Abstract
Background: Recent changes to legislation in British Columbia (BC) have expanded the scope of pharmacist-provided services to include pharmacist prescribing for minor ailments and contraception (PPMAC). The purpose of this study was to gather community-based pharmacists’ perspectives on these changes to practice.
Methods: This was a cross-sectional online survey study. The study population was pharmacists practicing in community settings in BC. A 28-question survey was developed to capture the uptake of prescribing in the pharmacists’ practices, their views on PPMAC, educational supports, and workplace-specific questions. Invitations to participate were disseminated by using fax, social media platform posts, and email.
Results: A total of 246 respondents completed all or part of the survey. A majority felt they should be able to assess and prescribe for minor ailments and contraception, and were satisfied with the regulatory changes. Pharmacists had varying degrees of comfort with prescribing for specific patient populations, with the highest for patients >75 years of age and lowest for patients with renal disease. Respondents felt that patients who were without a primary care provider or did not have easy access to walk-in clinics would benefit the most from PPMAC. Pharmacists expressed concerns about their workplace’s level of support for their providing these new services to patients.
Discussion: Most pharmacist respondents were supportive of and have begun prescribing for minor ailments and contraception in their practices. While they identified many perceived benefits to patient care, workplace barriers may hinder full provision of pharmacist prescribing in their practice.
Keywords: pharmacy practice, prescribing, legislation
Background
Pharmacist prescribing can take many different forms: recommending a non-prescription medication to help manage a patient’s minor condition, refilling or adapting a prescription to ensure safe and effective medication use, or prescribing a medication independently.1 Benefits of pharmacist prescribing of antimicrobials, cardiovascular risk reduction medications, and lipid-lowering medications have been demonstrated.2-5 Pharmacist prescribing has also been shown to improve symptoms of minor ailments (e.g., cold sores, seasonal allergies) and to reduce hemoglobin A1C levels.6 Pharmacist prescribing has also been shown to be as effective as other prescribers’ and is cost-effective.7,8
Legislation permitting pharmacist prescribing varies across Canada.9 Some provinces allow for full independent or collaborative prescribing, while others restrict prescribing to adaptation of existing prescriptions (e.g., prescription renewal, therapeutic substitution, or changes to the drug dose, formulation, or regimen). 9 Additional prescribing activities may include deprescribing, prescribing of vaccines, or prescribing for minor ailments.9
On June 1, 2023, pharmacists in British Columbia (BC) gained the authority to prescribe medications for certain minor ailments and contraception through changes in pharmacy regulations.10, 11 The impetus for the pharmacist prescribing for minor ailments and contraception (PPMAC) program was to improve BC residents’ access to healthcare.11 Although BC was the last province in Canada to enact this scope of practice change, it represented a significant practice shift for BC pharmacists.9
In order for pharmacists to participate in PPMAC, they were required to complete a regulatory education module that reviewed the framework and professional responsibilities of the pharmacist when providing the service.11 No additional training was required although a number of continuing education was offered to pharmacists on the topics for free.11 The process of providing the PPMAC service itself required an in-person assessment of a patient and corresponding documentation of the pharmacist’s assessment and recommendation.11
Two surveys of BC pharmacists’ opinions about prescribing have been published since the COVID-19 pandemic, one involving hospital-based pharmacists in one health authority and the other involving pharmacists working in northern BC in hospital and community practice.12,13 Both showed that pharmacists had positive attitudes about prescribing before the COVID-19 pandemic. However, given the additional roles pharmacists have taken on since the pandemic, there is a need to update our understanding of pharmacists’ perspectives and elicit the views of a broader spectrum of pharmacists. The purpose of this study was to gather the perspectives of BC pharmacists on PPMAC in community-based practices. Perceptions of related regulatory changes, educational needs and preparedness, and barriers and facilitators in the workplace were also explored.
Methods
This was a cross-sectional survey of pharmacists who practice in community-based settings in BC. Community pharmacy refers to the brick-and-mortar pharmacy that is licensed to dispense medications to the public. At the time of the study, there were 1479 community pharmacies in BC and approximately 4000 pharmacists practicing in this setting.
Survey Development and Dissemination
A literature search was conducted to capture previous studies that have investigated pharmacist perceptions of prescribing. Primarily, two studies were used to develop an initial set of survey questions that were refined by the study team.12, 13 Feedback on the survey content and clarity was obtained from 7 stakeholders representing the target population. The final survey consisted of 42 questions with questions divided into 5 categories. The exact distribution of the survey questions was as follows: demographic information (11 questions), uptake of PPMAC in their own practice (6 questions), views on PPMAC (11 questions), educational supports (6 questions), and workplace-based questions (8 questions).
The survey was administered using the University of British Columbia’s version of the web-based Qualtrics platform and was available between July 24 and September 8, 2023. All questions were optional, resulting in different response rates for each question.
The study population was pharmacists practicing in community settings in BC. A screening question at the start of the survey confirmed respondents met this criterion. All 1476 community pharmacies listed on the BC College of Pharmacists website were sent an invitation by fax for their pharmacist staff to participate. These faxes were sent electronically. Pharmacists who work as practice educators (i.e., practicing pharmacists who teach pharmacy students) at the Faculty of Pharmaceutical Sciences at the University of British Columbia (UBC) were also sent an email invitation to participate. It is noteworthy that these practice educators were all practicing pharmacists. For those who worked in a community pharmacy, they might receive the invitations both through fax or email. Invitations to participate were also posted on online social media platforms [Facebook, LinkedIn, and X (Twitter)] on the investigators’ personal accounts and on the UBC Faculty of Pharmaceutical Sciences’ social media accounts. Respondents were asked for their informed consent before proceeding to the survey questions.
No personally identifying information was collected in the survey. However, respondents could enter a draw for two $25 Amazon gift cards by giving their email address, which was collected separately and not linked to their survey responses. Approval to conduct this research study was obtained from UBC’s Behavioural Research Ethics Board (certificate H23-02130).
Statistical Analysis
Descriptive statistics were used for quantitative items and content analysis was used for open-ended responses to classify and summarize the data.
Results
A total of 246 responses were received. Characteristics of the respondents that answered the demographic questions are shown in Table 1. Note the total number of respondents that answered the question is reported as “N” and the number of responses specific to a parameter being reported for a question is reported as “n.”
Table 1.
Demographic Information
| N (%) | |
|---|---|
| Age | Total N=190 |
| 20-29 years | 44 (23) |
| 30-39 years | 67 (35) |
| 40-49 years | 43 (23) |
| 50-59 years | 23 (12) |
| 60-69 years | 7 (4) |
| ≥70 years | 1 (1) |
| Prefer not to answer | 5 (3) |
| Gender | Total N=189 |
| Man | 84 (44) |
| Woman | 96 (51) |
| Non-binary | 2 (1) |
| Prefer not to answer | 7 (4) |
| Primary Role | Total N=190 |
| Staff pharmacist | 95 (50) |
| Pharmacy manager | 65 (34) |
| Pharmacy owner | 23 (12) |
| Other | 5 (3) |
| Prefer not to answer | 2 (1) |
| Years Practiced as a Community Pharmacist | Total N=190 |
| 0-5 | 58 (31) |
| 6-10 | 45 (24) |
| 11-15 | 36 (19) |
| 16-20 | 16 (8) |
| >20 | 32 (17) |
| Prefer not to answer | 3 (2) |
| Additional training after becoming a licensed pharmacist | Total N=195 |
| Yes | 108 (55) |
| No | 87 (45) |
| Additional training | Total N=201 |
| Injection training | 84 (42) |
| iOAT certification | 34 (17) |
| Certified Diabetes Educator | 26 (13) |
| Compounding certification | 24 (12) |
| Other | 10 (5) |
| Board Certification | 6 (3) |
| Certified Travel Educator | 6 (3) |
| Hospital Pharmacy Residency | 5 (2) |
| Community/Ambulatory Pharmacy Residency | 3 (2) |
| Certified Asthma/COPD Educator | 3 (2) |
| Industry Residency | 0 (0) |
| Worked in another province or in the US? | Total N=188 |
| Yes | 37 (20) |
| No | 151 (80) |
| Geographic area of practice | Total N=187 |
| Vancouver Coastal Health | 53 (28) |
| Fraser Health | 51 (27) |
| Interior Health | 40 (21) |
| Island Health | 30 (16) |
| Northern Health | 13 (7) |
| First Nations Health Authority | 0 (0) |
| Primary community pharmacy workplace setting* | Total N=188 |
| Corporate (e.g., London Drugs, Rexall, Shoppers Drug Mart, Walmart, Safeway, Costco, Loblaws) | 74 (39) |
| Independent | 65 (35) |
| Banner (e.g., Pharmasave, Medicine Shoppe) | 47 (25) |
| Others (please specify) [free form answer] | 2 (1) |
COPD, chronic obstructive pulmonary disease; iOAT, injectable opioid agonist treatment.
• Corporate = chain pharmacies operating within large corporate structures; Independent = independently owned and operated; Banner = independently owned but operated under the support of a banner brand
Half of the respondents (n=95, 50%) were employed as a staff pharmacist and most (n=103, 55%) had practiced for less than 10 years. More than half of the respondents had completed additional formal training after pharmacist licensure (n=108, 55%). There was representation from across all five of the province’s regional health authorities from the 187 respondents that provided their geographical location. There were no respondents specifically selecting First Nations Health Authority.
Table 2 shows the distribution of minor ailments for which respondents prescribed, and the rate of prescribing contraceptives. The most common minor ailments prescribed for were uncomplicated urinary tract infection, allergic rhinitis, conjunctivitis, and dermatitis. Sixty-five percent of the 218 respondents had prescribed contraception.
Table 2.
Uptake of Prescribing
| N (%) | |
|---|---|
| Provided minor ailments prescribing services since June 1, 2023 | Total N=224 |
| Yes | 206 (92) |
| No | 18 (8) |
| Total N=182 | |
| Number of times prescribing for minor ailments provided, mean ± SD | 20 ± 15 |
| Minor ailments services provided | Total N of Respondents=198 Total N of responses=1575 |
| Urinary tract infection (uncomplicated) | 169 (85) |
| Allergic rhinitis | 142 (72) |
| Conjunctivitis (allergic, bacterial, or viral) | 137 (69) |
| Dermatitis (allergic, atopic, contact, diaper, or seborrheic) | 121 (61) |
| Fungal infections (onychomycosis, Tinea corporis infection, Tinea cruris infection or Tinea pedis infection) | 96 (48) |
| Herpes labialis | 94 (47) |
| Gastroesophageal reflux disease | 93 (47) |
| Acne | 91 (46) |
| Musculoskeletal pain | 66 (33) |
| Nicotine dependence | 64 (32) |
| Dyspepsia | 62 (31) |
| Oral ulcers (canker sores or aphthous ulcers) | 62 (31) |
| Hemorrhoids | 56 (28) |
| Urticaria, including insect bites | 55 (28) |
| Shingles | 50 (25) |
| Vaginal candidiasis | 48 (24) |
| Oropharyngeal candidiasis | 44 (22) |
| Headache | 43 (22) |
| Impetigo | 35 (17) |
| Dysmenorrhea | 26 (13) |
| Threadworms or pinworms | 21 (11) |
| Provided contraception prescribing services since June 1, 2023 | Total N=218 |
| Yes | 141 (65) |
| No | 77 (35) |
| Total N=135 | |
| Number of times contraceptive prescribing services provided, mean ± SD | 8 ± 10 |
SD, standard deviation.
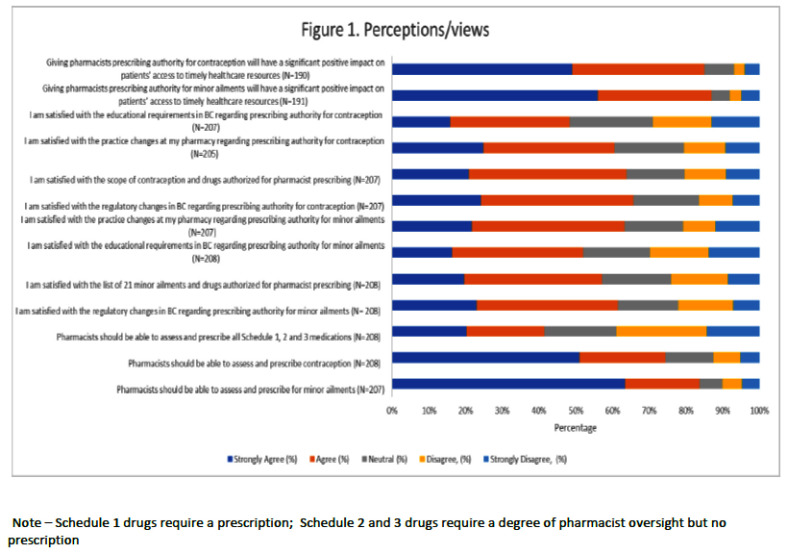
Respondents’ opinions about the PPMAC program are shown in Figure 1. Respondents rated agree or strongly agree with most items. The statement with the highest rating of disagree or strongly disagree was “Pharmacists should be able to assess and prescribe all Schedule 1, 2 and 3 medications.” (n=207, 39%). Most respondents rated agree or strongly agree that pharmacists should be able to assess and prescribe for minor ailments (N=206, 84%) and contraception (N=207, 74%), and were satisfied with the regulatory changes and educational requirements (N=207, 62%).
Figure 1.
Community Pharmacists Perceptions and Views of the Prescribing Changes
Note – Schedule 1 drugs require a prescription; Schedule 2 and 3 drugs require a degree of pharmacist oversight but no prescription
Nearly all respondents had completed the mandatory regulatory education for PPMAC (n=193, 98%) and had accessed the optional education resources (n=154, 77%). Among the optional education resources used, 89% of respondents used the medSask resources, while 56% had reviewed the Prescribing for Minor Ailments modules offered by UBC’s Continuing Pharmacy Professional Development program. These were online self-learning programs. Most respondents noted that these resources refreshed their therapeutic knowledge (n=172, 89%), increased their awareness of the regulatory changes (n=149, 77%), and allowed them to feel more prepared to offer the prescribing services (n=144,75%). Respondents did identify they required additional educational supports (n=90, 48%) and felt they would like additional certification programs to help prepare them (n=81, 43%).
Information regarding pharmacists’ comfort with prescribing to different patient populations was also collected. Comfort was highest with older patients, which was defined as >75 years of age, (N=199, 71%), followed by patients with comorbidities (N=119, 60%), pregnant/lactating patients (N=107, 54%), and children (N=48, 48%). Patient populations with the lowest level of comfort ranked was those with renal disease (N=200, 37%). When asked to identify what patient groups would most benefit from pharmacist minor ailment or contraception prescribing, respondents identified patients without primary care providers (n=175 for minor ailment prescribing, n=171 for contraception prescribing), those without walk-in clinics in their area (n=158, n=148), and those who wanted to avoid long wait times (n=140, n=129).
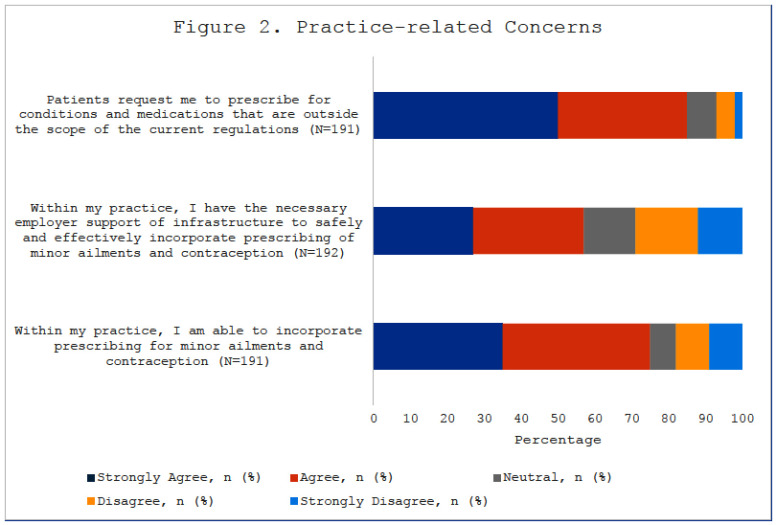
Respondents’ workplace-related opinions about the PPMAC program are summarized in Figure 2. A majority rated agree or strongly agree for the statement, “Patients request me to prescribe for conditions and medications that are outside the scope of the current regulations” (N=190, 85%). However, only half of the respondents agreed or strongly agreed that their employers had provided support for them to incorporate PPMAC safely and effectively into their practices (N=192, 57%). A majority agreed or strongly agreed that having prescribing authority would significantly and positively impact patients’ access to timely healthcare (N=191, 85%). Most respondents also agreed that they would be able to incorporate minor ailments and contraception prescribing services into their practice (N=191, 75%).
Figure 2.
Pharmacists Identified Practice Related Concerns
Table 3 details workplace changes and barriers. Regarding hiring practice changes that have been made to their workplace in preparation for PPMAC, most responded that there were no changes with the service being incorporated into workflow (n=109). When asked about what barriers might impact their ability to prescribe for minor ailments and contraception, increased workload (n=152), time constraints with walk-in requests (n=124), and insufficient renumeration to the pharmacists (n=122) were the top three barriers identified. In response to what things had been implemented in their workplace setting to prepare for PPMAC, the top three changes included accepting both walk-in patients and those by appointment (n=138), using the provincial appointment booking system (n=92), and updating pharmacy software (n=57).
Table 3.
Workplace Changes since Prescribing Implementation
| Number of Responses | |
|---|---|
| Hiring practice changes that have been made to the respondents primary workplace setting in preparation for minor ailments and contraception | Total N of respondents=187 Total N of responses=277 |
| No changes (incorporated into workflow) | 109 |
| No changes (have pharmacist overlap) | 61 |
| No changes (low prescription volume) | 51 |
| No changes (not intending to provide MACS) | 19 |
| Added pharmacist overlap | 13 |
| Other | 12 |
| Hired more pharmacy assistants | 9 |
| Hired pharmacy students | 2 |
| Hired more pharmacy technicians | 1 |
| Implementations in respondents primary workplace setting in preparation for minor ailments and contraception | Total N of respondents=171 Total N of responses=394 |
| Accept both walk ins and appointments | 138 |
| Used provincial appointment booking system | 92 |
| Updated pharmacy software program | 57 |
| Created in-store calendar or booking system for appointments | 44 |
| Provided educational materials, such as handouts, slide decks | 39 |
| Other | 15 |
| Additional structural modifications to the current pharmacy layout | 9 |
| Barriers that impact respondents ability to prescribe for minor ailments and contraception | Total N of respondents=188 Total N of responses=954 |
| Increased workload (do more with less staffing) | 152 |
| Time constraints with walk-in requests | 124 |
| Insufficient renumeration to the pharmacist | 122 |
| Time constraints to follow up with patient. | 111 |
| Documentation requirements | 87 |
| Increased risk of liability | 80 |
| Insufficient renumeration to the pharmacist | 70 |
| Lack of support from physicians and other prescribers | 43 |
| Lack of knowledge base in contraception | 41 |
| Lack of access to patient information (e.g., CareConnect) | 36 |
| Lack of references and resources within workplace | 28 |
| Lack of interest from patients | 26 |
| Lack of knowledge base in minor ailments | 22 |
| Other (please specify) | 12 |
MACS, minor ailments and contraception service.
Respondents had an opportunity to provide additional commentary or thoughts around pharmacist prescribing at the end of the survey. The open-ended responses were categorized into several groupings: advocating for more reimbursement or direct billing for individual pharmacists, additional training programs to feel more competent, and further expansion of scope of practice. Respondents also expressed concerns about the scope of practice and believed that it should be more limited, about the increased workload and lack of staffing support, about public misperceptions of the extent of the prescribing authority, and about concerns related to liability and conflicts of interest. Logistical concerns, such as the available booking systems, were also voiced.
Discussion
This survey-based study of community-based pharmacists in BC revealed overall positive views of PPMAC and vigorous uptake of PPMAC into respondents’ practice. Prescribing was particularly frequent for uncomplicated urinary tract infections, allergic rhinitis, and conjunctivitis. While a majority of respondents had also prescribed contraception during the approximately 2 months since the program began, this was slightly lower than those who had prescribed for minor ailments. These findings for minor ailments are consistent with uptake data shared by the BC Ministry of Health.14 Attitudes about the regulatory framework and educational resources available were generally positive. Despite this, respondents were not in agreement about expansion of prescribing to all medications and expressed concerns about increased workload and lack of staffing support.
The incremental expansion of pharmacist prescribing authority in BC is unlike Alberta’s all-at-once approach authorizing independent pharmacist prescribing of medications since 2007.15 The BC context also differs in that the PPMAC scope was implemented following the COVID-19 pandemic when additional workload had been placed on pharmacists including unprecedented volumes of vaccine administration in community pharmacies and removal of restrictions on adapting and renewing prescriptions. The BC program of expansion is similar to the program implemented recently in Ontario, where pharmacists were given authority to prescribe for 19 minor ailments.16 In addition, the Ontario pharmacists were required to only complete a “Mandatory Orientation for Minor Ailments Prescribing” module which outlines the pharmacists ethical, legal, and professional obligations.16 Any additional continuing education undertaken was up to the discretion of the individual pharmacist.16
Research to date involving pharmacists has identified a variety of views on prescribing authority. Qualitative research using semi-structured interviews of pharmacy managers and owners found that they acknowledged the benefits to stakeholders, but had concerns about barriers such as the time and human resources required, and the lack of collaboration with other prescribers in community practice coupled with insufficient remuneration.17 Increased workload with uptake of new programs can be a challenge. Our study found that 58% of respondents had no additional supports added in their workplace and had just incorporated PPMAC into their normal workflow. The Canadian Pharmacy Mental Health and Workforce Wellness Survey conducted in 2023 showed improvements in pharmacists mental health, but still 79% of those that participated were at risk for burnout.18 Providing patient care contributes the most to a feeling of fulfillment for pharmacists, but conversely, workload has the most significant impact on mental health.18
Related to our results, while pharmacists held overall positive views about the changes with good uptake, there is a risk of negative effects if workplaces do not adjust to support pharmacist prescribing. However, as our survey started just after the implementation of the legislation, this may not have allowed sufficient time for changes to staffing levels. Especially in the context of challenging health human resources shortages of pharmacists and pharmacy technicians across the urban and rural areas of the province.
Research in England found that the provision of community pharmacy minor ailment prescribing was unsustainable, with multiple barriers identified including poor integration of community pharmacy service provision within the larger healthcare system and challenges with the perceptions of the public and other healthcare professionals with community pharmacists.19 Pharmacists in our study reported being asked by patients to prescribe for conditions outside their current scope, which may indicate a more positive perception by patients on the change in practice that has occurred. The positive outlook of pharmacist prescribing has been identified in previous literature with patients reporting benefits such as accessibility and quality of services received.24 However, other studies have found a lack of coherence in the pharmacy workforce. One study noted that community pharmacists did not share information and learning of best practices with each other or have a consistent vision of their role in patient care and the healthcare system at large.19 While pharmacists in our study were generally positive about the practice changes, some were not as supportive with further expansion of prescribing.
Pharmacists may not be willing to incorporate prescribing into their practice for a variety of reasons, including concerns about the reaction of other prescribers, lack of access to patient records, limited diagnostic skills, and lack of organizational support.20, 21 Other studies have found that pharmacists preferred that their authority be limited, as they were worried about the potential for liability and preferred to prescribe medications for which adverse events were less common or severe, and for conditions that were relatively easy to diagnose.21 While pharmacists have been found to be competent in prescribing, some may not feel confident due to lack of self-awareness and education.12
Our study found differing degrees of comfort prescribing for specific patient populations, such as those with renal disease. While the pharmacists in this study made good use of the available resources, additional learning opportunities may be needed to increase confidence in prescribing for more challenging or complex patient populations. A survey that explored pharmacists learning needs related to expanded scopes of practice found pharmacists wanting additional training in physical assessment, interpreting laboratory tests, and making decisions about complex drug therapy.22 In addition, a scoping review that examined confidence and competence related to prescribing found limited research in the area of pharmacist prescribing.25 One of the major themes identified was around the lack of education and educational improvements and highlighted the need for increased pharmacist training in such areas as diagnostics and physical assessment. 25
If further expansion of pharmacist practice occurs, additional education as early as during university education may be required to support uptake by pharmacists.
Based on our study results, there are a number of different ways that policy makers can support expansion of pharmacist services. With policy changes that have the potential to increase the workload of pharmacists, there is a need for the work environment to provide supports to allow pharmacists to adopt these new practices. Policy makers could identify whether regulations are needed to mandate minimum workplace requirements to provide additional services. In addition, direct remuneration to compensate pharmacists for their services could be explored to provide additional incentives. Other strategies focusing on ensuring that community pharmacists are able to access patient records may also be needed to be implemented along with new policies. Future research could explore the optimal education supports required to support pharmacist practice expansion. In addition, patient views of pharmacist prescribing, is also an important area of research. And there is a need for longitudinal studies to track changes in pharmacist prescribing behavior over time.
Limitations
The study had several limitations. There are approximately 4000 community pharmacists in BC, so the sample size of this study reflects a low participation rate.23 Engaging community-based pharmacists to participate in research is challenging, as there are no central means of recruitment. We attempted to overcome this barrier by using multiple methods of recruitment, but still had a low response rate and may have contributed to bias in terms of those who chose to respond and subsequently our overall results. Because we contacted pharmacists in their workplace via fax invitations, their inclination to participate may have been influenced by their perceptions of their employer’s attitudes towards PPMAC. In addition, we do not have any way of confirming if our faxed invitation reached the intended audience. Respondents may have been more engaged with PPMAC than non-respondents, and/or have had stronger views about it. And, while we had representation from the majority of geographic areas of practice, the majority of participants came from the greater populated areas within the province. Hence, our results may not be generalizable to all pharmacists in BC or other jurisdictions.
Conclusions
Overall, community-based pharmacists in BC were supportive of the recent changes in legislation that allowed for PPMAC. This study demonstrated a relatively high practice-based uptake of prescribing among respondents, particularly for minor ailments. While pharmacists identified many patient care benefits to the PPMAC program, barriers related to their workplace may hinder full provision of PPMAC in their practice.
Acknowledgments
Disclaimer: The statements, opinions, and data contained in all publications are those of the authors.
References
- 1.Pharmacist Prescribing Task Force. Prescribing by pharmacists: information paper. Can J Hosp Pharm 2010;63(3):267-74. doi: 10.4212/cjhp.v63i3.926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu JHC, Khalid F, Langford BJ, Beahm NP, McIntyre M, Schwarts KL, Garber G, Leung V. Community pharmacist prescribing of antimicrobials: A systematic review from an antimicrobial stewardship perspective. Can Pharm J 2021; 154: 179-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beahm NP, Smyth DJ, Tsuyuki RT. Management by Pharmacists (RxOUTMAP): A study of pharmacist prescribing and care in patients with uncomplicated urinary tract infections in the community. Can Pharm J 2018; 151: 305-314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsuyuki RT, Al Hamarneh YN, Jones CA, Hemmelgarn BR. The Effectiveness of Pharmacist Interventions on Cardiovascular Risk: The Multicenter Randomized Controlled RxEACH Trial. J Am Coll Cardiol 2016;67(24):2846-54. doi: 10.1016/j.jacc.2016.03.528. Epub 2016 Apr 4. [DOI] [PubMed] [Google Scholar]
- 5.Tsuyuki RT, Rosenthal M, Pearson GJ. A randomized trial of a community-based approach to dyslipidemia management: Pharmacist prescribing to achieve cholesterol targets (RxACT study). Can Pharm J 2016; 149: 283-292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Faruquee CF, Guirguis LM. A scoping review of research on the prescribing practice of Canadian pharmacists. Can Pharm J 2015;148(6):325-48. doi: 10.1177/1715163515608399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al Hamarneh YN, Johnston K, Marra CA, Tsuyuki RT. Pharmacist prescribing and care improves cardiovascular risk, but is it cost-effective? A cost-effectiveness analysis of the RxEACH study. Can Pharm J 2019; 152: 257-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weeks G, George J, Maclure K, Stewart D. Non-medical prescribing versus medical prescribing for acute and chronic disease management in primary and secondary care. Cochrane Database of Systematic Reviews 2016, Issue 11. Art. No.: CD011227. DOI: 10.1002/14651858.CD011227.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Canadian Pharmacists Association. Pharmacists Scope of Practice in Canada, https://www.pharmacists.ca/advocacy/scope-of-practice/ (2023, accessed 8 Dec 2023)
- 10.Government of British Columbia. Minor Ailments and Contraception Service (MACS). https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/pharmacare/initiatives/ppmac#:~:text=As%20announced%20in%20September%202022,launch%20on%20June%201%2C%202023 (accessed 6 April 2023)
- 11.College of Pharmacists of British Columbia. https://www.bcpharmacists.org/ppmacPharmacists Prescribing for Minor Ailments and Contraception. (2024, accessed 30 August 2024)
- 12.Lewis, J, Barry AR, Bellefeuille K, Pammett RT. Perceptions of Independent Pharmacist Prescribing among Health Authority- and Community-Based Pharmacists in Northern British Columbia. Pharmacy (Basel, Switzerland) 2021; 9(2), 92. 10.3390/pharmacy9020092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prasad M, Loewen PS, Shalansky S, Salmasi S, Barry AR. Health Authority Pharmacists’ Perceptions of Independent Pharmacist Prescribing. Can J Hosp Pharm. 2019. 72(3), 185–193. [PMC free article] [PubMed] [Google Scholar]
- 14.Government of British Columbia. Pharmacists prescribing for minor ailments and contraception – data. https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/pharmacare/initiatives/sop/monitoring-evaluation-ppmac (2024, accessed 22 May 2024) [Google Scholar]
- 15.Bacovsky RA. Pharmacist prescribing: has the momentum started? Can J Hosp Pharm. 2012;65(6):421-6. doi: 10.4212/cjhp.v65i6.1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ontario College of Pharmacists. Minor Ailments. https://www.ocpinfo.com/practice-education/expanded-scope-of-practice/minor-ailment/ (2024, accessed 27 May 2024)
- 17.Donald M, King-Shier K, Tsuyuki RT, Al Hamarneh YN, Jones CA, Manns B, Tonelli M, Tink W, Scott-Douglas N, Hemmelgarn BR. Patient, family physician and community pharmacist perspectives on expanded pharmacy scope of practice: a qualitative study. CMAJ Open. 2017. Mar 6;5(1):E205-E212. doi: 10.9778/cmajo.20160135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Canadian Pharmacists Association. National survey shows mental health of pharmacy professionals has improved but more support and investments needed to address continued challenges. https://www.pharmacists.ca/news-events/news/national-survey-shows-mental-health-of-pharmacy-professionals-has-improved-but-more-support-and-investments-needed-to-address-continued-challenges/ (accessed 23 May 2024)
- 19.Nazar H, Nazar Z. Community pharmacy minor ailment services: Pharmacy stakeholder perspectives on the factors affecting sustainability. Research in Social and Administrative Pharmacy 2019; 15: 292-302. [DOI] [PubMed] [Google Scholar]
- 20.Ramos DC, Ferreira L, Santos Júnior GAD, Ayres LR, Esposti CDD. Pharmacist prescribing: a review of perceptions and attitudes of patients, pharmacists and other interested professionals. Cien Saude Colet. 2022;27(9):3531-3546. Portuguese, English. doi: 10.1590/1413-81232022279.19972021. Epub 2022 May 28. [DOI] [PubMed] [Google Scholar]
- 21.Feehan M, Durante R, Ruble J, Munger MA. Qualitative interviews regarding pharmacist prescribing in the community setting. Am J Health Syst Pharm. 2016; 73(18):1456-61. doi: 10.2146/ajhp150691. [DOI] [PubMed] [Google Scholar]
- 22.Schindel TJ, Yuksel N, Pharmacist learning needs in the era of expanding scopes of practice: Evolving practices and changing needs. Research in Social and Administrative Pharmacy 2019; 15: 448-458 [DOI] [PubMed] [Google Scholar]
- 23.National Association of Pharmacy Regulatory Authorities. National Statistics 2023. https://www.napra.ca/wp-content/uploads/2023/03/NAPRA-National-Statistics-2023-EN-Final.pdf (accessed 22 May 2024)
- 24.Famiyeh IM, McCarthy L. Pharmacist prescribing: A scoping review about the views and experiences of patients and the public. Res Social Adm Pharm. 2017. Jan-Feb;13(1):1-16. doi: 10.1016/j.sapharm.2016.01.002. Epub 2016 Jan 18. [DOI] [PubMed] [Google Scholar]
- 25.Woit C, Yuksel N, Charrois TL. Competence and confidence with prescribing in pharmacy and medicine: a scoping review. Int J Pharm Pract. 2020. Aug;28(4):312-325. doi: 10.1111/ijpp.12595. Epub 2019 Dec 25. [DOI] [PubMed] [Google Scholar]