Abstract
Objectives
In the Philippines, an estimated half million are affected annually by stroke. It is the third most common cause of mortality among Filipinos. Locally, there are limited data on the epidemiology of stroke in the country. This study aimed to study cerebrovascular disease in the rural setting in the country, primarily exploring the demographic characteristics, risk factors, clinical profile, and outcomes of patients assessed with cerebrovascular disease in the province of Sorsogon.
Methods
This was a retrospective study of all adult patients admitted to two tertiary hospitals in Sorsogon between February 1, 2020, and January 31, 2021, with a stroke diagnosis (International Classification of Diseases, Revision 10). A manual review of the charts and demographics, risk factors, clinical presentation, neuroimaging findings, and outcome were recorded.
Results
A total of 721 cases with a mean age of 63.06 ± 13.96 years were involved in the analysis. Of all the stroke cases, 64.7% were ischemic, and 29.7% were hemorrhagic strokes. The most common risk factors for stroke occurrence were hypertension (65%), history of stroke (16.2%), and diabetes (11.4%). Most sought consultation was due to one-sided weakness (41.3%) and slurring speech (14.2%).
Conclusion
In a third-class province in the Philippines, the most common type of stroke was an ischemic stroke. Analysis showed that diabetes was more associated with ischemia while hypertension was significantly associated with hemorrhagic stroke. A mortality rate of 26.8% was seen in this cerebrovascular disease population.
Keywords: stroke, clinical profile, risk factors, Philippines, rural, epidemiology
INTRODUCTION
Stroke currently accounts for the second leading cause of death and a second most common cause of global Disability Adjusted Life Years (DALYs) worldwide.1 Parallel to international studies, ischemic stroke occurs more frequently than hemorrhagic stroke.2 Age-standardized death rates of stroke increased in East Asia.3 Locally, with an estimated half a million affected annually, stroke is included in the top three most common causes of mortality among Filipinos.4 As low to middle-income countries go through the epidemiological transition from infectious to non-communicable diseases as the predominant cause of morbidity, the burden of stroke will further increase until effective stroke prevention strategies are more widely implemented. The DALYs lost reflect the stroke burden as it translates to net effects of the morbidity and economic productivity of the affected population.2,5,6
A study of first-time cerebrovascular disease cases across tertiary hospitals in 13 of 16 administrative regions of the Philippines identified hypertension, diabetes, transient ischemic attack (TIA), myocardial infarction (MI), atrial fibrillation (AF), rheumatic heart disease (RHD), migraine, habitual snoring, stress, frequent alcohol use, and body mass index (BMI) as significant local risk factors.7 Most of these are modifiable risk factors. Many Filipinos continue to die and get disabled from a preventable disease.
In the Philippines, many hospital-based studies, a few nationwide surveys, and one community-based study have investigated local epidemiological data on stroke.8 Most measured the prevalence of lifestyle-related diseases and risk factors in Filipinos. All with similar outcomes, the prevalence of stroke is estimated to be 1.4%. This study aimed to study cerebrovascular disease in the rural setting in the country, primarily exploring the demographic characteristics, risk factors, clinical profile, and outcomes of patients assessed with cerebrovascular disease in the province of Sorsogon, a region at the tip of the Bicol peninsula.
Sorsogon is a third-class province subdivided into fourteen municipalities and one city, ranging from first to fifthclass municipalities.9 It covers a total area of 2,119.01 square kilometers. It has an estimated population of 922,358 inhabitants in 2020.10 The Sorsogon Provincial Hospital, and Sorsogon Medical Mission Group Hospital and Health Services Cooperative are two of the three tertiary hospitals in the province. As the country embarks on launching the Universal Health Care Act toward a primary healthcareoriented and integrated health system, further local epidemiological data such as these can help the government identify the need to work together with an informed public on the gravity of stroke education and primary stroke management.
METHODS
Population and Sample
This was a retrospective study of all adult patients (≥18 years old) who were admitted at the Sorsogon Provincial Hospital and the Sorsogon Medical Mission Group Hospital and Health Services Cooperative between February 1, 2020, and January 31, 2021, with a diagnosis of stroke (International Classification of Diseases, Revision 10). Cerebrovascular disease diagnosis was mainly based on the physician's opinion, clinical features, and Computed Tomography (CT scan) reports.
Data Collection
A comprehensive list of patients admitted between February 1, 2020, and January 31, 2021, with a discharge diagnosis of cerebrovascular disease, was requested. The list was cross-referenced with a manual review of the charts contained in the medical records of both institutions. Charts were accessed with appropriate permissions. Patient identifiers were removed or kept confidential. In an excel form, the following criteria and clinical parameters were recorded: patient demographic data (age, gender, and town of origin), history of diseases (such as hypertension, diabetes, previous stroke, heart and kidney diseases), clinical profile (Glasgow Coma Scale [GCS], vital signs) and type of stroke seen in neuroimaging (hemorrhagic or ischemic). History of diseases was recorded based on self and family reporting.
Analysis
The Chi-square test was used to compare demographic groups, stroke occurrence, and types. One-way Analysis of Variance ANOVA and Kruskal-Wallis tests were used to compare proportions of chief complaints, comorbidities, and clinical profiles with stroke and stroke types. Logistic regression was used to identify significant risk factors for stroke and subtypes. Statistical significance is tested at 0.05 alpha with a 95% confidence level. Statistical calculations were run using SPSS version 20.
RESULTS
In total, 721 participants (479 were from Sorsogon Provincial Hospital and 241 from Sorsogon Medical Mission Group Hospital), with a mean age of 63.06 ± 13.96 years, were involved in the analysis. Of all the stroke cases, 64.7% were ischemic strokes, 29.7% were hemorrhagic strokes, and 5.5% were nontraumatic subarachnoid hemorrhages. Fifty-five percent (399) were men, and 44% (321) were women. A third (35.6%) of the participants were from Sorsogon City, while the majority was distributed from the 14 municipalities of the province.
As shown in Table 1, the risk of stroke (ischemic, hemorrhagic, and subarachnoid hemorrhage) increased with age (p<0.001). However, there was no statistically significant difference in the risk of stroke between men and women. In addition, the proportion of different types of stroke showed no significant differences by age group, sex, place of residence, or the number of hospital stays. The mean hospital stay was 6.55 ± 6.7 days.
Table 1.
Stroke types by demographic characteristics ICH* Infarct SAH
| ICH* | Infarct | SAH* | ||
|---|---|---|---|---|
| Total | 213 | 464 | 40 | |
| Age | Less 40 | 4.7% | 3.8% | 5.0% |
| 40-59 | 9.3% | 21.1% | 5.0% | |
| 50-59 | 18.8% | 29.1% | 20.0% | |
| 60-69 | 26.9% | 22.5% | 25.0% | |
| 70+ | 40.3% | 23.5% | 45.0% | |
|
| ||||
| Sex | F | 38.5% | 46.6% | 55.0% |
| M | 61.5% | 53.4% | 45.0% | |
ICH – intracerebral hemorrhage, SAH – subarachnoid hemorrhage
Figure 1 describes the proportion of stroke types by risk factors, clinical profile, and outcome. The most common risk factors for stroke occurrence are hypertension (65%), a previous history of cerebrovascular disease (16.2%), and diabetes mellitus (11.4%). Previous medical history of coronary artery disease was observed in 3.8% of cases, chronic kidney disease in 0.8%, chronic heart failure in 0.3%, and atrial fibrillation in 0.3% of cases.
Figure 1.
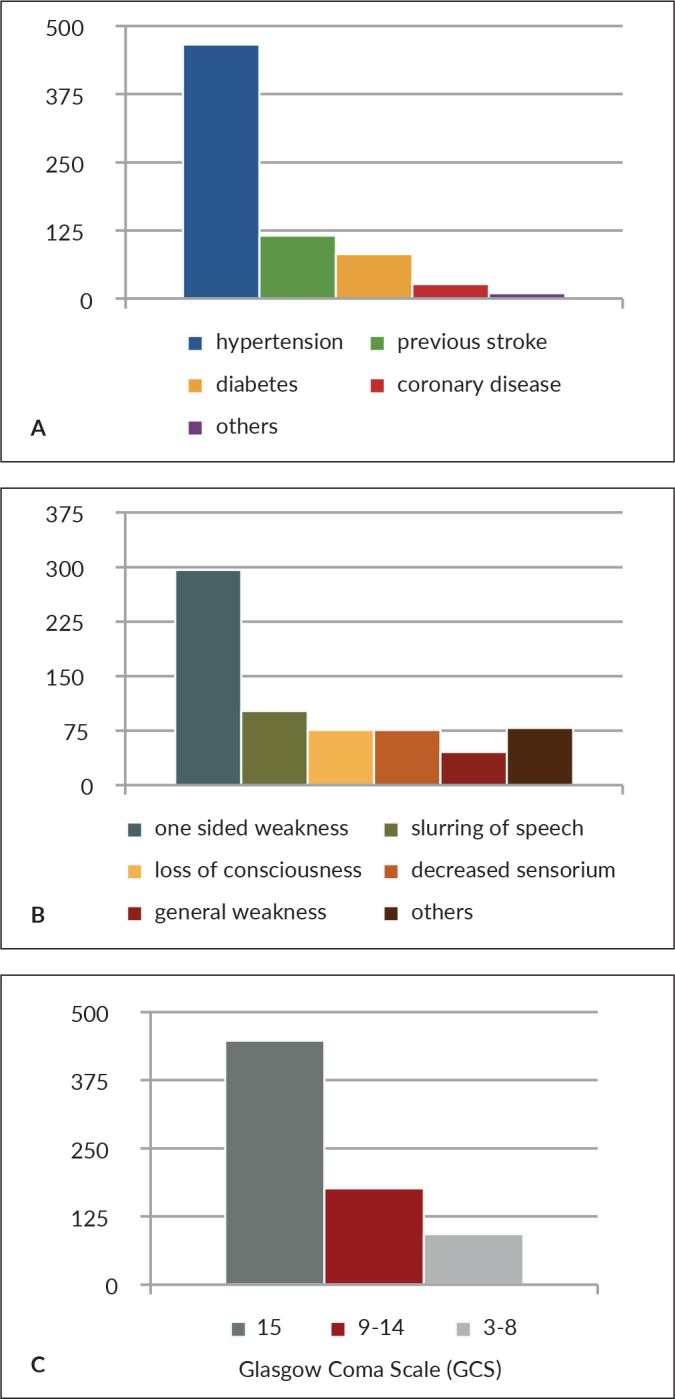
(A) Risk factors, (B) chief complaints and (C) clinical profile of stroke patients in Sorsogon.
Among the stroke cases in the province, most of them sought medical consultation due to one-sided weakness (41.3%), followed by slurring of speech (14.2%), decrease in sensorium (10.6%), and loss of consciousness (10.6%). Other chief complaints recorded were general weakness (6.4%), dizziness (6.3%), decrease in verbal output (2.6%), one-sided numbness (2.1%), headache (1.4%), and vomiting (1.3%).
Upon arrival at the institution, most would come in fully awake, GCS 15 (62.3%). Disoriented, drowsy to obtunded, Cerebrovascular Disease Population in Sorsogon or GCS 9-14 in 24.5% of stroke cases, and around 12.8% are stuporous or comatose, GCS 3-8. Almost 3/4 of stroke cases (75.9%) had systolic blood pressure levels greater than 130 mmHg. The majority of the stroke cases (73.2%) were discharged. However, a mortality rate of 26.8% is seen in this cerebrovascular disease population.
The multivariable logistic regression model indicated that multiple characteristics were positively associated with ischemic stroke, including age, diabetes, and a decrease in verbal output as clinical presentation. Table 2 shows that the older patients (OR = 1.027, 95%CI 1.015 to 1.039), patients with diabetes (OR= 1.763, 95%CI 0.994 to 3.125) or patients with a chief complaint of decrease in verbal output (OR= 4.528, 95%CI 1.254 to 16.347) were more likely to have an ischemic stroke. The model states that age and reduction of verbal output as a clinical presentation are statistically significant.
Table 2.
Multivariate logistic analysis of ischemic stroke profile among the population
| B | S.E. | Wald | df | Sig. | Odds | |
|---|---|---|---|---|---|---|
| Age | 0.027 | 0.006 | 19.340 | 1 | 0.000 | 1.027 |
| Decrease in verbal output | 1.510 | 0.655 | 5.318 | 1 | 0.021 | 4.528 |
| GCS 3-8 | -1.489 | 0.249 | 35.637 | 1 | 0.000 | 0.226 |
| GCS 9-14 | -1.002 | 0.195 | 26.351 | 1 | 0.000 | 0.367 |
| Hypertension | -0.726 | 0.210 | 11.890 | 1 | 0.001 | 0.484 |
| Diabetes | 0.567 | 0.292 | 3.767 | 1 | 0.052 | 1.763 |
| Constant | -0.113 | 0.411 | 0.076 | 1 | 0.783 | 0.893 |
In contrast, as shown in Table 3, the multivariate analyses of stroke profile showed that hemorrhagic stroke was associated with hypertension (OR = 2.223, 95%CI 1.438 to 3.437), history of chronic kidney disease (OR = 5.419, 95%CI 0.877 to 33.498) and decrease in sensorium, GCS 9-14 upon arrival at the hospital (OR = 2.474, 95%CI 1.698 to 3.604). The model found that hypertension and a decrease in sensorium were significantly associated with hemorrhagic stroke.
Table 3.
Multivariate logistic analysis of hemorrhagic stroke profile among the population
| B | S.E. | Wald | df | Sig. | Odds | |
|---|---|---|---|---|---|---|
| Age | -0.030 | 0.006 | 23.659 | 1 | 0.000 | 0.970 |
| Decrease in verbal output | -1.193 | 0.662 | 3.243 | 1 | 0.072 | 0.303 |
| GCS 9-14 | 0.906 | 0.192 | 22.232 | 1 | 0.000 | 2.474 |
| Hypertension | 0.799 | 0.222 | 12.913 | 1 | 0.000 | 2.223 |
| Kidney disease | 1.690 | 0.929 | 3.306 | 1 | 0.069 | 5.419 |
| Constant | 0.159 | 0.420 | 0.143 | 1 | 0.705 | 1.172 |
For subarachnoid hemorrhage, the multivariate analyses, as shown in Table 4, found that headache (OR = 2.223, 95%CI 1.438 to 3.437) and loss of consciousness (OR = 2.223, 95%CI 1.438 to 3.437) as primary complaints, and coming in stuporous or comatose, GCS 3-8 (OR = 2.223, 95%CI 1.438 to 3.437) were significantly associated with subarachnoid hemorrhage.
Table 4.
Multivariate logistic analysis of subarachnoid hemorrhage profile among the population
| B | S.E. | Wald | df | Sig. | Odds | |
|---|---|---|---|---|---|---|
| Loss of consciousness | 1.614 | 0.500 | 10.422 | 1 | 0.001 | 5.021 |
| Headache | 3.263 | 0.838 | 15.162 | 1 | 0.000 | 26.131 |
| Decreased sensorium | 1.206 | 0.518 | 5.421 | 1 | 0.020 | 3.340 |
| Comatose | 2.414 | 0.434 | 30.913 | 1 | 0.000 | 11.182 |
| Diabetes | -18.670 | 3866.107 | 0.000 | 1 | 0.996 | 0.000 |
| Previous stroke | -1.017 | 0.650 | 2.446 | 1 | 0.118 | 0.362 |
| Constant | -4.146 | 0.358 | 134.158 | 1 | 0.000 | 0.016 |
DISCUSSION
In this retrospective study, we have identified ischemic stroke (64.7%) as the most common stroke type in the cerebrovascular disease population in the two tertiary hospitals in Sorsogon. More than half of the recorded stroke cases were due to an occlusion of a cerebral blood vessel.
Ischemic stroke causes cerebral infarction. Hemorrhagic stroke type comprises 29.7% of cases, parallel to nationwide and global studies in Asian countries.2,11 This is also the case in the Philippines, wherein three out of 10 cases of diagnosed stroke are the hemorrhagic type of stroke.12 With a global advancement in healthcare, life expectancies have also increased.6 The local data available is a community-based survey that stated that the national prevalence of stroke is 486 per 100,000 of the population and 1,400 per 100,000 in those aged ≥40 years.13
The risk of stroke (of any type) significantly increases with age, consistent with those of other studies. The study showed that there was no statistically significant difference between sex. In this hospital-based study, we found that hyper-tension, a previous history of cerebrovascular disease, and diabetes mellitus were ranked as the top three cerebrovascular risk factors, with rates of 65%, 16.2%, and 11.4%, respectively. This was supported by 75.9% of stroke patients with elevated blood pressure levels. The age-adjusted national prevalence of hypertension is 20.6%, and 6% for diabetes.11 These are primarily modifiable risk factors, and the burden of stroke is attributable to the exponential effects of modifiable risk factors. In the modifiable risk factors observed, diabetes is more associated with the ischemic type of stroke.
In contrast, hypertension is significantly associated with hemorrhagic stroke, also observed in the RIFASAF study among Filipinos.7 They sustained high blood pressure damage to arteries, making them susceptible to rupture.14 Hence, hypertension poses significant public health importance.
With a mortality rate of 26.8 % seen in this hospitalbased study, the Philippines included the highest number of deaths and DALYs attributable to stroke.15 The thirty-day mortality rate of 15% is estimated for ischemic stroke in high-income countries, with age-sex standardized mortality of 109.6 in 100,000 person-years in the Philippines.15,16
This study observed that most of those eventually diagnosed with cerebrovascular diseases had chief complaints of hemiparesis, dysarthria, and changes in sensorium. These include a few of the symptoms advocated in the BEFAST Stroke mnemonic. This study's subpopulation of subarachnoid hemorrhage was statistically significant, wherein a history of headache or loss of consciousness with a very depressed sensorium upon arrival in the institutions. Both intracerebral and subarachnoid hemorrhage are associated with a decreased level of sensorium on admission. This means patients presented an abnormal state of attentiveness in which ordinary people function while not asleep. A further depression or reduced consciousness is noted in GCS of patients who eventually were documented to have a subarachnoid hemorrhage.
The country has a limited number of acute strokeready hospitals equipped with trained staff and appropriate facilities. Most of these are in highly urbanized areas. Across the Philippines, there is a low stroke awareness. Most patients seek medical consultation beyond the time window of the standard of care (i.e., intravenous thrombolysis or endovascular therapy) for stroke.12 Patients, upon evaluation, undergo diagnostic procedures and are given appropriate treatments to the extent they can shoulder out of pocket.
As far as we know, this was the most recent investigation of stroke profiles in a rural area. This filled the gap of limited data on the epidemiological studies of stroke in the Philippines. One foreign study pointed out that risk factors were more prevalent but less likely to be controlled in rural areas than in the urban population without prior stroke.17 The burdening reality that rural hospitals lack clinical expertise of specialists, access to advanced therapies for stroke, and the infrastructures for imaging modalities impacts a higher mortality and morbidity rate compared to urban areas.18
In a third-class province in the Philippines, ischemic stroke is the most common type. The risk of stroke increases with age. Risk factors for stroke occurrence are hypertension, history of stroke, and diabetes. Most sought consultation due to one-sided weakness and slurring of speech. Analysis showed that diabetes is more associated with ischemia while hypertension is significantly associated with hemorrhagic stroke. A mortality rate of 26.8% is seen in this cerebrovascular disease population. Up to this writing, no local data is available on stroke presentation and outcomes in the country's rural areas.
The current study did not consider the COVID-19 status of the patients. The quality of medical records documentation was limited due to the incompleteness of some parameters such as educational attainment, weight, height, social history/vices, blood sugar, lipid profile levels, and electrocardiogram tracings. Discharge modified Rankin scores for better documentation of post-stroke outcomes and complete COVID-19 work, which could have contributed more to the profile of the population under study. The first documented COVID-19-positive patient in the province of Sorsogon was June 30, 2020. A limitation was mainly due to screening for COVID-19 was not done in all stroke patients. At the onset, COVID-19 testing was prioritized for patients with respiratory symptoms. Improvement in history taking and medical record documentation is recommended. The observation on primary reasons for consult included some symptoms advocated in the BEFAST Stroke mnemonic calls for further emphasis on the other focal neurological symptoms such as imbalance and visual disturbances to watch out for a stroke. The described statistical correlation of history of headache and depressed sensorium with an eventual finding of subarachnoid hemorrhage may be used by primary care physicians in a rural area lacking neurologic specialty care and neuroimaging facilities to be alerted of this fatal disease entity.
Acknowledgments
The authors would like to acknowledge the Sorsogon Provincial Hospital, the Sorsogon Medical Mission Group Hospital Health Services Cooperative Administrative and the Medical Records personnel for their support.
Statement of Authorship
Both authors contributed in the conceptualization of work, acquisition and analysis of data, drafting and revising, and approved the final version submitted.
Author Disclosure
Both authors declared no conflicts of interest.
Funding Source
This study has no funding support.
REFERENCES
- 1.Katan M, Luft A. Global Burden of Stroke. Semin Neurol. 2018. Apr;38(2):208–11. [DOI] [PubMed] [Google Scholar]
- 2.Venketasubramanian N, Yoon BW, Pandian J, Navarro JC. Stroke Epidemiology in South, East, and South-East Asia: A Review. J Stroke. 2017. Sep;19(3):286–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khatib R, Jawaada AM, Arevalo YA, Hamed HK, Mohammed SH, Huffman MD. Implementing Evidence-Based Practices for Acute Stroke Care in Low- and Middle-Income Countries. Curr Atheroscler Rep. 2017. Nov 8;19(12):61. [DOI] [PubMed] [Google Scholar]
- 4.Causes of Deaths in the Philippines (Preliminary): January to June 2021 [Internet]. 2021. [cited 2022 Feb]. Available from: https://www.psa.gov.ph
- 5.Primary Health Care for Noncommunicable Diseases in the Philippines [Discussion paper]. 2020. [cited 2022 Feb]. Available from: https://www.pids.gov.ph/publications/7166
- 6.Bertram MY, Sweeny K, Lauer JA, Chisholm D, Sheehan P, Rasmussen B, et al. Investing in Non-communicable Diseases: An Estimation of the Return on Investment for Prevention and Treatment Services. Lancet. 2018. May 19;391(10134):2071–8. [DOI] [PubMed] [Google Scholar]
- 7.Roxas, A. The RIFASAF project: A Case-control Study on Risk Factors for Stroke among Filipinos. Phil J Neurol. 2002; 6: 1–7. [Google Scholar]
- 8.Navarro JC, Venketasubramanian N. Stroke Burden, and Services in the Philippines. Cerebrovasc Dis Extra. 2021. May 11;11(2):52–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cities and Municipalities Competitive Index [Internet]. 2021. [cited 2022 Feb]. Available from https://cmci.dti.gov.ph/prov-profile.php?prov=Sorsogon
- 10.Sorsogon [Internet]. 2020. [cited 202 Feb]. Available from: https://www.philatlas.com/luzon/r05/sorsogon.html
- 11.Navarro JC, Baroque AC 2nd, Lokin JK, Venketasubramanian N. The Real Stroke Burden in the Philippines. Int J Stroke. 2014. Jul;9(5):640–1. [DOI] [PubMed] [Google Scholar]
- 12.Collantes MV, Zuniga YH, Granada CN, Uezono DR, De Castillo LC, et al. Current State of Stroke Care in the Philippines. Front Neurol. 2021. Aug 17;12:665086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Navarro, JC. Prevalence of stroke: A Community Survey. Phil J Neurol. 2005; 9:11–5. [Google Scholar]
- 14.Feldmann E, Broderick JP, Kernan WN, Viscoli CM, Brass LM, et al. Major Risk Factors for Intracerebral Hemorrhage in the Young are Modifiable. Stroke. 2005. Sep; 36 (9): 1881–5. [DOI] [PubMed] [Google Scholar]
- 15.Apor ADAO, Pagaling GT, Espiritu AI, Jamora RDG. Stroke Research Disparity in Southeast Asia: Socioeconomic Factors, Healthcare Delivery, and Stroke Disease Burden. J Stroke Cerebrovasc Dis. 2021. Feb;30(2):105481. [DOI] [PubMed] [Google Scholar]
- 16.Ganesh A, Lindsay P, Fang J, Kapral MK, Côté R, Joiner I, et al. Integrated Systems of Stroke Care and Reduction in 30-day Mortality: A Retrospective Analysis. Neurology. 2016. Mar 8;86(10): 898–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kapral MK, Austin PC, Jeyakumar G, Hall R, Chu A, et al. Rural-Urban Differences in Stroke Risk Factors, Incidence, and Mortality in People With and Without Prior Stroke. Circ Cardiovasc Qual Outcomes. 2019. Fe; 12(2); e004973. [DOI] [PubMed] [Google Scholar]
- 18.Hammond G, Luke AA, Elson L, Towfighi A, Joynt Maddox KE. Urban-Rural Inequities in Acute Stroke and In-Hospital Mortality. Stroke. 2020. Jul; 51 (7): 2131–8. [DOI] [PubMed] [Google Scholar]


