Abstract
Background
One in six Mexican adults’ lives with type 2 diabetes mellitus (T2DM), which is the third leading cause of death in the country. Analyzing the geographic distribution of T2DM mortality helps identify regions with higher mortality rates. This study aimed to examine the spatial patterns of mortality from type 2 diabetes mellitus (T2DM) across municipalities in Mexico and to analyze the main contextual factors linked to this cause of death in 2020.
Methods
We employed a spatial Bayesian hierarchical regression model to estimate the risk and probability of death from type 2 diabetes mellitus (T2DM) across Mexico’s municipalities.
Results
The SMR results revealed geographic and age-specific patterns. Central Mexico and the Yucatán Peninsula exhibited the highest excess mortality rates. For the population under 50 years of age, municipalities in Oaxaca had the highest T2DM mortality rates, whereas those aged 50 years old and older had the highest rates in Tlaxcala and Puebla. Socioeconomic factors such as low levels of educational attainment, lack of health services, dietary deficiency, and marginalization were positively associated with increased T2DM mortality risk. By contrast, GDP per capita showed a negative association. High-risk areas for T2DM mortality were prominent along the south of the Pacific Coast, the Bajío, Central Mexico, and southern Yucatán for those under 50, and along a central strip extending to the Yucatán Peninsula for the older population. Significant uncertainties in mortality risk were identified, with Central Mexico, Oaxaca, Chiapas, and Tabasco showing high probabilities of excess risk for those under 50 years of age and extended risk areas along the Gulf of Mexico for those 50 years old and older.
Conclusions
The assessment and identification of spatial distribution patterns associated with T2DM mortality, and its main contextual factors, are crucial for informing effective public health policies aimed at reducing the impact of this chronic disease in Mexico.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13690-024-01432-z.
Keywords: Diabetes mellitus, Socioeconomic factors, Mexico, Municipalities, Bayesian hierarchical model
| Text box 1. Contributions to the literature |
|---|
| • The study of diabetes at the municipal level helps gain deeper insights into the social determinants of health, highlighting disparities in healthcare access, socioeconomic factors, and environmental influences that contribute to differential disease burdens. |
| • To estimate the risk and probability of death from type 2 diabetes in Mexico |
| • We employed a spatial Bayesian hierarchical regression model as a methodological alternative to that used in previous studies |
| • The results revealed geographic and age-specific mortality patterns |
| • Socioeconomic factors were associated with increased T2DM mortality risk, while GDP per capita showed a negative association with T2DM mortality |
Introduction
Type 2 diabetes mellitus (T2DM) is a growing health concern worldwide. In 2021, an estimated 537 million individuals aged 20–79 were living with diabetes globally. Projections indicate that this number will rise to 783 million by 2045 [1]. The increase in T2DM will predominantly occur in low- and middle-income nations [2, 3], such as Mexico, where resources for treating the disease and its complications are limited. The main T2DM complications are cardiovascular disease, visual impairment due to diabetes retinopathy, kidney failure, and lower limb amputation [4]. The projected increase is linked to several factors, such as the aging population, which will mean a higher percentage of individuals over 60 living with T2DM, higher rates of obesity and increases in excess weight due to lifestyle changes (such as an increased calorie intake and a decrease in physical activity) [1, 2], and improved medical treatments, leading to higher survival rates among those with T2DM. Excluding the mortality risks associated with COVID-19, the International Diabetes Federation estimated that approximately 6.7 million individuals aged 20 to 79 years died worldwide from T2DM or its complications in 2021. This accounted for approximately 12.2% of the total deaths in these age groups [1]. Most of these T2DM-related deaths occurred in low- and middle-income countries [5], with the 35–64 age group being the most affected [1].
In 2021, Mexico ranked seventh globally for the highest rates of individuals living with T2DM, totaling around 14.1 million adults aged 20 to 79. This indicates that one out of every six Mexican adults are affected by this condition. The number is projected to rise to 21.2 million by 2045 [1], largely driven by the high prevalence of obesity and physical inactivity [6, 7]. In 2020, T2DM was ranked as the third leading cause of death in the country, following cardiovascular diseases and COVID-19, with 151,019 recorded deaths. Over the past three decades, mortality associated with T2DM has surged by 77% in Mexico [8]. Mortality related to T2DM is associated with sociodemographic and economic inequalities [8], which have been exacerbated by the COVID-19 pandemic. For example, there was an estimated 41% increase in T2DM-related deaths in 2020 compared to the preceding period from 2017 to 2019, reflecting the significant impact the pandemic has had in Mexico [9].
Several social factors at the municipal level have been associated with the prevalence of T2DM. Socioeconomic factors like poverty [10] and income inequality [11], as well as social cohesion, can impact health behaviors and access to healthcare services, all of which are linked to T2DM [12]. Globalization and rapid urbanization can lead to sedentary lifestyles, increased consumption of processed foods, and higher levels of stress, all of which are also risk factors for T2DM. Furthermore, education level and access to education are associated with T2DM [13], likely influencing individuals’ understanding and awareness of the health benefits of preventive behaviors [14]. Low educational attainment levels are also correlated to higher overweight and obesity rates [15].
Analyzing the geographic distribution of T2DM mortality facilitates the identification of geographic areas with higher mortality rates [16]. The risk factors for T2DM can vary significantly between regions. Thus, by studying diabetes at the municipal level, we can gain deeper insights into the social determinants of health, highlighting disparities in healthcare access, socioeconomic factors, and environmental influences that contribute to differential disease burdens. Consequently, examining type 2 diabetes at this scale provides valuable insights into the local disease burden, informing targeted strategies for prevention, public health planning, resource allocation, and policy development [12]. Therefore, the main objective of this study is to examine the spatial patterns of mortality from T2DM across municipalities in Mexico and to investigate the main contextual factors linked to this cause of death in 2020. For this purpose, we used a spatial Bayesian hierarchical regression model [17–19] based on the Integrated Nested Laplace Approximation (INLA) [20].
Variables, data sources, and scale of analysis
This study assembles data from multiple sources. Municipal-level deaths from type 2 diabetes mellitus (T2DM) (International Classification of Diseases, ICD-10 codes E110-E119) serve as the dependent variable in this study. Data on this cause-specific, which includes information on the cause of death by sex and municipality of residence, as well as age-specific (population under 50 years of age and those 50 years old and older), and comes from the National Institute of Statistics and Geography of Mexico [21]. We also used population estimates from the Mexican Population Council (CONAPO). This population estimate is corrected for completeness, age misstatements, and international migration [22]. We selected 2020 to analyze T2DM mortality because the most recent municipal-level data for many socioeconomic indicators is from that year, as they are based on the 2020 Population Census.
We also analyzed five socioeconomic indicators that have been shown to correlate with the prevalence of T2DM: (i) low levels of educational attainment, which refers to individuals or populations that have not been able to access or achieve expected educational benchmarks for their age/learning level. Education is one of the main factors associated with the risk of T2DM [13]. This data was obtained from the 2020 municipal poverty measurement conducted by the National Council for the Evaluation of Social Development Policy [23]; (ii) lack of access to health services. This refers to the proportion of individuals who do not have access to essential healthcare services or face barriers to accessing healthcare facilities. This data also comes from the National Council for the Evaluation of Social Development Policy [23]. Access to healthcare is crucial for preventing the onset of T2DM and managing the disease to avoid serious complications [13, 24]; (iii) dietary deficiency, an indicator used by CONEVAL to measure municipal poverty, was utilized as a proxy for food insecurity [23]. Food insecurity significantly impacts the risk and management of T2DM by forcing individuals to rely on low-cost, calorie-dense, nutrient-poor foods that are high in sugars, refined carbohydrates, and unhealthy fats, and by creating a stress environment that can lead to the development of insulin resistance and T2DM [25]; (iv) Since there is no gross domestic product (GDP) at the municipal level in Mexico, we used the gross value added from the 2019 Economic Census (INEGI) as a proxy. This variable is the best approximation of GDP that could be implemented to achieve the objectives of this study. GDP per capita is one of the most widely used socioeconomic predictors of mortality and health [26–32]; and (v) the marginalization index, which measures socioeconomic disparities across municipalities in Mexico [33].
Finally, the units of analysis used were the 2,469 Mexican municipalities, that are divided into thirty-two states and six regions (see Fig. 1).
Fig. 1.
Mexico by regions and states
Methods
Standardized mortality ratio (SMR)
Regional disparities in mortality rates often stem from differences in the age structures of populations. To facilitate comparisons across regions, researchers commonly employ the standardized mortality ratio (SMR), an indirect age-adjustment technique. SMR is calculated as the ratio of observed deaths in a given population to the expected number of deaths [34].
 |
 |
The formula for SMR involves dividing the observed deaths  in a municipality i (i = 1, 2, …, 2468, 2469) by the expected deaths
in a municipality i (i = 1, 2, …, 2468, 2469) by the expected deaths  . The expected deaths
. The expected deaths  are determined by multiplying the mortality rate of a standard population
are determined by multiplying the mortality rate of a standard population  by the total population of municipality i (
by the total population of municipality i ( ). A SMR exceeding one indicates excess mortality within the study population. Despite its unbiased nature in estimating mortality, the SMR method has some limitations. Notably, it does not elucidate the spatial structure inherent in these data and struggles to discern regions with limited or absent death records. This drawback has been highlighted previously [35].
). A SMR exceeding one indicates excess mortality within the study population. Despite its unbiased nature in estimating mortality, the SMR method has some limitations. Notably, it does not elucidate the spatial structure inherent in these data and struggles to discern regions with limited or absent death records. This drawback has been highlighted previously [35].
Bayesian spatial model
The Bayesian spatial model offers a remedy to the drawbacks inherent in the Standardized Mortality Ratio (SMR) approach. Because of its simplicity, SMR overlooks spatial dependencies between areas, which means that essentially no spatial structure in risk is modeled [36]. Moreover, the SMR can be easily affected when applied to areas with small populations, which may cause large fluctuations in the estimation [37]. By contrast, the Bayesian spatial model demonstrates superior efficacy in capturing spatial patterns by incorporating global and local information to mitigate instability [35].
Typically, health data encompass various outcomes, such as the number of deaths or occurrences of specific diseases, along with spatial and/or temporal factors. A key advantage of employing Bayesian modeling is its ability to accommodate unobservable variables, treating them as random effects within the model. This flexibility is particularly valuable when not all factors influencing outcomes can be measured directly. By considering all observed data and covariates, Bayesian inference facilitates the direct estimation of posterior probability distributions, with straightforward interpretation when posterior probabilities exceed or fall within confidence intervals. Consequently, the Bayesian approach has gained traction across disciplines for estimating potential risk factors.
In our study, we modeled the number of type 2 diabetes mellitus (T2DM) deaths, denoted as  , using a Poisson distribution, where a log-linear model is specified for T2DM mortality. The log-linear model is expressed as:
, using a Poisson distribution, where a log-linear model is specified for T2DM mortality. The log-linear model is expressed as:
 |
 |
Here, represents the expected number of T2DM deaths in area i (
represents the expected number of T2DM deaths in area i ( ), and
), and  denotes the specific relative risk in that area.
denotes the specific relative risk in that area.  quantifies the average T2DM mortality across all 2,469 municipalities;
quantifies the average T2DM mortality across all 2,469 municipalities;  is a spatially structured random effect modeled using an intrinsic conditional autoregressive distribution (iCAR),
is a spatially structured random effect modeled using an intrinsic conditional autoregressive distribution (iCAR),  [17], whereas
[17], whereas  is a spatially unstructured random effect modeled using an exchangeable prior,
is a spatially unstructured random effect modeled using an exchangeable prior,  .
.
Expanding upon this formulation, we incorporated covariates to assess their impact on T2DM mortality risk. The extended model is expressed as:
 |
Here,  represents the global intercept, while
represents the global intercept, while  are coefficients for the covariates. The model includes predictor variables, such as the percentage of the population with low levels of educational attainment (
are coefficients for the covariates. The model includes predictor variables, such as the percentage of the population with low levels of educational attainment ( ), percentage of the lack of health services (
), percentage of the lack of health services ( , percentage of the population with dietary deficiency (
, percentage of the population with dietary deficiency ( ), gross domestic product (GDP) per capita (
), gross domestic product (GDP) per capita ( ), and marginalization index (
), and marginalization index ( ). The coefficients
). The coefficients  are interpretable as relative risk (RR), indicating the percentage increase or decrease in T2DM mortality risk associated with a one-unit change in the respective covariate (
are interpretable as relative risk (RR), indicating the percentage increase or decrease in T2DM mortality risk associated with a one-unit change in the respective covariate ( , where j = 1, …, 5). The Besag-York-Mollié (BMY) specification is adopted for this model, along with first-order neighborhood spatial weights [17].
, where j = 1, …, 5). The Besag-York-Mollié (BMY) specification is adopted for this model, along with first-order neighborhood spatial weights [17].
Results
Standardized mortality ratio (SMR)
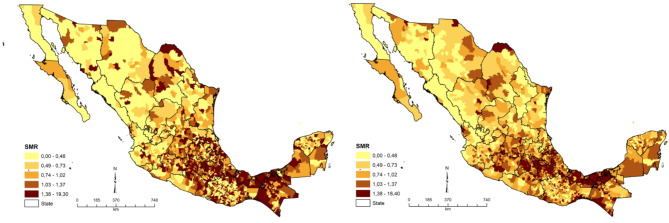
Figure 2 shows the spatial distribution of SMR in 2020 across 2,469 municipalities in Mexico, for both the population under 50 years of age (left) and those 50 years old and older (right). Overall, excess mortality (> 1) was the most widespread in the regions of Central Mexico and Yucatán Peninsula. These regions are characterized by a lower socioeconomic development, limited access to healthcare facilities, a higher percentage of the population with dietary deficiencies, and higher marginalization. The municipalities of San Miguel Achiutla, San Pedro Nopala, and Abejones, all in the state of Oaxaca, have the highest T2DM mortality rates for the population under 50. Meanwhile, the municipalities of La Magdalena Tlaltelulco and San Pablo del Monte in Tlaxcala state, as well as Acatzingo in Puebla state, have the highest T2DM mortality rates for those aged 50 years and older.
Fig. 2.
Standardized Mortality Ratio of T2DM by municipality in Mexico, 2020. Under 50 years old (left) and 50 years old and older (right)
Spatial model
Tables 1 and 2 present the fixed effects ( ) estimated by R-INLA. First, the two models (< 50 years of age and ≥ 50 years of age) agree on the algebraic sign (positive or negative) of all the coefficient estimates. Furthermore, as they are reported on a natural scale, it is possible to interpret them as relative risks. In other words, an increase of one unit in the percentage of the population with low levels of educational attainment (
) estimated by R-INLA. First, the two models (< 50 years of age and ≥ 50 years of age) agree on the algebraic sign (positive or negative) of all the coefficient estimates. Furthermore, as they are reported on a natural scale, it is possible to interpret them as relative risks. In other words, an increase of one unit in the percentage of the population with low levels of educational attainment ( ) is associated with a 1.3% increase in the risk of death from Type 2 diabetes for populations under 50 years of age, and a 0.2% increase for those 50 years old and older. Regarding the percentage of the lack of health services (
) is associated with a 1.3% increase in the risk of death from Type 2 diabetes for populations under 50 years of age, and a 0.2% increase for those 50 years old and older. Regarding the percentage of the lack of health services ( ), although positive, the relationships are not very strong for either age groups. The percentage of the population with dietary deficiency (
), although positive, the relationships are not very strong for either age groups. The percentage of the population with dietary deficiency ( ) also has a positive association with T2DM mortality, with increases of 1.2% and 0.9% in populations under 50 years of age and 50 years and older, respectively. On the other hand, an increase of one unit in GDP per capita (
) also has a positive association with T2DM mortality, with increases of 1.2% and 0.9% in populations under 50 years of age and 50 years and older, respectively. On the other hand, an increase of one unit in GDP per capita ( ) is associated with a decrease of 13.4% and 10.1% in the risk of T2DM mortality, respectively. Finally, a one-unit increase in the marginalization index (
) is associated with a decrease of 13.4% and 10.1% in the risk of T2DM mortality, respectively. Finally, a one-unit increase in the marginalization index ( ) is associated with an increase of approximately 0.3% in the risk of death from T2DM for the population under 50 years of age, and 3.4% for those 50 years and older.
) is associated with an increase of approximately 0.3% in the risk of death from T2DM for the population under 50 years of age, and 3.4% for those 50 years and older.
Table 1.
Summary statistics for T2DM mortality: posterior mean, posterior standard deviation (sd) and posterior 95% confidence interval for the fixed effects of the model (< 50 years of age), Mexico, 2020
| Mean | sd | 2.5% | 50% | 97.5% | |
|---|---|---|---|---|---|
Global intercept ( ) ) |
-0.666 | 0.544 | -1.744 | -0.662 | 0.391 |
Educational attainment ( ) ) |
0.013 | 0.003 | 0.006 | 0.013 | 0.020 |
Lack of health services ( ) ) |
0.001 | 0.002 | -0.002 | 0.001 | 0.005 |
Dietary deficiency ( ) ) |
0.012 | 0.002 | 0.008 | 0.012 | 0.016 |
GDP per capita ( ) ) |
-0.134 | 0.088 | -0.309 | -0.133 | 0.036 |
Marginalization index ( ) ) |
0.003 | 0.009 | -0.014 | 0.003 | 0.020 |
Table 2.
Summary statistics for T2DM mortality: posterior mean, posterior standard deviation (sd) and posterior 95% confidence interval for the fixed effects of the model (≥ 50 years of age), Mexico, 2020
| Mean | sd | 2.5% | 50% | 97.5% | |
|---|---|---|---|---|---|
Global intercept ( ) ) |
-2.376 | 0.308 | -2.982 | -2.376 | -1.773 |
Educational attainment ( ) ) |
0.002 | 0.002 | -0.001 | 0.002 | 0.006 |
Lack of health services ( ) ) |
0.006 | 0.001 | 0.004 | 0.006 | 0.008 |
Dietary deficiency ( ) ) |
0.009 | 0.001 | 0.007 | 0.009 | 0.011 |
GDP per capita ( ) ) |
-0.101 | 0.070 | -0.238 | -0.101 | 0.035 |
Marginalization index ( ) ) |
0.034 | 0.005 | 0.024 | 0.034 | 0.044 |
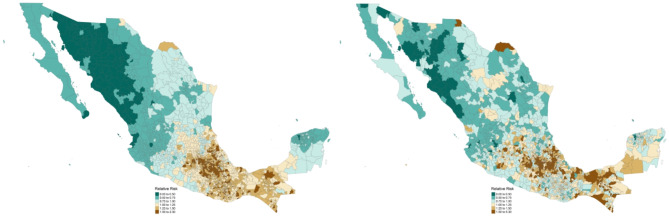
Figures 3 and 4 show the spatial distribution of the posterior mean of the specific relative risks,  , and their posterior probability of exceeding unity,
, and their posterior probability of exceeding unity,  , respectively. They should be interpreted as the residual RR for each municipality after the risk factors
, respectively. They should be interpreted as the residual RR for each municipality after the risk factors  ,
,  ,
,  ,
,  , and
, and  are considered.
are considered.
Fig. 3.
Posterior mean for relative risks of T2DM mortality by municipality in Mexico, 2020. Population under 50 years of age (left) and those 50 years old and older (right)
Fig. 4.
Posterior probability of T2DM mortality by municipality in Mexico, 2020. Population under 50 years of age (left) and those 50 years old and older (right)
The posterior mean of mortality from T2DM in 2020 (Fig. 3) exhibits well-defined spatial patterns, although it is more evident for the population under 50 years old (left). For this population age-group, the regions south of the Pacific Coast, The Bajío, Central Mexico, and south of the Yucatán Peninsula show RR > 1, indicating areas with higher risk than expected and, therefore, of greater interest. On the other hand, for the population 50 years old and older (right), there are more municipalities with exceptionally high risks (1.5 to 5.3), 341 out of 2,469 (13.8%), spreading from a central strip of Mexico to the Yucatán Peninsula.
The uncertainties in T2DM mortality risk in 2020 associated with the posterior means,  , are shown in Fig. 4. The colors show municipalities with high (red) and low (green) probabilities. Notably, an increased risk, characterized by posterior probabilities surpassing 0.8 (excess risk), can be observed in Central Mexico and in the states of Oaxaca, Chiapas, and Tabasco for the population under 50 years of age (left). On the other hand, for the population 50 years old and older (right), an excess risk can be seen in Central Mexico, extending along the cost of the Gulf of Mexico, and encompassing the states of Chiapas, Campeche, Tabasco (southeast).
, are shown in Fig. 4. The colors show municipalities with high (red) and low (green) probabilities. Notably, an increased risk, characterized by posterior probabilities surpassing 0.8 (excess risk), can be observed in Central Mexico and in the states of Oaxaca, Chiapas, and Tabasco for the population under 50 years of age (left). On the other hand, for the population 50 years old and older (right), an excess risk can be seen in Central Mexico, extending along the cost of the Gulf of Mexico, and encompassing the states of Chiapas, Campeche, Tabasco (southeast).
Discussion
The assessment and identification of spatial distribution patterns associated with uncommonly high or low relative risks of mortality and morbidity are crucial for informing effective public health policies. However, conventional methodologies, although straightforward and efficient, often overlook the inherent spatial interdependence among geographical units [36]. Acknowledging the significance of addressing this relationship, we examined the spatial patterns of T2DM mortality across municipalities in Mexico and explored the main contextual factors linked to this cause of death in 2020.
Overall, the Standardized Mortality Ratio (SMR) results (Fig. 2) revealed notable geographic and age-specific patterns. Central Mexico and Yucatán Peninsula exhibited the highest excess mortality rates. For the population under 50 years of age, municipalities in Oaxaca had the highest T2DM mortality rates, while those 50 years old and older experienced the highest rates in Tlaxcala and Puebla. Socioeconomic factors, such as low levels of educational attainment, lack of health services, dietary deficiency, and marginalization, were positively associated with increased T2DM mortality risk. In contrast, GDP per capita showed a negative association (Tables 1 and 2). High-risk areas for T2DM mortality were prominent along the south of the Pacific Coast, The Bajío, Central Mexico, and southern Yucatán for the younger population, and along a central strip extending to the Yucatán Peninsula for the older population. Significant uncertainties in mortality risk were identified, with Central Mexico, Oaxaca, Chiapas, and Tabasco showing high probabilities of excess risk for those under 50 years of age and extended risk areas along the Gulf of Mexico for those 50 years old and older (Figs. 3 and 4).
One of the main findings was that the high-risk areas for T2DM mortality were in municipalities in the states of Chiapas, Tabasco, Oaxaca, Puebla, Guerrero, Tlaxcala, and Veracruz. According to CONAPO [33], these states are characterized by high levels of marginalization. Furthermore, most of these states are characterized by low levels of overall educational attainment, high levels of food insecurity, and low levels of access to health services [38]. We also observed a relatively similar distribution of T2DM mortality risk among individuals under 50 years old and those 50 years old and older across municipalities in Mexico, although with a more homogeneous spatial pattern for the first age-group. This suggests that these states may harbor environments conducive to obesity and T2DM development, characterized by various factors that promote unhealthy lifestyles and elevated disease risk. These include high levels of marginalization, substandard diet quality, and limited access to healthcare services. Such conditions contribute to higher rates of obesity, a key risk factor for T2DM, leading to more severe disease progression and higher mortality rates owing to complications associated with poorly controlled diabetes.
We found that low levels of educational attainment are associated with higher risks of T2DM mortality. This finding aligns with existing research demonstrating that higher levels of education are associated with a reduced risk of developing T2DM and experiencing its complications [12, 14]. Lower levels of education may limit health literacy, which can lead to a poorer understanding of preventive measures, management strategies, and healthcare utilization related to T2DM [14]. This lower awareness may result in a delayed diagnosis, inadequate self-management, and higher mortality rates. Educational attainment also influences lifestyle behaviors that affect diabetes risk and mortality, such as diet quality, physical activity levels, and adherence to medical recommendations. Therefore, it is crucial to provide more educational resources to populations in high-risk regions to improve T2DM control [39].
We also found that a higher percentage of the population with dietary deficiencies had increased T2DM mortality. This finding aligns with other studies demonstrating that food availability [10] and food insecurity [25] are also associated with diabetes. Food insecurity often forces individuals to depend on low-cost, calorie-dense, nutrient-poor foods that are typically high in sugars, refined carbohydrates, and unhealthy fats [25]. These diets contribute to obesity and insulin resistance, which are primary risk factors for the development of T2DM. Poor access to healthy foods makes it difficult to maintain a healthy diet and has an adverse impact on diabetes care [12], which helps manage blood sugar levels. This can lead to poor glycemic control, increased complications, and higher mortality rates. Food availability, or lack thereof, is a significant source of chronic stress, which can contribute to the development of insulin resistance and T2DM. Chronic stress can lead to unhealthy eating behaviors, further increasing the risk of T2DM [40]. Moreover, heightened food insecurity impedes effective self-management diabetes. Stress associated with food insecurity may be related to a greater burden of diabetes [12].
An increase in municipal GDP per capita is associated with a decrease in the risk of T2DM mortality. As stated previously, GDP per capita is one of the most widely used socioeconomic predictors of mortality and health. This finding aligns with other studies that show that gross national per capita income is inversely linked to a rapidly growing trend of type 2 diabetes burden [5], that is, low- and middle-GDP areas have higher prevalence rates of T2DM [41, 42]. In areas with lower GDP, poor health awareness among diabetes patients often leads to significant delays in diagnosis and treatment, resulting in a severe burden of diabetes-related disability and complications [5]. People in these areas tend to have restricted access to high-quality nutritious foods, and instead consume high-calorie foods (often western-style), with low intake of fruits and vegetables, and high intake of sugar-sweetened beverages [43]. This can lead to obesity, accumulation of abdominal fat, and insulin resistance, which are strong risk factors for T2DM. In contrast, a higher GDP per capita usually correlates with better access to nutritious foods and positively impacts various health determinants crucial for the prevention and management of type 2 diabetes [42]. This leads to lower prevalence and better health outcomes in individuals with T2DM.
Finally, the results indicate that marginalization increases the risk of T2DM mortality. These outcomes align with those of other studies conducted in Mexico, which found that socioeconomic inequalities and higher rates of poverty are associated with a higher T2DM prevalence [44], and that the inequality gap in DM mortality between states has recently widened [45]. Marginalized populations often have reduced access to healthcare services, leading to delayed diagnosis and treatment of T2DM [46], and poorer compliance with diabetes treatment. This delay can result in more severe disease progression and higher mortality rates [47]. Economic constraints and limited access to healthy foods and recreational facilities can contribute to unhealthy diets and sedentary lifestyles, which are significant risk factors for T2DM [46]. Marginalized populations often face higher levels of stress owing to financial instability, unsafe living conditions, and social exclusion. Chronic stress can exacerbate the development of T2D [48], whereas financial barriers limit the ability to afford medications and regular medical check-ups, resulting in poor glycemic control and higher complication rates.
Limitations
The findings of this study should be interpreted with caution in light of these limitations. The first limitation concerns data quality and availability. We used municipal-level data that may suffer from underreporting or misreporting in death certificates, leading to underestimation of T2DM mortality rates. Advanced and chronic type 2 diabetes mellitus leads to complications such as renal and coronary diseases, which are often the direct causes of death. Consequently, these conditions may ultimately be recorded as the primary cause of death [13]. To minimize underreporting, it is essential to emphasize the importance of physicians accurately completing death certificates [49]. Second, working with smaller populations can lead to a higher variability in mortality rates, making it difficult to detect significant trends or differences. Third, the associations analyzed in this study are based on aggregated data. We were unable to infer all identified associations at the individual or local level, as we used municipal-level variables. Thus, while our findings align with other spatial-epidemiological studies on T2DM, it is important that future research confirms whether the associations observed at the ecological level also hold true at the individual level [24]. Fourth, the analyses were conducted for 2020, an exceptional year for overall mortality due to the impact of the COVID-19 pandemic. As a result, it is important to interpret our findings within this context. We also recommend that future studies revisit this analysis in the coming years.
Conclusion
In conclusion, this study on T2DM mortality in Mexico revealed statistically significant geographic patterns, with Central Mexico and the Yucatán Peninsula exhibiting the highest excess mortality rates. Socioeconomic factors, such as low levels of educational attainment, dietary deficiency, and marginalization, were positively associated with increased T2DM mortality risk, while GDP per capita showed a negative association. The Bayesian spatial model effectively captured spatial patterns of T2DM mortality. Despite limitations in data quality and availability, the findings highlight the crucial need to address T2DM risk factors at both individual and population levels to reduce the impact of this chronic disease in Mexico.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank Nina Ebner for her editing help.
Abbreviations
- BMY
Besag-York-Mollié
- CONAPO
Mexican Population Council
- CONEVAL
National Council for the Evaluation of Social Development Policy
- GDP
Gross domestic product
- INEGI
National Institute of Statistics and Geography of Mexico
- INLA
Integrated Nested Laplace Approximation
- RR
Relative risk
- SMR
Standardized Mortality Ratio
- T2DM
Type 2 diabetes mellitus
Author contributions
CADC contributed to the study design and the methodology, interpreted the results and prepared the original draft of the manuscript. EAB contributed to the study design and the methodology, performed the statistical analysis, interpreted the results and revised the manuscript. All authors approved the final version of the manuscript.
Funding
The authors declare that no funds was received during the preparation of this manuscript.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.IDF. Diabetes Atlas 10th edition. 2021 Brussels, Belgium: International Diabetes Federation (IDF). 2021 [ https://diabetesatlas.org/idfawp/resource-files/2021/07/IDF_Atlas_10th_Edition_2021.pdf
- 2.Zhu R, Zhou S, Xia L, Bao X. Incidence, morbidity and years lived with disability due to type 2 diabetes mellitus in 204 countries and territories: trends from 1990 to 2019. Front Endocrinol. 2022;13:905538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abdul Basith Khan M, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of type 2 diabetes—global burden of disease and forecasted trends. J Epidemiol Global Health. 2020;10(1):107–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Reviews Endocrinol. 2018;14(2):88–98. [DOI] [PubMed] [Google Scholar]
- 5.Liu J, Bai R, Chai Z, Cooper ME, Zimmet PZ, Zhang L. Low- and middle-income countries demonstrate rapid growth of type 2 diabetes: an analysis based on global burden of Disease 1990–2019 data. Diabetologia. 2022;65(8):1339–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arredondo A. Type 2 diabetes and health care costs in Latin America: exploring the need for greater preventive medicine. BMC Med. 2014;12:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barquera S, Hernández-Barrera L, Oviedo-Solís C, Rodríguez-Ramírez S, Monterrubio-Flores E, Trejo-Valdivia B, Martínez-Tapia B, Aguilar-Salinas C, Galván-Valencia O, Chávez-Manzanera E, Rivera-Dommarco J, Campos-Nonato I. Obesidad en adultos. Salud Publica Mex. 2024;66:414–24. [Google Scholar]
- 8.Gutiérrez-León E, Escamilla-Santiago RA, Martínez-Amezcua P, Bilal U, Lazo M, Ogaz-González R, et al. Trends and effect of marginalization on diabetes mellitus-related mortality in Mexico from 1990 to 2019. Sci Rep. 2022;12(1):9190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bello-Chavolla OY, Antonio-Villa NE, Fermín-Martínez CA, Fernández-Chirino L, Vargas-Vázquez A, Ramírez-García D, et al. Diabetes-related excess mortality in Mexico: a comparative analysis of National Death registries between 2017–2019 and 2020. Diabetes Care. 2022;45(12):2957–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siordia C, Saenz J, Tom SE. An introduction to macro- level spatial nonstationarity: a geographically weighted regression analysis of diabetes and poverty. Hum Geographies. 2012;6(2):5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen Y, Zhou X, Bullard KM, Zhang P, Imperatore G, Rolka DB. Income-related inequalities in diagnosed diabetes prevalence among US adults, 2001 – 2018. PLoS ONE. 2023;18(4):e0283450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hill-Briggs F, Adler NE, Berkowitz SA, Chin MH, Gary-Webb TL, Navas-Acien A, et al. Social Determinants Health Diabetes: Sci Rev Diabetes Care. 2020;44(1):258–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Montoya-Betancur KV, Caicedo-Velásquez B, Álvarez-Castaño LS. Exploratory spatial analysis of diabetes mortality and its relationship with the socioeconomic conditions of Colombian municipalities. Cadernos De saúde pública. 2020;36. [DOI] [PubMed]
- 14.Chiolero A, Faeh D, Paccaud F, Cornuz J. Consequences of smoking for body weight, body fat distribution, and insulin resistance1. Am J Clin Nutr. 2008;87(4):801–9. [DOI] [PubMed] [Google Scholar]
- 15.Hill JO, Galloway JM, Goley A, Marrero DG, Minners R, Montgomery B, et al. Scientific Statement: Socioecological determinants of Prediabetes and Type 2 diabetes. Diabetes Care. 2013;36(8):2430–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kouchaki E, Moraveji SA, Boojari H, Yaallah M, Behizad F, Rahimi H. The relationship of climate and diabetes mellitus prevalence with applying spatial analysis; an ecological study. Int Archives Health Sci. 2023;10(2):76–83. [Google Scholar]
- 17.Besag J, York J, Mollié A. Bayesian image restoration, with two applications in spatial statistics. Ann Inst Stat Math. 1991;43(1):1–20. [Google Scholar]
- 18.Banerjee S, Carlin BP, Gelfand AE. Hierarchical Modeling and Analysis for Spatial Data. Chapman and Hall/CRC; 2014.
- 19.Johnelle Sparks P, Sparks CS, Campbell JJA. An application of bayesian spatial statistical methods to the study of racial and poverty segregation and infant mortality rates in the US. GeoJournal. 2013;78(2):389–405. [Google Scholar]
- 20.Rue H, Martino S, Chopin N. Approximate bayesian inference for latent gaussian models by using Integrated Nested Laplace approximations. J Royal Stat Soc Ser B: Stat Methodol. 2009;71(2):319–92. [Google Scholar]
- 21.INEGI. Estadísticas de Defunciones Registradas Mexico City: Instituto Nacional de Estadística y Geografía (INEGI). 2024 [ https://www.inegi.org.mx/programas/edr/
- 22.CONAPO. Proyecciones de la Población de México y de las Entidades Federativas, 2020–2070 Mexico City: Consejo Nacional de Población (CONAPO). 2024 [ https://datos.gob.mx/busca/dataset/proyecciones-de-la-poblacion-de-mexico-y-de-las-entidades-federativas-2020-2070
- 23.CONEVAL. Medición de la pobreza Mexico City: Consejo Nacional de Evaluacion de la Politica de Desarrollo Social (CONEVAL). 2024 [ https://www.coneval.org.mx/Medicion/Paginas/PobrezaInicio.aspx
- 24.Kauhl B, Schweikart J, Krafft T, Keste A, Moskwyn M. Do the risk factors for type 2 diabetes mellitus vary by location? A spatial analysis of health insurance claims in Northeastern Germany using kernel density estimation and geographically weighted regression. Int J Health Geogr. 2016;15(1):38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sharma A. Exploratory spatial analysis of food insecurity and diabetes: an application of multiscale geographically weighted regression. Ann GIS. 2023;29(4):485–98. [Google Scholar]
- 26.Preston SH. The changing relation between Mortality and level of Economic Development. Popul Stud. 1975;29(2):231–48. [PubMed] [Google Scholar]
- 27.Murray CJL, Lopez AD. Alternative projections of mortality and disability by cause 1990–2013;2020: global burden of Disease Study. Lancet. 1997;349(9064):1498–504. [DOI] [PubMed] [Google Scholar]
- 28.Berger MC, Messer J. Public financing of health expenditures, insurance, and health outcomes. Appl Econ. 2002;34(17):2105–13. [Google Scholar]
- 29.Mackenbach JP, Martikainen P, Looman CWN, Dalstra JAA, Kunst AE, Lahelma E, et al. The shape of the relationship between income and self-assessed health: an international study. Int J Epidemiol. 2005;34(2):286–93. [DOI] [PubMed] [Google Scholar]
- 30.James SL, Gubbins P, Murray CJL, Gakidou E. Developing a comprehensive time series of GDP per capita for 210 countries from 1950 to 2015. Popul Health Metrics. 2012;10(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baptista EA, Queiroz BL. The relation between cardiovascular mortality and development: a study of small areas in Brazil, 2001–2015. Demographic Res. 2019;41:1437–52. [Google Scholar]
- 32.Baptista EA, Kakinuma K, Queiroz BL. Association between Cardiovascular Mortality and Economic Development: a spatio-temporal study for prefectures in Japan. Int J Environ Res Public Health [Internet]. 2020; 17(4). [DOI] [PMC free article] [PubMed]
- 33.CONAPO. Índice de Marginación municipal Mexico City: Consejo Nacional de Población (CONAPO). 2020 [ https://www.gob.mx/conapo/documentos/indices-de-marginacion-2020-284372
- 34.Court B, Cheng K. Pros and cons of standardised mortality ratios. Lancet (London England). 1995;346(8987):1432. [DOI] [PubMed] [Google Scholar]
- 35.Blangiardo M, Cameletti M, Baio G, Rue H. Spatial and spatio-temporal models with R-INLA. Spatial and spatio-temporal epidemiology. 2013;4:33–49. [DOI] [PubMed]
- 36.Blangiardo M, Cameletti M. Spatial and spatio-temporal bayesian models with. R-INLA: Wiley; 2015. [Google Scholar]
- 37.Johnson DP, Ravi N, Braneon CV. Spatiotemporal associations between Social Vulnerability, Environmental measurements, and COVID-19 in the Conterminous United States. GeoHealth. 2021;5(8):e2021GH000423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.CONEVAL, Información. de pobreza y evaluación en las entidades federativas y municipios Mexico City: Consejo Nacional de Evaluacion de la Politica de Desarrollo Social (CONEVAL); 2024 [ https://www.coneval.org.mx/coordinacion/entidades/Paginas/inicioent.aspx
- 39.Wu J, Wang Y, Xiao X, Shang X, He M, Zhang L. Spatial analysis of incidence of diagnosed type 2 diabetes Mellitus and its Association with obesity and physical inactivity. Front Endocrinol. 2021;12. [DOI] [PMC free article] [PubMed]
- 40.Keenan GS, Christiansen P, Hardman CA. Household Food Insecurity, Diet Quality, and obesity: an explanatory model. Obesity. 2021;29(1):143–9. [DOI] [PubMed] [Google Scholar]
- 41.Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, Das AK, et al. High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia. 2001;44(9):1094–101. [DOI] [PubMed] [Google Scholar]
- 42.Tang K, Wang H, Liu Y, Tan SH. Interplay of regional economic development, income, gender and type 2 diabetes: evidence from half a million Chinese. J Epidemiol Commun Health. 2019;73(9):867. [DOI] [PubMed] [Google Scholar]
- 43.Gittelsohn J, Trude A. Diabetes and obesity prevention: changing the food environment in low-income settings. Nutr Rev. 2017;75(suppl1):62–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Denova-Gutiérrez E, Vargas-Chanes D, Hernández S, Muñoz-Aguirre P, Napier D, Barquera S. Linking socioeconomic inequalities and type 2 diabetes through obesity and lifestyle factors among Mexican adults: a structural equations modeling approach. Salud Publica Mexico. 2020;62(2):192–202. [DOI] [PubMed] [Google Scholar]
- 45.Medina-Gómez OS, Peña JE. Inequalities in diabetes mortality in Mexico: 2010–2019. Gac Med Mex. 2023;159(2):113–8. [DOI] [PubMed] [Google Scholar]
- 46.Vanstone M, Rewegan A, Brundisini F, Giacomini M, Kandasamy S, DeJean D. Diet modification challenges faced by marginalized and nonmarginalized adults with type 2 diabetes: a systematic review and qualitative meta-synthesis. Chronic Illn. 2016;13(3):217–35. [DOI] [PubMed] [Google Scholar]
- 47.Barnard-Kelly KD, Cherñavvsky D. Social Inequality and Diabetes: a Commentary. Diabetes Therapy. 2020;11(4):803–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Madhu SV, Siddiqui A, Desai NG, Sharma SB, Bansal AK. Chronic stress, sense of coherence and risk of type 2 diabetes mellitus. Diabetes Metabolic Syndrome: Clin Res Reviews. 2019;13(1):18–23. [DOI] [PubMed] [Google Scholar]
- 49.Dias-Lima RA, Istilli PT, de Souza-Teixeira CR, Zanetti ML. da Costa Gonçalves-Torquato MT. Diabetes mellitus mortality in a municipality in the state of São Paulo, 2010 to 2014. Revista de Saúde Pública. 2019;53:24. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.