. doi: 10.1177/23743735221112631. PMID: 35846246; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oche M, Adamu H. Determinants of patient waiting time in the general outpatient department of a tertiary health institution in north Western Nigeria. Ann Med Health Sci Res. 2013. Oct;3(4):588-92. doi: 10.4103/2141-9248.122123. PMID: 24380014; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Enabulele O, Ajokpaniovo J, Enabulele JE. Patient waiting and consultation time in the General Practice Clinic of the University of Benin Teaching Hospital, Edo State, Nigeria. J Family Med Community Health. 2018;5(2):1146. [Google Scholar]
- 7.Anyanwu O, Ezeonu T, Orji ML, Ezeanosike O, Ikegwuonu C, Omeje K, et al. Waiting time analysis in a paediatric outpatient clinic in South East Nigeria. Med Sci Discov. 2021;8(2):50–9. doi: 10.36472/msd.v8i2.459. [DOI] [Google Scholar]
- 8.Torres AR, Soto ECJ, Patiño DC. Medical consultation, time and duration. Medwave. 2018. Sep;18(5):e7266. doi: 10.5867/medwave.2018.05.7264. PMID: 30312289. [DOI] [PubMed] [Google Scholar]
- 9.Patwardhan A, Davis J, Murphy P, Ryan SF. Comparison of waiting and consultation times in convenient care clinics and physician offices: a cross-sectional study. J Prim Care Community Health. 2013. Apr;4(2):124-8. doi: 10.1177/2150131912450030. PMID: 23799720. [DOI] [PubMed] [Google Scholar]
- 10.Irving G, Neves AL, Dambha-Miller H, Oishi A, Tagashira H, Verho A, et al. International variations in primary care physician consultation time: a systematic review of 67 countries. BMJ Open. 2017. Nov;7(10):e017902. doi: 10.1136/bmjopen-2017-017902. PMID: 29118053; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kringos D, Boerma W, Bourgueil Y, Cartier T, Dedeu T, Hasvold T, et al. The strength of primary care in Europe: an international comparative study. Br J Gen Pract. 2013. Nov;63(616):e742-50. doi: 10.3399/bjgp13X674422. PMID: 24267857; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elmore N, Burt J, Abel G, Maratos FA, Montague J, Campbell J, et al. Investigating the relationship between consultation length and patient experience: a cross-sectional study in primary care. Br J Gen Pract. 2016. Dec;66(653):e896-e903. doi: 10.3399/bjgp16X687733. PMID: 27777231; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahmad BA, Khairatul K, Farnaza A. An assessment of patient waiting and consultation time in a primary healthcare clinic. Malays Fam Physician. 2017. Apr;12(1):14–21. PMID: 28503269; PMCID: . [PMC free article] [PubMed] [Google Scholar]
- 14.Das MC, Zakaria M, Cheng F, Xu J. Appointment length with patients in medical consultations in Bangladesh: a hospital-based cross-sectional study. Healthcare (Basel). 2021. Sep;9(9):1164. doi: 10.3390/healthcare9091164. PMID: 34574938; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hajizadeh A, Kakemam E, Khodavandi M, Khodayari-Zarnaq R. Factors affecting outpatient consultation length among specialists in Tabriz, Iran. Evid Based Health Policy Manage Econ. 2019;3(4):276-83. doi: 10.18502/jebhpme.v3i4.2069. [DOI] [Google Scholar]
- 16.Petek Ster M, Svab I, Zivcec Kalan G. Factors related to consultation time: experience in Slovenia. Scand J Prim Health Care. 2008;26(1):29-34. doi: 10.1080/02813430701760789. PMID: 18297560; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cenizal C, Anuran G. Triage and Registration Time in the Outpatient Services of a Government Tertiary Hospital in Manila, Philippines: A Time Motion Study. Department of Family and Community Medicine, University of the Philippines – Philippine General Hospital; 2019. Unpublished. [Google Scholar]
- 18.Laviña SMS, Mejia-Samonte M, Anuran GO, Lenora Villarante K, Limpoco AGO. Patient flow, health delivery processes, and areas for improvement in the UPHealth Service (UPHS) during May to June 2020 of the COVID-19 pandemic. Acta Med Philipp. 2021;55(2):231-6. doi: 10.47895/amp.v55i2.2755. [DOI] [Google Scholar]
- 19.Philippine Statistics Authority . SPECIAL RELEASE - Household Population, Number of Households, and Average Household Size of Municipality of Samal (2020 Census of Population and Housing) [Internet] 2022 May 26 [cited 2022 Jul]. Available from: https://rsso03.psa.gov.ph/article/special-release-household-population-number-households-and-average-household-size-8.
- 20.Bernal-Sundiang N, De Mesa RYH, Marfori JRA, Fabian NMC, Calderon YT, Dans LF, et al. Governance in primary care systems: experiences and lessons from urban, rural, and remote settings in the Philippines. Acta Med Philipp. 2023;57(3):5-16. doi: 10.47895/amp.vi0.4834. [DOI] [Google Scholar]
- 21.Tu K, Sarkadi Kristiansson R, Gronsbell J, de Lusignan S, Flottorp S, Goh LH, et al. INTRePID . Changes in primary care visits arising from the COVID-19 pandemic: an international comparative study by the International Consortium of Primary Care Big Data Researchers (INTRePID). BMJ Open. 2022. May;12(5):e059130. doi: 10.1136/bmjopen-2021-059130. PMID: 35534063; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schäfer I, Hansen H, Menzel A, Eisele M, Tajdar D, Lühmann D, et al. The effect of COVID-19 pandemic and lockdown on consultation numbers, consultation reasons and performed services in primary care: results of a longitudinal observational study. BMC Fam Pract. 2021. Jun;22(1):125. doi: 10.1186/s12875-021-01471-3. PMID: 34162343; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Esconde E. Samal RHU opens online consultation. Punto! Central Luzon [Internet]. 2020. Apr 21 [cited 2022 Aug]. Available from: https://punto.com.ph/samal-rhu-opens-online-consultation/.