Abstract
Saharan dust storms, which originate from the Sahara desert, have a significant impact on global health, especially on respiratory conditions of populations exposed to fine particulate matter that travels across continents. Dust events, characterized by the transport of mineral dust such as quartz and feldspar, lead to the suspension of particulate matter in the atmosphere, capable of traversing long distances and affecting air quality adversely. Emerging research links these dust episodes with increased incidence and exacerbation of lung diseases, including asthma and chronic obstructive pulmonary disease, especially during peak dust emission seasons from November to March. The present review aims to synthesize existing scientific evidence concerning the respiratory health impacts of Saharan dust, examining the environmental dynamics of dust transmission, the physical and chemical properties of dust particles, and their biological effects on human health. Further, it assesses epidemiological studies and discusses public health strategies for mitigating adverse health outcomes. Given the complexity of interactions between atmospheric dust particles and respiratory health, this review also highlights critical research gaps that need attention to better understand and manage the health risks associated with Saharan dust.
Keywords: Saharan dust, respiratory health, particulate matter, Sahara desert, public health strategies
1. Introduction
Saharan dust storms, also known as Saharan dust events, are natural phenomena characterized by the transport of vast quantities of mineral dust from the Sahara Desert across the African continent and beyond. These dust events occur predominantly during the dry season, typically from November to March, when intense atmospheric pressure systems over North Africa drive the movement of dust-laden air masses towards the Atlantic Ocean and surrounding regions. In West Africa, the Harmattan winds are a specific example of winds that can deliver Saharan dust, but other wind patterns contribute to dust transport across wider areas (1,2).
The Sahara desert, the largest hot desert in the world, serves as the primary source of Saharan dust emissions. With its extensive arid and semi-arid landscapes, the Sahara experiences frequent dust uplift due to strong surface winds, convective processes, and occasional thunderstorms. The resulting dust plumes can travel thousands of kilometers, crossing international borders and affecting diverse ecosystems, from the Caribbean to the Amazon rainforest and even reaching as far as Europe and North America (3,4).
The global impact of Saharan dust storms is profound, influencing various environmental, atmospheric and socio-economic processes. Dust particles suspended in the atmosphere play a crucial role in modulating Earth's radiative balance, affecting regional and global climate patterns through the scattering and absorption of solar radiation. Additionally, Saharan dust deposition contributes essential nutrients, such as iron and phosphorus, to marine and terrestrial ecosystems, influencing ecosystem dynamics and productivity (5,6).
Furthermore, Saharan dust can have significant implications for air quality and human health, particularly in regions downwind of dust source areas. Dust storms can elevate levels of particulate matter (PM) in the atmosphere, including coarse and fine particles capable of penetrating deep into the respiratory system. This can exacerbate respiratory conditions, trigger allergic reactions, and contribute to cardiovascular morbidity, posing risks to vulnerable populations, such as children, the elderly, and individuals with pre-existing respiratory diseases (7,8).
In recent years, there has been increasing recognition of the association between exposure to Saharan dust particles and the incidence and exacerbation of lung diseases. While research on this topic is still evolving, emerging evidence suggests that inhalation of Saharan dust may contribute to respiratory symptoms, exacerbate pre-existing lung conditions, and increase the risk of developing respiratory illnesses (9,10).
The composition and characteristics of Saharan dust particles, including their size distribution, mineralogical composition, and surface chemistry, play a critical role in determining their biological effects on the respiratory system. Fine dust particles, with diameters <2.5 micrometers (PM2.5), are of particular concern due to their ability to penetrate deep into the lungs and potentially induce inflammation, oxidative stress and tissue damage (11).
The associations between Saharan dust events and adverse respiratory health outcomes in affected populations are well documented. These include an increase in hospital admissions for respiratory conditions, such as asthma exacerbations, chronic obstructive pulmonary disease (COPD) exacerbations and respiratory tract infections, during periods of elevated dust concentrations. Additionally, epidemiological investigations have identified correlations between dust exposure levels and respiratory symptoms, such as coughing, wheezing and shortness of breath, particularly among individuals with underlying respiratory conditions (12,13).
The present review focuses on the critical interactions between Saharan dust particles and respiratory health, highlighting how the unique physical and chemical properties of the dust exacerbate conditions such as asthma and COPD, particularly in vulnerable populations.
2. Composition and characteristics of Saharan dust
Origins and pathways of Saharan dust transport
The Sahara desert, spanning over 9 million square kilometers, serves as the primary source of Saharan dust emissions (14). Dust uplift events occur throughout the year but peak during the dry season, from late fall to early spring, when intense surface heating leads to convective instability and strong winds across the desert region. These winds, often associated with the Saharan heat low and the Azores high pressure systems, drive the movement of dust-laden air masses towards the Atlantic Ocean and surrounding continents (15).
Several pathways facilitate the long-range transport of Saharan dust across the globe. The most prominent is the Saharan Air Layer (SAL), a well-defined layer of warm, dry and dusty air that extends from the Sahara across the tropical North Atlantic. The SAL acts as a conduit for dust particles, carrying them thousands of kilometers westward towards the Caribbean, South America and North America. Additionally, atmospheric circulation patterns, such as the African easterly jet and the African easterly waves, play crucial roles in transporting dust plumes across Africa, Europe and the Mediterranean basin (16-18).
The interplay between synoptic weather systems, regional topography and land-atmosphere interactions influences the spatial and temporal variability of dust emissions and transport. Dust storms can originate from various source regions within the Sahara, including the Bodele Depression in Chad, the Bodélé Escarpment in Niger, and the Libyan desert, each characterized by unique geomorphological features and dust emission mechanisms. Moreover, episodic weather phenomena, such as convective thunderstorms and haboobs (dust storms associated with cold fronts), can locally enhance dust production and mobilization, leading to intense dust storms with significant impacts on air quality and visibility (19,20).
Chemical composition of Saharan dust particles
Saharan dust particles are predominantly mineralogical in nature, composed primarily of silicates, carbonates, oxides and sulfates derived from the weathering and erosion of geological formations in the Sahara desert. Quartz, feldspar and clay minerals are among the most abundant components of Saharan dust, reflecting the diverse lithological composition of the source regions (21).
In addition to mineral dust, Saharan dust particles may also contain organic matter, trace elements and anthropogenic pollutants, resulting from surface interactions, atmospheric processing, and mixing with pollution plumes during transport (22).
The chemical composition of Saharan dust particles varies spatially and temporally, reflecting differences in source rock types, weathering processes, and atmospheric processing during transport. Elemental analysis of dust samples has revealed enrichment in elements such as silicon, aluminum, iron, calcium, magnesium and potassium, which are characteristic of silicate minerals abundant in the Sahara region (23). Additionally, trace elements, including heavy metals such as lead, cadmium and zinc, may be present in Saharan dust particles, originating from both natural sources and anthropogenic activities within the source region (24).
Furthermore, chemical reactions occurring on the surface of dust particles during atmospheric transport can alter their composition and properties, affecting their reactivity, hygroscopicity and potential health impacts. For example, iron-rich dust particles can act as carriers of bioavailable iron, which may stimulate biological productivity in marine and terrestrial ecosystems upon deposition (25). Additionally, the interaction of dust particles with atmospheric gases, such as sulfur dioxide and nitrogen oxides, can lead to the formation of secondary aerosols and affect regional air quality and climate (26).
Physical properties and atmospheric behavior
Saharan dust particles exhibit a wide range of physical properties, including size, shape, density and aerodynamic characteristics, which influence their transport, deposition and atmospheric behavior (27).
Dust particles generated by aeolian processes in the Sahara desert range in size from submicron (<1 µm) to coarse (>10 µm) particles, with the majority falling within the fine (<2.5 µm) and coarse (2.5-10 µm) fractions (28). Fine dust particles, known as PM2.5, are of particular concern due to their potential to penetrate deep into the respiratory system and impact human health (29).
The shape and morphology of Saharan dust particles vary depending on their mineralogical composition and the processes involved in their formation and transport. Dust particles may exhibit angular, irregular, or spheroidal shapes, reflecting differences in the degree of weathering, abrasion and transport history. Coarse particles tend to be more angular and irregular, while fine particles may undergo rounding and surface smoothing during long-range transport, resulting in more spherical shapes (30).
The density of Saharan dust particles also varies depending on their mineral composition and porosity, with typical values ranging from 2.5 to 3.5 g/cm³ for silicate minerals such as quartz and feldspar. Coarse dust particles tend to have higher densities than fine particles due to their larger grain sizes and higher packing densities. Additionally, the aerodynamic properties of dust particles, such as settling velocity and terminal velocity, play a crucial role in determining their transport and deposition patterns in the atmosphere and the environment (31,32).
Atmospheric behavior of Saharan dust particles is influenced by a complex interplay of meteorological factors, including wind speed and direction, atmospheric stability, turbulence, and vertical mixing processes. Dust particles injected into the atmosphere by surface winds can be transported over long distances by prevailing winds aloft, reaching altitudes of several kilometers and forming extensive dust plumes. The vertical distribution of dust in the atmosphere is controlled by atmospheric stability and vertical mixing processes, with higher concentrations typically observed near the surface during dust events and loftier layers aloft during transport (33,34).
3. Health effects of Saharan dust exposure on the respiratory system
Inhalation of PM and its effects on lung health
PM is a complex mixture of solid and liquid particles suspended in the air, varying in size, composition and origin. Inhalation of PM, particularly fine and ultrafine particles, can have detrimental effects on respiratory health, ranging from acute irritation to chronic lung diseases and cardiovascular morbidity. Saharan dust events contribute to elevated levels of PM in the atmosphere, exposing populations to increased health risks, especially in regions downwind of dust source areas. Fine dust particles, PM2.5, pose the greatest health concern due to their ability to penetrate deep into the respiratory system and reach the alveolar region of the lungs. Upon inhalation, PM2.5 particles can induce inflammation, oxidative stress and cellular damage in lung tissues, leading to a range of adverse respiratory effects. Additionally, ultrafine particles (<0.1 micrometers) can translocate across the respiratory epithelium into systemic circulation, potentially exacerbating cardiovascular diseases and systemic inflammation (35,36).
The biological mechanisms underlying the respiratory effects of PM inhalation are multifaceted and involve inflammatory responses, oxidative stress and disruption of cellular signaling pathways. PM particles can activate immune cells, such as macrophages and neutrophils, leading to the release of pro-inflammatory mediators, cytokines and reactive oxygen species (ROS) (37,38).
Chronic exposure to PM has been associated with airway inflammation, epithelial damage, mucous hypersecretion and impaired lung function, contributing to the development and progression of respiratory diseases, including asthma, chronic bronchitis and COPD (39,40).
Association between Saharan dust events and respiratory symptoms
Epidemiological studies have provided evidence of associations between Saharan dust events and adverse respiratory health outcomes in affected populations. During dust storm episodes, increases in ambient PM concentrations have been correlated with elevated rates of respiratory symptoms, exacerbations of pre-existing lung conditions, and hospital admissions for respiratory illnesses. These associations are particularly pronounced in vulnerable individuals, such as children, the elderly and individuals with underlying respiratory diseases (41,42).
A study conducted in the Caribbean region found that increases in PM10 concentrations during Saharan dust episodes were associated with higher rates of emergency room visits for asthma exacerbations and acute respiratory infections in children (43). Similarly, investigations in West Africa have reported elevated levels of respiratory symptoms, such as coughing, wheezing and shortness of breath, among residents exposed to high dust concentrations during Harmattan periods (44). Furthermore, longitudinal studies have identified temporal trends linking dust exposure to changes in respiratory health indicators, including decreased lung function, increased airway reactivity, and higher medication use among asthma and COPD patients during dust storm seasons (45).
Impact on vulnerable populations, such as children, elderly and pregnant women
Vulnerable populations, such as children, the elderly and individuals with pre-existing respiratory conditions, are particularly susceptible to the adverse health effects of Saharan dust exposure. Children, whose respiratory systems are still developing, may experience exacerbated symptoms of asthma and respiratory infections during dust storm episodes due to increased airway inflammation and susceptibility to respiratory irritants (46).
Elderly individuals, especially those with underlying cardiovascular diseases or compromised lung function, are at higher risk of experiencing respiratory symptoms and exacerbations of chronic conditions during dust events. Reduced lung elasticity and impaired mucociliary clearance in the elderly can exacerbate the deposition and retention of dust particles in the airways, leading to respiratory distress and functional decline (47). Furthermore, individuals with pre-existing respiratory diseases, such as asthma, COPD and allergic rhinitis, may experience worsened symptoms and decreased disease control during Saharan dust episodes. The pro-inflammatory and irritant properties of dust particles can trigger airway inflammation, bronchoconstriction and exacerbations of respiratory conditions, necessitating increased medication use and healthcare utilization among affected individuals (48,49).
Vodonos et al (50) identified a positive correlation between dust storms and hospitalization rates for COPD exacerbations, showing a 16% increase in Southern Israel. This effect was more pronounced with age and higher in women. In a laboratory study involving young healthy adults, researchers found that women had 11-23% greater deposition of inhaled particles in the central airways compared with men (51). This sex disparity was most evident with coarser particles (>5 µm). Women may experience greater susceptibility to air pollution, including dust, due to physiological factors such as smaller lung volume and airway size, leading to more particulate deposition in the lungs. The elevated concentration of PM in the central airways leads to greater irritation and inflammation, potentially triggering acute COPD exacerbations (52). During pregnancy, a woman's respiratory system undergoes significant changes, including a 20% increase in oxygen consumption to accommodate the increased oxygen demands of her and the growing fetus (53). As a result of these changes, pregnant women are particularly vulnerable to the effects of air pollution because of the increased number of pollutants inhaled.
Air pollution can trigger common respiratory diseases such as asthma and allergic rhinitis. The major adverse maternal outcome associated with air pollution is maternal hypertensive disorders such as pre-eclampsia (54). A meta-analysis of 33 cohort studies revealed that exposure to PM10 increased the relative risk (55). Furthermore, an increasing number of research suggests that maternal exposure to PM may also impact the fetus. Pollutants can cross the placenta, entering the fetal circulation during gestation (56).
Maternal exposure to Saharan dust appears to influence the fetal lung development and respiratory system after birth. A study evaluated that exposure to PM2.5 was associated with tachypnea of the newborn, asphyxia and respiratory distress syndrome (57). Different studies have looked at the effects on fetal growth. A systematic review of 52 studies and a meta-analysis of 54 studies found that maternal exposure to PM2.5, PM10 and other air pollutants was generally positively associated with low birth weight (58).
4. Mechanisms underlying the pathogenicity of Saharan dust
Inflammatory responses triggered by dust particle exposure
Inhalation of Saharan dust particles can trigger inflammatory responses in the respiratory system, leading to acute and chronic respiratory conditions. Upon deposition in the airways, dust particles activate innate immune cells, such as macrophages and neutrophils, through pattern recognition receptors and toll-like receptors (59,60). Recognition of microbial components and danger-associated molecular patterns on the surface of dust particles induces the production of pro-inflammatory cytokines, chemokines and ROS by immune cells, initiating an inflammatory cascade. It has been demonstrated that exposure to Saharan dust induces significant expression of pro-inflammatory cytokines such as GM-CSF and G-CSF, which play crucial roles in the exacerbation of respiratory conditions (61). Pro-inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-α), interleukin-1 beta (IL-1β), and interleukin-6 (IL-6), recruit additional immune cells to the site of inflammation and activate downstream signaling pathways, amplifying the inflammatory response (62,63). Chemokines, such as interleukin-8 (IL-8), promote the migration of neutrophils and other immune cells to the airways, further exacerbating inflammation and tissue damage. Additionally, ROS generated by activated immune cells contribute to oxidative stress, lipid peroxidation and DNA damage, exacerbating inflammatory responses and tissue injury (64,65).
Chronic exposure to Saharan dust particles can lead to sustained inflammation and airway remodeling, characterized by epithelial hyperplasia, mucus hypersecretion, fibrosis and smooth muscle hypertrophy, contributing to the pathogenesis of respiratory diseases such as asthma, chronic bronchitis and COPD (66,67). Furthermore, interactions between inflammatory mediators and neural pathways can exacerbate airway hyperresponsiveness and bronchoconstriction, leading to respiratory symptoms and functional impairment (68).
Moreover, it has been highlighted that airborne particles such as PM2.5, cigarette smoke and diesel exhaust can induce endothelial dysfunction, promoting inflammation and increasing the risk of chronic respiratory diseases (69).
Activation of immune pathways and oxidative stress
In addition to inflammatory responses, exposure to Saharan dust particles can activate immune pathways and induce oxidative stress in the respiratory system. Dust particles contain a variety of biologically active components, including microbial antigens, endotoxins, metals and organic pollutants, which can stimulate immune cells and promote inflammatory and immune responses. Upon inhalation, Saharan dust particles interact with the respiratory epithelium, triggering an inflammatory response that can exacerbate pre-existing respiratory conditions. The interaction of fine PM (PM2.5) with immune cells, such as macrophages, further amplifies oxidative stress, leading to airway hyperresponsiveness and long-term damage (70,71).
Endotoxins, derived from the outer membrane of gram-negative bacteria, are abundant in Saharan dust and can activate toll-like receptor 4 (TLR4) signaling pathways, leading to the production of pro-inflammatory cytokines, such as interleukin-1 beta (IL-1β) and interleukin-6 (IL-6), by immune cells (72,73). Additionally, microbial components and allergens present in dust particles can trigger allergic immune responses, leading to the production of immunoglobulin E antibodies and the activation of mast cells and eosinophils, contributing to allergic asthma and allergic rhinitis (74).
Oxidative stress, resulting from an imbalance between the production of ROS and antioxidant defenses, is a common feature of Saharan dust-induced inflammation and respiratory injury. Dust particles can contain transition metals, such as iron, manganese and copper, which catalyze the generation of ROS through Fenton and Haber-Weiss reactions, leading to lipid peroxidation, protein oxidation and DNA damage in lung tissues (75,76). Additionally, ROS can activate redox-sensitive transcription factors, such as nuclear factor kappa B (NF-κB) and activator protein 1 (AP-1), leading to the upregulation of pro-inflammatory genes and the perpetuation of inflammatory responses (77,78). Moreover, inhalation of Saharan dust has been demonstrated to induce oxidative stress and activate the NLRP3 inflammasome, leading to significant release of pro-inflammatory cytokines, thereby exacerbating lung inflammation (79).
Contribution to the development and exacerbation of lung diseases
The inflammatory and oxidative effects of Saharan dust exposure contribute to the development and exacerbation of various respiratory diseases, including asthma, chronic bronchitis, COPD and allergic rhinitis. Acute exposure to high levels of Saharan dust particles can trigger asthma exacerbations and respiratory symptoms in susceptible individuals, leading to increased medication use, emergency department visits, and hospital admissions (80,81).
Chronic exposure to Saharan dust particles can exacerbate pre-existing respiratory conditions and impair lung function over time, particularly in vulnerable populations, such as children, the elderly, and individuals with underlying lung diseases. The persistent inflammatory responses induced by dust exposure can lead to airway remodeling, fibrosis and bronchial hyperresponsiveness, contributing to the progression of chronic respiratory diseases and the development of irreversible airflow obstruction (82,83).
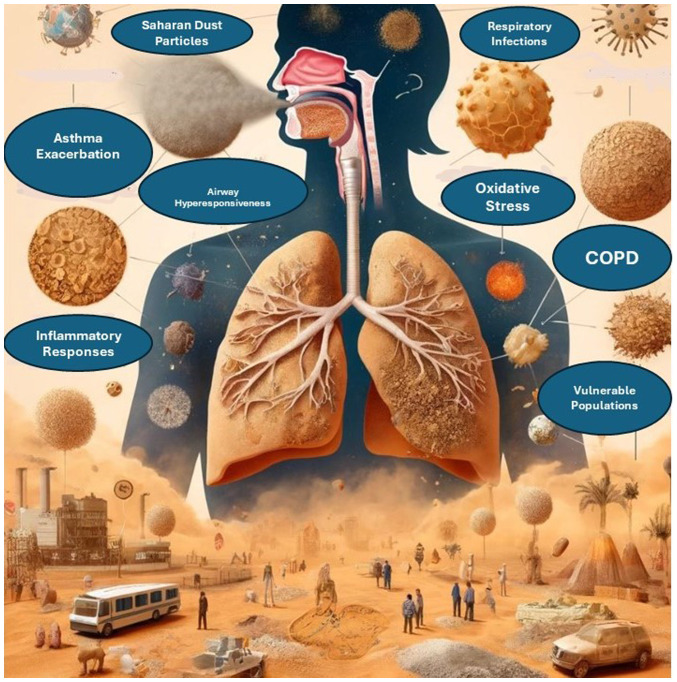
Furthermore, Saharan dust exposure may interact with other environmental pollutants, such as vehicular emissions, industrial pollutants and biomass burning aerosols, to exacerbate respiratory health effects and increase the risk of adverse outcomes. Synergistic interactions between dust particles and other pollutants can amplify inflammatory responses, oxidative stress and airway injury, leading to more severe respiratory symptoms and poorer health outcomes (84). The various respiratory health effects associated with the inhalation of Saharan dust particles are illustrated in Fig. 1.
Figure 1.
Impact of Saharan dust on respiratory health. This figure illustrates various health conditions associated with exposure to Saharan dust particles, including asthma exacerbation, airway hyperresponsiveness, inflammatory responses, respiratory infections, oxidative stress and COPD. Vulnerable populations, such as individuals with pre-existing respiratory conditions and children, are particularly at risk. Dust particles can cause significant respiratory issues through pathways such as oxidative stress and airway inflammation. COPD, chronic obstructive pulmonary disease.
5. Geographic variability and environmental factors influencing health outcomes
The health effects of Saharan dust exposure exhibit geographic variability, with differences observed in the magnitude and frequency of dust events, as well as in the susceptibility of populations to respiratory health effects. Environmental factors, including meteorological conditions, air pollution levels, land use patterns and socio-economic factors, play crucial roles in modulating the health impacts of dust storms and influencing health outcomes in affected regions.
Regions located downwind of major dust source areas, such as the Sahel region of West Africa and the Caribbean islands, experience higher levels of dust exposure and are more susceptible to respiratory health effects during dust events (85). The frequency and intensity of dust storms in these regions are influenced by seasonal weather patterns, such as the West African monsoon and the North Atlantic Oscillation, which affect dust emission, transport and deposition processes (86).
Additionally, environmental factors such as air pollution levels and background PM concentrations can interact with Saharan dust particles to exacerbate respiratory health effects and increase the risk of adverse outcomes. Coarse and fine PM from local sources, such as vehicular emissions, industrial pollution and biomass burning, can mix with Saharan dust plumes during transport, leading to elevated levels of airborne pollutants and exacerbating air quality problems in dust-affected regions (87).
Furthermore, socio-economic factors, including housing conditions, access to healthcare and socio-demographic characteristics, can influence the vulnerability of populations to dust-related health risks. Socio-economically disadvantaged communities, such as low-income neighborhoods and rural settlements, may face greater challenges in accessing healthcare services, implementing preventive measures and mitigating the impacts of dust storms on respiratory health (88).
6. Mitigation strategies and public health implications
Strategies for reducing exposure to Saharan dust particles
Mitigating exposure to Saharan dust particles requires a multi-faceted approach involving individual actions, community measures and environmental management strategies. While it may not be possible to completely eliminate exposure to dust particles, several strategies can help reduce the risk of respiratory health effects associated with dust storms.
To mitigate the infiltration of outdoor air laden with dust particles into indoor environments, it is advised to keep windows and doors closed during dust events. Additionally, employing air purifiers equipped with high-efficiency particulate air filters can effectively remove dust particles from indoor air sources (14). During episodes of poor outdoor air quality resulting from dust storms, individuals are encouraged to utilize face masks or respirators. Optimal choices for filtration include N95 respirators, designed to effectively filter fine PM, thereby reducing the inhalation of dust particles (89). Enhancing indoor air quality can be achieved through the installation of air filtration systems in various settings such as homes, schools and workplaces. Employing high-efficiency HVAC filters aids in capturing airborne dust particles and preventing their re-circulation within indoor environments (90).
Mitigating dust impacts within urban settings necessitates the integration of urban design elements such as green spaces, street trees and vegetated buffers. Furthermore, incorporating dust control measures into construction projects and infrastructure development endeavors aids in minimizing dust emissions (91). Employing dust suppressants, such as water sprays, chemical stabilizers and soil binders, offers an effective approach to reduce dust emissions from unpaved roads, construction sites and open land areas. Consistent application of these techniques, including regular surface wetting, aids in controlling dust and preventing its resuspension by wind. Promoting awareness regarding the health risks associated with exposure to Saharan dust and advocating preventive measures are essential components of public health initiatives. Dissemination of educational materials, issuance of health advisories, and implementation of outreach programs serve to inform communities about dust-related health hazards and encourage the adoption of protective measures (2).
Public health interventions to mitigate respiratory health risks
In addition to individual and community-level strategies, public health interventions play a critical role in mitigating respiratory health risks associated with Saharan dust exposure. These interventions aim to enhance surveillance, monitoring and response efforts to protect vulnerable populations and reduce the burden of dust-related respiratory diseases.
Establishing and maintaining air quality monitoring networks is crucial for tracking dust concentrations and pollutant levels during dust events. Real-time monitoring data should be utilized to issue air quality alerts, advisories, and warnings to the public and healthcare providers (92).
The development and implementation of health surveillance systems are essential to monitor respiratory symptoms, hospital admissions and mortality rates during dust events. Collecting and analyzing epidemiological data enables the assessment of the impact of dust exposure on respiratory health outcomes and identification of at-risk populations (45).
Developing emergency response plans and protocols is imperative to address respiratory health emergencies associated with Saharan dust storms. Coordination with healthcare facilities, emergency responders, and public health agencies ensures timely access to medical care and support services for affected individuals (81).
Providing training and education for healthcare providers on the recognition, diagnosis, and management of respiratory conditions related to Saharan dust exposure is essential. Promoting evidence-based clinical practices and treatment guidelines facilitates the management of acute exacerbations and complications of dust-related respiratory diseases (82).
Engaging community stakeholders, advocacy groups, and local organizations in dust awareness campaigns, public forums, and community-based interventions is vital. Partnerships with schools, workplaces and community centers facilitate the dissemination of health information and promotion of preventive measures (71).
Policy recommendations and future directions for research and action
Addressing the public health implications of Saharan dust exposure necessitates coordinated efforts across multiple sectors, including environmental protection, public health, urban planning, and climate resilience. Future research should focus on understanding the complex interactions between Saharan dust and urban pollutants, as well as their combined effects on respiratory health. Identifying how these interactions differ based on geography and population demographics could inform more effective public health interventions. The following policy recommendations and future research priorities can guide efforts to mitigate dust-related respiratory health risks and promote sustainable development.
Developing comprehensive air quality management strategies that address the sources, transport, and impacts of Saharan dust on respiratory health is imperative. Integrating dust monitoring and mitigation measures into existing air quality management frameworks and regulations is recommended (84).
Incorporating dust-related health risks into climate adaptation and resilience plans is essential for safeguarding public health in the face of climate change. Implementing strategies to enhance community resilience, build adaptive capacity, and reduce vulnerability to dust storms and other environmental hazards is crucial (59).
Fostering collaboration and knowledge exchange among countries affected by Saharan dust storms is essential. Promoting regional cooperation and joint initiatives to address transboundary air pollution and cross-border health impacts facilitates the sharing of best practices, research findings and capacity-building efforts (93).
Investing in research and innovation to advance understanding of the mechanisms, drivers, and health effects of Saharan dust exposure is necessary. Supporting interdisciplinary research projects, observational studies, and modeling efforts improves predictive capabilities and informs evidence-based interventions (94).
Ensuring coherence and alignment between policies related to air quality, public health, environmental management and sustainable development is critical. Integrating dust mitigation measures into national and regional policy frameworks, including climate action plans, health strategies and disaster risk reduction policies, promotes policy integration and coherence (95).
These recommendations and future directions underscore the importance of proactive measures and collaborative approaches in addressing the complex challenges posed by Saharan dust exposure and its implications for respiratory health and sustainable development.
7. Conclusions
In summary, Saharan dust storms pose significant respiratory health risks, driven by the transport of mineral dust across continents. Inhalation of PM from these events exacerbates respiratory conditions and increases the risk of developing lung diseases, particularly among vulnerable populations. Tailored mitigation strategies, including air quality management and public health interventions, are essential for addressing these risks. Collaboration, research investment and policy coherence are vital for effective mitigation and promoting sustainable development in the face of Saharan dust exposure.
Acknowledgements
Not applicable.
Funding Statement
Funding: Not funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
AD and VEG conceptualized the study. AD, CT, VEG, PP, DB, NT and DAS made substantial contributions to data interpretation and analysis, and wrote and prepared the draft of the manuscript. AD and VEG analyzed the data and provided critical revisions. All authors contributed to manuscript revision, read and approved the final version of the manuscript. Data authentication is not applicable.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
DAS is the Editor-in-Chief for the journal, but had no personal involvement in the reviewing process, or any influence in terms of adjudicating on the final decision, for this article. The other authors confirm that they have no competing interests.
Use of artificial intelligence tools
During the preparation of this work, artificial intelligence tools were used to improve the readability and language of the manuscript or to generate images, and subsequently, the authors revised and edited the content produced by artificial intelligence tools as necessary, taking full responsibility for the ultimate content of the present manuscript.
References
- 1.Knippertz P. Mineral dust generation across northern Africa and its impacts. In: Oxford Research Encyclopedia of Climate Science. Storch H (ed). Oxford University Press, New York, NY, 2017. [Google Scholar]
- 2.Goudie AS. Dust storms: Recent developments. J Environ Manage. 2009;90:89–94. doi: 10.1016/j.jenvman.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 3.Thomas N, Nigam S. Twentieth-century climate change over Africa: Seasonal hydroclimate trends and Sahara desert expansion. J Clim. 2018;31:3349–3370. [Google Scholar]
- 4.Griffin DW, Kellogg CA, Garrison VH, Shinn EA. The global transport of dust: An intercontinental river of dust, microorganisms and toxic chemicals flows through the Earth's atmosphere. Am Sci. 2002;90:228–235. [Google Scholar]
- 5.Prospero JM. Long-range transport of mineral dust in the global atmosphere: Impact of African dust on the environment of the southeastern United States. Proc Natl Acad SciUSA. 1999;96:3396–3403. doi: 10.1073/pnas.96.7.3396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schepanski K. Transport of mineral dust and its impact on climate. Geosciences. 2018;8(151) [Google Scholar]
- 7.Griffin DW. Atmospheric movement of microorganisms in clouds of desert dust and implications for human health. Clin Microbiol Rev. 2007;20:459–477. doi: 10.1128/CMR.00039-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Varrica D, Alaimo MG. Influence of Saharan dust on the composition of urban aerosols in Palermo City (Italy) Atmosphere. 2024;15(254) [Google Scholar]
- 9.Gutierrez MP, Zuidema P, Mirsaeidi M, Campos M, Kumar N. Association between African dust transport and acute exacerbations of COPD in Miami. J Clin Med. 2020;9(2496) doi: 10.3390/jcm9082496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schweitzer MD, Calzadilla AS, Salamo O, Sharifi A, Kumar N, Holt G, Campos M, Mirsaeidi M. Lung health in era of climate change and dust storms. Environ Res. 2018;163:36–42. doi: 10.1016/j.envres.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 11.Scheuvens D, Schütz L, Kandler K, Ebert M, Weinbruch S. Bulk composition of northern African dust and its source sediments-A compilation. Earth Sci Rev. 2013;116:170–194. [Google Scholar]
- 12.Trianti SM, Samoli E, Rodopoulou S, Katsouyanni K, Papiris SA, Karakatsani A. Desert dust outbreaks and respiratory morbidity in Athens, Greece. Environ Health. 2017;16(72) doi: 10.1186/s12940-017-0281-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rublee CS, Sorensen CJ, Lemery J, Wade TJ, Sams EA, Hilborn ED, Crooks JL. Associations between dust storms and intensive care unit admissions in the United States, 2000-2015. Geohealth. 2020;4(e2020GH000260) doi: 10.1029/2020GH000260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Longueville F, Hountondji YC, Henry S, Ozer P. What do we know about effects of desert dust on air quality and human health in West Africa compared to other regions? Sci Total Environ. 2010;409:1–8. doi: 10.1016/j.scitotenv.2010.09.025. [DOI] [PubMed] [Google Scholar]
- 15.Marsham JH, Parker DJ, Grams CM, Taylor CM, Haywood JM. Uplift of Saharan dust south of the intertropical discontinuity. J Geophys Res Atmos. 2008;113(D21102) [Google Scholar]
- 16.Prospero JM, Mayol-Bracero OL. Understanding the transport and impact of African dust on the Caribbean Basin. Bull Am Meteorol Soc. 2013;94:1329–1337. [Google Scholar]
- 17.Harrison AD, O'Sullivan D, Adams MP, Porter GCE, Blades E, Brathwaite C, Chewitt-Lucas R, Gaston C, Hawker R, Krüger OO, et al. The ice-nucleating activity of African mineral dust in the Caribbean boundary layer. Atmos Chem Phys. 2022;22:9663–9680. [Google Scholar]
- 18.Boose Y, Sierau B, García MI, Rodríguez S, Alastuey A, Linke C, Schnaiter M, Kupiszewski P, Kanji ZA, Lohmann U. Ice nucleating particles in the Saharan air layer. Atmos Chem Phys. 2016;16:9067–9087. [Google Scholar]
- 19.Namdari S, Karimi N, Sorooshian A, Mohammadi G, Sehatkashani S. Impacts of climate and synoptic fluctuations on dust storm activity over the Middle East. Atmos Environ (1994) 2018;173:265–276. doi: 10.1016/j.atmosenv.2017.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Knippertz P. Meteorological aspects of dust storms. Mineral dust: A key player in the earth system, pp121-147, 2014. [Google Scholar]
- 21.Navarro-Ciurana D, Corbella M, Farré-de-Pablo J, Corral I, Buixadera E, Morera-Valverde R, Proenza JA. Rare Earth Elements' particles in road dust: A mineralogical perspective for source identification. Atmos Environ. 2023;309(119927) [Google Scholar]
- 22.Erel Y, Dayan U, Rabi R, Rudich Y, Stein M. Trans boundary transport of pollutants by atmospheric mineral dust. Environ Sci Technol. 2006;40:2996–3005. doi: 10.1021/es051502l. [DOI] [PubMed] [Google Scholar]
- 23.Kumar A, Shukla G, Singh A. Long-range global transport and characterization of dust. In Asian Atmospheric Pollution. Elsevier, pp483-504, 2022. [Google Scholar]
- 24.Schleicher NJ, Dong S, Packman H, Little SH, Ochoa Gonzalez R, Najorka J, Sun Y, Weiss DJ. A global assessment of copper, zinc, and lead isotopes in mineral dust sources and aerosols. Front Earth Sci. 2020;8(167) [Google Scholar]
- 25.Jickells TD, An ZS, Andersen KK, Baker AR, Bergametti G, Brooks N, Cao JJ, Boyd PW, Duce RA, Hunter KA, et al. Global iron connections between desert dust, ocean biogeochemistry, and climate. Science. 2005;308:67–71. doi: 10.1126/science.1105959. [DOI] [PubMed] [Google Scholar]
- 26.Sokan-Adeaga AA, Ana GREE, Sokan-Adeaga MA, Sokan-Adeaga ED, Ejike OM. Secondary inorganic aerosols: Impacts on the global climate system and human health. Biodiversity Int J. 2019;3:249–59. [Google Scholar]
- 27.Formenti P, Schütz L, Balkanski Y, Desboeufs K, Ebert M, Kandler K, Petzold A, Scheuvens D, Weinbruch S, Zhang D. Recent progress in understanding physical and chemical properties of African and Asian mineral dust. Atmos Chem Phys. 2011;11:8231–8256. [Google Scholar]
- 28.González-Flórez C, Klose M, Alastuey A, Dupont S, Escribano J, Etyemezian V, Gonzalez-Romero A, Huang Y, Kandler K, Nikolich G, et al. Insights into the size-resolved dust emission from field measurements in the Moroccan Sahara. Atmos Chem Phys. 2023;23:7177–7212. [Google Scholar]
- 29.Xing YF, Xu YH, Shi MH, Lian YX. The impact of PM2.5 on the human respiratory system. J Thorac Dis. 2016;8:E69–E74. doi: 10.3978/j.issn.2072-1439.2016.01.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Candeias C, Vicente E, Tomé M, Rocha F, Ávila P, Alves C. Geochemical, mineralogical and morphological characterisation of road dust and associated health risks. Int J Environ Res Public Health. 2020;17(1563) doi: 10.3390/ijerph17051563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wagner F, Bortoli D, Pereira S, Costa MJ, Maria Silva A, Weinzierl B, Esselborn M, Petzold A, Rasp K, Heinold B, Tegen IN. of dust aerosol particles transported to Portugal from the Sahara desert. Tellus B: Chem Phys Meteorol. 2009;61:297–306. [Google Scholar]
- 32.Mallios SA, Drakaki E, Amiridis V. Effects of dust particle sphericity and orientation on their gravitational settling in the earth's atmosphere. J Aerosol Sci. 2020;150(105634) [Google Scholar]
- 33.Zhang J, Shao Y. A new parameterization of particle dry deposition over rough surfaces. Atmos Chem Phys. 2014;14:12429–12440. [Google Scholar]
- 34.Lian S, Zhou L, Murphy DM, Froyd KD, Toon OB, Yu P. Global distribution of Asian, Middle Eastern, and North African dust simulated by CESM1/CARMA. Atmos Chem Phys. 2022;22:13659–13676. [Google Scholar]
- 35.Brook RD, Rajagopalan S, Pope CA III, Brook JR, Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA, et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation. 2010;121:2331–2378. doi: 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- 36.Kim KH, Kabir E, Kabir S. A review on the human health impact of airborne particulate matter. Environ Int. 2015;74:136–143. doi: 10.1016/j.envint.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 37.Li N, Hao M, Phalen RF, Hinds WC, Nel AE. Particulate air pollutants and asthma. A paradigm for the role of oxidative stress in PM-induced adverse health effects. Clin Immunol. 2003;109:250–265. doi: 10.1016/j.clim.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 38.Kelly FJ, Fussell JC. Size, source and chemical composition as determinants of toxicity attributable to ambient particulate matter. Atmos Environ. 2012;60:504–526. [Google Scholar]
- 39.Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014;383:1581–1592. doi: 10.1016/S0140-6736(14)60617-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schraufnagel DE. The health effects of ultrafine particles. Exp Mol Med. 2020;52:311–317. doi: 10.1038/s12276-020-0403-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Perez L, Tobias A, Querol X, Künzli N, Pey J, Alastuey A, Viana M, Valero N, González-Cabré M, Sunyer J. Coarse particles from Saharan dust and daily mortality. Epidemiology. 2008;19:800–807. doi: 10.1097/ede.0b013e31818131cf. [DOI] [PubMed] [Google Scholar]
- 42.Prospero JM, Blades E, Mathison G, Naidu R. Interhemispheric transport of viable fungi and bacteria from Africa to the Caribbean with soil dust. Aerobiologia. 2005;21:1–9. [Google Scholar]
- 43.Gyan K, Henry W, Lacaille S, Laloo A, Lamsee-Ebanks C, McKay S, Antoine RM, Monteil MA. African dust clouds are associated with increased paediatric asthma accident and emergency admissions on the Caribbean island of Trinidad. Int J Biometeorol. 2005;49:371–376. doi: 10.1007/s00484-005-0257-3. [DOI] [PubMed] [Google Scholar]
- 44.McElroy S, Dimitrova A, Evan A, Benmarhnia T. Saharan dust and childhood respiratory symptoms in Benin. Int J Environ Res Public Health. 2022;19(4743) doi: 10.3390/ijerph19084743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pope CA III, Dockery DW. Health effects of fine particulate air pollution: Lines that connect. J Air Waste Manag Assoc. 2006;56:709–742. doi: 10.1080/10473289.2006.10464485. [DOI] [PubMed] [Google Scholar]
- 46.Mortimer KM, Neas LM, Dockery DW, Redline S, Tager IB. The effect of air pollution on inner-city children with asthma. Eur Respir J. 2002;19:699–705. doi: 10.1183/09031936.02.00247102. [DOI] [PubMed] [Google Scholar]
- 47.Carrozzi L, Giuliano G, Viegi G, Paoletti P, Di Pede F, Mammini U, Carmignani G, Saracci R, Giuntini C, Lebowitz MD. The Po River Delta epidemiological study of obstructive lung disease: Sampling methods, environmental and population characteristics. Eur J Epidemiol. 1990;6:191–200. doi: 10.1007/BF00145793. [DOI] [PubMed] [Google Scholar]
- 48. Asthma and Allergy Foundation of America. Asthma facts and figures, 2020. Retrieved from https://www.aafa.org/asthma-facts/. [Google Scholar]
- 49.Mölter A, Simpson A, Berdel D, Brunekreef B, Custovic A, Cyrys J, de Jongste J, de Vocht F, Fuertes E, Gehring U, et al. A multicentre study of air pollution exposure and childhood asthma prevalence: The ESCAPE project. Eur Respir J. 2015;45:610–624. doi: 10.1183/09031936.00083614. [DOI] [PubMed] [Google Scholar]
- 50.Vodonos A, Friger M, Katra I, Avnon L, Krasnov H, Koutrakis P, Schwartz J, Lior O, Novack V. The impact of desert dust exposures on hospitalizations due to exacerbation of chronic obstructive pulmonary disease. Air Qual Atmos Health. 2014;7:433–439. [Google Scholar]
- 51.Kim CS, Hu SC. Regional deposition of inhaled particles in human lungs: Comparison between men and women. J Appl Physiol (1985) 1998;84:1834–1844. doi: 10.1152/jappl.1998.84.6.1834. [DOI] [PubMed] [Google Scholar]
- 52.Seaton A, MacNee W, Donaldson K, Godden D. Particulate air pollution and acute health effects. Lancet. 1995;345:176–178. doi: 10.1016/s0140-6736(95)90173-6. [DOI] [PubMed] [Google Scholar]
- 53.Fan W, Zlatnik MG. Climate change and pregnancy: Risks, mitigation, adaptation, and resilience. Obstet Gynecol Surv. 2023;78:223–236. doi: 10.1097/OGX.0000000000001116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sanders B, Davis M. Effects of climate change and air pollution on perinatal health. J Midwifery Womens Health. 2023;68:383–390. doi: 10.1111/jmwh.13522. [DOI] [PubMed] [Google Scholar]
- 55.Aguilera J, Konvinse K, Lee A, Maecker H, Prunicki M, Mahalingaiah S, Sampath V, Utz PJ, Yang E, Nadeau KC. Air pollution and pregnancy. Semin Perinatol. 2023;47(151838) doi: 10.1016/j.semperi.2023.151838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bongaerts E, Lecante LL, Bové H, Roeffaers MBJ, Ameloot M, Fowler PA, Nawrot TS. Maternal exposure to ambient black carbon particles and their presence in maternal and fetal circulation and organs: an analysis of two independent population-based observational studies. Lancet Planet Health. 2022;6:e804–e811. doi: 10.1016/S2542-5196(22)00200-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Seeni I, Ha S, Nobles C, Liu D, Sherman S, Mendola P. Air pollution exposure during pregnancy: Maternal asthma and neonatal respiratory outcomes. Ann Epidemiol. 2018;28:612–618.e4. doi: 10.1016/j.annepidem.2018.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Uwak I, Olson N, Fuentes A, Moriarty M, Pulczinski J, Lam J, Xu X, Taylor BD, Taiwo S, Koehler K, et al. Application of the navigation guide systematic review methodology to evaluate prenatal exposure to particulate matter air pollution and infant birth weight. Environ Int. 2021;148(106378) doi: 10.1016/j.envint.2021.106378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ciencewicki J, Jaspers I. Air pollution and respiratory viral infection. Inhal Toxicol. 2007;19:1135–1146. doi: 10.1080/08958370701665434. [DOI] [PubMed] [Google Scholar]
- 60.Becker S, Soukup JM, Sioutas C, Cassee FR. Response of human alveolar macrophages to ultrafine, fine, and coarse urban air pollution particles. Exp Lung Res. 2003;29:29–44. doi: 10.1080/01902140303762. [DOI] [PubMed] [Google Scholar]
- 61.Bredeck G, Dobner J, Rossi A, Schins RPF. Saharan dust induces the lung disease-related cytokines granulocyte-macrophage colony-stimulating factor and granulocyte colony-stimulating factor. Environ Int. 2024;186(108580) doi: 10.1016/j.envint.2024.108580. [DOI] [PubMed] [Google Scholar]
- 62.Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, Balakrishnan K, Brunekreef B, Dandona L, Dandona R, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: An analysis of data from the global burden of diseases study 2015. Lancet. 2017;389:1907–1918. doi: 10.1016/S0140-6736(17)30505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Anderson JO, Thundiyil JG, Stolbach A. Clearing the air: A review of the effects of particulate matter air pollution on human health. J Med Toxicol. 2012;8:166–175. doi: 10.1007/s13181-011-0203-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mazzarella G, Ferraraccio F, Prati MV, Annunziata S, Bianco A, Mezzogiorno A, Liguori G, Angelillo IF, Cazzola M. Effects of diesel exhaust particles on human lung epithelial cells: An in vitro study. Respir Med. 2007;101:1155–1162. doi: 10.1016/j.rmed.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 65.Diaz-Sanchez D, Tsien A, Fleming J, Saxon A. Combined diesel exhaust particulate and ragweed allergen challenge markedly enhances human in vivo nasal ragweed-specific IgE and skews cytokine production to a T helper cell 2-type pattern. J Immunol. 1997;158:2406–2413. [PubMed] [Google Scholar]
- 66.Nel A, Xia T, Mädler L, Li N. Toxic potential of materials at the nanolevel. Science. 2006;311:622–627. doi: 10.1126/science.1114397. [DOI] [PubMed] [Google Scholar]
- 67.Valavanidis A, Fiotakis K, Vlachogianni T. Airborne particulate matter and human health: Toxicological assessment and importance of size and composition of particles for oxidative damage and carcinogenic mechanisms. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev. 2008;26:339–362. doi: 10.1080/10590500802494538. [DOI] [PubMed] [Google Scholar]
- 68.Ghio AJ, Smith CB, Madden MC. Diesel exhaust particles and airway inflammation. Curr Opin Pulm Med. 2012;18:144–150. doi: 10.1097/MCP.0b013e32834f0e2a. [DOI] [PubMed] [Google Scholar]
- 69.Almeida-Silva M, Cardoso J, Alemão C, Santos S, Monteiro A, Manteigas V, Marques-Ramos A. Impact of particles on pulmonary endothelial cells. Toxics. 2022;10(312) doi: 10.3390/toxics10060312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pozzi R, De Berardis B, Paoletti L, Guastadisegni C. Inflammatory mediators induced by coarse (PM2.5-10) and fine (PM2.5) urban air particles in RAW 264.7 cells. Toxicology. 2003;183:243–254. doi: 10.1016/s0300-483x(02)00545-0. [DOI] [PubMed] [Google Scholar]
- 71.Becker S, Dailey LA, Soukup JM, Grambow SC, Devlin RB, Huang YCT. Seasonal variations in air pollution particle-induced inflammatory mediator release and oxidative stress. Environ Health Perspect. 2005;113:1032–1038. doi: 10.1289/ehp.7996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Thompson JE. Airborne particulate matter: Human exposure and health effects. J Occup Environ Med. 2018;60:392–423. doi: 10.1097/JOM.0000000000001277. [DOI] [PubMed] [Google Scholar]
- 73.Mar TF, Koenig JQ, Jansen K, Sullivan J, Kaufman J, Trenga CA, Siahpush SH, Liu LJ, Neas L. Fine particulate air pollution and cardiorespiratory effects in the elderly. Epidemiology. 2005;16:681–687. doi: 10.1097/01.ede.0000173037.83211.d6. [DOI] [PubMed] [Google Scholar]
- 74.Kelly FJ, Fussell JC. Linking ambient particulate matter pollution effects with oxidative biology and immune responses. Ann N Y Acad Sci. 2015;1340:84–94. doi: 10.1111/nyas.12720. [DOI] [PubMed] [Google Scholar]
- 75.O'Neill MS, Veves A, Zanobetti A, Sarnat JA, Gold DR, Economides PA, Horton ES, Schwartz J. Diabetes enhances vulnerability to particulate air pollution-associated impairment in vascular reactivity and endothelial function. Circulation. 2005;111:2913–2920. doi: 10.1161/CIRCULATIONAHA.104.517110. [DOI] [PubMed] [Google Scholar]
- 76.Ghio AJ, Devlin RB. Inflammatory lung injury after bronchial instillation of air pollution particles. Am J Respir Crit Care Med. 2001;164:704–708. doi: 10.1164/ajrccm.164.4.2011089. [DOI] [PubMed] [Google Scholar]
- 77.Li N, Sioutas C, Cho A, Schmitz D, Misra C, Sempf J, Wang M, Oberley T, Froines J, Nel A. Ultrafine particulate pollutants induce oxidative stress and mitochondrial damage. Environ Health Perspect. 2003;111:455–460. doi: 10.1289/ehp.6000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nunes C, Pereira AM, Morais-Almeida M. Asthma costs and social impact. Asthma Res Pract. 2017;3(1) doi: 10.1186/s40733-016-0029-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bredeck G, Busch M, Rossi A, Stahlmecke B, Fomba KW, Herrmann H, Schins RPF. Inhalable Saharan dust induces oxidative stress, NLRP3 inflammasome activation, and inflammatory cytokine release. Environ Int. 2023;172(107732) doi: 10.1016/j.envint.2023.107732. [DOI] [PubMed] [Google Scholar]
- 80.Jaspers I, Ciencewicki JM, Zhang W, Brighton LE, Carson JL, Beck MA, Madden MC. Diesel exhaust enhances influenza virus infections in respiratory epithelial cells. Toxicol Sci. 2005;85:990–1002. doi: 10.1093/toxsci/kfi141. [DOI] [PubMed] [Google Scholar]
- 81.Janssen NAH, Fischer P, Marra M, Ameling C, Cassee FR. Short-term effects of PM2.5, PM10 and PM2.5-10 on daily mortality in The Netherlands. Sci Total Environ. 2013;463-464:20–26. doi: 10.1016/j.scitotenv.2013.05.062. [DOI] [PubMed] [Google Scholar]
- 82.Grahame TJ, Klemm R, Schlesinger RB. Public health and components of particulate matter: The changing assessment of black carbon. J Air Waste Manag Assoc. 2014;64:620–660. doi: 10.1080/10962247.2014.912692. [DOI] [PubMed] [Google Scholar]
- 83.Beelen R, Hoek G, van den Brandt PA, Goldbohm RA, Fischer P, Schouten LJ, Jerrett M, Hughes E, Armstrong B, Brunekreef B. Long-term effects of traffic-related air pollution on mortality in a Dutch cohort (NLCS-AIR study) Environ Health Perspect. 2008;116:196–202. doi: 10.1289/ehp.10767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Delfino RJ, Sioutas C, Malik S. Potential role of ultrafine particles in associations between airborne particle mass and cardiovascular health. Environ Health Perspect. 2005;113:934–946. doi: 10.1289/ehp.7938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chow JC, Watson JG, Edgerton SA, Vega E. Chemical composition of PM2.5 and PM10 in Mexico City during winter 1997. Sci Total Environ. 2002;287:177–201. doi: 10.1016/s0048-9697(01)00982-2. [DOI] [PubMed] [Google Scholar]
- 86.Pope CA III, Burnett RT, Thun MJ, Calle EE, Krewski D, Ito K, Thurston GD. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA. 2002;287:1132–1141. doi: 10.1001/jama.287.9.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kelly FJ, Fussell JC. Air pollution and airway disease. Clin Exp Allergy. 2011;41:1059–1071. doi: 10.1111/j.1365-2222.2011.03776.x. [DOI] [PubMed] [Google Scholar]
- 88.Epton MJ, Dawson RD, Brooks WM, Kingham S, Aberkane T, Cavanagh JAE, Frampton CM, Hewitt T, Cook JM, McLeod S, et al. The effect of ambient air pollution on respiratory health of school children: A panel study. Environ Health. 2008;7(16) doi: 10.1186/1476-069X-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yang CY, Huang CC, Chiu HF, Chiu JF, Lan SJ, Ko YC. Effects of occupational dust exposure on the respiratory health of Portland cement workers. J Toxicol Environ Health. 1996;49:581–588. [PubMed] [Google Scholar]
- 90.Schwartz J, Dockery DW. Increased mortality in Philadelphia associated with daily air pollution concentrations. Am Rev Respir Dis. 1992;145:600–604. doi: 10.1164/ajrccm/145.3.600. [DOI] [PubMed] [Google Scholar]
- 91.Martinez FD. Genes, environments, development and asthma: A reappraisal. Eur Respir J. 2007;29:179–184. doi: 10.1183/09031936.00087906. [DOI] [PubMed] [Google Scholar]
- 92.Vichit-Vadakan N, Vajanapoom N. Health impact from air pollution in Thailand: Current and future challenges. Environ Health Perspect. 2011;119:A197–A198. doi: 10.1289/ehp.1103728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rehfuess E, Mehta S, Prüss-Ustün A. Assessing household solid fuel use: Multiple implications for the millennium development goals. Environ Health Perspect. 2006;114:373–378. doi: 10.1289/ehp.8603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bauer SE, Tsigaridis K, Miller RL. Significant atmospheric aerosol pollution caused by world food cultivation. Geophys Res Lett. 2016;43:5394–5400. [Google Scholar]
- 95.Dockery DW, Pope CA III. Acute respiratory effects of particulate air pollution. Annu Rev Public Health. 1994;15:107–132. doi: 10.1146/annurev.pu.15.050194.000543. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.