Abstract
Background
Gallstones are strongly associated with eating occasion (EO) and energy distribution, but few studies have addressed this aspect. Therefore, we utilize the data from 2017 to 2018 National Health and Nutrition Examination Survey (NHANES) to explore the association between temporal eating patterns and energy distribution patterns with the incidence of gallstones.
Methods
Our study comprised participants who completed the NHANES dietary intake interview and self-reported health questionnaire at age 20 or older. The self-report method for gallstones (have you ever been told by a doctor) was used. We use the latent class analysis (LCA) identified temporal eating patterns, and identified energy distribution patterns through latent profile analysis (LPA). The association between temporal eating patterns, energy distribution patterns, and gallstones was examined using logistic regression modeling.
Results
The study included a total of 4,692 participants. LCA identified four temporal eating patterns labeled as “Conventional,” “Early breakfast,” “Later breakfast,” and “Grazing.” Compared to the “Conventional” pattern, the “Early breakfast” pattern (OR 0.809, 95%CI 0.808–0.811) was associated with a reduced risk of gallstones, while the “Later breakfast” (OR 1.435, 95%CI 1.432–1.438) and “Grazing” (OR 1.147, 95%CI 1.145–1.148) patterns were associated with an increased risk of gallstones. LPA identified four energy distribution patterns labeled as “Guideline,” “High carbohydrates,” “Carbs-fat balance,” and “High fat.” The “High carbohydrates” pattern (OR 1.329, 95%CI 1.326–1.331) was associated with an increased risk of gallstones compared to the “Guideline” pattern. The “Carbs-fat balance” pattern (OR 0.877, 95%CI 0.876–0.879) and the “High fat” pattern (OR 0.848, 95%CI 0.846-0.850) were significantly and negatively associated with the risk of gallstones.
Conclusions
To summarize, inappropriate timing of eating and energy sources are associated with gallstones. As a dietary prevention measure for gallstones, we suggest adhering to a regular eating routine and avoiding overly casual and frequent food consumption. If the main EO routine occurs in the morning, this time should not exceed 9:00 a.m. Additionally, reducing carbohydrate intake and maintaining a moderate level of fat intake is believed to contribute to a lower risk of gallstones.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-20512-x.
Keywords: Gallstone, Eating occasion, Temporal eating patterns, NHANES, Macronutrients, Carbohydrate, Latent class analysis, Latent profile analysis
Introduction
Gallbladder stones represent one of the most prevalent gastrointestinal diseases, affecting approximately 10–15% of the adult population in the United States (U.S.) [1]. According to the National Health and Nutrition Examination Survey III [2], over 20 million American adults grapple with gallbladder stones, incurring an estimated cost exceeding $6 billion [3, 4]. The burden of gallstone disease in the United States is considerable and trending upward [5].
The formation of gallbladder stones results from a complex interplay of genetics, environmental factors, and lifestyle choices. Numerous studies have explored the risk factors associated with gallbladder stones, yet definitive conclusions remain elusive [6]. Unmodifiable risk factors include age, gender, race, and family history, while modifiable factors encompass obesity, comorbidities, diet, and physical activity [6]. Among these, diet emerges as a primary modifiable risk factor, drawing significant attention from researchers [6, 7]. A growing body of evidence links various foods (meat, nuts, fats, vegetables, coffee, etc [7]). and dietary patterns (such as the Western dietary pattern [8], Mediterranean dietary pattern [9], rice dietary pattern [10], etc.) to the development of gallbladder stones. Among the multitude of foods and nutrients studied, energy intake appears to be the sole identified risk factor [7, 11]. Excessive energy intake can lead to elevated BMI or obesity, subsequently influencing gallbladder stone formation through impaired gallbladder dynamics [12], insulin resistance, and abnormal lipid metabolism [13, 14]. Conversely, low energy intake resulting from skipped meals or rapid weight loss may increase bile cholesterol saturation and reduce the stimulation of the gallbladder, thereby affecting emptying and ultimately elevating the risk of stone formation [15].
Nevertheless, as research advances and the field of Chrono-nutrition gains prominence [16], it becomes evident that the quantity of energy intake alone does not entirely elucidate the relationship between energy and health outcomes. Inappropriately timed energy acquisition can contribute to adverse consequences such as weight gain, obesity, and metabolic disorders [17]. Notably, randomized clinical trials demonstrate that adjusting the temporal pattern of the diet may yield more significant benefits than altering the amount of energy intake [18].
Existing studies have primarily examined the relationship between the quantity of energy intake and gallbladder stones in isolation, which proves inadequate in explaining their association [7], especially considering that eating events at different times substantially influence gallbladder emptying [19]. The introduction of temporal eating patterns addresses this gap effectively, employing latent class analysis (LCA), a data-driven analytic approach, to explore the connection between the timing of food intake or Eating Occasions (EO) and health outcomes [20, 21]. Unlike prior studies that subjectively and arbitrarily assessed eating time periods [22], this approach enables the identification of distinctive temporal eating patterns from dietary data without the need for predefined eating times.
This study aims to employ the innovative approach of LCA to investigate the association between temporal eating patterns and the occurrence of gallbladder stones in U.S. adults. Furthermore, considering that energy intake is derived from the three major essential nutrients—carbohydrates, proteins, and fats—and the relationship between these nutrients and gallbladder stones remains a subject of controversy [23], we will utilize latent profile analysis (LPA) to delve deeper into the connection between energy distribution patterns and the presence of gallbladder stones.
Method
Data collection and research population
The data for our study were sourced from the 2017–2018 National Health and Nutrition Examination Survey (NHANES), a continuous survey administered by the National Center for Health Statistics (NCHS) at the Centers for Disease Control and Prevention (CDC) in the United States. In the 2017–2018 cycle, a total of 8,704 participants were initially enrolled. After excluding individuals with incomplete dietary data (n = 1,064), those below the age of 20 (n = 2,899), participants with missing information on gallbladder stones (n = 10) and pregnant (n = 39). This study ultimately included 4,692 eligible subjects.
Study variables
The prevalence of gallbladder stones in the subjects was assessed by the following questionnaire, “Have you ever been told you have gallstones?“. Additionally, our study collected information on various factors that could potentially influence the prevalence of gallbladder stones. These factors encompassed family demographic details, lifestyle habits, and self-reported health status (Supplementary Table 1).
Family demographic information included: sex (male/female), age (years), race (Mexican American, Other Hispanic, Non-Hispanic White, Non-Hispanic Black, Other race), marital status (Married, Widowed, Divorced, Separated, Never married, Living with partner), educational level (Less Than 9th Grade, 9-11th Grade, High School Grad/GED or Equivalent, Some College or AA degree, College Graduate or above), poverty income ratio (PIR, < 1.3, ≥ 1.3 and<3.5, ≥ 3.5). Drinking status is categorized as: never (had < 12 drinks in lifetime); former (had ≥ 12 drinks in 1 year and did not drink last year, or did not drink last year but drank ≥ 12 drinks in lifetime); mild (had ≥ 1 drinks per day for females, ≥ 2 drinks per day for males); moderate (had ≥ 2 drinks per day for females, ≥ 3 drinks per day for males, or binge drinking ≥ 2 days per month); heavy (had ≥ 3 drinks per day for females, ≥ 4 drinks per day for males). Smoking status is categorized as: never (smoked less than 100 cigarettes in life); former (smoked more than 100 cigarettes in life and smoke not at all now); now (smoked moth than 100 cigarettes in life and smoke some days or every day). Minutes sedentary activity per day (Minutes). Current medical conditions were based on self-reported outcomes including diabetes mellitus (yes/impaired fasting glucose (IFG)/no), hypertension (yes/no).
Dietary assessment
NHANES primarily employs the 24-hour Dietary Recall Interview (DRI) as its key dietary assessment method. This method gathers comprehensive data on all foods consumed by respondents over a 24-hour period, including the time of day each food item was consumed, measured in minutes [24]. We chose the first-day 24-h dietary recall for the subsequent analyses [25, 26].
To enhance the nutritional analysis, respondents’ dietary information was linked to the USDA Food and Nutrient Database for Dietary Studies (FNDDS), which serves as a repository of nutrient content [27]. The FNDDS encompasses information on thousands of food items, allowing us to determine the energy and nutrient content acquired by each respondent per meal using corresponding food codes. To facilitate analysis, the total amounts of carbohydrates, fats, and proteins consumed were initially measured in grams and then converted to kilocalories (kcal). Subsequently, these values were divided by the total energy intake over the course of the day, yielding the percentage of total energy contributed by each nutrient.
EO
EO was defined as any instance where the energy content of the consumed food or drink exceeded 50 kcal (210 KJ), and two consecutive EOs were separated by more than 15 min. To analyze EOs, we assessed each hour of the first day’s dietary data for eligible subjects. Subsequently, a dichotomous variable was generated to signify whether an EO occurred at each specific point in time [20].
Statistical analysis
Descriptive analysis
The data were processed using R 4.2.1 software, and subsequent descriptive analyses were carried out using SPSS 26.0 software. To address the intricate survey design of NHANES data, we adhered to the survey instructions and applied appropriate sampling weights. Participants were categorized into two groups based on the presence or absence of gallbladder stones. For quantitative data exhibiting a normal distribution, mean ± standard deviation (mean ± SD) was employed for description, and group differences were assessed using one-way analysis of variance (ANOVA). For quantitative data with non-normal distribution, values were expressed as median and quartiles [M (Q1, Q3)], and group comparisons were conducted using the Mann-Whitney U test. Categorical variables were described using percentages, and group comparisons were made using the chi-square test (χ2). Statistical significance was considered at P-values <0.05.
Latent classes of temporal eating patterns
Latent classes analysis (LCA) was conducted using M-Plus Version 8.3 (Muthen & Muthen, Los Angeles, CA, USA). LCA is a statistical technique designed for identifying latent categories based on categorical variables. In this study, a dichotomous categorical variable, EO, was created as an input variable for LCA by examining participants’ hourly energy intake. The LCA process involved initially testing models with two potential categories, followed by the gradual addition of more categories until determining the optimal number of potential categories. The final number of categories was determined through: (1) Evaluation of model fit metrics, including Akaike Information Criterion (AIC) and Bayesian Information Criterion (BIC), with a smaller value indicating a better model fit. (2) Lo-Mendell-Rubin Likelihood Ratio Test (LMRLRT) and Bootstrap Likelihood Ratio Test (BS-LRT), comparing k and k-1 class models, where k is the number of potential classes. (3) Model Interpretability [20]. These criteria collectively guided the selection of the most appropriate number of categories in the LCA model.
Latent profile of energy distribution patterns
LPA was conducted using M-Plus Version 8.3 (Muthen & Muthen, Los Angeles, CA, USA). LPA is a statistical technique utilized for identifying latent categories based on continuous variables. In this study, LPA was employed to discern participants’ energy distribution characteristics, considering three continuous variables: carbohydrate, protein, and fat ratios to total energy. Initially, models with two potential categories were tested, and additional categories were incrementally introduced until determining the optimal number. The final number of categories was established using the same criteria as for LCA.
Following these procedures, both LCA and LPA categorized the population into four distinct groups, determined as the most appropriate outcome. Subsequently, multivariate binary logistic regression was conducted, adjusting for confounding variables such as age, sex, ethnicity, marital status, education, poverty income ratio (PIR), alcohol consumption, smoking, sedentary time, diabetes, and hypertension. This regression aimed to investigate the association of temporal eating patterns and energy distribution patterns with gallbladder stones. The results were expressed through odds ratios (OR) and 95% confidence intervals (CI), with statistical significance set at P<0.05.
Results
Participants’ characteristics
The essential demographic characteristics of the participants are outlined in Table 1. The overall weighted prevalence of gallbladder stones stood at 11.4%, with prevalence rates of 16.0% for women and 6.4% for men. In comparison to the normal group, the population with gallbladder stones tended to be older, predominantly female, and exhibited a higher proportion of individuals being divorced or widowed. Moreover, this group displayed a lower prevalence of smoking and alcohol consumption, engaged in more sedentary behavior, and had a higher incidence of accompanying conditions such as hypertension and diabetes mellitus (P < 0.05).
Table 1.
Characteristics of the participants1
| Without gallstone | With gallstone | All | P-value | ||
|---|---|---|---|---|---|
| n | 4163 | 529 | 4692 | ||
| Age(year) 2 | 47.0 (32.0,61.0) | 59.0 (47.0,70.0) | 48.0 (33.0,62.0) | <0.001 | |
| Sex, % | |||||
| Female | 48.9 | 72.8 | 51.6 | <0.001 | |
| Male | 51.1 | 27.2 | 48.4 | ||
| Eth, % | |||||
| MA | 9.1 | 7.4 | 8.9 | ||
| NHB | 12.2 | 7.5 | 11.7 | ||
| NHW | 61.5 | 66.4 | 62.0 | ||
| OH | 6.8 | 6.6 | 6.8 | ||
| OR | 10.4 | 12.0 | 10.6 | ||
| Marital, % | <0.001 | ||||
| Married | 52.9 | 50.1 | 52.6 | ||
| Widowed | 4.9 | 14.4 | 6.0 | ||
| Divorced | 10.0 | 11.8 | 10.2 | ||
| Separated | 2.7 | 2.4 | 2.7 | ||
| Never married | 20.1 | 15.1 | 19.5 | ||
| Living with partner | 9.5 | 6.1 | 9.1 | ||
| Edu, % | <0.001 | ||||
| Less than 9th grade | 3.6 | 2.9 | 3.5 | ||
| 9-11th grade | 7.2 | 7.1 | 7.2 | ||
| High school graduate/GED or equivalent | 27.9 | 30.0 | 28.1 | ||
| Some college or AA degree | 30.5 | 34.7 | 31.0 | ||
| college graduate or above | 30.9 | 25.3 | 30.2 | ||
| PIR, % | <0.001 | ||||
| < 1.3 | 24.5 | 26.1 | 24.6 | ||
| ≥ 1.3, <1.5 | 30.9 | 37.1 | 31.6 | ||
| ≥ 3.5 | 44.6 | 36.8 | 43.7 | ||
| Sedentary time(min) 2 | 300.0 (180.0,480.0) | 360.0 (240.0,480.0) | 300.0 (180.0,480.0) | <0.001 | |
| Alcohol user, % | <0.001 | ||||
| Never | 8.2 | 10.9 | 8.5 | ||
| Mild | 45.5 | 45.8 | 45.5 | ||
| Moderate | 21.9 | 22.1 | 21.9 | ||
| Heavy | 24.4 | 21.2 | 24.1 | ||
| Smoke, % | <0.001 | ||||
| Never | 58.7 | 51.9 | 57.9 | ||
| Former | 23.9 | 33.2 | 24.9 | ||
| Now | 17.5 | 14.9 | 17.2 | ||
| Hypertension, % | <0.001 | ||||
| No | 61.7 | 41.5 | 59.4 | ||
| Yes | 38.3 | 58.5 | 40.6 | ||
| DM, % | <0.001 | ||||
| No | 79.4 | 65.0 | 77.8 | ||
| IFG | 6.4 | 8.3 | 6.7 | ||
| DM | 14.1 | 26.7 | 15.5 | ||
| Energy intake(kcal) 2 | 2001.0 (1486.0,2685.0) | 1770.0 (1325.0,2462.0) | 1984.0 (1468.0,2668.0) | <0.001 |
1All results were survey-weighted except for counts of categorical variables;
2Median (25%,75%)
PIR, Poverty income ratio; MA, Mexican American; OH, Other Hispanic; NHW, Non-Hispanic White; NHB, Non-Hispanic Black; OR, Other race; DM, Diabetes Mellitus; IFG, Impaired Fasting Glucose
Latent classes of temporal eating patterns
The model fit indices for LCA are outlined in Supplementary Table 2. Each categorization demonstrated statistical significance surpassing the previous one, and we opted for the four-category model for enhanced interpretability. The category labels are characterized based on the high or low probability of an EO occurring throughout the day. The four identified categories of temporal eating patterns are detailed in Fig. 1.
Fig. 1.
Conditional probabilities of eating occasion consumption across the day by latent class membership. Lines with a diamond represent the “Conventional” temporal eating pattern. Dashed lines with a triangle represent the “Later breakfast” temporal eating pattern. Lines with a square represent the “Conventional” temporal eating pattern. Dashed lines with a cross represent the “Grazing” temporal eating pattern
The first pattern, labeled “Conventional” pattern, exhibits three distinct peaks for breakfast (7:00), lunch (12:00), and dinner (16:00), aligning with traditional meal times. Both Class 2 and Class 3 demonstrate a very high probability (> 0.9) of EOs occurring specifically at breakfast time, with no significant probability of EOs occurring at any other time of the day. There is a 1-hour difference between the two classes, leading to the designation of Class 2 as “Early breakfast” pattern and Class 3 as “Later breakfast” pattern. In contrast, Class 4 is characterized by frequent but not significant peaks in the probability of EO occurrence (probability < 0.4 in all cases), earning the label “Grazing” pattern.
Table 2 shows the basic characteristics of each category. Participants in the “Conventional” pattern exhibited the highest percentage of males, the most favorable economic status, and the lowest incidence of hypertensive disease and diabetes compared to other categories (P<0.001).Participants in the “Early breakfast” pattern were older, more likely to be female, more likely to be married, possessed the highest educational attainment, fewer smokers and drinkers, higher rates of hypertension and diabetes, and lower rates of gallbladder stones (P<0.001). Participants following the “Later breakfast” pattern were the least educated, had the most sedentary behavior, and displayed the highest percentage of gallbladder stones (P<0.001). Participants in the “Grazing” pattern were younger, more likely to be unmarried or divorced, faced greater economic challenges, and had a higher proportion of smokers (P<0.001).
Table 2.
Characteristics of the participants by latent class of temporal eating patterns1
| Conventional | Early breakfast | Later breakfast | Grazing | P-value | |
|---|---|---|---|---|---|
| Variable | (n = 893) | (n = 1001) | (n = 863) | (n = 1935) | |
| Age(year) 2 | 50.0 (35.0,61.0) | 53.0 (36.0,66.0) | 49.0 (33.0,61.0) | 47.0 (32.0,60.0) | <0.001 |
| Sex, % | <0.001 | ||||
| Female | 47.2 | 56.3 | 52.7 | 51.0 | |
| Male | 52.8 | 43.7 | 47.3 | 49.0 | |
| Eth, % | <0.001 | ||||
| MA | 9.3 | 9.2 | 7.6 | 9.1 | |
| NHB | 7.9 | 10.0 | 13.1 | 13.6 | |
| NHW | 66.2 | 60.8 | 60.1 | 61.5 | |
| OH | 5.1 | 8.5 | 9.2 | 5.7 | |
| OR | 11.4 | 11.6 | 10.0 | 10.1 | |
| Marital, % | <0.001 | ||||
| Married | 57.3 | 61.0 | 53.2 | 46.0 | |
| Widowed | 4.1 | 8.7 | 4.8 | 6.0 | |
| Divorced | 9.6 | 9.5 | 9.0 | 11.4 | |
| Separated | 3.1 | 1.9 | 2.4 | 3.0 | |
| Never married | 18.8 | 11.5 | 21.9 | 22.6 | |
| Living with partner | 7.1 | 7.4 | 8.7 | 11.0 | |
| Edu, % | <0.001 | ||||
| Less than 9th grade | 3.7 | 3.4 | 4.6 | 3.0 | |
| 9-11th grade | 5.7 | 7.6 | 7.4 | 7.6 | |
| High school graduate/GED or equivalent | 24.2 | 23.5 | 31.2 | 30.8 | |
| Some college or AA degree | 32.2 | 30.2 | 29.9 | 31.2 | |
| college graduate or above | 34.2 | 35.2 | 26.9 | 27.4 | |
| PIR, % | <0.001 | ||||
| < 1.3 | 21.7 | 23.4 | 23.9 | 27.0 | |
| ≥ 1.3, <1.5 | 24.3 | 33.1 | 33.0 | 33.8 | |
| ≥ 3.5 | 54.0 | 43.5 | 43.1 | 39.2 | |
| Sedentary time(min) 2 | 300.0 (180.0,480.0) | 300.0 (180.0,480.0) | 300.0 (240.0,480.0) | 300.0 (180.0,480.0) | <0.001 |
| Alcohol user, % | <0.001 | ||||
| Never | 5.3 | 9.2 | 10.8 | 8.8 | |
| Mild | 48.7 | 49.2 | 46.3 | 41.9 | |
| Moderate | 22.4 | 24.0 | 16.3 | 23.1 | |
| Heavy | 23.6 | 17.6 | 26.6 | 26.2 | |
| Smoke, % | <0.001 | ||||
| Never | 59.5 | 63.3 | 57.4 | 54.8 | |
| Former | 24.0 | 24.8 | 26.1 | 24.9 | |
| Now | 16.5 | 11.9 | 16.5 | 20.3 | |
| Hypertension, % | <0.001 | ||||
| No | 63.5 | 53.4 | 56.9 | 61.5 | |
| Yes | 36.5 | 46.6 | 43.1 | 38.5 | |
| DM, % | <0.001 | ||||
| No | 80.0 | 75.5 | 76.5 | 78.5 | |
| IFG | 7.4 | 6.7 | 5.8 | 6.6 | |
| DM | 12.6 | 17.8 | 17.7 | 14.9 | |
| Energy intake(kcal) 2 | 2068.0 (1556.0,2807.0) | 2054.0 (1584.0,2655.0) | 2095.0 (1509.0,2751.0) | 1846.0 (1365.0,2584.0) | <0.001 |
| Gallstone, % | <0.001 | ||||
| No | 89.7 | 89.7 | 87.2 | 88.2 | |
| Yes | 10.3 | 10.3 | 12.8 | 11.8 |
1All results were survey-weighted except for counts of categorical variables
2Median (25%,75%)
PIR, Poverty income ratio; MA, Mexican American; OH, Other Hispanic; NHW, Non-Hispanic White; NHB, Non-Hispanic Black; OR, Other race; DM, Diabetes Mellitus; IFG, Impaired Fasting Glucose
Associations between temporal eating patterns and gallstone
In the unadjusted model, a significant positive correlation with gallbladder stones was observed in all other patterns compared to the “Conventional” model (P < 0.001). Upon adjusting for covariates in model 2, the odds ratio for the “Early breakfast” pattern was 0.809 (95% CI 0.808, 0.811), indicating a significant association with a reduced risk of gallbladder stones (P < 0.001). Conversely, both the “Later breakfast” and “Grazing” patterns were significantly and positively associated with gallbladder stones (P < 0.001), with odds ratios of 1.435 (95% CI 1.432, 1.438) and 1.147 (95% CI 1.145, 1.148), respectively (Table 3).
Table 3.
Odds ratios (OR) and 95% confidence intervals (CI) for gallstone according to temporal eating patterns 1
| Temporal eating patterns | n (%) | Model 1 | P-value | Model 2 | P-value |
|---|---|---|---|---|---|
| Conventional | 893 (19.9) | Ref. | Ref. | ||
| Early breakfast | 1001 (20.1) | 1.001(1.000,1.002) | 0.114 | 0.809(0.808,0.811) | <0.001 |
| Later breakfast | 863 (18.1) | 1.285(1.283,1.286) | <0.001 | 1.435(1.432,1.438) | <0.001 |
| Grazing | 1935 (41.9) | 1.166(1.165,1.168) | <0.001 | 1.147(1.145,1.148) | <0.001 |
1 All results were survey-weighted except for sample counts
Model 1: unadjusted; Model 2: adjusted by age, gender, race, marital, education level, poverty income ratio, smoke, alcohol user, sedentary time, hypertension, diabetes mellitus and energy intake
Latent profiles of energy distribution patterns
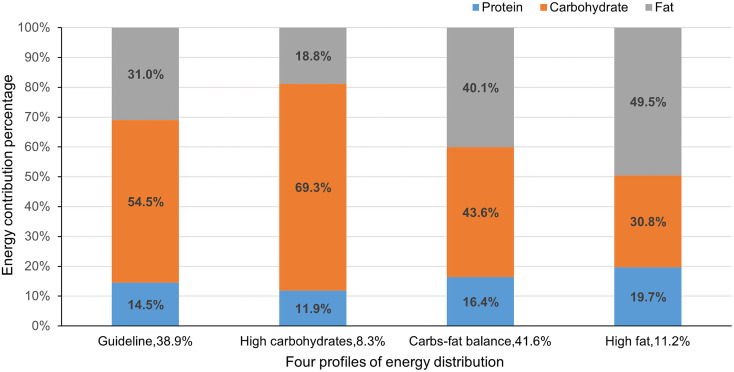
The model fit indices for LPA are presented in Supplementary Table 3. Each categorization demonstrated statistical significance compared to the previous one, and the four-category model were selected to improve interpretability finally. The characteristics of the category labels are based on the probability of how much the intake of carbohydrates, proteins, and fats contributes to the total energy during the day. Figure 2 depicts the four identified energy distribution patterns.
Fig. 2.
Four energy distribution patterns based on carbohydrate, protein, and fat percentages of energy
The distribution of the three macronutrients in the first model aligns with the Dietary Guidelines for Americans [28], hence labeled “Guideline” pattern. Participants in Class 2 derived 69.3% of their daily energy intake from carbohydrates, earning the designation “High carbohydrates” pattern. In Class 3, carbohydrate intake was slightly lower, and fat intake slightly higher, leading to the label “Carbs-fat balance” pattern. Class 4 participants predominantly sourced their energy from fat, constituting half of the daily energy intake and earning the label “High fat” pattern.
Table 4 outlines the fundamental characteristics of each identified energy distribution pattern. The major findings include: Participants following the “Guideline” pattern exhibited a lower prevalence of hypertension and more frequent alcohol consumption compared to other patterns (P < 0.001). Participants in the “High carbohydrates” pattern were prone to being divorced, better educated, higher income, and had higher rates of comorbid diabetes and gallbladder stones (P < 0.001). Participants in the “Carbs-fat balance” pattern were older, more likely to be married, less likely to smoke, and displayed higher rates of hypertension (P < 0.001). Participants in the “High fat” pattern had a poorer economic status, were more sedentary, smoke more frequently, and had lower rates of diabetes and gallstones (P < 0.001).
Table 4.
Characteristics of the participants by potential profile models of the energy contribution1
| Guideline | High carbohydrates | Carbs-fat balance | High fat | P-value | |
|---|---|---|---|---|---|
| Variable | (n = 1763) | (n = 394) | (n = 1956) | (n = 579) | |
| Age(year) 2 | 47.0 (32.0,62.0) | 48.0 (33.0,63.0) | 50.0 (35.0,62.0) | 47.0 (33.0,61.0) | <0.001 |
| Sex, % | <0.001 | ||||
| Female | 50.2 | 54.5 | 51.3 | 55.5 | |
| Male | 49.8 | 45.5 | 48.7 | 44.5 | |
| Eth, % | <0.001 | ||||
| MA | 8.2 | 9.5 | 9.2 | 9.7 | |
| NHB | 11.8 | 11.3 | 11.5 | 12.1 | |
| NHW | 63.7 | 63.8 | 60.7 | 59.8 | |
| OH | 6.9 | 5.3 | 7.2 | 6.0 | |
| OR | 9.4 | 10.1 | 11.4 | 12.5 | |
| Marital, % | <0.001 | ||||
| Married | 52.0 | 50.9 | 53.5 | 52.2 | |
| Widowed | 5.6 | 7.7 | 6.2 | 5.0 | |
| Divorced | 8.8 | 9.9 | 11.0 | 12.3 | |
| Separated | 2.2 | 3.9 | 2.4 | 4.7 | |
| Never married | 23.2 | 19.4 | 16.5 | 17.8 | |
| Living with partner | 8.2 | 8.2 | 10.4 | 8.0 | |
| Edu, % | <0.001 | ||||
| Less than 9th grade | 3.6 | 4.5 | 3.1 | 3.9 | |
| 9-11th grade | 7.0 | 6.9 | 6.7 | 9.7 | |
| High school graduate/GED or equivalent | 25.4 | 23.9 | 31.5 | 28.2 | |
| Some college or AA degree | 30.8 | 30.1 | 31.5 | 30.3 | |
| college graduate or above | 33.2 | 34.6 | 27.2 | 27.9 | |
| PIR, % | <0.001 | ||||
| < 1.3 | 24.1 | 27.2 | 23.8 | 27.7 | |
| ≥ 1.3, <1.5 | 30.0 | 23.8 | 33.2 | 37.0 | |
| ≥ 3.5 | 45.9 | 49.0 | 43.0 | 35.3 | |
| Sedentary time(min) 2 | 300.0 (180.0,480.0) | 300.0 (180.0,480.0) | 300.0 (240.0,480.0) | 360.0 (240.0,480.0) | <0.001 |
| Alcohol user, % | <0.001 | ||||
| Never | 8.1 | 6.7 | 9.3 | 8.2 | |
| Mild | 45.2 | 45.0 | 45.7 | 46.2 | |
| Moderate | 20.9 | 23.5 | 21.8 | 24.9 | |
| Heavy | 25.8 | 24.8 | 23.2 | 20.7 | |
| Smoke, % | <0.001 | ||||
| Never | 58.7 | 54.4 | 59.2 | 52.9 | |
| Former | 24.2 | 25.3 | 25.1 | 26.6 | |
| Now | 17.1 | 20.4 | 15.7 | 20.5 | |
| Hypertension, % | <0.001 | ||||
| No | 62.7 | 60.0 | 55.6 | 62.1 | |
| Yes | 37.3 | 40.0 | 44.4 | 37.9 | |
| DM, % | <0.001 | ||||
| No | 79.9 | 74.1 | 75.1 | 83.2 | |
| IFG | 5.7 | 8.5 | 7.8 | 4.2 | |
| DM | 14.3 | 17.4 | 17.1 | 12.6 | |
| Energy intake(kcal) 2 | 1973.0 (1438.5,2664.5) | 2103.0 (1514.0,2752.0) | 1913.0 (1397.0,2577.0) | 1842.0 (1466.0,2414.0) | <0.001 |
| Gallstone, % | <0.001 | ||||
| No | 88.0 | 82.0 | 88.9 | 89.4 | |
| Yes | 12.0 | 18.0 | 11.1 | 10.6 |
1All results were survey-weighted except for counts of categorical variables
2Median (25%,75%)
PIR, Poverty income ratio; MA, Mexican American; OH, Other Hispanic; NHW, Non-Hispanic White; NHB, Non-Hispanic Black; OR, Other race; DM, Diabetes Mellitus; IFG, Impaired Fasting Glucose
Association between energy distribution patterns and gallstones
In the unadjusted model, the “High carbohydrates” and “High fat” patterns were positively associated with the occurrence of gallbladder stones (P < 0.001), while the “Carbs-fat balance” pattern was negatively associated with the occurrence of gallbladder stones (P < 0.001). After adjusting for confounders, the “High carbohydrates” pattern was linked to an increased risk of gallbladder stones (P < 0.001), with an OR of 1.329 (95% CI 1.326, 1.331). In contrast, both the “Carbs-fat balance” and “High fat” patterns were significantly and negatively correlated with gallbladder stones (P < 0.001), with OR of 0.877 (95% CI 0.876, 0.879) and 0.848 (95% CI 0.846, 0.850), respectively (Table 5).
Table 5.
Odds ratios (OR) and 95% confidence intervals (CI) for gallstone according to energy distribution patterns 1
| Energy distribution patterns | n, % | Model 1 | P-value | Model 2 | P-value |
|---|---|---|---|---|---|
| Guideline | 1763 (38.9) | Ref. | Ref. | ||
| High carbohydrates | 394 (8.3) | 0.849(0.848,0.851) | <0.001 | 1.329(1.326,1.331) | <0.001 |
| Carbs-fat balance | 1956 (41.6) | 0.916(0.915,0.916) | <0.001 | 0.877(0.876,0.879) | <0.001 |
| High fat | 579 (11.2) | 0.871(0.870,0.873) | <0.001 | 0.848(0.846,0.850) | <0.001 |
1 All results were survey-weighted except for sample counts
Model 1: unadjusted; Model 2: adjusted by age, gender, race, marital, education level, poverty income ratio, smoke, alcohol user, sedentary time, hypertension, diabetes mellitus and energy intake
Association between energy distribution patterns and temporal eating patterns with gallstones
To comprehensively assess the relationship between eating time and macronutrients with the risk of gallbladder stones, a joint analysis of temporal eating patterns and energy distribution patterns was conducted (Table 6). In the unadjusted model, the “Carbs-fat balance” pattern was negatively associated with the occurrence of gallbladder stones (P < 0.001), while the remaining temporal eating patterns and energy distribution patterns were positively associated with the occurrence of gallbladder stones (P < 0.001).
Table 6.
Association of temporal eating patterns and energy distribution patterns with gallstones 1
| Joint analysis | n (%) | Model 1 | P-value | Model 2 | P-value |
|---|---|---|---|---|---|
| Temporal eating patterns | |||||
| Conventional | 893 (19.9) | Ref. | Ref. | ||
| Early breakfast | 1001 (20.1) | 0.849(0.848,0.850) | <0.001 | 0.883(0.881,0.884) | <0.001 |
| Later breakfast | 863 (18.1) | 0.856(0.855,0.857) | <0.001 | 1.384(1.382,1.387) | <0.001 |
| Grazing | 1935 (41.9) | 1.102(1.100,1.103) | <0.001 | 1.105(1.104,1.107) | <0.001 |
| Energy distribution patterns | |||||
| Guideline | 1763 (38.9) | Ref. | Ref. | ||
| High carbohydrates | 394 (8.3) | 0.832(0.831,0.833) | <0.001 | 1.205(1.203,1.207) | <0.001 |
| Carbs-fat balance | 1956 (41.6) | 0.915(0.914,0.916) | <0.001 | 0.915(0.914,0.917) | <0.001 |
| High fat | 579 (11.2) | 0.862(0.861,0.864) | <0.001 | 0.820(0.818,0.821) | <0.001 |
1 All results were survey-weighted except for sample counts
Model 1: unadjusted; Model 2: adjusted by age, gender, race, marital, education level, poverty income ratio, smoke, alcohol user, sedentary time, hypertension, diabetes mellitus and energy intake
After adjusting for confounders, the results remained consistent with those of the separate analyses. Among the temporal eating patterns, the “Early breakfast” pattern was negatively associated with the occurrence of gallbladder stones (P < 0.001), while the “Later breakfast” pattern and the “Grazing” pattern were positively associated with the occurrence of gallbladder stones (P < 0.001). Among the energy distribution patterns, the “High carbohydrates” pattern was associated with an increased risk of gallbladder stones (P < 0.001), whereas the “Carbs-fat balance” and “High fat” patterns were associated with a decreased risk of gallbladder stones (P < 0.001).
Subgroup analysis
To assess the stability of the results, subgroup analyses were conducted (Supplementary Tables 4 and Supplementary Table 5). Notably, the “Grazing” pattern in the temporal eating patterns exhibited varying effects in the gender groups. In the male group, the “Grazing” pattern displayed a negative association with the occurrence of gallbladder stones, with an OR of 0.917 (95% CI 0.915, 0.920). Additionally, the “Early breakfast” pattern indicated an increased risk of gallbladder stones in the age subgroup of individuals over 60 years, with an OR (95% CI) of 1.579 (1.592, 1.603). Conversely, the energy distribution patterns remained relatively stable, showing no differential effects in either age or sex subgroups.
Discussion
The present study employed LCA and LPA, introducing a novel approach to investigate, for the first time, the relationship between temporal eating patterns and energy distribution patterns with gallbladder stones in a representative sample of adults from the United States (U.S.). The primary temporal eating patterns, namely “Conventional,” “Early breakfast,” “Later breakfast,” and “Grazing,” were identified among American adults in this study through LCA. The “Grazing” pattern, marked by frequent and random EOs, is associated with an elevated risk of gallbladder stones. Both the “Early breakfast” and “Later breakfast” patterns exhibited an early morning peak in EO. The findings suggested that the “Later breakfast” pattern, characterized by a delayed morning eating event, increased the risk of gallbladder stones, whereas the “Early breakfast” pattern, featuring an earlier main eating event, was linked to a reduced risk of gallbladder stones. Furthermore, four prominent energy distribution patterns - “Guideline,” “High carbohydrates,” “Carbs-fat balance,” and “High fat” - were identified among U.S. adults through LPA. The “High carbohydrate” pattern, involving obtaining energy mainly from carbohydrates throughout the day, was associated with an increased risk of developing gallstones. Conversely, reducing carbohydrates and increasing the proportion of fat might have been correlated with a decreased risk of gallstones. This comprehensive analysis provided valuable insights into the intricate interplay between temporal eating patterns, energy distribution, and the risk of gallbladder stones in the U.S. adult population.
Two studies [19, 29] indicated that prolonged overnight fasting was associated with an increased risk of gallbladder stones. The present study aligned with this finding, as the “Later breakfast” pattern exhibits EO peaks later, and the timing of dinner largely overlapped in different patterns, suggesting that longer overnight fasting times elevated the risk of gallbladder stones. Prolonged fasting contributed to the retention of cholesterol oversaturated bile, thereby promoting the formation of gallbladder stones [30]. Contrary to this, a recent study from China did not find a significant association between overnight fasting time and gallbladder stones [31]. However, it was worth noting that this study did not consider the frequency of overnight fasting times and lacked dietary data for most of the daytime, potentially limiting its ability to fully capture the relationship between eating habits and gallbladder stones. Unlike this study, our research encompassed the timing of each meal throughout the day and avoided isolating the effect of eating at a specific time of day on gallbladder stones.
We also observed that the “Early breakfast” and “Later breakfast” patterns, characterized by an EO peak during the breakfast period, had the main eating event (EO peak) earlier compared to the “Conventional” pattern. While many intermittent fasting programs have demonstrated varying degrees of metabolic and disease benefits [32], this was not universally applicable. Despite the earlier EO peak, there was a 1–2 h delay in the timing of the first meal for both the “Early breakfast” and “Later breakfast” patterns. The “Later breakfast” pattern exhibited an even greater delay, influencing the timing of subsequent meals with delayed EO peaks for both lunch and dinner. From a “Chrono-nutrition” perspective [33], a delayed eating window was associated with reduced insulin sensitivity, obesity, and metabolic syndrome, which may have indirectly contributed to gallbladder stone formation. It was noteworthy that studies related to intermittent eating often involved randomized clinical trials with strict limits on participants’ energy intake and eating time window, making it challenging for the general population to replicate such conditions. This may have explained why participants in the “Later breakfast” pattern, despite having earlier major eating events, did not experience the anticipated benefits. Therefore, individuals whose primary eating time was during the breakfast period should have aimed to finish by 9:00 a.m., and attention should have been given to the timing of subsequent lunches and dinners.
Early studies suggested that reducing meal frequency might have increased the likelihood of gallstone formation [19], but our findings indicated that the frequent, unstructured eating pattern of “Grazing” did not confer benefits. Despite the promotion of gallbladder emptying by frequent meals, this pattern was associated with a significant metabolic burden [34]. Moreover, it led to an increase in daily calorie intake and a decrease in diet quality [35], possibly evolving into a pathological subtype of “compulsive” grazing [36], which could have had serious consequences for both physical and mental health. In our study, 41.8% of participants exhibited the “Grazing” pattern, reflecting a prevalent behavior. A cross-sectional study in a representative Australian population found that up to 48.2% of participants engaged in grazing behaviors in their diet [37]. Given the close association of the “Grazing” pattern with various major public health issues, further research is urgently needed to elucidate the health impacts of the “Grazing” pattern or grazing behaviors in the future.
Our results suggested that a high proportion of carbohydrates as a source of daily energy intake was particularly important for the development of gallbladder stones, and this finding remained consistent across participants of different genders and ages. The consumption of excessive carbohydrates can contribute to the formation of gallbladder stones through various pathways. These included increasing biliary cholesterol saturation [38], decreasing gallbladder volume [39], shortening the time for cholesterol crystal formation, and increasing the mass of the crystals [39]. Additionally, it might have caused steatocholecystitis leading to biliary dyskinesia [40]. Furthermore, insulin resistance, identified as an independent risk factor for gallbladder stones [41], was more significantly influenced by a high-carbohydrate diet than by a diet high in monounsaturated fats [42]. However, it was crucial to note that the impact of carbohydrates on chronic disease extended beyond the percentage of dietary energy, and the type of carbohydrate was equally important [43]. Differentiating between “good carbs” and “bad carbs” was essential, as failure to do so might have explained why some studies did not find a consistent association between carbohydrates and gallbladder stones [44]. For instance, a prospective study of pregnant women discovered that high fructose intake increased the risk of gallbladder stones, and this association was not solely related to total carbohydrate intake [45]. Additionally, this study noted no association between starch, sucrose, lactose, or galactose intake and the risk of gallbladder disease, which was not entirely consistent with recent findings. Excessive dietary levels of simple carbohydrates, including glucose, fructose, lactose, galactose, and maltose, were found to be associated with an increased risk of gallbladder stones in a cross-sectional Mexican study [46]. Therefore, further research is needed to explore the specific effects of different types of carbohydrates on gallbladder stones.
The role of fat in gallbladder stones was as controversial as that of carbohydrates, and our results suggested that increasing the proportion of fat might have helped prevent gallbladder stones. Some studies have indicated that maintaining a certain amount of dietary fat intake can significantly reduce the risk of gallstones during rapid weight loss by promoting gallbladder emptying and avoiding gallbladder stasis [47, 48]. Additionally, a recent (in 2023) 6-month randomized controlled trial [49] noted that a high-fat, low-carbohydrate diet (50–60% of energy from fat and less than 20% of energy from carbohydrates) was significantly more effective than a high-carbohydrate, low-fat diet (20–30% of energy from fat and 50–60% of energy from carbohydrates) in terms of improving glycemic control and weight reduction. Furthermore, a high-carb diet (60% carbohydrate, 25% fat) rather than a high-fat diet (40% carbohydrate, 45% fat) significantly elevated fasting plasma triglycerides [50].
Meat, a major source of fat, has been found to be positively associated with the risk of gallbladder stones in some past studies [51–53]. A 2017 case-control study in South Korea similarly noted that a dietary pattern characterized by large amounts of meat increased the risk of gallbladder stones [54]. However, it should be noted that this dietary pattern also included fried foods and had a factor loading of 0.799. Trans fatty acids in fried foods significantly increased plasma triglycerides and decreased plasma HDL cholesterol levels [55], as well as decreased gallbladder sensitivity to cholecystokinin and impair gallbladder motility [56]. Therefore, both cooking methods and types of lipids should have received more attention. Overall, the effects of dietary fats and carbohydrates on obesity, glycemia, lipids, and chronic diseases remain ambiguous [57], but our results need to be viewed with caution in light of the large body of evidence demonstrating the harms of consuming too much fat.
Interestingly, subgroup analyses revealed that men did not seem to be affected by the negative effects of the “Grazing” pattern. In a large cross-sectional study in Korea [58], meal frequency was found to be negatively associated with the prevalence of abdominal obesity, elevated blood pressure, and elevated triglycerides in men, but not in women. Furthermore, all the remaining temporal eating patterns posed a higher risk of gallbladder stones in older adults over the age of 60 compared to “Conventional” patterns. In a short-term pilot study, time-restricted eating improved functional capacity (endurance) and glucose tolerance in middle-aged and older adults but increased their total cholesterol and LDL cholesterol compared to normal feeding [59]. Similar findings have been reported in long-term randomized clinical trials [60] and animal trials [61]. This might be one of the reasons why temporal eating patterns increase the risk of gallbladder stones in the elderly, but the mechanism still requires further study.
In conclusion, our study marked the first investigation into the association of temporal eating patterns and energy distribution patterns with gallbladder stone risk in U.S. adults. The study held several strengths, with NHANES providing a representative sample of Americans through careful sampling and strict study protocols ensuring reliable quality control. Our novel approach not only reduced the loss of dietary data but also rendered the results more objective and comprehensive, offering insights into the dietary characteristics and patterns of the sample population. However, there were some limitations to our study, namely that, being a cross-sectional study, it couldn’t establish a causal relationship between temporal eating patterns, energy distribution patterns, and gallbladder stones. Second, the diagnosis of gallbladder stones relied on questionnaires, potentially introducing recall bias. Third, although LCA and LPA offered advantages as relatively novel methods, being data-driven exploratory analyses, their applicability to other populations might have had limitations. Also, O’Hara et al. [62] emphasized that the extent to which different methods affect the results is not yet known, and therefore comparisons with other methods should be made with great caution. Due to this concern, we did not compare the effects of the different methods on creating temporal dietary patterns. More studies using multiple methods for simultaneous analysis are needed in the future to help researchers understand the differences between methodologies.
Conclusion
In conclusion, our study reveals significant associations between temporal eating patterns identified through the LCA method, energy distribution patterns characterized by the LPA method, and the risk of developing gallbladder stones. In short, to prevent gallbladder stones, it is advisable to maintain a regular diet, avoid random and frequent eating, and, if the primary eating occasions habitually occur in the morning, ensure this time does not extend beyond 9:00 a.m. Moreover, reducing carbohydrate intake while maintaining a certain level of fat intake is deemed beneficial in mitigating the risk of gallbladder stones. Future research should delve into the nuanced relationship between different nutrient types and gallbladder stones.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Acknowledgements
We sincerely thank Zhang Jing (Second Department of Infectious Disease, Shanghai Fifth People’s Hospital, Fudan University) for his work on the NHANES database. His outstanding work, nhanesR package and webpage, makes it easier for us to explore NHANES database.
Abbreviations
- NHANES
National Health and Nutrition Examination Survey
- EO
Eating Occasion
- LCA
Latent Class Analysis
- LPA
Latent Profile Analysis
- PIR
Poverty Income Ratio
- MA
Mexican American
- OH
Other Hispanic
- NHW
Non-Hispanic White
- NHB
Non-Hispanic Black
- OR
Other Race
- DM
Diabetes Mellitus
- IFG
Impaired Fasting Glucose
- OR
Odds Ratios
- CI
Confidence Intervals
Author contributions
Conceptualization and design, Z.H., L.S., C.W. and H.Z.; methodology, L.S.; software, C.X., J.Z.; formal analysis, H.Z., C.X., N.Y., X.Z., Z.L. and L.S.; data curation, J.Y. and Q.P.; draft, H.Z.; review and editing, H.Z. and L.S.; supervision, D.W, Y.S., L.S. and Z.H. All authors have read and agreed to the published version of the manuscript.
Funding
None.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethical approval
As the data used in this study were obtained from publicly available NHANES data, all data-related research had previously received approval from their respective ethical review committees and had obtained written informed consent from the participants. Consequently, this study does not require additional ethical approval.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Huan Zhang and Chao Xu contributed equally to this work and share first authorship.
Lei Shang and Zheyi Han contributed equally to this work and share last authorship.
Contributor Information
Lei Shang, Email: shanglei@fmmu.edu.cn.
Zheyi Han, Email: zheyihan_fmmu@163.com.
References
- 1.Stinton LM, Myers RP, Shaffer EA. Epidemiology of gallstones. Gastroenterol Clin North Am. 2010;39(2):157–69. vii. [DOI] [PubMed] [Google Scholar]
- 2.Everhart JE, Khare M, Hill M, Maurer KR. Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology. 1999;117(3):632–9. [DOI] [PubMed] [Google Scholar]
- 3.Wilkins T, Agabin E, Varghese J, Talukder A. Gallbladder Dysfunction: Cholecystitis, Choledocholithiasis, Cholangitis, and Biliary Dyskinesia. Prim Care. 2017;44(4):575–97. [DOI] [PubMed] [Google Scholar]
- 4.Pisano M, Allievi N, Gurusamy K, Borzellino G, Cimbanassi S, Boerna D, Coccolini F, Tufo A, Di Martino M, Leung J, et al. 2020 World Society of Emergency Surgery updated guidelines for the diagnosis and treatment of acute calculus cholecystitis. World J Emerg Surg. 2020;15(1):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li ZZ, Guan LJ, Ouyang R, Chen ZX, Ouyang GQ, Jiang HX. Global, regional, and national burden of gallbladder and biliary diseases from 1990 to 2019. World J Gastrointest Surg. 2023;15(11):2564–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pak M, Lindseth G. Risk Factors for Cholelithiasis. Gastroenterol Nurs. 2016;39(4):297–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Di Ciaula A, Garruti G, Fruhbeck G, De Angelis M, de Bari O, Wang DQ, Lammert F, Portincasa P. The Role of Diet in the Pathogenesis of Cholesterol Gallstones. Curr Med Chem. 2019;26(19):3620–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barre A, Gusto G, Cadeau C, Carbonnel F, Boutron-Ruault MC. Diet and Risk of Cholecystectomy: A Prospective Study Based on the French E3N Cohort. Am J Gastroenterol. 2017;112(9):1448–56. [DOI] [PubMed] [Google Scholar]
- 9.Wirth J, Song M, Fung TT, Joshi AD, Tabung FK, Chan AT, Weikert C, Leitzmann M, Willett WC, Giovannucci E, et al. Diet-quality scores and the risk of symptomatic gallstone disease: a prospective cohort study of male US health professionals. Int J Epidemiol. 2018;47(6):1938–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nie C, Yang T, Wang Z, Suolang D, Wang S, Baima K, Wei L, Ling H, Liu L, Zeng Q, et al. Dietary Patterns and Gallstone Risks in Chinese Adults: A Cross-sectional Analysis of the China Multi-Ethnic Cohort Study. J Epidemiol. 2023;33(9):471–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kazi FN, Ghosh S, Sharma JVP, Saravanan S, Patil S. Trends in Gallbladder Disease in Young Adults: A Growing Concern. Cureus. 2022;14(8):e28555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mathus-Vliegen EM, Van Ierland-Van Leeuwen ML, Terpstra A. Determinants of gallbladder kinetics in obesity. Dig Dis Sci. 2004;49(1):9–16. [DOI] [PubMed] [Google Scholar]
- 13.Portincasa P, Moschetta A, Palasciano G. Cholesterol gallstone disease. Lancet. 2006;368(9531):230–9. [DOI] [PubMed] [Google Scholar]
- 14.Stender S, Nordestgaard BG, Tybjaerg-Hansen A. Elevated body mass index as a causal risk factor for symptomatic gallstone disease: a Mendelian randomization study. Hepatology. 2013;58(6):2133–41. [DOI] [PubMed] [Google Scholar]
- 15.Festi D, Colecchia A, Larocca A, Villanova N, Mazzella G, Petroni ML, Romano F, Roda E. Review: low caloric intake and gall-bladder motor function. Aliment Pharmacol Ther. 2000;14(Suppl 2):51–3. [DOI] [PubMed] [Google Scholar]
- 16.Almoosawi S, Vingeliene S, Gachon F, Voortman T, Palla L, Johnston JD, Van Dam RM, Darimont C, Karagounis LG. Chronotype: Implications for Epidemiologic Studies on Chrono-Nutrition and Cardiometabolic Health. Adv Nutr. 2019;10(1):30–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van der Merwe C, Munch M, Kruger R. Chronotype Differences in Body Composition, Dietary Intake and Eating Behavior Outcomes: A Scoping Systematic Review. Adv Nutr. 2022;13(6):2357–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Galindo Munoz JS, Gomez Gallego M, Diaz Soler I, Barbera Ortega MC, Martinez Caceres CM, Hernandez Morante JJ. Effect of a chronotype-adjusted diet on weight loss effectiveness: A randomized clinical trial. Clin Nutr. 2020;39(4):1041–8. [DOI] [PubMed] [Google Scholar]
- 19.Capron JP, Delamarre J, Herve MA, Dupas JL, Poulain P, Descombes P. Meal frequency and duration of overnight fast: a role in gall-stone formation? Br Med J (Clin Res Ed). 1981;283(6304):1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leech RM, Worsley A, Timperio A, McNaughton SA. Temporal eating patterns: a latent class analysis approach. Int J Behav Nutr Phys Act. 2017;14(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leech RM, Timperio A, Livingstone KM, Worsley A, McNaughton SA. Temporal eating patterns: associations with nutrient intakes, diet quality, and measures of adiposity. Am J Clin Nutr. 2017;106(4):1121–30. [DOI] [PubMed] [Google Scholar]
- 22.Almoosawi S, Prynne CJ, Hardy R, Stephen AM. Time-of-day of energy intake: association with hypertension and blood pressure 10 years later in the 1946 British Birth Cohort. J Hypertens. 2013;31(5):882–92. [DOI] [PubMed] [Google Scholar]
- 23.Mathew LK, Ko C. Dietary fat and protein intake are not associated with incident biliary sludge and stones during pregnancy. JPEN J Parenter Enter Nutr. 2015;39(1):124–8. [DOI] [PubMed] [Google Scholar]
- 24.Nhanes - what we eat in America. Centers for Disease Control and Prevention 2015. (accessed February 5, 2024). [https://www.cdc.gov/nchs/nhanes/wweia.htm]
- 25.Aqeel MM, Guo J, Lin L, Gelfand SB, Delp EJ, Bhadra A, Richards EA, Hennessy E. Eicher-Miller HA: Temporal Dietary Patterns Are Associated with Obesity in US Adults. J Nutr. 2020;150(12):3259–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lin L, Guo J, Li Y, Gelfand SB, Delp EJ, Bhadra A, Richards EA, Hennessy E, Eicher-Miller HA. The Discovery of Data-Driven Temporal Dietary Patterns and a Validation of Their Description Using Energy and Time Cut-Offs. Nutrients 2022, 14(17). [DOI] [PMC free article] [PubMed]
- 27.Group FSR. Food and nutrient database for dietary studies (FNDDS). Figshare 2023.(accessed February 5, 2024). [https://data.nal.usda.gov/dataset/food-and-nutrient-database-dietary-studies-fndds]
- 28.Phillips JA. Dietary Guidelines for Americans, 2020–2025. Workplace Health Saf. 2021;69(8):395. [DOI] [PubMed] [Google Scholar]
- 29.Attili AF, Scafato E, Marchioli R, Marfisi RM, Festi D. Diet and gallstones in Italy: the cross-sectional MICOL results. Hepatology. 1998;27(6):1492–8. [DOI] [PubMed] [Google Scholar]
- 30.Nakano K, Chijiiwa K, Noshiro H, Hirota I, Yamasaki T. Human gallbladder bile becomes lithogenic during short-term intravenous hyperalimentation. J Surg Res. 1992;53(4):396–401. [DOI] [PubMed] [Google Scholar]
- 31.Zhihong W, Jiayi L, Surong H, Bo T, Tao H, Wei L, Xiaodong H. Analysis of influencing factors for the development of gallstone in population of Beijing. Chin J Dig Surg. 2022;21(7):910. [Google Scholar]
- 32.de Cabo R, Mattson MP. Effects of Intermittent Fasting on Health, Aging, and Disease. N Engl J Med. 2019;381(26):2541–51. [DOI] [PubMed] [Google Scholar]
- 33.Franzago M, Alessandrelli E, Notarangelo S, Stuppia L, Vitacolonna E. Chrono-Nutrition: Circadian Rhythm and Personalized Nutrition. Int J Mol Sci 2023, 24(3). [DOI] [PMC free article] [PubMed]
- 34.Overby NC, Margeirsdottir HD, Brunborg C, Dahl-Jorgensen K, Andersen LF, Norwegian Study Group for Childhood D. Sweets, snacking habits, and skipping meals in children and adolescents on intensive insulin treatment. Pediatr Diabetes. 2008;9(4 Pt 2):393–400. [DOI] [PubMed] [Google Scholar]
- 35.Zeballos E, Chelius C. The effects of grazing on daily caloric intake and dietary quality. Int J Behav Nutr Phys Act. 2021;18(1):163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heriseanu AI, Hay P, Corbit L, Touyz S. Grazing in adults with obesity and eating disorders: A systematic review of associated clinical features and meta-analysis of prevalence. Clin Psychol Rev. 2017;58:16–32. [DOI] [PubMed] [Google Scholar]
- 37.Heriseanu AI, Hay P, Touyz S. Grazing behaviour and associations with obesity, eating disorders, and health-related quality of life in the Australian population. Appetite. 2019;143:104396. [DOI] [PubMed] [Google Scholar]
- 38.Thornton JR, Emmett PM, Heaton KW. Diet and gall stones: effects of refined and unrefined carbohydrate diets on bile cholesterol saturation and bile acid metabolism. Gut. 1983;24(1):2–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mathur A, Megan M, Al-Azzawi HH, Lu D, Swartz-Basile DA, Nakeeb A, Pitt HA. High dietary carbohydrates decrease gallbladder volume and enhance cholesterol crystal formation. Surgery. 2007;141(5):654–9. [DOI] [PubMed] [Google Scholar]
- 40.Mathur A, Al-Azzawi HH, Lu D, Yancey KW, Swartz-Basile DA, Nakeeb A, Pitt HA. Steatocholecystitis: the influence of obesity and dietary carbohydrates. J Surg Res. 2008;147(2):290–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chang Y, Sung E, Ryu S, Park YW, Jang YM, Park M. Insulin resistance is associated with gallstones even in non-obese, non-diabetic Korean men. J Korean Med Sci. 2008;23(4):644–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Garg A, Bonanome A, Grundy SM, Zhang ZJ, Unger RH. Comparison of a high-carbohydrate diet with a high-monounsaturated-fat diet in patients with non-insulin-dependent diabetes mellitus. N Engl J Med. 1988;319(13):829–34. [DOI] [PubMed] [Google Scholar]
- 43.Ludwig DS, Hu FB, Tappy L, Brand-Miller J. Dietary carbohydrates: role of quality and quantity in chronic disease. BMJ. 2018;361:k2340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sarin SK, Negi VS, Dewan R, Sasan S, Saraya A. High familial prevalence of gallstones in the first-degree relatives of gallstone patients. Hepatology. 1995;22(1):138–41. [PubMed] [Google Scholar]
- 45.Wong AC, Ko CW. Carbohydrate intake as a risk factor for biliary sludge and stones during pregnancy. J Clin Gastroenterol. 2013;47(8):700–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Campos-Perez W, Perez-Robles M, Rodriguez-Echevarria R, Rivera-Valdes JJ, Rodriguez-Navarro FM, Rivera-Leon EA, Martinez-Lopez E. High dietary omega-6:omega-3 PUFA ratio and simple carbohydrates as a potential risk factors for gallstone disease: A cross-sectional study. Clin Res Hepatol Gastroenterol. 2022;46(3):101802. [DOI] [PubMed] [Google Scholar]
- 47.Gebhard RL, Prigge WF, Ansel HJ, Schlasner L, Ketover SR, Sande D, Holtmeier K, Peterson FJ. The role of gallbladder emptying in gallstone formation during diet-induced rapid weight loss. Hepatology. 1996;24(3):544–8. [DOI] [PubMed] [Google Scholar]
- 48.Vezina WC, Grace DM, Hutton LC, Alfieri MH, Colby PR, Downey DB, Vanderwerf RJ, White NF, Ward RP. Similarity in gallstone formation from 900 kcal/day diets containing 16 g vs 30 g of daily fat: evidence that fat restriction is not the main culprit of cholelithiasis during rapid weight reduction. Dig Dis Sci. 1998;43(3):554–61. [DOI] [PubMed] [Google Scholar]
- 49.Hansen CD, Gram-Kampmann EM, Hansen JK, Hugger MB, Madsen BS, Jensen JM, Olesen S, Torp N, Rasmussen DN, Kjaergaard M, et al. Effect of Calorie-Unrestricted Low-Carbohydrate, High-Fat Diet Versus High-Carbohydrate, Low-Fat Diet on Type 2 Diabetes and Nonalcoholic Fatty Liver Disease: A Randomized Controlled Trial. Ann Intern Med. 2023;176(1):10–21. [DOI] [PubMed] [Google Scholar]
- 50.Abbasi F, McLaughlin T, Lamendola C, Kim HS, Tanaka A, Wang T, Nakajima K, Reaven GM. High carbohydrate diets, triglyceride-rich lipoproteins, and coronary heart disease risk. Am J Cardiol. 2000;85(1):45–8. [DOI] [PubMed] [Google Scholar]
- 51.Misciagna G, Centonze S, Leoci C, Guerra V, Cisternino AM, Ceo R, Trevisan M. Diet, physical activity, and gallstones–a population-based, case-control study in southern Italy. Am J Clin Nutr. 1999;69(1):120–6. [DOI] [PubMed] [Google Scholar]
- 52.Tsai CJ, Leitzmann MF, Willett WC, Giovannucci EL. Long-chain saturated fatty acids consumption and risk of gallstone disease among men. Ann Surg. 2008;247(1):95–103. [DOI] [PubMed] [Google Scholar]
- 53.Tsai CJ, Leitzmann MF, Willett WC, Giovannucci EL. The effect of long-term intake of cis unsaturated fats on the risk for gallstone disease in men: a prospective cohort study. Ann Intern Med. 2004;141(7):514–22. [DOI] [PubMed] [Google Scholar]
- 54.Park Y, Kim D, Lee JS, Kim YN, Jeong YK, Lee KG, Choi D. Association between diet and gallstones of cholesterol and pigment among patients with cholecystectomy: a case-control study in Korea. J Health Popul Nutr. 2017;36(1):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tsai CJ, Leitzmann MF, Willett WC, Giovannucci EL. Long-term intake of trans-fatty acids and risk of gallstone disease in men. Arch Intern Med. 2005;165(9):1011–5. [DOI] [PubMed] [Google Scholar]
- 56.Jonkers IJ, Smelt AH, Ledeboer M, Hollum ME, Biemond I, Kuipers F, Stellaard F, Boverhof R, Meinders AE, Lamers CH, et al. Gall bladder dysmotility: a risk factor for gall stone formation in hypertriglyceridaemia and reversal on triglyceride lowering therapy by bezafibrate and fish oil. Gut. 2003;52(1):109–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hung T, Sievenpiper JL, Marchie A, Kendall CW, Jenkins DJ. Fat versus carbohydrate in insulin resistance, obesity, diabetes and cardiovascular disease. Curr Opin Clin Nutr Metab Care. 2003;6(2):165–76. [DOI] [PubMed] [Google Scholar]
- 58.Ha K, Song Y. Associations of Meal Timing and Frequency with Obesity and Metabolic Syndrome among Korean Adults. Nutrients 2019, 11(10). [DOI] [PMC free article] [PubMed]
- 59.Martens CR, Rossman MJ, Mazzo MR, Jankowski LR, Nagy EE, Denman BA, Richey JJ, Johnson SA, Ziemba BP, Wang Y, et al. Short-term time-restricted feeding is safe and feasible in non-obese healthy midlife and older adults. Geroscience. 2020;42(2):667–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Trepanowski JF, Kroeger CM, Barnosky A, Klempel MC, Bhutani S, Hoddy KK, Gabel K, Freels S, Rigdon J, Rood J, et al. Effect of Alternate-Day Fasting on Weight Loss, Weight Maintenance, and Cardioprotection Among Metabolically Healthy Obese Adults: A Randomized Clinical Trial. JAMA Intern Med. 2017;177(7):930–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rivera-Zavala JB, Molina-Aguilar C, Perez-Mendoza M, Olguin-Martinez M, Hernandez-Munoz R, Baez-Ruiz GA, Diaz-Munoz M. Daytime restricted feeding modifies the daily regulation of fatty acid beta-oxidation and the lipoprotein profile in rats. Br J Nutr. 2017;117(7):930–41. [DOI] [PubMed] [Google Scholar]
- 62.O’Hara C, Gibney ER. Meal Pattern Analysis in Nutritional Science: Recent Methods and Findings. Adv Nutr. 2021;12(4):1365–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.