Abstract
Primary cardiac lymphoma is an extremely rare disease, with the most common being diffuse large B-cell lymphoma (DLBCL). Fibrin-associated diffuse large B-cell lymphoma (FA-DLBCL) has been classified as a rare and unusual type of lymphoma and is included in the category of DLBCL associated with chronic inflammation (DLBCL-CI). In this study, we report a case of FA-DLBCL in the aortic valve and ascending aorta of a 51-year-old-woman.
Learning objective
In this rare case of FA-DLBCL in the aortic valve and ascending aorta, we highlight the features of FA-DLBCL and its differences from DLBCL-CI.
Keywords: Heart neoplasms, Prognosis, Lymphoma, Inflammation, World Health Organization
Introduction
Primary cardiac lymphomas (PCL) are extremely rare, with the most common being diffuse large B-cell lymphoma (DLBCL) [1,2]. Moreover, DLBCL is usually associated with an aggressive course and a high mortality rate [2]. Fibrin-associated diffuse large B-cell lymphoma (FA-DLBCL) has been classified as an unusual type of lymphoma and is considered a variant of DLBCL associated with chronic inflammation (DLBCL-CI), based on the 2017 WHO Classification [3]. DLBCL-CI occurs in the context of localized and maintained chronic inflammation and is commonly associated with Epstein–Barr virus (EBV) [4]. FA-DLBCL has been reported only in small cases and shows some differences when compared with DLBCL-CI [1,5,6]. However, FA-DLBCL has a more favorable prognosis than DLBCL-CI and is frequently associated with cardiac myxoma or prostheses in the heart [1,6]. In this study, we reported a rare case of FA-DLBCL of the aortic valve and ascending aorta.
Case report
A 51-year-old woman was referred to our hospital for surgery because of severe aortic regurgitation (AR) and thoracic aortic aneurysm. She was diagnosed with dermatomyositis and began steroid treatment 23 years before admission. She had been administered cyclosporine 18 years ago and methotrexate 6 years ago. She experienced stroke twice; the first stroke happened one year ago and the second stroke eight months ago. Although the cause of stroke was unclear, methotrexate-associated lymphoproliferative disorder (MTX-LPD) was considered to be the possible cause because of the multiple aneurysm formation with the uptake on FDG-PET on her face, skin, and liver and the biopsy results. Furthermore, multiple aneurysms disappeared after discontinuation of methotrexate.
After the patient's condition stabilized, she was referred to our hospital. Preoperative echocardiography showed severe aortic regurgitation, which was caused by dilatation of the aortic root and a small mass at the commissure between the noncoronary cusp and the right coronary cusp (Fig. 1A and B). The mass was classified as non-infectious endocarditis. Computed tomography revealed aortic enlargement from the aortic root to the descending aorta. The diameter of the ascending aortic aneurysm was 62 mm and the sinus of Valsalva was 54 mm, whereas that of the descending aorta was 50 mm (Fig. 1C). We performed mechanical-Bentall and arch replacement using the elephant trunk technique, which can be applied as a replacement technique for the descending aorta in the future. Multiple fibrin clots were found in the aortic valve, annulus, and ascending aorta, and were easy to peel (Fig. 2). As much as possible, we removed fibrin clots from the aorta and aortic annulus. The primary etiology of AR was thought to be enlargement of the aortic root and ascending aorta. Additionally, although adhesion of fibrin clots to the aortic cusp was noted, no obvious prolapse of the aortic cusp was observed.
Fig. 1.
Before treatment.
(A, B, and C) Transthoracic echocardiogram; parasternal long-axis view and short axis view revealing a small mass (arrows) in the aortic valve and severe aortic regurgitation.
(D) Computed tomography before treatment showing enlargement from the aortic root to the descending aorta.
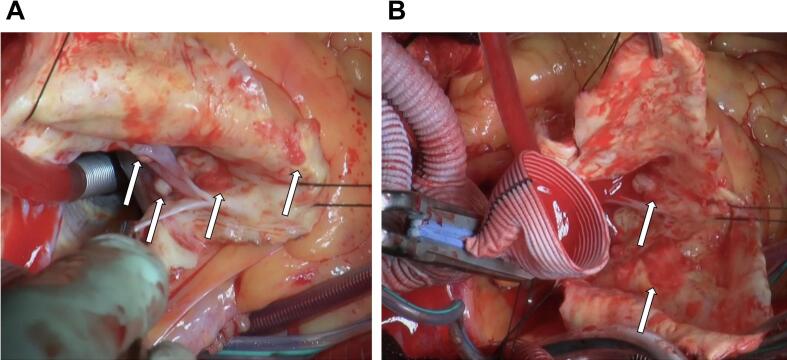
Fig. 2.
(A and B) Intraoperative view. Multiple fibrin clots in the aortic valve, annulus, and ascending aorta (arrows). Most of the fibrin clots were reddish in color, but some were white, as seen in the aortic valve leaflets.
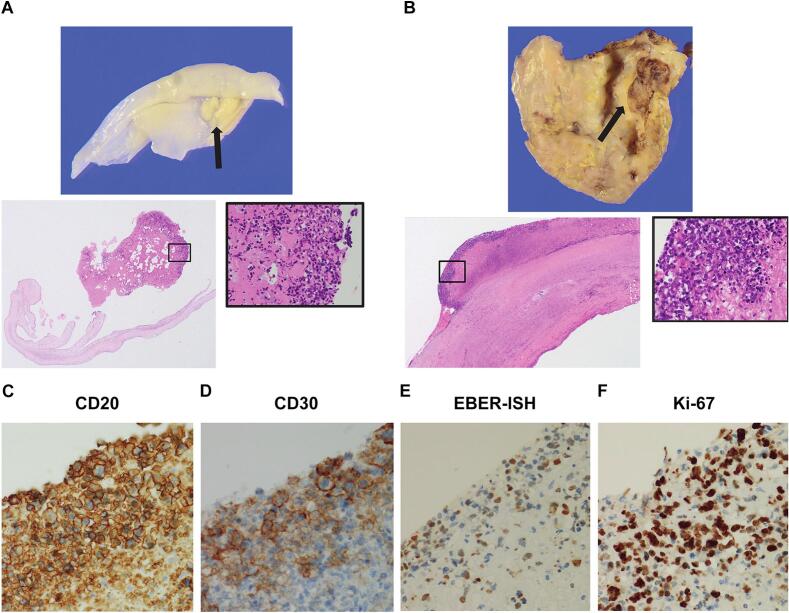
Based on the findings of histological examination, a hematoxylin and eosin-stained section of the clot showed lymphoid cell clustering near the surface of the fibrin clot material (Fig. 3A and B). Additional immunohistochemical staining was performed, and CD20, CD30, and Epstein–Barr virus early small RNAs in situ hybridization were positive, showing a high Ki67 proliferation index of >90 % (Fig. 3C–F). After the operation, the patient underwent bone marrow biopsy and presented with negative results. Therefore, the diagnosis of FA-DLBCL was limited to the aortic valve and ascending aorta. Her attending hematologist reported that the lymphoma was localized and additional chemotherapy was not required. Furthermore, she has had an uneventful course without the recurrence of lymphoma two years after surgery.
Fig. 3.
Pathological findings.
(A and B) Hematoxylin and eosin-stained sections of the clot (arrows) in the aortic valve and ascending aorta show lymphoid cell clustering near the surface of the fibrin clot material.
(C, D, E, and F) Immunohistochemical staining showed that CD20, CD30, and Epstein–Barr virus early small RNAs in situ hybridization were positive, indicating a high Ki67 proliferation index of >90 %.
Discussion
PCL is an extremely rare disease, with the most common histological type being DLBCL [1,2]. The diagnosis of PCL is usually conducted in the late disease course, and its estimated overall survival has been reported to be approximately 12 months [2]. FA-DLBCL is a rare type of DLBCL-CI and only a small number of cases have been reported. DLBCL-CI is included in the World Health Organization 2008 classification, occurs in the context of long-term chronic inflammation, and is associated with EBV [4]. The characteristics of DLBCL-CI include aggressive lymphoma and pyothorax-associated lymphoma occurring in patients treated with artificial pneumothorax for pulmonary tuberculosis. Furthermore, patients with DLBCL-CI tended to present significantly higher lymphoma-associated mortality rates.
FA-DLBCL is mediated by a local immunosuppression mechanism and can be associated with cardiac myxoma or prostheses in the heart. In FA-DLBCL, the tumor cells are arranged singly or in small clusters within the fibrin material or are associated with chronic blood effusions with a high proliferative index but without normal tissue invasion. Neoplastic cells typically have a non-GCB immunophenotype with a high proliferation index: CD20+, CD79a+, CD10−, BCL6-, IRF4/MUM1+, CD138+/−, and CD30+/−. FA-DLBCL is considered to have a more favorable prognosis with an indolent clinical course and may be cured by surgery alone without additional treatment. However, one study also suggested that diseases occurring in the primary cardiac or vascular sites are more likely to persist or recur than those occurring in other sites that are more amenable to complete resection.
In our case, the patient had a history of MTX-LPD, and its association with FA-DLBCL is unknown. Although FA-DLBCL typically occurs in immunocompetent patients, our patient was in an immunosuppressive state due to oral medicine. The clinical course was uneventful due to resection of the tumor without additional treatment. However, further studies are required to determine the optimal treatment method for FA-DLBCL.
Consent
We obtained the patient's written informed consent for publication of case details and images.
Declaration of competing interest
All authors declare that there is no conflict of interest.
Acknowledgments
We gratefully thank Hiroko Ikeda for his expert pathological review. The results of this case report were presented at the 65th Annual Meeting of Kansai Thoracic Surgical Association in June 2022.
References
- 1.Gruver A.M., Huba M.A., Dogan A., Hsi E.D. Fibrin-associated large B-cell lymphoma: part of the spectrum of cardiac lymphomas. Am J Surg Pathol. 2012;36:1527–1537. doi: 10.1097/PAS.0b013e31825d53b5. [DOI] [PubMed] [Google Scholar]
- 2.Petrich A., Cho S.I., Billett H. Primary cardiac lymphoma: an analysis of presentation, treatment, and outcome patterns. Cancer. 2011;117:581–589. doi: 10.1002/cncr.25444. [DOI] [PubMed] [Google Scholar]
- 3.Swerdlow S.H., Campo E., Harris N.L., Jaffe E.S., Pireli S.A., Stein H., Thiele J., Arber D.A., Hasserjian R.P., Beau M.L., Orazi A., Siebert R. International Agency for Research on Cancer; Lyon: 2017. WHO classification of tumours of haematopoietic and lymphoid tissues. Revised 4th ed. [Google Scholar]
- 4.Swerdlow S.H., Campo E., Harris N.L., Jaffe E.S., Pileri S.A., Stein H., Thiele J., Vardiman J.W. 4th ed. IARC Press; Lyon: 2008. WHO classification of tumours of haematopoietic and lymphoid tissues. [Google Scholar]
- 5.Boyer D.F., McKelvie P.A., de Leval L., Edlefsen K.L., Ko Y.H., Aberman Z.A., Kovach A.E., Masih A., Nishino H.T., Weiss L.M., Meeker A.K., Nardi V., Palisoc M., Shao L., Pittaluga S., et al. Fibrin-associated EBV-positive large B-cell lymphoma: an indolent neoplasm with features distinct from diffuse large B-cell lymphoma associated with chronic inflammation. Am J Surg Pathol. 2017;41:299–312. doi: 10.1097/PAS.0000000000000775. [DOI] [PubMed] [Google Scholar]
- 6.Moreno E.M., Ferrer-Gómez A., Arias H.P., García I.G., García-Cosío M. Fibrin-associated diffuse large B-cell lymphoma with plasmacytic differentiation: case report and literature review. Diagn Pathol. 2020;15:117. doi: 10.1186/s13000-020-01034-7. [DOI] [PMC free article] [PubMed] [Google Scholar]