Abstract
Isthmocele, also known as uterine niche, refers to a myometrial defect of the anterior wall of the uterine isthmus, specifically at the site of the previous C-section scar. The prevalence of isthmocele has increased in tandem with the rise in deliveries by caesarean section. Risk factors include aspects related to the surgical procedure. The present study aimed to assess the relationship between various suture types and the development of a niche. The analysis of the present study is based on data collected from the evaluation of 52 patients, 6 weeks post C-section performed in ‘Saint Pantelimon’ Hospital in Bucharest, Romania. The parameters examined included patient age, the number of previous births by C-section, the type of suture used and uterine anatomy. Out of all the 52 patients, 42.3% developed an isthmocele. The results confirm a significant association between the presence of the niche and the type of suture of the first layer, proving that when non-locking continuous suture was used, the absence of niche was observed in most cases, while using the locking continuous suture was associated with more niches. Using the continuous locking suture for the first layer was associated with severe niches, while no severe niches were observed in patients with the other two types of sutures. There is a statistically significant association between the use of continuous locking sutures for uterine closure in the first layer and the development of a uterine niche. Furthermore, all instances of severe niches were linked to this type of suture, compared with continuous non-locking suture or interrupted suture. Given the escalating rate of C-sections, further research is crucial to identify the suture type that minimizes the risk of isthmocele formation. The present study's limitations revolve around its exclusive focus on a single institution and the relatively small sample size.
Keywords: C-section scar, hysterorrhaphy, isthmocele, locking suture, niche, uterine scar defect
Introduction
Isthmocele, also referred to as a scar niche from a caesarean section, is characterized by an indentation exceeding 2 mm, representing myometrial discontinuity at the site of the previous C-section scar, in the anterior wall of the lower uterine segment (1).
Based on the most recent statistics regarding C section rates in the world, Romania is the 3rd leading country, with a rate of 443.2 caesarian sections per 1,000 live births (2). Official data from 2010 indicate a rate of 338.2 C-sections per 1,000 live births, indicating an increase of 31.05% (2). The prevalence of isthmocele has increased in tandem with the rise in deliveries by caesarean section.
Considering the implications of having an isthmocele and the rising number of births by C-section, a great number of individuals are exhibiting long-term effects (3). This has underscored the significance of diagnosing isthmoceles, which has become more accessible and essential than in the past (3). Knowledge about what to look for has streamlined the diagnostic process (3). The diagnosis can be made by transvaginal ultrasound, MRI or hysterosalpingography, by observing the extension of the contrast substance at the site of the defect (1). The estimated prevalence of isthmocele is as high as 70%, with ~30% of the patients experiencing symptoms (4).
Risk factors associated with the development of a niche are lower uterine incision, the presence of cervical dilation >5 cm, C-section after labor with a duration of more than 5 h (5,6). Furthermore, several factors related to surgical technique have been investigated, such as the number of myometrial layers used for the uterine closure (7), the use of locking sutures, non-locking sutures or interrupted sutures, the anatomical approximation of the myometrial margins with the suture of the whole layer, including the decidua (5,8-10). Additionally, certain risk factors have been identified that increase the likelihood of isthmocele development, including the position of the uterus, high number of C-sections in the past and high BMI (5).
The prevalent gynecological complications associated with the presence of an isthmocele are pelvic adhesions, chronic pelvic pain, menometrorrhagia and subfertility or even infertility (3,11). Additionally, secondary amenorrhea has been documented in medical literature (6).
Regarding secondary infertility, it is considered to stem from diminished mucus quality during the follicular phase, impacting sperm mobility and implantation (12). Additionally, fertility challenges are attributed in part to an inflammatory response, resembling the impact of chronic inflammation and oxidative stress observed in conditions such as endometriosis (5,13).
Menometrorrhagia is likely a result of blood accumulation at the site of the defect, leading to persistent spotting (12). The lymphocytic infiltration, anatomical distortion and abnormal continuous contraction of the myometrium with the purpose of emptying the niche, are part of the etiopathogenesis of the chronic pelvic pain (12).
In addition to the aforementioned gynecological complications, the presence of an isthmocele during subsequent pregnancies can be associated with various issues, including ectopic pregnancy with implantation in the uterine scar, placenta previa potentially accompanied by spectrum accreta, or uterine rupture (3,11).
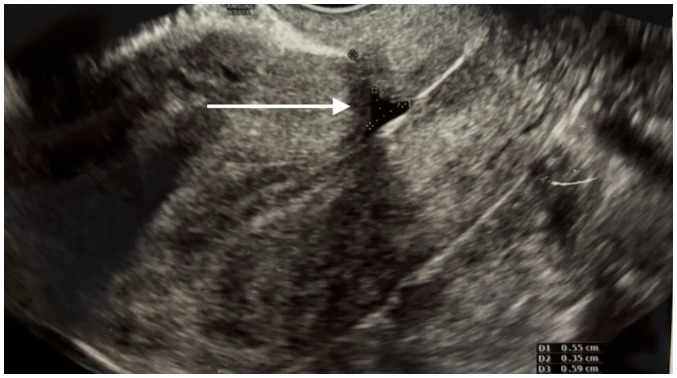
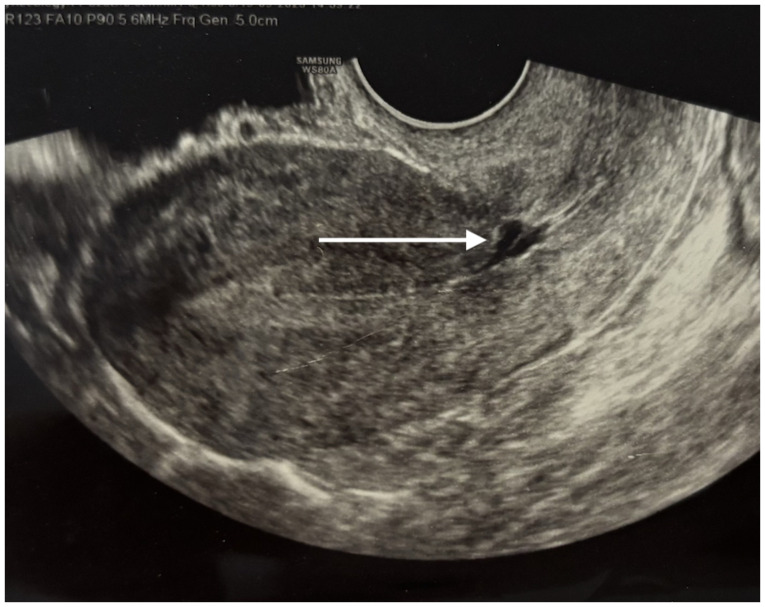
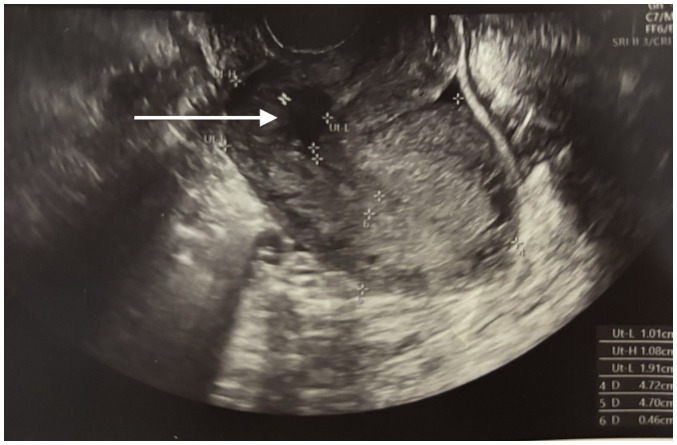
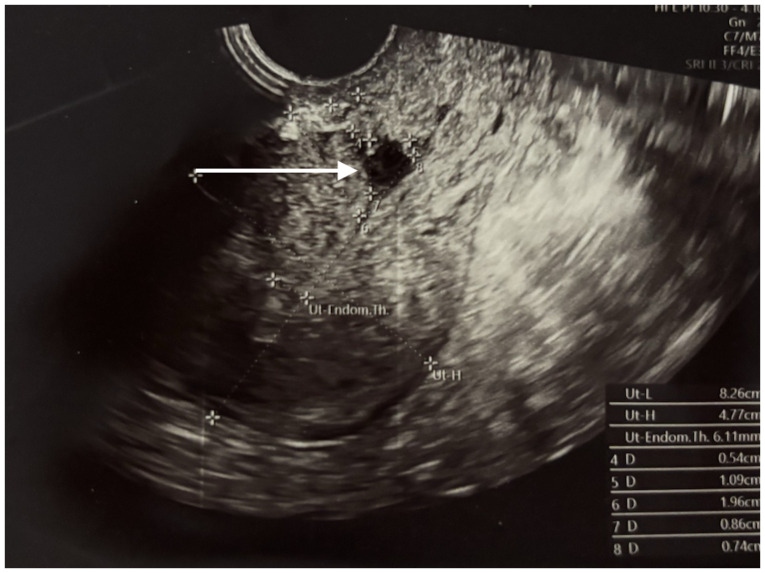
Considering the diverse aspects of isthmocele, there are a few classification systems that could be used, although none of them are standardized (4,12). One possible classification is based on ultrasound measurements, grading the niche by the ratio between its depth and the residual myometrium thickness, with a ratio >50% indicating a severe niche (12). Additionally, the isthmocele can be classified by its shape-triangular (as observed in Figs. 1 and 2), semicircular (as observed in Figs. 3 and 4), rectangular, droplet or inclusion cysts, with the first two being the most common (4,14).
Figure 1.
Triangular niche.
Figure 2.
Triangular niche.
Figure 3.
Semicircular niche.
Figure 4.
Semicircular niche.
The decision to treat an isthmocele is based on a few factors, including the size of the niche, the severity of the symptoms, the presence of secondary infertility and whether the patient wishes to obtain a pregnancy (12). Routine treatment is not recommended for patients incidentally diagnosed with an asymptomatic niche, who do not wish to conceive (4).
The surgical treatment can be performed by hysteroscopy, transabdominally (laparotomy, laparoscopy or robot-assisted), vaginally or a combination of hysteroscopy and laparoscopy (4,15). Hysterectomy stands as a definitive treatment for gynecological symptoms caused by the presence of the isthmocele (4).
Materials and methods
The present study constitutes a prospective analysis involving 52 women who were assessed 6 weeks postpartum after delivery via caesarian section at the Saint Pantelimon Emergency Clinical Hospital (Bucharest, Romania). The data collection period spanned from April 1, 2022 to April 1, 2023. The primary evaluation methods in the present study involved transvaginal ultrasound examinations and comprehensive anamnestic assessments. All patients signed written informed consent for the use of their data and associated images in research upon admission to the Obstetrics and Gynecology department (Bucharest, Romania).
The hypothesis of the present study posited that certain types of hysterorraphy associate more frequently with the development of the niche. With their purpose to confirm the hypothesis, these specific objectives were formulated: (i) The identification of anamnestic characteristics and uterine anatomy, through detailed anamnesis and transvaginal ultrasound; (ii) the evaluation of the niche and its ultrasound associated characteristics, such as depth, total myometrial thickness, residual myometrial thickness, severity degree (depth/total myometrial thickness ratio); (iii) the evaluation of the shape of the niche; (iv) the selection of patients with severe niches (ratio>50%); and (v) the evaluation of hysterorraphy type based on number of layers, type of suture (continuous locking, continuous non-locking or interrupted), the thickness of the thread and presence or absence of peritonization.
The inclusion criteria for patient selection were as follows: Individuals aged 18 years or older, patients who had undergone a caesarean section at ‘Saint Pantelimon’ Hospital (Bucharest, Romania) within the specified timeframe, patients who attended the 6-week postpartum medical examination, and patients who provided informed consent to participate in the present study.
The exclusion criteria encompassed individuals younger than 18 years old, those who had a vaginal birth, patients who had a C-section at a different hospital, patients for whom surgical technique information was unavailable, and patients who refused to participate in the present study.
To construct the database, a complementary document was utilized to record all pertinent information. In addition to this documentation, the physician had access to the patient's medical records, the birth registry and the C-section registry. The elements of descriptive statistics included the following: (i) Quantitative variables-age (in years completed), number of previous births by C-sections and the presence of labor prior to surgery; (ii) Qualitative dichotomous variables-presence of niche-yes/no; presence of peritonization-yes/no; presence of homogenous myometrium- yes/no; and (iii) qualitative nominal variables-anatomy (position of the uterus and size), depth of niche, the thickness of the residual myometrium, total thickness of the myometrium, ratio depth/myometrial total thickness, niche shape, number of layers during uterine closure, type of suture of the first layer +/- type of suture of the second layer.
After collecting the data, all information was integrated in Excel, for the statistical analysis using SPSS Statistics for Windows, version 29.0 (IBM Corp.). Continuous variables were expressed using mean value, median, standard deviation, minimum and maximum, while the categorial variables were presented as absolute frequency and percentage. The association between categorical variables was analyzed using the cross-tabulation table and the chi-square test. In cases where the chi-square test results were significantly altered, the Fisher's exact test was used. For comparing the means based on dichotomous variables in the study, the independent samples t-test was used. To compare three or more means of groups, the ANOVA test was used, followed by a Bonferroni post hoc test. P<0,05 was considered to indicate a statistically significant difference.
Results
The initial segment of the results focused on descriptive analysis. The first variable examined was the age of the patients. The mean age was 30,42 years, with values ranging from 20 to 46 years old. This seemingly higher mean age in the present study could be attributed to the tendency of younger patients to bypass prenatal and postpartum check-ups more frequently, compared with those who are older, resulting in a skewed average age.
Based on the presence of previous births by C-section, 26.9% of patients had only one previous caesarean section. Also, only 9.6% of the patients were in labor prior to the C-section.
In terms of uterine anatomy and position, the present study examined the positioning of the uterus. In two thirds of cases, the uterus was found to be in anteversion, while 19.2% of the patients had a retroverted uterus and 13.5% of them had the uterus in an intermediate position.
Out of the 52 patients included in the present study, 22 patients were observed to have an isthmocele, resulting in a prevalence of 42.3%. The results indicated that the mean depth of the niches was 0.55 cm and the maximum depth found in the present study was 1.01 cm. The distribution of patients included in the present study according to the depths of the niches is demonstrated in Fig. 5. These data are presented in Table SI, as supplementary data.
Figure 5.
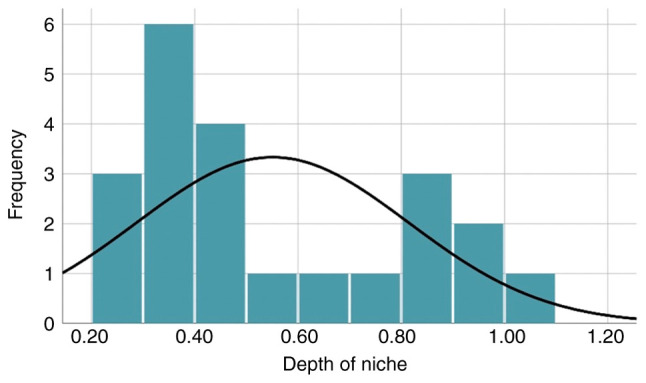
Distribution of patients based on depth of niche.
The thickness of the residual myometrium revealed a mean of 0.84 cm, with a median of 0.86 cm. When analyzing the patients with respect to the overall thickness of the myometrium, the mean was calculated to be 1.46 cm.
The mean ratio depth/total thickness of the myometrium was 37.6%, with a minimum ratio of 16% and a maximum ratio of 66%. The distribution of the patients according to the depth/total thickness ratios is presented in Fig. 6, while supplementary data is presented in Table SII. A ratio exceeding 50% indicates that the niche can be classified as severe.
Figure 6.
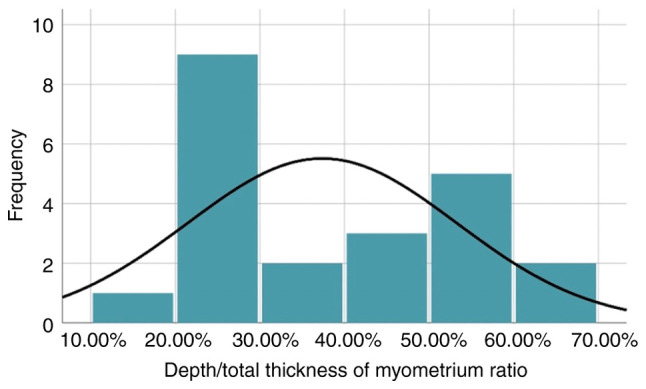
Distribution based on depth of niche/total thickness of myometrium ratio.
Based on the identified shapes of niches in the present study, 45.5% are triangular, 36.4% are semicircular while the rest are inclusion cysts and droplet type.
In the analysis of the types of sutures used during uterine closure, it was determined that 48.1% of patients received a single layered suture, while 51.9% of patients had a double layered suture.
During the hysterorraphy, the first layer involved a continuous locking suture in 48.1% of patients, while continuous non-locking suture and interrupted sutures were used in the remaining cases.
In the final segment of the descriptive analysis, the present study examined the number of patients in whom the visceral peritoneum was closed during surgery. It was observed that this was the case for 61.5% of the patients.
The association between the type of suture and the presence of a niche
Analyzing Table I, it can be noted that single layered closure of the uterus was observed in 40% of cases with no isthmocele and 59.1% of cases with isthmocele. For testing the relationship between the presence of niche and the number of layers, chi-square test was used. Bivariate chi-square test revealed no significant association (χ2=1.853; df=1, P=0.173).
Table I.
Association between number of layers and the presence of niche.
| Number of layers | |||||
|---|---|---|---|---|---|
| 1 | 2 | Total | |||
| Niche yes/no | No | Frequency | 12 | 18 | 30 |
| % | 40.0% | 60.0% | 100.0% | ||
| Yes | Frequency | 13 | 9 | 22 | |
| % | 59.1% | 40.9% | 100.0% | ||
| Total | Frequency | 25 | 27 | 52 | |
| % | 48.1% | 51.9% | 100.0% | ||
| Chi-square test | |||||
| Value | df | P-value | |||
| Pearson Chi-Square | 1.853 | 1 | 0.173 | ||
| Cramer's V | 0.189 | 0.173 | |||
| Number of cases | 52 | ||||
The results of Fisher's exact test confirm a significant association between the presence of the niche and the type of suture of the first layer (P=0.00560733). Based on the findings presented in Table II, when non-locking continuous suture was used, the absence of niche was observed in most cases (60% of cases), while using the locking continuous suture was associated with niches (63.6%).
Table II.
Association between the first layer type of suture and isthmocele.
| First layer | ||||||
|---|---|---|---|---|---|---|
| Continuous locking | Continuous non-locking | Interrupted sutures | Total | |||
| Niche yes/no | No | Frequency | 11 | 18 | 1 | 30 |
| % | 36.7% | 60.0% | 3.3% | 100.0% | ||
| Yes | Frequency | 14 | 4 | 4 | 22 | |
| % | 63.6% | 18.2% | 18.2% | 100.0% | ||
| Total | Frequency | 25 | 22 | 5 | 52 | |
| % | 48.1% | 42.3% | 9.6% | 100.0% | ||
| Exact probability | ||||||
| Fisher's exact test | 0.00560733 | |||||
The association between the number of layers and the thickness of the residual myometrium in patients with isthmocele
The mean thickness of the residual myometrium was 0.86 cm when hysterorrhaphy was performed in a single layer, while the mean thickness observed in patients with double-layered closure was 0.8211 cm. Because the results of the t test had a P=0.753, as demonstrated in Table SIII, it was concluded that the relationship between the two variables was not significant.
The association between the number of layers and the total thickness of the myometrium in patients with isthmocele
The total thickness of both types of sutures was also compared, with a t-test result that revealed no statistically significant difference [t(20)=-0.233; P=0.818]. These results are presented in Table SIV.
The association between the type of suture and the thickness of the residual myometrium in patients with niche
For finding out whether there is a significant association between the type of suture and the residual myometrial thickness, one-way ANOVA analysis was used.
The thickness of the residual myometrium was not significantly different (P=0.475) based on the type of suture, even though results in Table III revealed that when non-locking continuous suture was used, the mean thickness of the residual myometrium was 1.00 cm, while in other cases the residual myometrial thickness was 0.8. Even though these results were observed and analyzed in Table III, the difference is not statistically significant.
Table III.
Relationship between the type of suture and the thickness of the residual myometrium.
| N | Mean | Standard deviation | Minimum | Maximum | |
|---|---|---|---|---|---|
| Cont. locking | 14 | 0.8029 | 0.25644 | 0.40 | 1.30 |
| Cont. non-locking | 4 | 1.0025 | 0.41291 | 0.65 | 1.60 |
| Interrupted suture | 4 | 0.8325 | 0.23472 | 0.49 | 1.02 |
| Total | 22 | 0.8445 | 0.28084 | 0.40 | 1.60 |
| ANOVA | |||||
| Thickness of residual myometrium | |||||
| df | F | P-value | |||
| Between groups | 2 | 0.774 | 0.475 | ||
The association between the type of suture and the total thickness of the myometrium in patients with niche
The total thickness of the myometrium in patients with niche is not statistically significant different based on the type of suture used (P=0.607), with Table IV illustrating these results.
Table IV.
Relationship between the type of suture and total thickness of the myometrium in patients with niche.
| N | Mean | Standard deviation | Minimum | Maximum | |
|---|---|---|---|---|---|
| Cont. locking | 14 | 1.4693 | 0.33790 | 0.86 | 1.89 |
| Cont. non-locking | 4 | 1.5675 | 0.39911 | 1.21 | 2.10 |
| Interrupted suture | 4 | 1.3350 | 0.15264 | 1.20 | 1.54 |
| Total | 22 | 1.4627 | 0.31936 | 0.86 | 2.10 |
| ANOVA | |||||
| Total thickness of myometrium | |||||
| df | F | P-value | |||
| Between groups | 2 | 0.513 | 0.607 | ||
The association between the shape of the niche and the number of layers used in patients with isthmocele
For testing the relationship between the shape of the niche and the number of layers used, Fisher's exact test was used. Judging by the results that are illustrated in Fig. 7 and Table SV, there was no significant association between the two variables (P=0.63800905).
Figure 7.
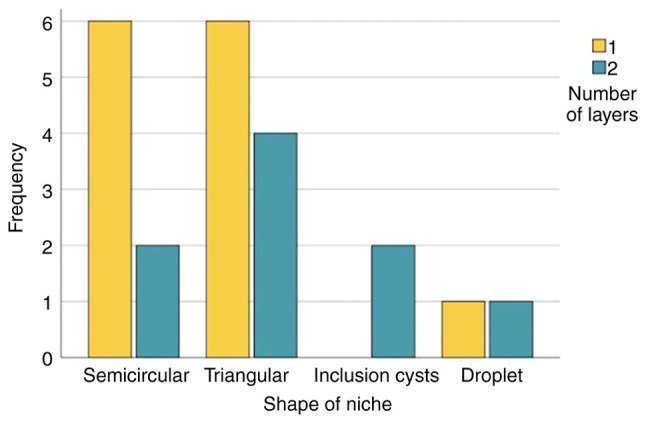
Association between shape of niche and number of layers.
The results regarding the inclusion cysts and droplet type were ignored, because their number was extremely low.
The association between the shape of niche and type of suture
The result of Fisher's exact test revealed that there was not statistically significant association (P=0.67420814) between the shape of niche and the type of suture. No matter the shape of the niche, in most cases continuous locking suture was used for the first layer. The association between the shape of niche and type of suture are demonstrated in Fig. 8 and Table V. The results regarding inclusion cysts and droplet were ignored as they were in an extremely small number.
Figure 8.
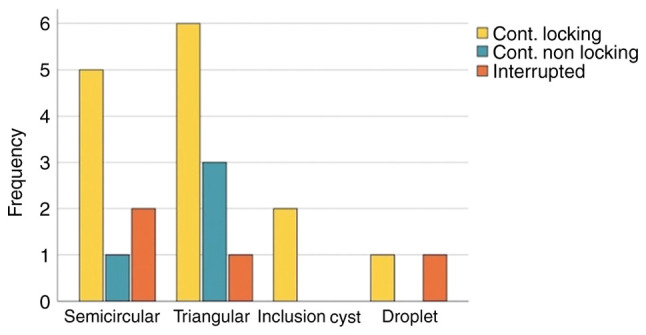
Association between shape of niche and type of suture.
Table V.
Association between the shape of niche and type of suture.
| First layer | ||||||
|---|---|---|---|---|---|---|
| Cont. locking | Cont. non-locking | Interrupted | Total | |||
| Shape | Semicircular | Frequency | 5 | 1 | 2 | 8 |
| % | 62.5% | 12.5% | 25.0% | 100.0% | ||
| Triangular | Frequency | 6 | 3 | 1 | 10 | |
| % | 60.0% | 30.0% | 10.0% | 100.0% | ||
| Inclusion cyst | Frequency | 2 | 0 | 0 | 2 | |
| % | 100.0% | 0.0% | 0.0% | 100.0% | ||
| Droplet | Frequency | 1 | 0 | 1 | 2 | |
| % | 50.0% | 0.0% | 50.0% | 100.0% | ||
| Total | Frequency | 14 | 4 | 4 | 22 | |
| % | 63.6% | 18.2% | 18.2% | 100.0% | ||
| Exact probability | ||||||
| Fisher's exact test | 0.67420814 | |||||
The association between the number of layers and severity of niche
Among all patients with a niche, 68.2% had a depth of niche/total myometrial thickness <50% (non-severe niche), while 31.8% of them had a ratio >50% (severe niche). These results are displayed in Table SVI.
With the use of single-layered uterine closure, the percentage of severe niches was 30.8%, while with the use of double-layered closure, the percentage was 33.3%. Based on the findings presented in Table VI, the difference is not statistically significant (P=0.9638).
Table VI.
Association between number of layers and severity of niche.
| Depth/total thickness ratio | |||||
|---|---|---|---|---|---|
| <50% | >50% | Total | |||
| Number of layers | 1 | Frequency | 9 | 4 | 13 |
| % | 69.2% | 30.8% | 100.0% | ||
| 2 | Frequency | 6 | 3 | 9 | |
| % | 66.7% | 33.3% | 100.0% | ||
| Total | Frequency | 15 | 7 | 22 | |
| % | 68.2% | 31.8% | 100.0% | ||
| Exact probability | |||||
| Fisher's exact test | 0.9638 | ||||
The association between the type of suture used for the first layer and the severity of niche
With the use of continuous locking suture for the first layer, the percentage of severe niches was 50%, while the other two types of suture (continuous non-locking or interrupted suture), there were no cases of severe niche (with a ratio >50%). In Table VII, the association between the type of suture of the first layer and the severity of niche can be observed.
Table VII.
Association between the type of suture of first layer and the severity of niche.
| Depth/total myometrial thickness ratio | |||||
|---|---|---|---|---|---|
| <50% | >50% | Total | |||
| First layer | Cont. locking | Frequency | 7 | 7 | 14 |
| % | 50.0% | 50.0% | 100.0% | ||
| Cont. non-locking | Frequency | 4 | 0 | 4 | |
| % | 100.0% | 0.0% | 100.0% | ||
| Interrupted suture | Frequency | 4 | 0 | 4 | |
| % | 100.0% | 0.0% | 100.0% | ||
| Total | Frequency | 15 | 7 | 22 | |
| % | 68.2% | 31.8% | 100.0% | ||
| Exact probability | |||||
| Fisher's exact test | 0.05661882 | ||||
Despite P=0.05661882, it is plausible to consider a statistically significant difference between the continuous locking suture and the other two types, regarding the risk of developing a severe niche. It's crucial to note that the relatively small sample size might account for this value. With larger groups and increased statistical power, a more pronounced association would likely become evident.
The association between niche and closure of the visceral peritoneum
In the cases presenting with niche, peritonization was performed in 63.6% of cases, while in the cases without niche, peritonization was observed in 60% of patients, as observed in Table SVII. Considering this, the difference between the two groups is not statistically significant (P=0.790).
Furthermore, a comparison was made between the depth of the isthmocele in patients without peritonization and those with peritonization. Based on the results included in Table SVIII, where similar means were observed, no significant difference was identified between the two groups.
The association between the niche presence and position of uterus
The analyzed data displayed in Table VIII revealed no statistically significant association between the presence of the niche and position of uterus (P=0.43952477). This association is visually represented in Fig. 9.
Table VIII.
Association between niche and position of uterus.
| Niche yes/no | |||||
|---|---|---|---|---|---|
| No | Yes | Total | |||
| Position of uterus | Retroverted | Frequency | 4 | 6 | 10 |
| % | 40.0% | 60.0% | 100.0% | ||
| Intermediate | Frequency | 4 | 3 | 7 | |
| % | 57.1% | 42.9% | 100.0% | ||
| Anteverted | Frequency | 22 | 13 | 35 | |
| % | 62.9% | 37.1% | 100.0% | ||
| Total | Frequency | 30 | 22 | 52 | |
| % | 57.7% | 42.3% | 100.0% | ||
| Exact probability | |||||
| Fisher's exact test | 0.43952477 | ||||
Figure 9.
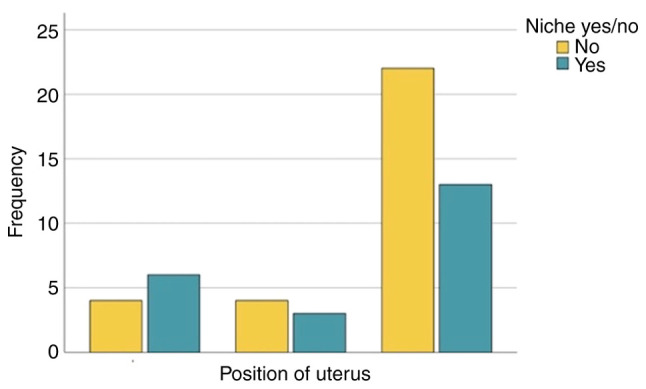
Association between niche and position of uterus.
The association between the presence of previous C-sections and niche development
The percentage of niche appearance in patients with previous C-sections, revealing an elevated incidence of niche in this group, is demonstrated in Fig. 10.
Figure 10.
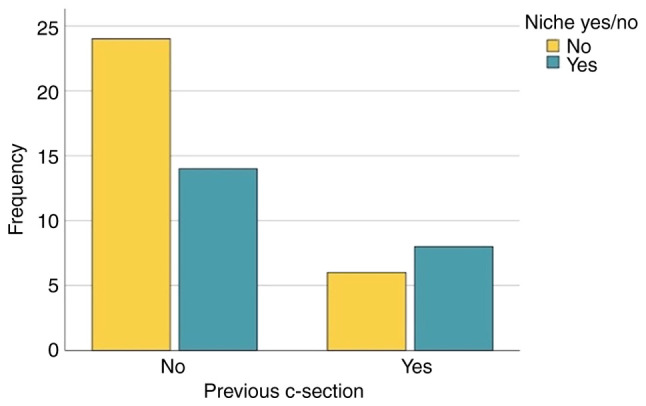
Association between previous C-section and niche.
The association between a homogenous myometrium and the presence of niche
Although it was observed that in the presence of fibromatosis or adenomyosis, the niche was developed in 71.4% of cases, while the percentage of niche was 37.8% in patients without fibroids or adenomyosis, the result of the statistical analysis observed in Table SIX (P=0.11884797) revealed no statistically significant association.
Discussion
Based on the results presented in the descriptive and statistical analysis, a comprehensive discussion can be initiated. Interestingly, in contrast to the lower mean age of patients who underwent C-section at Saint Pantelimon Emergency Clinical Hospital (Bucharest, Romania) during the specified period, which typically tends to be younger, the present study reported a mean age of 30.42 years. This deviation could be attributed to the fact that a portion of the patients who gave birth via C-section were younger women who tended to avoid prenatal care. Consequently, the mean age in the present study might have been influenced by the absence of adequate prenatal and postpartum medical visits of these patients.
Based on the position of the uterus, 67.3% of the patients had an anteverted uterus, the others presenting with retroverted uterus or in intermediate position. Despite previous studies suggesting a retroverted uterus a risk factor for isthmocele development, the present statistical analysis did not establish a significant association in the present study. However, upon reviewing the database, it was evident that the most severe niches were observed in patients with a retroverted uterus or in intermediate position, as indicated by their depth to total myometrial thickness ratios (66 and 63%, respectively).
The ultrasound appearance of the niche was observed in 22 patients out of the 52 participants in the present study, resulting in a prevalence of 42.3%. It's worth noting that international studies have reported a broader range of prevalence, reaching up to 70%. This variance in prevalence underscores the importance of considering regional and population-specific factors that might contribute to these differences in isthmocele occurrence.
The shapes of the niches exhibited variability, including triangular, semicircular, inclusion cysts and droplet shapes. Among these, triangular and semicircular shapes were the most prevalent, accounting for 45.5 and 36.4% respectively. Interestingly, the present study found that associations between the shape of the niche and factors such as the number of layers or the type of suture used did not demonstrate any statistically significant relationships.
Although previous studies had extensively explored and dismissed a connection, the present study deliberately examined the relationship between the number of layers in uterine closure and the presence of an isthmocele. Following statistical analysis, it was determined that there were no discernible differences in niche development between single-layered and double-layered uterine closures. Moreover, the present study delved in the relationship between the number of layers and both the total myometrial thickness and residual myometrial thickness in patients with an isthmocele. However, the results indicated to statistically significant differences in this regard.
The present study explored the association between the type of suture used and both the total myometrial thickness and the residual myometrial thickness. Notably, when utilizing a continuous non-locking suture, the mean thickness of the residual myometrium was found to be 1 cm, whereas in other types of suture, the mean thickness was 0.8 cm. However, despite these variations, the results did not demonstrate statistical significance.
In the present study, a statistically significant association was identified between the type of suture used for the first layer and the presence of an isthmocele (P=0.006). Notably, the continuous non-locking suture was predominantly utilized when the isthmocele was absent, whereas the continuous locking suture was more prevalent in cases where the isthmocele was present. This observed effect could likely be attributed to hypoxia induced by the ischemia-inducing suture and subsequent vicious scarring.
In the analysis of the present study, among all cases with an isthmocele, 31.8% had a depth-to-total myometrial thickness ratio exceeding 50%, which is the criterion for categorizing the niche as severe. The potential association between the severity of the niche and the number of layers was examined, however this did not yield significant results. However, the link between the type of suture used for the first layer and the severity of the niche was further investigated, and the results indicated a significant difference. Specifically, there was a notable distinction in the development of a severe niche when comparing uterine closure with a continuous locking suture vs. the other two types of sutures.
The potential association between the development of an isthmocele and the presence of fibroids or adenomyosis in patients was investigated. Interestingly, 71% of patients with fibroids or adenomyosis developed an isthmocele, whereas among those without this pathology, only 37.8% presented with a niche. However, despite the observed differences, the association between the presence of fibroids or adenomyosis and the development of an isthmocele did not reach a statistical significance.
In the present study, the potential association between the closure of the visceral peritoneum and the development of an isthmocele was explored. Historically, it was considered that the lack of peritoneal closure could be a risk factor for isthmocele development due to potential adhesion formation. There was no association found between peritonization and the presence of niche, nor any difference was observed between the depths of niches in patients with closure of the peritoneum vs. those without it.
The present study's limitations revolve around its exclusive focus on a single institution and the relatively small sample size. The second limitation was primarily driven by the challenge of recruiting research participants, which stemmed from difficulties related to accessing postnatal care due to refusal by some patients. In addition, another limit of the present study was the fact that potentially confounding variables, such as uterine position, body mass index and surgical technique were not controlled. There is a statistically significant association between the suture of the first uterine layer with continuous locking suture and the presence of the niche, which could be attributed to ischemia. Furthermore, there is also significant association between the closure of the first layer with continuous locking suture and the development of a severe niche. Further research and analysis may be needed to delve deeper into this aspect and its potential impact on isthmocele formation.
The present study did not find any significant differences in the rate of isthmocele development based on the number of layers used during uterine closure. Whether a single-layer or double-layer closure was performed did not appear to influence the likelihood of isthmocele development in the present study. Moreover, no significant associations were found between the number of layers used for hysterorraphy and the severity of the isthmocele.
Although the most severe niches in the present study were observed in patients with retroverted uterus or in intermediate position, the statistical analysis of the present study did not reveal a significant association between the niche development and the position of uterus, which is recognized as a significant factor in isthmocele development. It is important to acknowledge that the limited sample size may have contributed to the inability to establish a statistically significant association.
The present study noted that there were no significant associations found between the shape of the isthmocele and either the number of layers used, or the type of suture used for the first layer of uterine closure. There is no statistically significant association between the development of niche and absence of visceral peritoneal closure, as well as there are no differences in the depths of patients with niches based on the presence or absence of peritonization. Additionally, the presence of fibroids or adenomyosis was not found to be associated with an increased risk of developing an isthmocele.
These findings emphasize the potential impact of suture technique on isthmocele formation and severity, highlighting the importance of further research in this area.
Supplementary Material
Acknowledgements
Not applicable.
Funding Statement
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be requested from the corresponding author.
Authors' contributions
GZ collected the data, analyzed and interpreted the results, and prepared the draft of the manuscript. BN collected the data and prepared the draft of the manuscript. IP analyzed and interpreted the results, and prepared the draft of the manuscript. AN analyzed and interpreted the results, wrote, reviewed and edited the manuscript. CAI designed the research, wrote, reviewed and edited the manuscript, and supervised the present study. All authors have critically reviewed, read and approved the final version of the manuscript and are responsible for the content and similarity index of the manuscript. GZ and BN confirm the authenticity of all the raw data.
Ethics approval and consent to participate
The present study was approved (approval no. 21/20.03.2022) by the Ethics committee of the Saint Pantelimon Emergency Clinical Hospital (Bucharest, Romania).
Patient consent for publication
Informed oral consent was obtained from all patients. All patients signed written informed consent for the use of their data and associated images in research upon admission to the Obstetrics and Gynecology department of the Saint Pantelimon Emergency Clinical Hospital (Bucharest, Romania).
Competing interests
The authors declare that they have no competing interests.
Use of artificial intelligence tools
During the preparation of this work, artificial intelligence tools were used to improve the readability and language of the manuscript or to generate images, and subsequently, the authors revised and edited the content produced by the artificial intelligence tools as necessary, taking full responsibility for the ultimate content of the present manuscript.
References
- 1.Rupa R, Kushvaha S, Venkatesh K. Uterine isthmocele-a frequently overlooked complication of cesarean sections. Indian J Radiol Imaging. 2021;31:601–604. doi: 10.1055/s-0041-1736393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. C-Section Rates by Country 2024. https://worldpopulationreview.com/country-rankings/c-section-rates-by-country. [Google Scholar]
- 3.Nguyen AD, Duong GTT, Do DT, Nguyen DT, Tran DA, Phan TTH, Nguyen TK, Nguyen HTT. Primary cesarean section rate among full-term pregnant women with non-previous uterine scar in a hospital of Vietnam. Heliyon. 2022;8(e12222) doi: 10.1016/j.heliyon.2022.e12222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kulshrestha V, Agarwal N, Kachhawa G. Post-caesarean niche (isthmocele) in uterine scar: An update. J Obstet Gynecol India. 2020;70:440–446. doi: 10.1007/s13224-020-01370-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iannone P, Nencini G, Bonaccorsi G, Martinello R, Pontrelli G, Scioscia M, Nappi L, Greco P, Scutiero G. Isthmocele: From risk factors to management. Rev Bras Ginecol Obstet. 2019;41:044–052. doi: 10.1055/s-0038-1676109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Ghotani B, Martini N, Alabdallah E, Alawad I, Hussien K. A large post-caesarean Niche (Isthmocele) with amenorrhea, a symptom that was not reported in the medical literature: A rare case report. Int J Surg Case Rep. 2023;109(108528) doi: 10.1016/j.ijscr.2023.108528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Di Spiezio Sardo A, Saccone G, McCurdy R, Bujold E, Bifulco G, Berghella V. Risk of cesarean scar defect following single- vs double-layer uterine closure: Systematic review and meta-analysis of randomized controlled trials. Ultrasound Obstet Gynecol. 2017;50:578–583. doi: 10.1002/uog.17401. [DOI] [PubMed] [Google Scholar]
- 8.Yıldız E, Timur B. Comparison of classic single-layer uterin suture and double-layer purse-string suture techniques for uterus closure in terms of postoperative short-term uterine isthmocele: A prospective randomized controlled trial. Turk J Obstet Gynecol. 2023;20:206–213. doi: 10.4274/tjod.galenos.2023.90522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turan GA, Gur EB, Tatar S, Gokduman A, Guclu S. Uterine closure with unlocked suture in cesarean section: Safety and quality. Pak J Med Sci. 2014;30:530–534. doi: 10.12669/pjms.303.4545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vervoort AJMW, Uittenbogaard LB, Hehenkamp WJK, Brölmann HAM, Mol BWJ, Huirne JAF. Why do niches develop in caesarean uterine scars? Hypotheses on the aetiology of niche development. Hum Reprod. 2015;30:2695–702. doi: 10.1093/humrep/dev240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Setubal A, Alves J, Osório F, Guerra A, Fernandes R, Albornoz J, Sidiroupoulou Z. Treatment for uterine isthmocele, a pouchlike defect at the site of a cesarean section scar. J Minim Invasive Gynecol. 2018;25:38–46. doi: 10.1016/j.jmig.2017.09.022. [DOI] [PubMed] [Google Scholar]
- 12.Hosseini E, Aghajanpour S, Zameni N, Hafezi M. Isthmocele-a neglected cause of secondary infertility and implantation failure: A case report. Clin Case Rep. 2022;10(e05853) doi: 10.1002/ccr3.5853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scutiero G, Iannone P, Bernardi G, Bonaccorsi G, Spadaro S, Volta CA, Greco P, Nappi L. Oxidative stress and endometriosis: A systematic review of the literature. Oxid Med Cell Longev. 2017;2017(7265238) doi: 10.1155/2017/7265238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bij de Vaate AJM, Brölmann HAM, van der Voet LF, van der Slikke JW, Veersema S, Huirne JAF. Ultrasound evaluation of the cesarean scar: Relation between a niche and postmenstrual spotting. Ultrasound Obstet Gynecol. 2011;37:93–99. doi: 10.1002/uog.8864. [DOI] [PubMed] [Google Scholar]
- 15.Setúbal A, Alves J, Osório F, Sidiropoulou Z. Demonstration of isthmocele surgical repair. J Minim Invasive Gynecol. 2021;28:389–390. doi: 10.1016/j.jmig.2020.09.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data generated in the present study may be requested from the corresponding author.