Abstract
Background
Column interruption duration (CID) is a noninvasive surrogate for venous refill time (VFT), a parameter used in ambulatory venous pressure measurement. CID is more accurate than invasive VFT measurement because it avoids errors involved with indirect access of the deep system through the dorsal foot vein. The aim of this retrospective single center study is to analyze the clinical usefulness of CID in assessment of chronic venous disease (CVD).
Methods
A total of 1551 limbs (777 patients) were referred with CVD symptoms over a 5-year period (2018-2023); CID, air plethysmography, and duplex reflux data were analyzed. Of these limbs, 679 had supine venous pressure data as well. The pathology was categorized as obstruction if supine peripheral venous pressure was >11 mm Hg and as reflux if duplex reflux time in superficial or deep veins was >1 second. CID was measured via Doppler monitoring of flow in the great saphenous vein (GSV) and one of the paired posterior tibial (PT) veins near the ankle in the erect posture. The calf is emptied by rapid inflation cuff. CID is the time interval in seconds when cephalad venous flow in great saphenous vein and posterior tibial veins reappear after calf ejection. A CID <20 seconds in either vein is abnormal similar to the threshold used in VFT measurement.
Results
Thirty-two percent of the limbs had obstruction, 17% had reflux, and 37% had a combination; 14% had neither. Higher clinical-etiology-anatomy-pathophysiology (CEAP) clinical classes (C4-6) were prevalent in 44% of pure reflux, significantly less (P < .0001) than in pure obstruction (73%) or obstruction plus reflux subsets (72%), partly reflecting distribution of pathology. There is a progressive increase in supine venous pressure and abnormal CID (P < .0001 and P < .0001, respectively) in successive CEAP clinical class. No such correlation between CEAP and any of the reflux severity grading methods (reflux segment score, Venous Filling Index, and Kistner axial grading) was observed. Abnormal CID (55%) was more prevalent in higher CEAP classes (>4) (P < .0001) than in lesser clinical classes (0-2) or limbs with neither obstruction nor reflux (P < .01).
Conclusions
Obstruction seems to be a more dominant pathology in clinical progression among CEAP clinical classes than reflux. CID is abnormal in both obstructive and refluxive pathologies and may represent a common end pathway for similar clinical manifestations (eg, ulcer). These data suggest a useful role for CID measurement in clinical assessment of limbs with CVD.
Keywords: Ambulatory venous pressure, Column interruption duration, CID, Venous pressure, Venous reflux, Venous obstruction
Article Highlights.
-
•
Type of Research: Single-center retrospective analysis of prospectively collected data in a large cohort with chronic venous disease (CVD)
-
•
Key Findings: The pathology of 1551 limbs with CVD (679 with pressure data) were analyzed. Clinical-etiology-anatomy-pathophysiology (CEAP) class was strongly correlated to obstruction but not reflux. Column interruption duration, a noninvasive measure of ambulatory venous pressure, was shortened in both obstruction and reflux correlating with CEAP class.
-
•
Take Home Message: Measurement of supine venous pressure and column interruption duration are useful investigatory tools in limbs with CVD to define pathology. Obstruction is more dominant than reflux in CEAP class hierarchy.
Column interruption duration (CID) is a noninvasive measure of ambulatory venous pressure (AMVP).1 The importance of AMVP as a global index of calf pump function was recognized early with the discovery of the unique venous pressure changes that occur in superficial and deep veins in the calf with ambulation.2 Clinical measurement of AMVP however was not easy because of difficulty and risks of access, particularly of deep veins (eg, posterior tibial [PT] vein). This difficulty was eased somewhat with the proposition that dorsal foot venous pressure access can reflect deep venous pressure dynamics.3, 4, 5, 6 Clinical measurement of AMVP in patients with chronic venous disease (CVD) in the last four decades have mostly used this technique for AMVP measurement. It is now known that the pressure profile in the dorsal foot vein is different from that in deep veins and also from the great saphenous vein (GSV).7,8 This is due to differences in capacitance, compliance, and variable compartmentalization of the segments by order of valve closure during pressure recovery.
It has been known that the decrease in the pressures in the GSV and the PT vein with calf exercise is related to closure of a key valve or valves in these veins at or below the knee.4,9 We now know that these key valves are more caudally located than previously thought; they are positioned in the saphenous and PT veins in the lower one-third of the leg.1 The closure of these key valves is accompanied by tube collapse (deflation) of the veins below the closed valves. This process results in a steep decrease in the venous pressures in the collapsed segments lasting a period of ≥20 seconds until refill from inflow restores pressure and flow. Measured AMVP parameters are known as percentage drop and venous refill time (VFT). A percent decrease of ≥50% and a VFT of ≥20 seconds is considered normal. The VFT is more important than percent drop because it is abnormal thrice more often than the percent drop in limbs with CVD and is abnormal in all but 4% of limbs with abnormal percent drop.10 Axial flow in the great saphenous and PT veins is interrupted until there is full recovery of pressure from inflow. There is segmentation of the venous column during the period of tube collapse below the closed key valves. The resumption of flow in the axial veins (GSV and PT veins) indicates the end of column interruption and corresponds with pressure recovery. We showed in an earlier publication that the CID in the great saphenous and PT veins can be measured noninvasively by monitoring flow resumption in these veins via duplex doppler after calf emptying is accomplished with rapid inflation/deflation cuffs. CID is thus a noninvasive surrogate for the VFT parameter in AMVP.1
The aim of this retrospective, single-center study is to analyze the clinical usefulness of CID in the assessment of a large cohort of patients with symptoms of CVD referred to our tertiary center for evaluation; peripheral venous pressure measurement and duplex examination for reflux are used respectively to identify obstruction and reflux in the patient cohort.
Methods
Patients
A total of 1551 limbs (777 patients) with symptoms of CVD referred to our institution over a 5-year period (2018-2023) were analyzed.
Normal volunteers
Normal values obtained from 32 limbs in 16 healthy volunteers without clinical history or manifestation of venous disease were used as controls for comparison.
Clinical assessment
Patients underwent CVD-oriented clinical evaluation and investigations for assessment of reflux and obstruction in the symptomatic limb. The information provides pathology the “P” component in the clinical-etiology-anatomy-pathophysiology (CEAP) classification. Investigations for reflux included Duplex examination and air plethysmography (APG). Obstruction was assessed by measurement of supine venous pressure, which is a more objective parameter than phasic variations in flow assessed by duplex. CID measurements were routinely carried out in all patients.1
Duplex examination for reflux
Patients were examined for reflux in the erect position using rapid inflation/deflation cuffs (Hokanson, Bellevue, WA) as previously described.11 A segmental score was derived when reflux was present. One point was awarded for each of the following vein segments when reflux was present: GSV, small saphenous, femoral, profunda femoris, popliteal, PT, and perforator veins. The maximum score of 7 was obtained when all the named segments were refluxive.11 Reflux was also classified by Kistner's Axial reflux grading: grade 0, no reflux; grade 1, reflux to the thigh; grade 2, reflux below the knee; and grade 3, reflux to the ankle.
Air plethysmography
A commercially available instrument (ACI Medical, San Diego, CA) was used. Plethysmographic parameters were obtained per the protocol described by Christopoulos.12 A venous filling index VFI90 of >2.3 mL/second was considered abnormal.
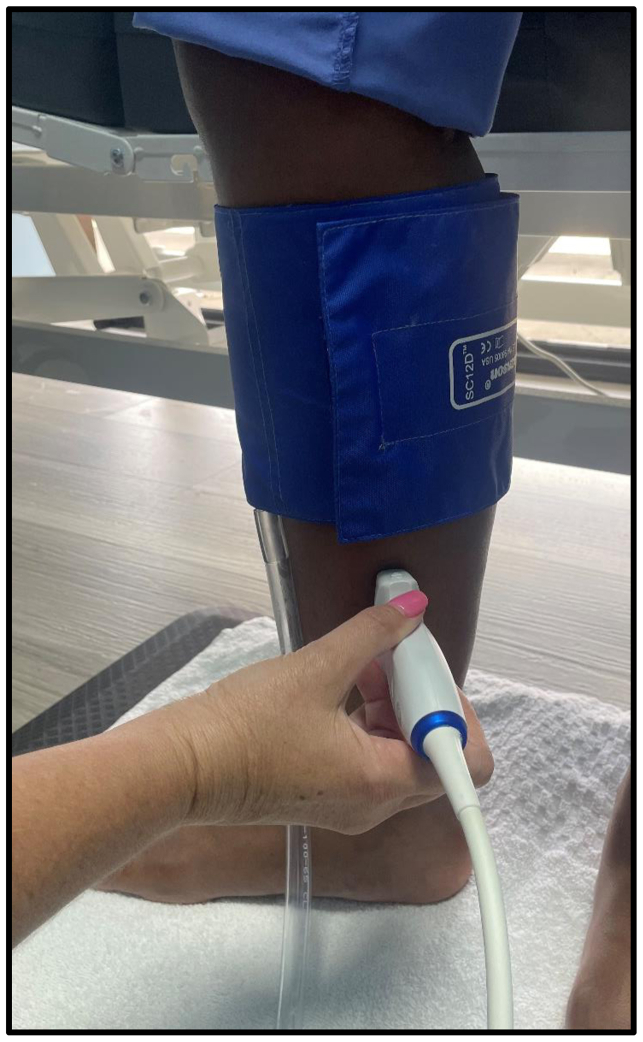
CID measurement
CID was measured in the erect position as previously described.1 Briefly, calf emptying was obtained by rapid inflation cuffs pressurized to 110 mm Hg. This is known to empty the calf as well as or better than the traditional 10 toe stands. All flow in the PT vein and GSV cease with column interruption. Calf emptying results in tube collapse (disinflation) of the calf veins. Duplex monitoring of GSV and one of the paired PT veins above the ankle shows cessation of flow which can last ≤2 minutes in healthy limbs. Resumption of flow indicates column restoration (Fig 1). Pressure recovery and flow restoration are coincident; the latter is, therefore, a noninvasive surrogate for VFT, a parameter used in AMVP measurement. A CID of <20 seconds in either the GSV or the PT vein is considered abnormal as used in VFT measurement. CID abnormality was graded similar to VFT: mild, 16 to 20 seconds; moderate, 10 to 15 seconds; and severe, <10 seconds. CID can be different in the GSV and PT veins and the shorter one can pressurize the ankle skin before the other. The shorter of the two CID values is chosen as the key CID value.
Fig 1.
Column interruption duration (CID) measurement. The calf muscles are emptied by rapid inflation of a cuff placed around the calf to 110 mm Hg. Resumption of flow in the great saphenous vein (GSV) and the posterior tibial (PT) vein is timed with a duplex probe; a hockey stick works best with GSVD, whereas a linear probe is best for the tibial vein. Resumption of flow indicates end of postejection column segmentation. Normal CID may extend to ≥2 minutes. A CID of <20 seconds is considered abnormal similar to the threshold used in venous refill time (VFT) measurement. See text.
Pressure measurement
Supine venous pressure was measured through a vein in the calf or foot with the subject in the recumbent position; the transducer was level with the midaxillary line. A supine venous pressure of ≥11 mm Hg was considered abnormal and indicative of obstructive pathology.
Statistics
Prospectively entered data were retrieved from an electronic medical records program for retrospective analysis. A commercially available statistics package was used (PRISM; www.graphpad.com). A two-tailed t test (nonparametric) was used for continuous and the χ2 test for categorical data. Spearman's correlation coefficient was used for comparison of reflux assessment parameters. Informed consent was obtained from patients and volunteers. Institutional review board permission for data acquisition, analysis, and publication of deidentified data was granted.
Results
The demographics of the patients and healthy volunteers are shown in Table I. There were no significant differences in patient characteristics of pathologic subsets. Pathology detail and CEAP distribution is shown in the bottom of Table I.
Table I.
Demographics
| Parameters | Normal volunteers (n = 32) | Limbs with CVD (n = 1551) |
|---|---|---|
| Age (median, range) | 31 (20-43) | 59 (17-76) |
| Laterality L:R | 1:1 | 1:1 |
| Gender M:F | 7:9 | 1:2 |
| Limbs with CVD with supine venous pressure and duplex positive for reflux (n = 679) | ||||
|---|---|---|---|---|
| CEAP clinical class | Obstruction only: 32% (n = 214) | Reflux only: 17% (n = 117) | Both obstruction and reflux: 37% (n = 254) | Neither obstruction nor reflux: 14% (n = 94) |
| C 0-1 | 8% (n = 17) | 22% (n = 26) | 6% (n = 15) | 11% (n = 10) |
| C2 | 4% (n = 8) | 11% (n = 13) | 6% (n = 14) | 12% (n = 11) |
| C3 | 16% (n = 34) | 22% (n = 26) | 17% (n = 43) | 14% (n = 13) |
| C4 | 64% (n = 136) | 40% (n = 47) | 63% (n = 160) | 62% (n = 58) |
| C5 | 3% (n = 6) | 2% (n = 2) | 4% (n = 11) | 1% (n = 1) |
| C6 | 6% (n = 13) | 3% (n = 3) | 4% (n = 11) | 1% (n = 1) |
| C4-6 | 72% (n = 155) | 44% (n = 52) | 72% (n = 182) | 64% (n = 60) |
CVD, Chronic venous disease.
Boldface entries indicate statistical significance.
Pure reflux pathology was found in 17% of the limbs with CVD. The prevalence of pure obstruction (32%) and combined obstruction and reflux (37%) was roughly twice as common as pure reflux (P < .0001). Neither reflux nor obstruction was found in 14% of limbs referred with CVD-like symptoms.
The distribution of CEAP clinical classes was different among the pathologic subsets: obstruction and combined obstruction reflux pathologies had significantly greater prevalence of higher CEAP classes (≥C4); prevalence of (C4 + C5 + C6) in these subsets (72% and 72%, respectively) were each higher than the prevalence (44%) in pure reflux pathology (P < .0001). Ninety-four limbs (14%) that had neither obstruction or reflux as defined had the following CEAP distribution: 21 limbs had reticular veins or varices and 13 limbs had leg swelling; 58 limbs, or <0.1% of total limbs (n = 1551) had CEAP class 4 manifestations without obstruction or reflux as defined.
CID in normal and limbs with CVD
CID detail in normal volunteers and pathologic subsets are shown in Table II. CID (either of the GSV or PT vein) was shortened in 14 of 32 normal limbs (44%). The mean CID values were moderately abnormal (10-15 seconds). Supine venous pressure was not measured in the current set of volunteers because prior data were available.
Table II.
Supine venous pressure and CID data in normal limbs and limbs with CVD
| Group | % (n) | Supine pressure, mean ± SD | Abnormal GSV CID |
Abnormal PT CID |
Abnormal CID (GSV and/or PT)a |
|||
|---|---|---|---|---|---|---|---|---|
| Abnormal prevalence, -% (n) | Mean ± SD | Abnormal prevalence, -% (n) | Mean ± SD | Abnormal prevalence, -% (n) | Mean ± SD | |||
| Normal volunteers | 100% (n = 32) | – | 34% (n = 11) | 10 ± 5.9 | 22% (n = 7) | 13.3 ± 2.8 | 44% (n = 14) | 10.6 ± 5.7 |
| Limbs with CVD (n = 679) | ||||||||
| Obstruction onlyb | 32% (n = 214) | 16.9 ± 4.3 | 50% (n = 107) | 7.1 ± 6.7 | 33% (n = 71) | 7.5 ± 6.3 | 53% (n = 114) | 7.0 ± 6.6 |
| Reflux only | 17% (n = 117) | 7.2 ± 2.7 | 51% (n = 60) | 4.8 ± 6.0 | 27% (n = 32) | 7.1 ± 6.4 | 62% (n = 72) | 5.3 ± 6.4 |
| Both obstruction and reflux | 37% (n = 254) | 16.7 ± 3.9 | 47% (n = 119) | 6.7 ± 6.2 | 36% (n = 91) | 9.6 ± 6.3 | 59% (n = 149) | 6.8 ± 6.4 |
| Neither obstruction nor reflux | 14% (n = 94) | 7.9 ± 2.2 | 35% (n = 33) | 4 ± 5.6 | 23% (n = 22) | 7.9 ± 5.9 | 40% (n = 38) | 4.8 ± 6.1 |
CID, Column interruption duration; CVD, chronic venous disease; GSV, great saphenous vein; PT, posterior tibial; SD, standard deviation.
Bold indicates significance. See text for P values.
Lower of the two CID values between GSV and PT veins.
Supine venous pressure ≥11 mm Hg.
The peripheral venous pressure was elevated (>11 mm Hg), by definition, in limbs with pure obstruction or combined obstruction and reflux. The mean peripheral venous pressure was normal at 7.2 and 7.9 mm Hg, respectively, in limbs with pure reflux and those when neither obstruction nor reflux could be identified.
CID was abnormal in the majority of limbs with obstruction, reflux, or both. Shortened CID prevalence (either GSV or PT) was high ranging from 53% to 62% in limbs with obstructive, refluxive or combined pathology; prevalence in these pathological subsets was higher (P < .01) than in limbs with neither obstruction nor reflux pathology. The mean CID values were in the severe category (<10 seconds) in all foregoing subsets. A shortened CID in GSV was more prevalent than in the PT vein in both normal and patient subsets shown in Table II.
CEAP clinical classes and pathology
Obstruction seemed to have a stronger correlation with CEAP clinical class than reflux (Table III). There is a progressive increase in the prevalence of peripheral venous hypertension (>11 mm Hg) with each successive CEAP clinical class, starting with 47% in CEAP classes 0 and 1, increasing stepwise to 86% in clinical class 6 (P < .0001). A similar trend is seen in the prevalence of abnormal CID (either GSV or PT), increasing from 41% in CEAP classes 0 or 1 to 70% in CEAP class 6 (P < .0001). The relationship of CEAP class to reflux severity is weaker and random. The values for the three reflux grading methods shown (reflux segment score, VFI90, and Kistner axial grading) are spread out among CEAP classes with no clear pattern.
Table III.
Supine venous pressure, reflux severity and column interruption duration (CID) data in limbs with chronic venous disease (CVD)
| CEAP clinical class | Obstructive limbs n = 679a,b |
Limbs with CVD n = 1551 |
|||||
|---|---|---|---|---|---|---|---|
| Prevalence of supine venous pressure ≥11 mm Hg, % (n) | Supine pressure in obstructive limbs, mean ± std. dev. | Reflux segmental score, median (range) | VFI90, mean ± std. dev. | Kistner axial grading, median (range) | Prevalence of abnormal CID (GSV and/or PT), % (n) | Abnormal CID value, mean ± std. dev. | |
| C0-1 | 47% (n = 68) | 15.8 ± 4 | 1 (0-6) | 1.1 ± 1.6 | 0 (0-3) | 41% (n = 167) | 5.7 ± 6.6 |
| C2 | 48% (n = 46) | 14.9 ± 3.9 | 1 (0-6) | 2.6 ± 9.6 | 0 (0-3) | 38% (n= 86) | 5.4 ± 7.0 |
| C3 | 66% (n = 116) | 17.2 ± 3.4 | 1 (0-6) | 1.7 ± 3.9 | 0 (0-3) | 46% (n = 275) | 5.3 ± 6.3 |
| C4 | 74% (n = 401) | 16.9 ± 4.2 | 1 (0-7) | 1.4 ± 2.6 | 0 (0-3) | 53% (n = 919) | 5.6 ± 6.4 |
| C5 | 85% (n = 20) | 16.2 ± 3.2 | 1 (0-6) | 3.7 ± 2.3 | 0 (0-3) | 73% (n = 51) | 4.6 ± 5.7 |
| C6 | 86% (n = 28) | 16.9 ± 4.1 | 1 (0-7) | 2.8 ± 2.6 | 0 (0-3) | 70% (n = 53) | 4.5 ± 5.6 |
| C4-6 | 75% (n = 449) | 16.9 ± 4.2 | 1 (0-6) | 1.9 ± 3.3 | 0 (0-3) | 55% (n = 1023) | 5.4 ± 6.3 |
CEAP, Clinical-etiology-anatomy-pathophysiology; CID, column interruption duration; CVD, chronic venous disease; GSV, great saphenous vein; PT, posterior tibial.
Boldface entries indicate statistical significance. See text for P values.
There is a trend for progressive increase of supine venous hypertension (≥11 mm Hg) as well as shortened CID in limbs with CVD (P < .0001).
Subset of total limbs with CVD with supine venous pressure data.
Discussion
CID is a noninvasive surrogate for VFT, a parameter used in AMVP measurement. CID differs between GSV and PT veins and the values are measured separately. The lower of the two is the critical value as either can pressurize the skin in the gaiter area. CID is more accurate than invasive VFT measurement because it avoids errors involved with indirect access of the deep system through the dorsal foot vein.1 We report herein CID data in 32 normal limbs (controls) and 1551 limbs with CVD seen in our tertiary center over a 5-year period.
The pathology in the dataset was categorized as obstruction, reflux, or a combination based on elevated supine venous pressure (≥11 mm Hg), indicating obstruction, and duplex reflux time to identify reflux. Pure reflux was present in 17% of the limbs, whereas obstruction and combined obstruction and reflux were nearly twice as common (32% and 37%, respectively). The dominant prevalence of these pathologies in advanced CEAP classes (C4-C6) seem to roughly mirror their prevalence ratios in the overall dataset (ie, reflux is less common than pure obstruction or obstruction/reflux combination in higher (C>4) CEAP classes (Table I). Reflux and obstruction seem to shorten CID nearly the same without any such proportional difference in prevalence (Table II). CID may be the end mechanism in both pathologies that results in advanced CEAP clinical manifestations. However, obstruction and reflux impact CID by different mechanisms.
The prevalence of obstruction (supine venous pressure of ≥11 mm Hg) was noted to increase progressively with each successive CEAP class (Table III) starting at 47% for CEAP classes 0 and 1 ending with a high of 86% for C6 (P < .0001). Even though it has been known that the prevalence of obstruction in CVD had been underestimated in the past, the progressive increase of obstruction with each CEAP clinical class is a novel finding.13,14 In contrast, a correlation between reflux severity and CEAP clinical class if any was not apparent. Reflux severity was assessed by three different techniques: reflux segment score, VFI90 with APG, and Kistner's axial reflux grading; these values were widely spread out over CEAP clinical classes with no clear pattern.
CID abnormalities in normal limbs
The CID was abnormal in 44% of asymptomatic normal limbs (silent) included in this report. Presence of silent reflux or obstruction in asymptomatic limbs is well-known.15, 16, 17 This factor had been explained as an example of permissive pathology common in human disease.
Position of key valves
Invasive pressure measurement in the GSV and popliteal vein had shown only minor changes during calf exercise while pressure variations were more profound in the superficial and deep veins at the ankle level.4,18 This led to the assumption that the key valves controlling the calf pump were located below the knee level. Recent studies using doppler localization indicate that the position of key valve or valves is closer to the ankle than the knee.1 This was surmised by Sumner and colleagues on teleological grounds.19,20 The PT vein hosts numerous (≥40) closely spaced valves around the ankle; the GSV in the lower calf has approximately four valves.19,21 Findings from the current study confirm the pathophysiologic importance of the distal GSV and tibial valves located near the ankle. They are functionally more important than the proximal valves in the upper thigh (saphenofemoral and femoral valves). Measuring reflux times in the latter valves is the major focus of duplex examination in current clinical practice.
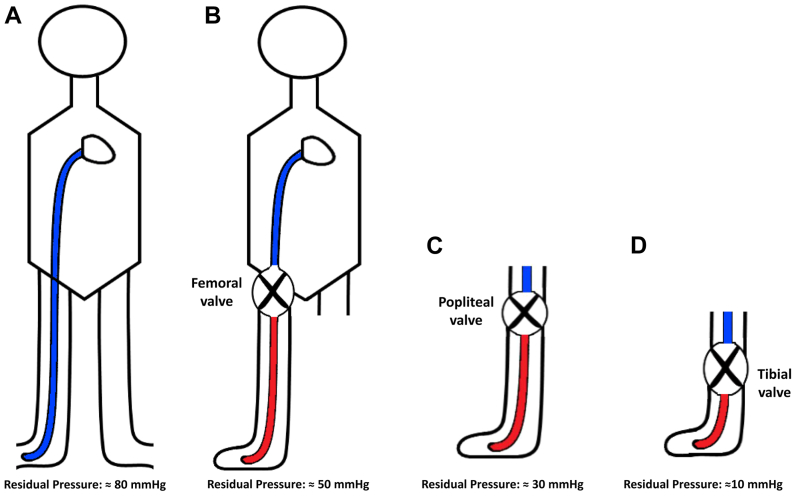
Level of column interruption
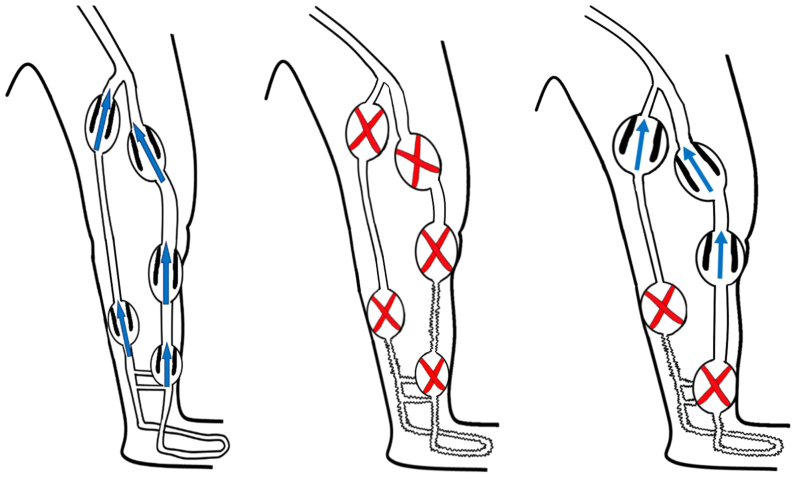
There is quasisteady venous flow in the lower limb in the erect resting posture. All the venous valves are open in this state. There is rapid ejection of blood in cephalad direction in both superficial and deep veins when there is calf muscle contraction.22,23 There is transient brief reversal of flow (physiological reflux) at the end of ejection, which helps to close the valves owing to the Venturi effect.24 A reflux duration of ≤0.5 seconds in the superficial veins and 1 second in the deep system is considered physiological. The valves remain closed for a variable period of time after closure depending upon their location. A longer duration of reflux is pathological and will shorten the duration of the VFT. Venous flow in the GSV and the tibial veins cease when the key valves are closed, and there is physiological segmentation of the venous column until the valves reopen to allow flow to resume. The saphenofemoral and femoral valves reopen first (Fig 2), followed a few seconds later by the popliteal valve and the adjoining mid GSV valve near the knee. The group of key valves in the PT vein and the adjacent saphenous valves near the ankle remain closed the longest and are among the last to reopen (≤120 seconds in healthy limbs). The level of column segmentation at the femoral or knee level is brief and associated with higher residual pressure at the foot level. Column segmentation near the ankle level persists the longest after calf pump action and is associated with lower postejection pressures at the foot level (Fig 3). Thus, column segmentation at the ankle level is longer lasting and produces lower postexercise foot venous pressure than segmentation at the groin or popliteal level.
Fig 2.
Illustration of the sequence of valve closure and reopening with calf pump action. There is phasic flow upward in the erect limb in the resting state with all the valves open (left). There is emptying of the calf veins with calf pump contraction. All of the valves in the axial veins (great saphenous vein [GSV] and posterior tibial [PT] vein) close (middle), but reopen in a certain sequence. The femoral and saphenofemoral valves open first approximately 8 seconds after closure. This is quickly followed by the popliteal valve and the nearby valve in the GSV at approximately 12 seconds after closure. The upper tibial valves and the valve in the gastrocnemius vein open next. There is resumption of flow in the thigh and upper calf at this stage. The lower segment of the PT veins and the adjacent portion of the GSV near the ankle remain collapsed without flow (right). Multiple valves in these segments maintain the collapsed state protecting the vulnerable gaiter area from the high hydrostatic pressure in the erect posture for a period of ≥2 minutes (column interruption duration [CID]) in healthy limbs before flow and pressure are restored. The duration distal venous collapse as measured by CID is the key hemodynamic parameter in chronic venous disease (CVD). See text.
Fig 3.
Column segmentation and residual foot venous pressure associated with valve closure at the femoral, popliteal and tibial valves near the ankle. (A) The resting foot venous pressure is approximately 80 mm Hg in an erect individual of normal height. The hydrostatic column pressure is largely responsible for the high pressure. (B) Column segmentation resulting from femoral valve closure results in a foot venous pressure of approximately 50 mm Hg represented by the residual column height (C) Column segmentation resulting from popliteal valve closure results in a foot venous pressure of approximately 30 mm Hg. (D) The lowest foot venous pressure (approximately 10 mm Hg) results from closure of distal tibial and great saphenous vein (GSV) valves near the ankle. They also provide the longest column interruption duration (CID) compared with proximal valves. See text.
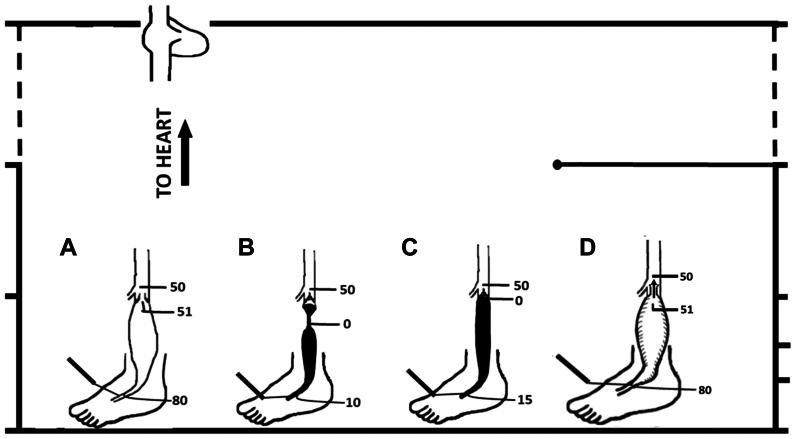
CID and calf pump mechanics
The fluid mechanics of postejection valve closure and their reopening is more complex than it seems at first sight (Fig 4).25 The emptying of calf veins with calf contraction simultaneously with the closure of key valves controlling the calf pump results in their transient partial collapse. Some residual volume may remain, which tends to pool near the lower part of the segment owing to gravity. Flow into the collapsed segments occurs from venous outflow from the surrounding musculature. The residual venous column gradually grows in height and touches the closed valve. The pressure at the top of the column is zero, and the pressure immediately above the closed key valve is approximately 50 mm Hg, representing the hydrostatic column extending from the closed key valve to the heart. The column height below the closed valve at this stage is at the maximum; no further increment in pressure can be obtained by growth in column height. However, inflow into the segment below the key valve from the capillaries (approximately 120 mm Hg pressure in the erect position) will gradually inflate the closed segment like a balloon, ultimately reaching a level to reopen the valve and resume venous flow. Thus, compliance (wall property) and capacitance of the superficial and deep veins of the calf influence CID measurement. CID in the PT vein is different from that in the adjoining saphenous vein due to differences in segment size, compliance, and inflow.1 Therefore, CID should be measured separately in these two vein segments because either can pressurize the ankle skin.
Fig 4.
The hemodynamics of valve closure and reopening of key axial valves in the lower leg with calf pump action is more complex than it would seem at first. (A) There is phasic venous flow through open valves in the resting erect limb. The pressure differential above and below the key valve is <1 mm Hg. (B) The key valve closes after calf pump ejection. The vein segment collapses below the closed valve largely emptied of blood. A residual foot venous pressure of approximately 10 to 20 mm Hg may be recorded at this stage. The column pressure at the top of the column is 0 mm Hg, whereas the pressure immediately above the closed key valve is approximately 50 mm Hg representing the column pressure above the closed valve. (C) The residual column in the collapsed segment will gradually grow in height from venous flow from the surrounding musculature eventually touching the closed key valve. The pressure at the top of the column immediately below the valve is still 0 mm Hg, unable to reopen the valve. No further increment in column height and related pressure is possible. (D) An increase in the segment pressure below the closed valve now occurs from a different mechanism: continuing venous inflow into the segment occurs distending the segment and increasing segment pressure from increasing wall tension. The increment in distending pressure will eventually reach high enough level to reopen the closed key valve and restore flow. See text.
Any reflux present in the key controlling valves will shorten their respective CIDs. CID in obstruction may be shortened from a different mechanism-poor calf emptying due to obstruction or because capacitance/compliance is decreased from post-thrombotic changes. Fig 5 illustrates reflux and obstruction interacting with capacitance/compliance of the distal superficial and deep axial vein segments in different ways to produce the same result-shortened CID. Arterial inflow from the arteriolar network that refills the calf pump is controlled by arteriolar tone. It is largely uninfluenced by calf pump pressure except where arteriolar-venous reflux is present.11 VFI90 (2.3 mL/second) represents normal ‘arterial inflow’ in the absence of reflux.12 This value will be increased when reflux is present to add to the volume that refills the calf pump after ejection.
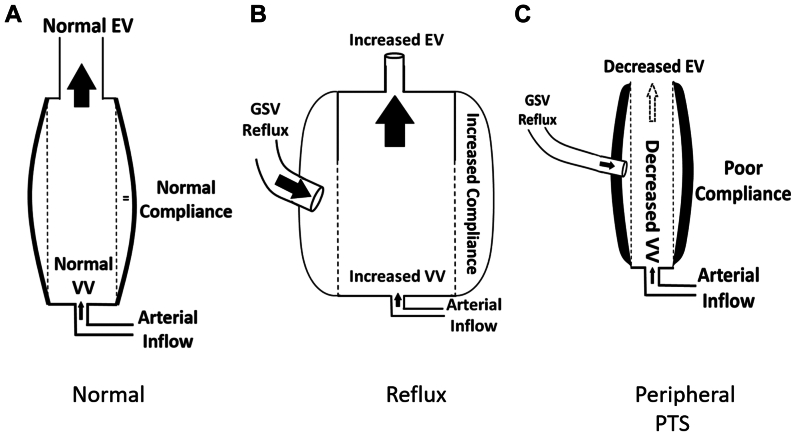
Fig 5.
(A) Normal column interruption duration (CID) in a calf with normal compliance, capacitance (VV) and ejection volume (EV) is related to normal inflow from the capillary network. (B) There is compensatory increase in VV and EV when pathologic reflux is present. The compliance may be increased as well in the bending regimen of tube mechanics. (C) Post-thrombotic syndrome (PTS) involving veins in the calf will lead to decreased VV, poor compliance, and decreased EV. This will decrease CID independent of any reflux present. This is because “arterial inflow” is largely unaffected by calf pump pressure. ie there is no compensatory increase in “arterial inflow” after poor ejection. See text.
Conclusions
CID is a noninvasive measure of AMVP, specifically the VFT parameter. CID is probably a truer reflection of calf pump dynamics than pressure measurement in the dorsal foot vein. The latter may be inaccurate owing to variable flow dynamics during pressure recovery in interconnected valved conduits. CID should be measured with a Doppler probe separately in the GSV and PT veins near the ankle after the calf pump is emptied; the lower of the two is the key value. The presence of obstructive pathology in limbs with CVD can be objectively identified by peripheral venous pressure measurement in the supine position. A pressure of ≥11 mm Hg indicates obstruction. The prevalence of obstruction progressively increases with each higher CEAP clinical class. The prevalence of shortened CID (normal is >20 seconds) is higher and the mean CID value lower in limbs with either reflux or obstruction. The prevalence of shortened CID also increases with each successive CEAP clinical class reaching a high of 70% to 73% in CEAP classes 4, 5, and 6. Severely shortened CID from reflux, obstruction, or a combination may be a common pathway for tissue damage and skin ulceration in advanced CID.
CID seems to be more important than the traditional valve reflux time in clinical assessment of CVD. This is the initial first analysis of CID in the clinical context. A fundamental parameter of this nature will require further analysis of differing clinical contexts (eg, obesity), including treatment outcomes etc. CID seems to be a basic measurement in CVD; its diagnostic usefulness and its role in assessing treatment outcome remains to be evaluated.
Author Contributions
Conception and design: SR
Analysis and interpretation: SR, AJ
Data collection: DT, OB, HP
Writing the article: SR, DT, OB, HP
Critical revision of the article: SR, AJ
Final approval of the article: SR, DT, OB, HP, AJ
Statistical analysis: SR, DT, HP
Obtained funding: SR
Overall responsibility: SR
Funding
All research is self-funded by The RANE Center.
Disclosures
S.R. reports US Patent for Venous Stent Design and IVUS Diagnostics. The remaining authors have no competing interests.
Footnotes
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Raju S., Walker W., May C. Measurement of ambulatory venous pressure and column interruption duration in normal volunteers. J Vasc Surg Venous Lymphat Disord. 2020;8:127–136. doi: 10.1016/j.jvsv.2019.06.012. [DOI] [PubMed] [Google Scholar]
- 2.Hojensgard I.C., Sturup H. Venous pressure in primary and postthrombotic varicose veins. Acta Chir Scand. 1948;99:133–153. [Google Scholar]
- 3.Arnoldi C. Incompetent communicating veins of the lower leg. Danish Medical Bulletin. 1958;5:65–71. [PubMed] [Google Scholar]
- 4.Arnoldi C. Venous pressure in the leg of healthy human subjects at rest and during muscular exercise in the nearly erect position. Acta Chir Scand. 1965;130:570–583. [PubMed] [Google Scholar]
- 5.Arnoldi C.C., Greitz T., Linderholm H. Variations in cross sectional area and pressure in the veins of the normal human leg during rhythmic muscular exercise. Acta Chir Scand. 1966;132:507–522. [PubMed] [Google Scholar]
- 6.Nicolaides A.N., Zukowski A.J. The value of dynamic venous pressure measurements. World J Surg. 1986;10:919–924. doi: 10.1007/BF01658640. [DOI] [PubMed] [Google Scholar]
- 7.Neglen P., Raju S. Differences in pressures of the popliteal, long saphenous, and dorsal foot veins. J Vasc Surg. 2000;32:894–901. doi: 10.1067/mva.2000.110351. [DOI] [PubMed] [Google Scholar]
- 8.Neglen P., Raju S. Ambulatory venous pressure revisited. J Vasc Surg. 2000;31:1206–1213. doi: 10.1067/mva.2000.105669. [DOI] [PubMed] [Google Scholar]
- 9.Ludbrook J. Functional aspects of the veins of the leg. Am Heart J. 1962;64:706–713. doi: 10.1016/0002-8703(62)90257-0. [DOI] [PubMed] [Google Scholar]
- 10.Raju S., Knepper J., May C., Knight A., Pace N., Jayaraj A. Ambulatory venous pressure, air plethysmography, and the role of calf venous pump in chronic venous disease. J Vasc Surg Venous Lymphat Disord. 2019;7:428–440. doi: 10.1016/j.jvsv.2018.08.009. [DOI] [PubMed] [Google Scholar]
- 11.Raju S., Knight A., Lamanilao L., Pace N., Jones T. Peripheral venous hypertension in chronic venous disease. J Vasc Surg Venous Lymphat Disord. 2019;7:706–714. doi: 10.1016/j.jvsv.2019.03.006. [DOI] [PubMed] [Google Scholar]
- 12.Christopoulos D.G., Nicolaides A., Szendro G., Irvine A.T., Bull M.L., Eastcott H.H. Air-plethysmography and the effect of elastic compression on venous hemodynamics of the leg. J Vasc Surg. 1987;5:148–159. doi: 10.1067/mva.1987.avs0050148. [DOI] [PubMed] [Google Scholar]
- 13.Labropoulos N., Volteas N., Leon M., et al. The role of venous outflow obstruction in patients with chronic venous dysfunction. Arch Surg. 1997;132:46–51. doi: 10.1001/archsurg.1997.01430250048011. [DOI] [PubMed] [Google Scholar]
- 14.Neglen P., Thrasher T.L., Raju S. Venous outflow obstruction: an underestimated contributor to chronic venous disease. J Vasc Surg. 2003;38:879–885. doi: 10.1016/s0741-5214(03)01020-6. [DOI] [PubMed] [Google Scholar]
- 15.Kibbe M.R., Ujiki M., Goodwin A.L., Eskandari M., Yao J., Matsumura J. Iliac vein compression in an asymptomatic patient population. J Vasc Surg. 2004;39:937–943. doi: 10.1016/j.jvs.2003.12.032. [DOI] [PubMed] [Google Scholar]
- 16.Labropoulos N., Delis K.T., Nicolaides A.N. Venous reflux in symptom-free vascular surgeons. J Vasc Surg. 1995;22:150–154. doi: 10.1016/s0741-5214(95)70109-5. [DOI] [PubMed] [Google Scholar]
- 17.Raju S., Buck W.J., Crim W., Jayaraj A. Optimal sizing of iliac vein stents. Phlebology. 2018;33:451–457. doi: 10.1177/0268355517718763. [DOI] [PubMed] [Google Scholar]
- 18.Ludbrook J, M. C, F.R.C.S., F.R.A.C.S. Functional aspects of the veins of the leg. Am Heart J. 1962;64:706–713. doi: 10.1016/0002-8703(62)90257-0. [DOI] [PubMed] [Google Scholar]
- 19.Gooley N.A., Sumner D.S. Relationship of venous reflux to the site of venous valvular incompetence: implications for venous reconstructive surgery. J Vasc Surg. 1988;7:50–59. [PubMed] [Google Scholar]
- 20.Moore D.J., Himmel P.D., Sumner D.S. Distribution of venous valvular incompetence in patients with the postphlebitic syndrome. J Vasc Surg. 1986;3:49–57. doi: 10.1067/mva.1986.avs0030049. [DOI] [PubMed] [Google Scholar]
- 21.Ludbrook J. Charles C Thomas; Springfield, IL: 1966. Aspects of venous function in the lower limbs. [Google Scholar]
- 22.Arnoldi C. The venous return from the lower leg in health and in chronic venous insufficiency: a synthesis. Acta Orthopaedica Scand. 1964;35:3–75. doi: 10.3109/ort.1964.35.suppl-64.01. [DOI] [PubMed] [Google Scholar]
- 23.Ricci S., Moro L., Antonelli Incalzi R. The foot venous system: anatomy, physiology and relevance to clinical practice. Dermatol Surg. 2014;40:225–233. doi: 10.1111/dsu.12381. [DOI] [PubMed] [Google Scholar]
- 24.van Bemmelen P.S., Beach K., Bedford G., Strandness D.E., Jr. The mechanism of venous valve closure. Its relationship to the velocity of reverse flow. Arch Surg. 1990;125:617–619. doi: 10.1001/archsurg.1990.01410170063013. [DOI] [PubMed] [Google Scholar]
- 25.Raju S., Fredericks R., Lishman P., Neglen P., Morano J. Observations on the calf venous pump mechanism: determinants of postexercise pressure. J Vasc Surg. 1993;17:459–469. [PubMed] [Google Scholar]