Abstract
Background
GPs’ participation in continuous medical education (CME) is essential for patient care, GPs’ wellbeing, and healthcare expenditure. However, one-quarter of Danish GPs did not use their reimbursement for CME in 2022. Knowledge of barriers for participating in CME is limited.
Aim
To analyse the barriers GPs face to participation in CME, and patterns in perceived barriers.
Design & setting
A cross-sectional questionnaire study design was used. The study population comprised all 3257 GPs in Denmark who, in May 2023, were registered as entitled to reimbursement for CME.
Method
The response rate was n = 1303/3257 (40%). Based on a question about use of CME, the responders were divided into ‘frequent', ‘partial', and ‘seldom’ users. Partial and seldom users answered questions about barriers related to CME (n = 726). The presence of barriers was quantified, and a latent class analysis (LCA) was used to stratify GPs according to their barrier patterns.
Results
The most frequent barriers were as follows: too busy (67%); fully booked courses (45%); and no substitute or locum doctor (39%). Based on the LCA, we found three distinctive patterns, clustering around the following: GPs from clinics with no tradition for CME (class 1, 17%); GPs who used time on professional work outside clinic (teaching, organisational work) (class 2, 43%); and GPs who were personally or professionally affected (class 3, 40%). Singled-handed and male GPs were slightly overrepresented among seldom users.
Conclusion
We have identified barriers for CME. We found three different profiles of GPs who perceived different patterns of barriers. Identified patterns in barriers should be considered in future CME initiatives.
How this fits in
GPs’ participation in continuous medical education (CME) is essential for the quality of patient care, 1–3 the wellbeing of the GPs, 4 and the level of healthcare expenditure. 5 The value of CME is well documented and generally accepted but nevertheless some GPs do not engage in CME. Only a few studies have addressed barriers for GPs’ participation in CME. To recruit more GPs for CME, we need to understand how to make CME more achievable and attractive for GPs who are currently not engaging in CME.
Introduction
CME and continuous professional development (CPD) describe the process where healthcare professionals engage in ongoing learning and skill development to maintain, update, and enhance their professional knowledge, skills, and competencies. In this article, we use ‘CME’ to describe this process.
Organisation of CME for GPs
Different countries have chosen different models to ensure postgraduate education of GPs. CME can be mandatory, or it can be voluntary with the expectation that doctors have an ethical and professional obligation to undertake further education. CME can be based on public funding or rely on sponsorship from private or commercial actors. The way CME programmes are organised seems to influence the outcome. 1,6,7 Deliberate recruitment to CME, active learner participation, and mixed interactive and didactic educational meetings improves the outcome. 1 Funding relying on the pharmaceutical industry can bias the educational goals and topics. 6,8 From a patient perspective, however, the most important issue is the educational outcome and the improvement of clinical care. 9
Within Europe, CME varies from voluntary CME administered by the individual GP, to partly or mainly mandatory CME, with or without recertification. 7
The Danish GP CME programme consists of both mandatory centrally planned activities and self-chosen voluntary activities. 10 Both types of CME are remunerated. CME arranged by the pharmacological industry cannot be remunerated. The CME refund for a GP is approximately €6500 per year. 11 The CME programme is based on professional integrity and trust without recertification. 10 Despite a well-remunerated and comprehensive CME model, one-quarter of Danish GPs did not use renumeration for CME in 2022. 12
Barriers for participation in CME
Few studies have explored barriers for participation in CME. A study from Portugal found lack of time and bureaucracy overload as barriers for use of a digital CME platform. 13 Two Irish studies found that main barriers for participation in mandatory CME and maintenance of professional competence was lack of protected time and financial costs of CME participation. 14,15 Other noticeable barriers were expense of locum cover, lack of high quality and relevant CME themes, inconvenient locations, and technical difficulties. 14,15
However, we do not know if these barriers are relevant to GPs working under the Danish model. In a former qualitative study, 16 we uncovered 18 barriers for participation in CME. We do not know the magnitude or significance of these barriers. In a nationwide questionnaire survey in Denmark, we aim to generate quantitative data about barriers for participating in CME.
The objectives are:
to determine the frequency of barriers for CME;
to explore disparities in barriers between partial and seldom users of CME;
to identify profiles of GPs who experience barriers for participation in CME.
Method
Setting
In Denmark there is a specified specialist training scheme that lasts for 6 years to qualify as a GP. 17 General practice plays a vital role in the Danish healthcare system. 18 GPs are responsible for most of primary care and serve as the patient's first contact with the healthcare system. 18 Referral from a GP is required for most office-based specialists and in- and out-patient hospital treatment. 18 The average number of listed patients per GP is 1600.
Study population
The study population was all GPs in Denmark who in May 2023 were registered as entitled to reimbursement for participation in CME (n = 3257).
Study design
A cross-sectional questionnaire was conducted of Danish GPs’ motivation and barriers for participation in remunerated CME, and the GPs’ attitudes towards CME activities. In this article, we report data regarding barriers for participating in CME.
Data collection
In May 2023, all registered GPs in Denmark received an email invitation with an electronically administered questionnaire. Non-responders were sent a reminder after 1 week and 2 weeks. The response ratio was calculated as responders/study population. The link to the questionnaire was personal and contained a unique serial number. Demographic data were obtained through the questionnaire and through a central database in the Danish Organisation of General Practitioners (PLO). The research group received the anonymised dataset. Data were transferred to a secure server.
Questionnaire
The questionnaire was developed for the purpose by the research group based on literature search and interviews with 10 Danish GPs who had not used reimbursement for CME in a 2-year period. 16 The questionnaire was evaluated for construct and content validity using an educational expert review and a pilot test.
Six skilled people reviewed the questionnaire: two with research experience, two educationalists, and two GPs with educational insight. Four GPs were strategically selected with best variance in sex, seniority as a GP, geography, and practice type. They participated in a dynamic and repeated pilot test. The questionnaire was modified in the process for clarity and comprehensibility and for content and perspective.
Responders were initially asked: ‘Do you use all your reimbursement for CME?', with response options being: ‘frequent use', ‘partial use', ‘seldom use', or ‘do not know'. ‘Partial users’ and ‘seldom users’ were asked to rate 18 barriers on a Likert scale (strongly agree, agree, disagree, strongly disagree). See Supplementary Box 1 for questions regarding barriers.
Statistical methods
Descriptive statistics were used to examine the distribution of responses, expressed as numbers and percentages, among participants in the investigated categories ('strongly agree', ‘agree', ‘disagree', and ‘strongly disagree') in relation to the different questions about barriers. Categories with a limited number of responders were merged owing to the Danish General Data Protection Regulation (GDPR).
P values, used to assess differences in barriers between partial users and seldom users, were calculated using χ2 test or Fisher’s exact test, when the frequency in one of the cells was <5.
To investigate the representativeness of our study population, we compared baseline characteristics on sex, age, practice type, and geography in our study population with data from the PLO covering all GPs in Denmark.
To investigate whether certain barriers were more likely to be mentioned together, we employed the statistical method latent class analysis (LCA). 19 LCA identifies patterns among selected barriers potentially revealing subgroups of GPs associated with these barriers. LCA is a statistical method employed to identify distinct subgroups within a population that share similar characteristics. 20 The Akaike Information Criterion (AIC) and the Bayesian Information Criterion (BIC) were used to evaluate the model fit. Models with more than three latent classes were incompatible with the data. Among the models with two and three classes, the model with three classes exhibited the best fit based on both AIC and BIC. The LCA exclusively focused on barrier-related responses and were not adjusted for covariates. Nevertheless, differences in covariate distributions across the three identified classes were assessed using χ2 test. All analyses were conducted using Stata (version 18.0).
Results
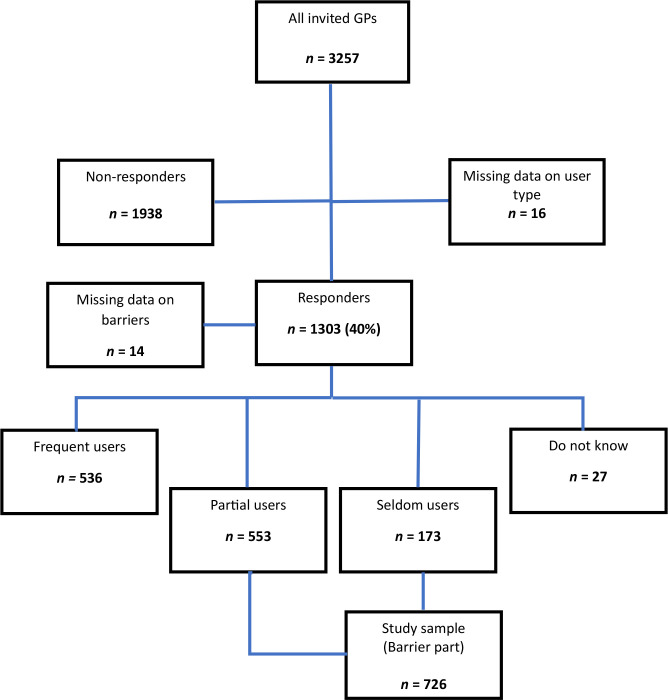
Of the 3257 invited GPs, 1303 GPs (40%) took part in the survey. In this article, we focus on a subset of 726 GPs categorised as ‘seldom users’ (n = 173) and ‘partial users’ (n = 553), as they form the population of interest regarding barriers to CME. A flowchart of the study population is shown in Figure 1.
Figure 1. Flowchart of study population.
Representativeness of study population
Demographic factors in the responder group (sex, age, practice type, and geographical regions in Denmark) showed a balanced distribution compared with all Danish GPs except from a larger proportion of female responders (68%) compared with overall female representation in the GP population (60%) (Supplementary Table S1).
Association between use of reimbursement and demographic data
GPs in singled-handed practices and male GPs were overrepresented and female GPs were underrepresented among ‘seldom users'. The other demographic data were evenly distributed. Table 1 shows characteristics of our study sample ('partial users’ and ‘seldom users') compared with all responders with P-values for differences between groups demonstrated in Supplementary Table S2.
Table 1. Baseline characteristics of all responders stratified by use of continuous medical education.
| Frequent users (n = 536, 42.5%) | Partial users (n = 553, 43.8%) | Seldom users (n = 173, 13.7%) | Total (n = 1262) | |
|---|---|---|---|---|
| Sexa | ||||
| Female | 386 (72.3) | 370 (66.9) | 98 (56.7) | 854 (67.8) |
| Male | 148 (27.7) | 183 (33.1) | 75 (43.4) | 406 (32.2) |
| Age in years, mean (SD) | 51.9 (7.6) | 51.3 (8.0) | 52.1 (8.7) | 51.7 (8.0) |
| Seniority as a GP | ||||
| <5 years | 91 (17.0) | 103 (18.6) | 34 (19.7) | 228 (18.1) |
| 5–15 years | 229 (42.7) | 268 (48.5) | 86 (49.7) | 583 (46.2) |
| >15 years | 216 (40.3) | 182 (32.9) | 53 (30.6) | 451 (35.7) |
| Practice type | ||||
| Shared practice | 39 (7.3) | 32 (5.8) | 9 (5.2) | 80 (6.3) |
| Partnership | 410 (76.5) | 408 (73.8) | 95 (54.9) | 913 (72.3) |
| Collaboration | 33 (6.2) | 45 (8.1) | 12 (6.9) | 90 (7.1) |
| Singled-handed | 54 (10.1) | 68 (12.3) | 57 (33.0) | 179 (14.2) |
Data are n (%) unless stated otherwise.
SD = standard deviation.
aTwo participants did not report their sex in the survey
Perceived barriers
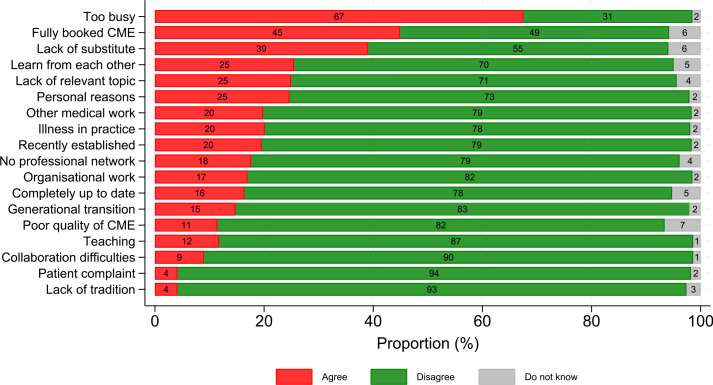
The most frequently barrier (recognised by 67%) was being too busy. Figure 2 shows the extent to which GPs expressed agreement or disagreement within each barrier. Differences in barriers between partial and seldom users are demonstrated in Supplementary Tables S3–S6.
Figure 2. Frequency of barriers for participation in continuous medical education (CME) among GPs who are not using all their reimbursement for CME (n = 726).
Fully booked courses (45%) and difficulties in finding a substitute or locum (39%) were the second and third most common barriers, whereas lack of tradition for CME, patients’ complaints, and collaboration difficulties were reported less often.
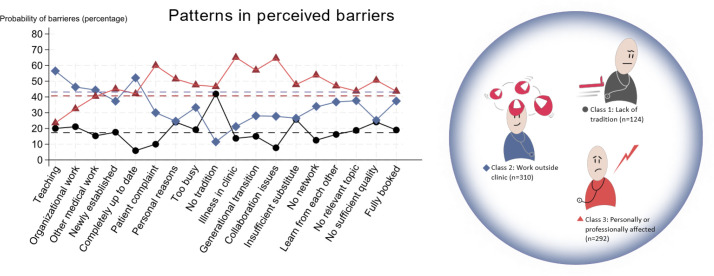
Three characteristic patterns of barriers
The statistical method LCA revealed three subgroups (classes) among GPs. The total of 726 GPs were categorised into the following three classes: class 1 (n= 124, 17% of the GPs); class 2 (n = 310, 43% of the GPs); and class 3 (n = 292, 40% of the GPs).
The distribution of the three classes and the probabilities of barrier responses reported is shown in Figure 3. When the reported barrier deviates from the dashed line in the class colour, it indicates that the barrier is selected more often or less often than expected based solely on the size of the class.
Figure 3. Barrier response probabilities reported by GPs with respect to the three latent classes.
Class 1 reported ‘No tradition for CME’ as their main barrier (42%). ‘Being completely up to date’ (6%) and ‘collaboration difficulties’ (8%) were uncommon barriers in this group. The other barriers were more evenly distributed corresponding to class 1’s share of responders.
Class 2 reported ‘teaching’ (57%), and ’being completely up to date’ (52%) as frequent barriers. ‘Lack of tradition for CME’ was less frequently reported (12%). Despite activities outside clinic (teaching), class 2 had the lowest propability of reporting ‘lack of substitute’ (27%) and being ‘too busy’ (33%).
The GPs in class 3 reported ‘illness in their clinics’ (65%) ‘collaboration problems’ in their clinics (65%), ‘patients’ complaints’ (60%), or ‘generational transition’ in their clinics (57%), ‘no network’ when on courses (54%), and ‘personal reasons’ (51%), which included illness experienced by the GP themselves, more often than the two other classes.
As showed in Table 2, responders’ perceived barriers vary significantly (P<0.05) across the three groups in 13 of 18 barriers.
Table 2. The comparison of barriers for continuous medical education across latent classes (n = 726).
| Class 1 n = 124 (17.1%) | Class 2 n = 310 (42.7%) | Class 3 n = 292 (40.2%) | P values | |
|---|---|---|---|---|
| Teaching | 17 (20.0) | 48 (56.5) | 20 (23.5) | 0.003* |
| Organisational work | 26 (21.1) | 57 (46.3) | 40 (32.5) | 0.126 |
| Other medical work | 22 (15.3) | 64 (44.4) | 58 (40.3) | 0.797 |
| Recently established | 25 (17.6) | 53 (37.3) | 64 (45.1) | 0.307 |
| Completely up to date | 7 (5.9) | 62 (52.1) | 50 (42.0) | 0.001* |
| Patient complaint | 3 (10.0) | 9 (30.0) | 18 (60.0) | 0.097 |
| Personal reasons | 43 (24.0) | 44 (24.6) | 92 (51.4) | <0.001* |
| Too busy | 94 (19.2) | 163 (33.3) | 233 (47.6) | <0.001* |
| Lack of tradition | 109 (41.9) | 30 (11.5) | 121 (46.5) | <0.001* |
| Illness in practice | 20 (13.7) | 31 (21.2) | 95 (65.1) | <0.001* |
| Generational transition | 16 (15.0) | 30 (28.0) | 61 (57.0) | <0.001* |
| Collaboration difficulties | 5 (7.7) | 18 (27.7) | 42 (64.6) | <0.001* |
| Lack of substitute or locum | 119 (25.7) | 123 (26.5) | 222 (47.8) | <0.001* |
| No professional network | 16 (12.5) | 43 (33.6) | 69 (53.9) | 0.003* |
| Learn from each other | 30 (16.2) | 68 (36.8) | 87 (47.0) | 0.049* |
| Lack of relevant topic | 34 (18.8) | 68 (37.6) | 79 (43.7) | 0.235 |
| Poor quality of CME | 20 (24.1) | 21 (25.3) | 42 (50.6) | 0.003* |
| Fully booked CME | 62 (19.0) | 122 (37.4) | 142 (43.6) | 0.013* |
Data are n (%). The P values were computed from χ2 tests or Fisher’s exact test when the frequency in one of the cells was <5. Significance levels P<0.05 are marked in bold with asterisk.
CME = continuous medical education.
The percentages shown for the barriers do not add up to 100% for each class as they demonstrate the distribution among the three classes.
Covariates
The responding GPs had similar sex, age, seniority as GPs, distribution of practice types, and distribution of practice owners and employed GPs between the classes.
The distribution of covariates across participants answering strongly agree and agree to barriers are demonstrated in Table 3.
Table 3. The covariate distribution across latent classes of situations where responders answer strongly agree or agree to barriers regarding continuous medical education (CME).
| Class 1 (n = 124, 17.1%) | Class 2 (n = 310, 42.7%) | Class 3 (n = 292, 40.2%) | P-values | |
|---|---|---|---|---|
| Sexa | 0.299 | |||
| Female | 82 (66.1) | 190 (61.3) | 196 (67.1) | |
| Male | 42 (33.9) | 120 (38.7) | 96 (32.9) | |
| Age in years, mean (SD) | 51.0 (7.9) | 52.4 (8.4) | 50.7 (8.0) | 0.278 |
| Users of CME | 0.514 | |||
| Partial users | 97 (78.2) | 240 (77.4) | 216 (74.0) | |
| Seldom users | 27 (21.8) | 70 (22.6) | 76 (26.0) | |
| Seniority as a GP | 0.630 | |||
| <5 years | 23 (18.6) | 55 (17.7) | 59 (20.2) | |
| 5–15 years | 63 (50.8) | 145 (46.8) | 146 (50.0) | |
| ≥16 years | 38 (30.7) | 110 (35.5) | 87 (29.8) | |
| Practice ownership | 0.664 | |||
| Owner | 121 (97.6) | 303 (97.7) | 288 (98.6) | |
| Employed | 3 (2.4) | 7 (2.3) | 4 (1.4) | |
| Practice type | 0.150 | |||
| Shared practice | 8 (6.5) | 21 (6.8) | 12 (4.1) | |
| Partnership | 82 (66.1) | 201 (64.8) | 220 (75.3) | |
| Collaboration | 12 (9.7) | 25 (8.1) | 20 (6.9) | |
| Singled-handed | 22 (17.7) | 63 (20.3) | 40 (13.7) | |
Data are n (%) unless stated otherwise. The P-values were computed from χ2 tests or Fisher’s exact test when the frequency in one of the cells was <5.
CME = continuous medical education. SD = standard deviation
aTwo participants did not report their sex in the survey
Discussion
Summary
In this cross-sectional questionnaire study, uncovering GPs’ perceived barriers to CME, the most frequently reported barrier was ‘being too busy with everyday work’. All GPs reported several barriers. Combinations of selected barriers revealed three possible profiles of GPs perceiving barriers for participating in CME:
GPs who had no tradition for CME and might need enhanced motivation;
GPs who used time on professional work outside clinic (teaching, organisational work);
GPs who were personally or professionally affected.
Patient complaints were reported more frequently as a barrier among the GPs who were personally or professionally affected. However, it does not necessarily imply that GPs in this subgroup receive more patient complaints. A complaint can have a negative psychological impact and may reduce GPs’ motivation for CME.
Male GPs and GPs in singled-handed practices were overrepresented among seldom users of CME.
Strengths and limitations
All GPs in Denmark were invited to the questionary survey. The response rate of 40% was comparable with other survey studies on GPs 21,22 but could entail selection bias. However, the study population reflected the total GP population except for a larger proportion of female GPs (68% versus 60%). This might underestimate barriers as female GPs were overrepresented among ‘frequent users’ of CME. The number of ‘seldom users’ in our study was in line with or above earlier studies. 16
We used qualitative interviews to identify possible barriers to CME. It is a strength that the questionnaire was based on barriers defined by GPs who had not engaged in CME in a 2-year period. 16
Using self-reported data can be a limitation if GPs are less likely to report themselves as ‘seldom users’ but the rate of responders classifying themselves as ‘seldom users’ was in line with the proportion of GPs who were not using their reimbursement in the annual report from PLO. 12
Comparison with existing literature
Studies from Portugal and Ireland 13–15 found ‘lack of time’ as a main barrier, which corresponds to our finding of ‘being too busy’, as the most frequently reported barrier. Similarly, to the Irish studies, 14,15 we found problems with locum cover as a frequent barrier.
‘Lack of quality of CME’ and ‘technical difficulties’ were seldom reported in Denmark, which differed from the Irish studies, 14,15 whereas ‘lack of relevant themes’ was recognised in both countries. ‘Overbooked courses’ was the second most reported barrier in Denmark but to our knowledge overbooked courses are not described in other studies. Financial costs were not relevant in our study because we investigated barriers among GPs who had not used all their reimbursement.
In a former study, 16 we found that all GPs stated ‘too busy’ but all GPs were able to point out other barriers that could explain their experience of being too busy. The barriers behind ‘too busy’ could be divided into the following three categories: barriers related to the clinic; barriers related to the CME; and personal barriers. In the present study, barriers related to CME and barriers related to the clinic were reported more often than barriers related to the individual GP. However, in our LCA, we identified a class where GPs reported personal reasons significantly more often (see Table 2). In this class, GPs expressed a higher level of being too busy compared with the other two classes. This suggests that the GP with barriers related to personal issues to a higher degree perceive themselves as overwhelmed by their workload.
We found no previous studies of underlying patterns in responders’ barrier-related responses among GPs.
We found male GPs and GPs in singled-handed practices slightly overrepresented among ‘seldom users'. A report from 2022 showed similar findings. 12
Implications for research and practice
Our study highlights potentials for CME organisers and health authorities. Focus on accessibility to relevant CME activities will probably support recruitment to CME.
A course that is set-up to be more adapted to busy workdays may ease the need for substitutes. In addition, facilitation of workplace learning, ‘learning from each other’, can strengthen an existing tradition.
Such a course can be appropriate with awareness of:
newly established GPs and ongoing retirement may result in temporary disengagement with CME;
GPs lacking a professional network may not engage with CME;
GPs struggling with work overload and/or social challenge may need support different from traditional CME activities;
a knowledge of profiles of GPs perceiving barriers for CME can be used to target CME to the GPs who are currently not engaging with CME.
Further research in preferred educational set-up, in attitudes to CME, and how to enhance GPs’ intrinsic professional motivation could be of interest. Additionally, there is a need to monitor barriers in future CME evaluations.
Conclusion
We have identified barriers for CME. Some can easily be addressed while others will be far more complex to overcome. We found the following three different profiles of GPs who perceived different patterns of barriers: GPs who have no tradition for CME and may need enhanced motivation; GPs who use time on professional work outside clinic (teaching, organisational work); and GPs who are personally or professionally affected. The patterns in barriers should be considered in future CME initiatives.
Funding
Open access funding provided by University Library of Southern Denmark. HI had funding from Research Unit of General Practice as well as The Faculty of Health Sciences, Department of Public Health, University of Southern Denmark.
Ethical approval
All methods were conducted in accordance with relevant guidelines and regulations. The project has been ethically approved by SDU (University of Southern Denmark) Research and Innovation Organisation, RIO (record number 11.659). The National Scientific Ethical Committee has been asked (record number 20222000-47) but according to the Danish legislation (Scientific Ethical Committees Act § 14/1 + 2)) the project needs no approval from the National Scientific Ethical Committee.
Provenance
Freely submitted; externally peer reviewed.
Data
The dataset relied on in this article is available from the corresponding author on reasonable request.
Acknowledgements
The authors want to thank the 1303 Danish GPs for participating in the questionnaire survey and PLO-E for sending emails with link to the questionnaire to all GPs in Denmark.
Competing interests
The authors declare that no competing interests exist.
References
- 1.Forsetlund L, O’Brien MA, Forsén L, et al. Continuing education meetings and workshops: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2021; 9 (9):CD003030. doi: 10.1002/14651858.CD003030.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McBride A, Collins C, Osborne B, McVeigh H. Does continuing professional development enhance patient care? A survey of Irish based general practitioners: successful implementation of mandatory CPD in Irish general practice. BMC Med Educ. 2022; 22 (1):220. doi: 10.1186/s12909-022-03292-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nørøxe KB, Vedsted P, Bro F, et al. Mental well-being and job satisfaction in general practitioners in Denmark and their patients’ change of general practitioner: a cohort study combining survey data and register data. BMJ Open. 2019; 9 (11):e030142. doi: 10.1136/bmjopen-2019-030142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kjaer NK, Steenstrup AP, Pedersen LB, Halling A. Continuous professional development for GPs: experience from Denmark. Postgrad Med J. 2014; 90 (1065):383–387. doi: 10.1136/postgradmedj-2012-131679. [DOI] [PubMed] [Google Scholar]
- 5.Nørøxe KB, Pedersen AF, Carlsen AH, et al. Mental well-being, job satisfaction and self-rated workability in general practitioners and hospitalisations for ambulatory care sensitive conditions among listed patients: a cohort study combining survey data on GPs and register data on patients. BMJ Qual Saf. 2019; 28 (12):997–1006. doi: 10.1136/bmjqs-2018-009039. [DOI] [PubMed] [Google Scholar]
- 6.Bednář JBJ, Michels NR, Kalda R, et al. Current state of the evidence-base for effective continuous medical education for family medicine and general practice: WONCA. 2021. https://www.euract.eu/resources/view/current-state-of-the-evidence-base-for-effective-continuous-medical-education-for-family-medicine-and-general-practice. [8 Jul 2024]. https://www.euract.eu/resources/view/current-state-of-the-evidence-base-for-effective-continuous-medical-education-for-family-medicine-and-general-practice accessed.
- 7.Löffler C, Altiner A, Blumenthal S, et al. Challenges and opportunities for general practice specific CME in Europe — a narrative review of seven countries. BMC Med Educ. 2022; 22 (1):761. doi: 10.1186/s12909-022-03832-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spurling GK, Mansfield PR, Montgomery BD, et al. Information from pharmaceutical companies and the quality, quantity, and cost of physicians’ prescribing: a systematic review. PLoS Med. 2010; 7 (10):e1000352. doi: 10.1371/journal.pmed.1000352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holm HA. Quality issues in continuing medical education. BMJ. 1998; 316 (7131):621–624. doi: 10.1136/bmj.316.7131.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kjaer NK, Vedsted M, Høpner J. A new comprehensive model for continuous professional development. Eur J Gen Pract. 2017; 23 (1):20–26. doi: 10.1080/13814788.2016.1256998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Praktiserende Lægers Organisation [Agreement on General Practice 2022] Overenskomst om almen paksis 2022 (in Danish) 2022. https://laeger.dk/media/bmhpndle/plo_overenskomst_2022_web-1.pdf. [8 Jul 2024]. https://laeger.dk/media/bmhpndle/plo_overenskomst_2022_web-1.pdf accessed.
- 12.Danish Organisation of General Practitioners (PLO) [Annual report for 2022] Årsberetning for 2022 (in Danish) https://laeger.dk/media/a3bm15x3/aarsberetning-for-fonden-for-almen-praksis-2022.pdf. [8 Jul 2024];Efteruddannelse.: Fonden for Almen Praksis. 2023 accessed.
- 13.Reis T, Faria I, Serra H, Xavier M. Barriers and facilitators to implementing a continuing medical education intervention in a primary health care setting. BMC Health Serv Res. 2022; 22 (1):638. doi: 10.1186/s12913-022-08019-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hanlon HR, Prihodova L, Russell T, et al. Doctors’ engagement with a formal system of continuing professional development in Ireland: a qualitative study in perceived benefits, barriers and potential improvements. BMJ Open. 2021; 11 (11):e049204. doi: 10.1136/bmjopen-2021-049204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Galvin E, Wiese A, Dahly D, et al. Maintenance of professional competence in Ireland: a national survey of doctors’ attitudes and experiences. BMJ Open. 2020; 10 (12):e042183. doi: 10.1136/bmjopen-2020-042183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ibsen H, Lillevang G, Søndergaard J, Kjaer NK. "We don't need no education" — a qualitative study of barriers to continuous medical education among Danish general practitioners. BMC Med Educ. 2023; 23 (1):450. doi: 10.1186/s12909-023-04432-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sundhedsstyrelsen [Curriculum, specialist training, family medicine] Målbeskrivelse for speciallægeuddannelsen i almen medicin (in Danish) 2013. https://www.sst.dk/-/media/Viden/Uddannelse/Uddannelse-af-speciallaeger/Maalbeskrivelser/Almen-medicin/Almen_medicin_2013_p3.ashx. [8 Jul 2024]. https://www.sst.dk/-/media/Viden/Uddannelse/Uddannelse-af-speciallaeger/Maalbeskrivelser/Almen-medicin/Almen_medicin_2013_p3.ashx accessed.
- 18.Pedersen KM, Andersen JS, Søndergaard J. General practice and primary health care in Denmark. J Am Board Fam Med. 2012; 25 Suppl 1 :S34–S38. doi: 10.3122/jabfm.2012.02.110216. [DOI] [PubMed] [Google Scholar]
- 19.Hagenaars JA, McCutcheon AL. Applied latent class analysis. Cambridge: Cambridge University Press; 2002. [Google Scholar]
- 20.Weller BE, Bowen NK, Faubert SJ. Latent class analysis: a guide to best practice. J Black Psychol. 2020; 46 (4):287–311. doi: 10.1177/0095798420930932. [DOI] [Google Scholar]
- 21.Sebo P, Maisonneuve H, Cerutti B, et al. Rates, delays, and completeness of general practitioners’ responses to a postal versus web-based survey: a randomized trial. J Med Internet Res. 2017; 19 (3):e83. doi: 10.2196/jmir.6308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sahlqvist S, Song Y, Bull F, et al. Effect of questionnaire length, personalisation and reminder type on response rate to a complex postal survey: randomised controlled trial. BMC Med Res Methodol. 2011; 11 :62. doi: 10.1186/1471-2288-11-62. [DOI] [PMC free article] [PubMed] [Google Scholar]