Abstract
Telangiectasia macularis eruptiva perstans (TMEP) is a rare disease, previously classified as a variant of cutaneous mastocytosis. While no gold standard of treatment exists, several treatments have been studied. We report a case of a 63-year-old woman who presented with long-standing asymptomatic telangiectatic macules beginning on the upper chest, back, and bilateral arms, with occasional pruritus and no other systemic symptoms. Skin biopsy, along with Giemsa stain, revealed findings consistent with TMEP. The patient underwent testing for serum tryptase level, which was within normal limits. The patient was started on topical steroids for two weeks and antihistamine therapy, with a noted decrease in pruritus but no change in cutaneous lesions. She was then advised to start phototherapy, and subsequently underwent a total of five sessions of narrow-band ultraviolet B phototherapy, after which she noted lightening of the lesions. Due to the COVID pandemic, the patient was shifted to heliotherapy with continued lightening of lesions after two months of thrice weekly sessions. This rare case is supportive of narrow-band ultraviolet B phototherapy and heliotherapy as promising treatment options for cases of TMEP.
Keywords: mastocytosis, telangiectasia macularis eruptiva perstans, phototherapy, heliotherapy
INTRODUCTION
Mastocytosis is a rare myeloproliferative disorder characterized by an abnormal collection of mast cells in one or more organs. Telangiectasia macularis eruptiva perstans (TMEP) is an extremely rare variant, comprising less than 1% of mastocytosis cases.1,2 Although it is generally confined to the skin, it can also manifest as headache, flushing, syncope, or diarrhea.1,2 Symptomatic treatment is the mainstay of treatment (antihistamines and trigger avoidance). For purely cutaneous disease, no gold standard of treatment is recognized.1,3
CASE REPORT
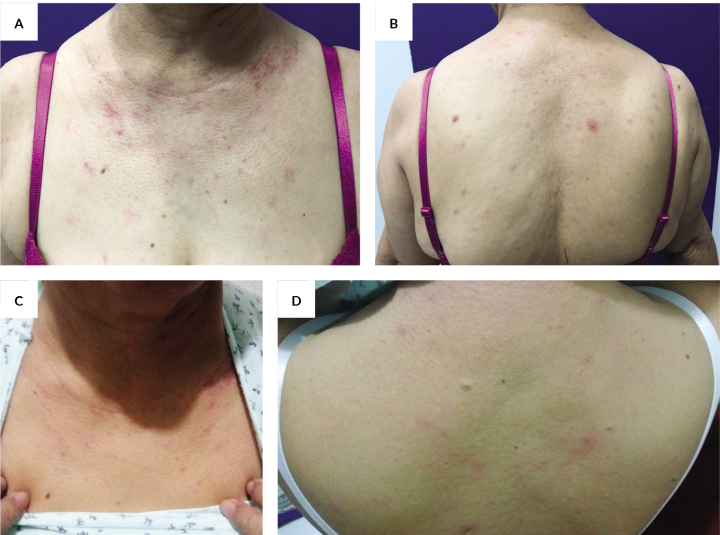
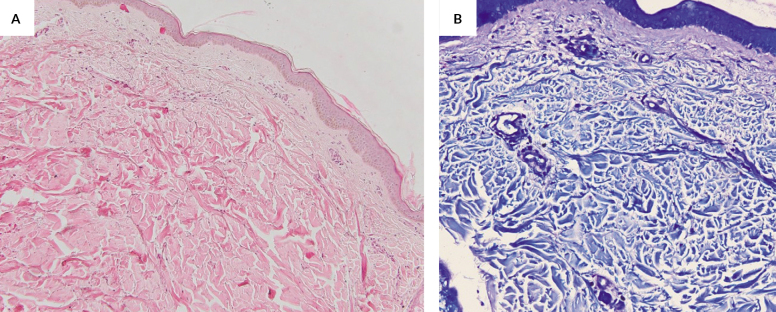
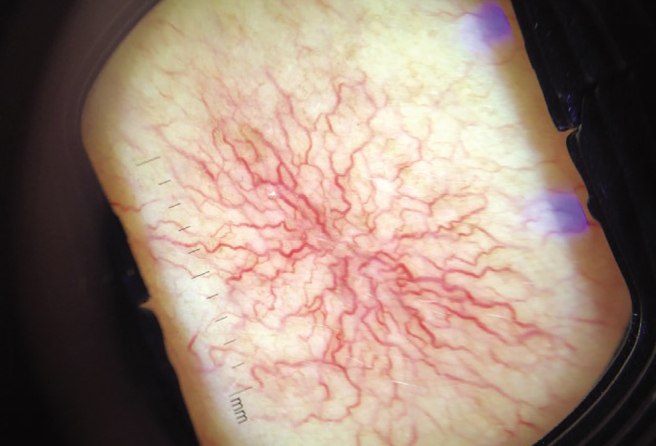
A 63-year-old Filipino woman presented with a 3-yearhistory of asymptomatic telangiectatic macules beginning on the upper chest and back, gradually spreading to bilateral arms, with occasional pruritus. She denied systemic symptoms (such as dizziness, fatigue, syncope, flushing, diarrhea, fever, weight loss, abdominal pain, or jaundice), aggravating factors, and other illnesses (such as hypertension, diabetes mellitus, thyroid disease, or liver disease). Multiple discrete erythematous telangiectatic macules and patches were found on the upper chest, back, and arms (Figures 1A and 1B). Darier’s sign was negative. Dermoscopy revealed thin and tortuous linear vessels with a reticular vascular pattern (Figure 2). Laboratory tests showed mild thrombocytopenia, elevated liver enzymes, and normal serum tryptase level. Biopsy demonstrated an atrophic epidermis and papillary dermal edema with sparse lymphocytic infiltrates and mast cells (Figure 3A). Giemsa stain was positive (Figure 3B).
Figure 1.
(A and B) Baseline photographs of a patient with multiple erythematous telangiectatic macules and patches distributed on the upper chest, upper back, and upper arms. (C and D) Significant improvement was observed after 5 sessions of NB-UVB phototherapy followed by 20 sessions of heliotherapy.
Figure 2.
Dermoscopy demonstrates thin and tortuous linear vessels with a reticular vascular pattern.
Figure 3.
(A) Biopsy demonstrated an atrophic epidermis and papillary dermal edema with sparse lymphocytic infiltrates and the presence of mast cells (H&E, x100). (B) Giemsa stain was positive for the presence of mast cells (x400).
The patient started topical steroids and antihistamine therapy for two weeks, with improvement in pruritus but no change in cutaneous lesions. She then started thrice weekly NB-UVB phototherapy at a dose of 300 mJ/cm2, increasing by 20% per session. Five sessions decreased the erythema and resolved her pruritus. Although the plan was to complete 30 sessions of NB-UVB phototherapy, this was impossible because of the enhanced community quarantine. She started heliotherapy by bathing in natural sunlight for 20 minutes from 7 to 8 am thrice weekly. As of this writing, she has completed seven weeks of heliotherapy (with a total of 20 sessions). On her follow-up consult via teledermatology, the patient reported significant lightening of most skin lesions (Figures 1C and 1D).
DISCUSSION
Mastocytosis is caused by an abnormal accumulation of mast cells in different organ systems and can be classified into cutaneous mastocytosis, extracutaneous mastocytosis, mast cell sarcoma, and systemic mastocytosis.4 Previously classified by the World Health Organization as a rare variant of cutaneous mastocytosis, TMEP demonstrates a prominent increase in mast cells in the superficial dermis with dilation of the superficial capillaries. Aside from affecting the skin, it may infiltrate other organs (bone, liver, spleen, lymph nodes, and gastrointestinal tract).1
Phototherapy is effective in treating cutaneous mastocytosis.3,4 Ultraviolet (UV) light inhibits the release of histamine, induces mast cell apoptosis, and decreases tryptase levels.4 Although psoralen-UVA (PUVA) phototherapy is more widely used, NB-UVB phototherapy has proven effective in mastocytosis, TMEP, and urticaria pigmentosa;2,3 it lightens lesions and decreases pruritus after 24 to 36 sessions.2,5 While PUVA works faster, NB-UVB requires lower UV exposure and is thus safer and more tolerable.4 Our patient improved after only five sessions of NB-UVB phototherapy; we can assume that more sessions would have even better results.
Heliotherapy is the therapeutic use of natural sunlight in the treatment of skin disease. It has since lost favor to its successor, modern-day phototherapy, but remains effective in compliant patients when phototherapy is inaccessible.6,7 The patient is instructed to expose the lesions to natural sunlight for “as long as possible without getting sunburned.”7 Like phototherapy, it treats lesions of mastocytosis and urticaria pigmentosa.8,9
This rare case shows that NB-UVB phototherapy and heliotherapy are viable treatment options for TMEP. We hope to study its outcomes in the long term.
Ethics Statement
The authors confirm that written consent was obtained from the patient for the publication of this case report. The authors have obtained the informed consent form in which the patient has given consent for her clinical information and photographs to be published in the journal. The patient was informed and understands that her name and initials will not be published and that efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Statement of Authorship
Both authors contributed in the conceptualization of work, acquisition and analysis of data, drafting and revising, and approved the final version submitted.
Author Disclosure
Both authors declared no conflicts of interest.
Funding Source
The study has no funding support.
REFERENCES
- 1.Watkins CE, Bokor WB, Leicht S, Youngberg G, Krishnaswamy G. Telangiectasia macularis eruptiva perstans: more than skin deep. Dermatol Rep. 2011; 3(12):23-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rishpon A, Matz H, Gat A, Brenner S. Telangiectasia macularis eruptiva perstans: unusual presentation and treatment. SKINmed. 2006; 300-2. [DOI] [PubMed] [Google Scholar]
- 3.Costa DL, Moura HH, Rodrigues R, Pineiro-Maceira J, Ramos-ESilva M. Telangiectasia macularis eruptiva perstans: a rare form of adult mastocytosis. J Clin Aesthet Dermatol. 2011; 4(10):52-4. [PMC free article] [PubMed] [Google Scholar]
- 4.Brazzelli V, Grassi S, Merante S, et al. Narrow-band UVB phototherapy and psoralen–ultraviolet A photochemotherapy in the treatment of cutaneous mastocytosis: a study in 20 patients. Photodermatol Photoimmunol Photomed. 2016. Sep; 32(5-6):238-46. [DOI] [PubMed] [Google Scholar]
- 5.Prignano F, Troiano M, Lotti T. Cutaneous mastocytosis: successful treatment with narrowband ultraviolet B phototherapy. Clin Exp Dermatol. 2010; 35(8):914-5. [DOI] [PubMed] [Google Scholar]
- 6.Campbell J. Safe and effective use of phototherapy and photochemotherapy in the treatment of psoriasis. Br J Nurs. 2020. May 28; 29(10):547-52. [DOI] [PubMed] [Google Scholar]
- 7.Koo J, Nakamura M. Clinical Cases in Phototherapy. Springer International Publishing; 2017. pp. 77-78. [Google Scholar]
- 8.Wilson TM, Metcalfe DD, Robyn J. Treatment of systemic mastocytosis. Immunol Allergy Clin. 2006. Aug 1; 26(3):549-73. [DOI] [PubMed] [Google Scholar]
- 9.Vire G, Roberts LJ, King LE. Urticaria pigmentosa and natural sunlight. J Am Acad Dermatol. 1986. Apr 1; 14(4):687-8. [DOI] [PubMed] [Google Scholar]