Abstract
Cancer care organizations often struggle to adequately address the unique needs of adolescent and young adult cancer patients, resulting in poorer outcomes compared with other age groups. Creation of adolescent and young adult cancer programs serves to bridge this gap and improve quality of care for this population. We aimed to describe the evolution and impact of the University of North Carolina at Chapel Hill’s Adolescent and Young Adult Cancer Program. To do so, we conducted a retrospective cohort study utilizing electronic health record data matched with North Carolina Cancer Registry data from 2014 to 2022. Between 2014 and 2022, a total of 4016 adolescents and young adults (aged 13-39 years) received cancer care at the University of North Carolina Medical Center, with 670 having contact with the Adolescent and Young Adult Cancer Program. Program-contacted patients were younger, more likely to be non-Hispanic Black race, and more likely to have metastatic disease or hematologic malignancies. We saw a steady increase in patient volume over the study period, corresponding with program growth.
Adolescents and young adults (aged 15-39 years) represent a growing portion of the cancer population, with more than 90 000 diagnosed annually in the United States (1). They face biological, developmental, and psychosocial needs distinct from pediatric or older adult populations (2). Historically, adolescents and young adults have been placed into pediatric or medical oncology settings ill-equipped to provide care tailored for their unique needs. This hampers delivery of high-quality, developmentally appropriate care for adolescents and young adults and contributes to poorer outcomes compared with non–adolescent and young adult cancer patients (3-5).
In response to this increasing need, the University of North Carolina (UNC) at Chapel Hill founded an Adolescent and Young Adult Cancer Program in 2015, serving patients aged 13-39 years. Over the past decade, this program has grown from 1 social worker to a team of 11 individuals focused on providing medical and psychosocial support to adolescents and young adults. Similar programs have emerged nationwide as recognition, and buy-in for adolescent and young adult needs across professional organizations has grown (6-9).
Despite the expansion of adolescent and young adult programs, there are limited data documenting the reach and impact of adolescent and young adult–specific models of care (10). To address this gap, we sought to describe the evolution of the UNC Adolescent and Young Adult Cancer Program over time and define the clinical and sociodemographic features of the patient population served by our program housed within a National Cancer Institute Comprehensive Cancer Center and public academic health system. This analysis will enhance our understanding of the reach of our program, informing expansion efforts and guiding other centers seeking to implement or grow similar programs. A second planned publication will examine how program contact influences outcomes. Across these 2 articles, this study aims to assess care delivered to adolescents and young adults and to highlight gaps to focus future interventions that increase delivery of guideline-concordant care.
We performed a retrospective cohort study using electronic health record data matched with North Carolina Cancer Registry data since 2014. We included individuals aged 13-39 years receiving some type of cancer treatment (ie, chemotherapy, immunotherapy, oral oncolytics, hormonal therapies and CAR-T, surgery, or radiation) at the UNC Medical Center (adult and pediatric settings). We extracted sociodemographic data, including race, ethnicity, sex, age, marital status, insurance status, and using census tract data, we extracted regional income and educational achievement. Race, ethnicity, and sex were defined by electronic health record documentation in structured fields, which represents largely self-report but likely some provider entry as well. Age was defined by birthdate, insurance was verified by the financial department, and marital status was self-reported. For clinical characteristics, we extracted types of cancer, stage, and treatment, including systemic therapy as above, surgery, or radiation. We compared sociodemographic and clinical criteria between those who did and did not receive Adolescent and Young Adult Cancer Program contact, as defined by a chart-documented encounter with a dedicated program social worker or nurse practitioner. The χ2 tests and t tests were used to assess these comparisons, with a P value less than .05 defined as statistically significant. Unadjusted log binomial regression modeling was used to produce unadjusted relative risks for associations between patients with Adolescent and Young Adult Program contact and their sociodemographic and clinical characteristics. All statistical testing was 2-sided.
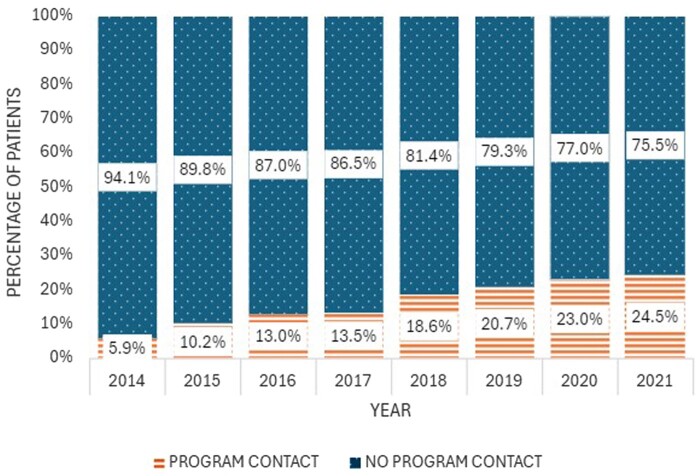
Between 2014 and 2022, a total of 4016 adolescents and young adults received cancer care at UNC, and 670 (17%) had contact with our Adolescent and Young Adult Cancer Program (Table 1). The program increased in volume and proportion of adolescents and young adults seen year over year (Figure 1). In 2014, 287 adolescents and young adults were seen, and 17 (6%) had documented program contact. In 2018, 484 adolescents and young adults were seen, and 90 (19%) had documented program contact. In 2021, the last year of complete data, 449 adolescents and young adults were seen, and 110 (25%) had documented program contact.
Table 1.
Characteristics of adolescents and young adults with and without program contact
| Characteristics | Program contact, No. (%) (n = 670) | No program contact, No. (%) (n = 3346) | P | Unadjusted RR (95% CI) | P |
|---|---|---|---|---|---|
| Age at diagnosis, y | |||||
| Mean yearsa | 27 | 31 | <.01 | — | |
| 13-19 | 120 (18) | 339 (10) | <.01 | 0.99 (0.82 to 1.19) | .91 |
| 20-29 | 293 (44) | 816 (24) | Referent | Referent | |
| 30-39 | 257 (38) | 2191 (66) | 0.40 (0.34 to 0.46) | <.01 | |
| Sex | |||||
| Female | 368 (55) | 2030 (61) | .02 | Referent | Referent |
| Male | 302 (45) | 1315 (39) | 1.22 (1.06 to 1.40) | .01 | |
| Raceb | |||||
| Hispanic | 85 (13) | 377 (11) | <.01 | 1.19 (0.96 to 1.48 | .10 |
| Non-Hispanic Black | 170 (25) | 653 (20) | 1.34 (1.14 to 1.58) | <.01 | |
| Non-Hispanic White | 362 (54) | 1988 (59) | Referent | Referent | |
| Other | 41 (6) | 177 (5) | 1.22 (0.91 to 1.63) | .18 | |
| Unknown | 12 (2) | 151 (5) | — | — | |
| Marital statusb | |||||
| Married or partnered | 214 (32) | 1376 (41) | <.01 | Referent | Referent |
| Not married | 415 (62) | 1554 (46) | 1.57 (1.35 to 1.82) | <.01 | |
| Insurance | |||||
| Private | 360 (54) | 1802 (54) | .02 | 0.84 (0.71 to 1.00) | .05 |
| Public | 147 (22) | 597 (18) | Referent | Referent | |
| Other | 42 (6) | 199 (6) | 0.88 (0.65 to 1.20) | .43 | |
| No insurance | 121 (18) | 748 (22) | 0.70 (0.57 to 0.88) | <.01 | |
| Median income | $59 595 | $62 764 | .01 | ||
| Cancer site | |||||
| Breast | 65 (10) | 373 (11) | <.01 | Referent | Referent |
| Leukemia | 174 (26) | 191 (6) | 3.21 (2.50 to 4.12) | <.01 | |
| Lymphoma | 137 (20) | 250 (8) | 2.39 (1.84 to 3.10) | <.01 | |
| Skin | 16 (2) | 468 (14) | 0.22 (0.13 to 0.38) | <.01 | |
| Thoracic | 13 (2) | 34 (1) | 1.86 (1.11 to 3.12) | .02 | |
| Gastrointestinal | 26 (4) | 202 (6) | 0.77 (0.50 to 1.18) | .23 | |
| Urologic | 32 (5) | 285 (9) | 0.68 (0.46 to 1.01) | .06 | |
| Gynecologic | 43 (6) | 395 (12) | 0.66 (0.46 to 0.95) | .03 | |
| Head and neck | 27 (4) | 384 (12) | 0.44 (0.29 to 0.68) | <.01 | |
| Neurologic | 32 (5) | 349 (10) | 0.57 (0.38 to 0.84) | .01 | |
| Other | 105 (16) | 415 (12) | 1.36 (1.03 to 1.80) | .03 | |
| Radiation | |||||
| None | 495 (74) | 2522 (75) | .41 | Referent | Referent |
| Received | 175 (26) | 824 (25) | 1.07 (0.91 to 1.25) | .41 | |
| Chemotherapy | |||||
| None | 101 (15) | 2084 (62) | <.01 | Referent | Referent |
| Received | 568 (85) | 1249 (37) | 6.76 (5.52 to 8.28) | <.01 | |
| Immunotherapy | |||||
| None | 556 (83) | 3036 (91) | <.01 | Referent | Referent |
| Received | 114 (17) | 037 (9) | 1.75 (1.47 to 2.08) | <.01 | |
| Hormone therapy | |||||
| None | 472 (70) | 2675 (80) | <.01 | Referent | Referent |
| Received | 198 (30) | 657 (19) | 1.54 (1.33 to 1.79) | <.01 | |
| Cancer type | |||||
| Solid | 359 (54) | 2905 (87) | <.01 | Referent | Referent |
| Hematologic | 311 (46) | 441 (13) | <.01 | 3.76 (3.30 to 4.28) | <.01 |
| Stageb | |||||
| Not metastatic | 306 (46) | 2665 (80) | <.01 | Referent | Referent |
| Metastatic | 349 (52) | 592 (18) | 3.60 (3.15 to 4.12) | <.01 | |
| Unknown | 15 (2) | 89 (3) | — | — | |
Relative risk not evaluated as it is not appropriate for a continuous variable. CI = confidence interval; RR = relative risk.
Percentages do not total 100% because of unknown or missing data.
Figure 1.
Growth of University of North Carolina Adolescent and Young Adult Cancer Program over time. Bar chart showing the growth in Adolescent and Young Adult Cancer Program patient contact between 2014 and 2021. The dotted bars represent the percentage of adolescent and young adult patients who did not have program contact, and the striped bars represent the percentage of adolescent and young adult patients who did have program contact.
Among program-contacted patients, the average age at diagnosis was 27 years vs 31 years among uncontacted patients. Racial distribution was representative of the state population, but program-contacted patients were more likely to be identified as non-Hispanic Black compared with non-Hispanic White (relative risk [RR] = 1.34, 95% confidence interval [CI] = 1.14 to 1.58). More program-contacted patients were unmarried (RR = 1.57, 95% CI = 1.35 to 1.82). Program-contacted patients were from regions with lower median income ($59 595 vs $62 764, P = .014) and similar educational achievement (highest education less than high school: 25% vs 24%, P = .27).
Program-contacted adolescents and young adults differed in terms of cancer diagnosis and stage (P = <.01). They were more likely to have leukemia (26% vs 6%) or lymphoma (20% vs 8%) and less likely to have skin cancer (2% vs 14%) or head and neck cancer (4% vs 12%). More than one-half (55%) of program-contacted patients had metastatic disease compared with 18% of uncontacted patients.
Treatment differed between the groups. Radiation was uncommon across groups (26% vs 25%), whereas all forms of systemic therapy were more likely among program-contacted patients (chemotherapy 85% vs 37%; immunotherapy 18% vs 9%; hormone therapy 30% vs 20%).
As the program grew, the racial makeup of program-contact patients remained quite diverse, with increasing proportions of non-Hispanic Black (18% in 2014 to 27% in 2021) and Hispanic (6% in 2014, 9% in 2021) patients. Driven by intentional expansion efforts, several cancer types increased in frequency over time. Breast increased from 0% in 2014 to 16% in 2021, gynecologic increased from 0% to 12%, head and neck from 0% to 8%, and central nervous system from 0% to 5%. Corresponding decreases were noted in leukemia (47% to 14%) and lymphoma (18% to 12%). Program-contacted patients continued to represent those with metastatic disease (53% in 2014, 49% in 2021) and receiving systemic therapy (88% in 2014, 81% in 2021).
At a single public academic institution, we have shown the feasibility of an adolescent and young adult–specific cancer program with growing footprint and clinical volume, increasing from 6% of the total adolescent and young adult population to 25% over 7 years. As a consult and referral-based service, this is far from a random intervention. Thus, the present analysis serves as a lens through which to understand the results of intentional growth of an adolescent and young adult program at a single academic institution and the population of adolescents and young adults who received this supportive care over the initial phase of program development. Several publications have highlighted the need for this type of analysis to guide adolescent and young adult program evaluation and expansion efforts (10,11).
From its outset, our program has focused on improving delivery of needed cancer care to adolescents and young adults, leading to our cohort representing those on active treatment and with high-risk diseases (hematologic malignancies, metastatic cancer). Additionally, to improve care delivery, we have focused on patients facing additional barriers to care, such as adolescents navigating self-advocacy in the health-care system and patients of color facing structural barriers to care because of systemic racism.
Place of care is an important consideration for who is referred to and seen by our program. Patients with hematologic malignancies are often admitted for weeks at the time of diagnosis and initial treatment. As a captive audience, this was one of the primary populations to receive Adolescent and Young Adult Program support, especially in the early years of the program. Integrating into outpatient specialty cancer clinics, often siloed by disease group and subspecialty (ie, gynecologic oncology; surgical oncology; neuro-oncology; ear, nose, and throat), is a much steeper challenge that requires substantial outreach and logistical effort to be successful. Our group showed distinct progress in this, with growth in breast cancer, head and neck, and central nervous system malignancies. This is likely to be a common challenge and pattern of care delivery for new and growing adolescent and young adult programs.
Further, patients experiencing additional challenges are more likely to be referred by their treatment teams seeking additional support. Reflective of this, we saw higher proportions of historically underserved populations contacted by the program (Black and Hispanic patients), and our patients came from areas of lower income and educational achievement. This also contributes to higher numbers of program patients with metastatic disease and those receiving systemic therapy. These results align with our program’s equity mission to support patients with the greatest needs. However, we must acknowledge that this can be profoundly difficult work—caring for young patients with terminal illnesses, receiving high toxicity treatments, and facing additional social barriers. As centers develop adolescent and young adult programs, it is imperative to support frontline staff in this demanding and emotionally intensive work.
Several limitations must be noted. This is a single-center experience. We have previously published on our program development (12), funded through a collaborative effort between a nonprofit foundation and cancer center leadership. The development of any clinical program is unique to that institution, with no one-size-fits-all solutions, especially in adolescent and young adult care. Additionally, adolescent and young adult program contact was defined by clinical documentation, which is likely an underestimate as clinical notes are not universal.
Delivery of specialized adolescent and young adult cancer care is feasible at an academic center. Growth of this program over time has led to increasing clinical volume and contact with a sizeable proportion of adolescents and young adults with cancer. Programmatic initiatives to target patients with specific cancers have increased engagement with these subgroups. Adolescents and young adults with hematologic malignancies and metastatic cancer were most likely to receive contact from our program, as were those receiving systemic therapy. Program-contacted patients were also more likely to be Black and younger than noncontacted patients. Centers seeking to develop and grow adolescent and young adult programs should be aware of the high degree of complexity of young patients with cancer and adequately support their clinical teams working in this space.
Acknowledgements
We are grateful to our patients and their caregivers who give us the privilege of getting to know them and care for them during this difficult period of their lives and who inspire us to improve the care we deliver on a daily basis.
The study sponsor was not involved in the design of the study; the collection, analysis, or interpretation of the data; the writing of the manuscript; or the decision to submit the manuscript for publication.
This work was approved by our institutional review board. A waiver of consent was obtained given that the project involved retrospective secondary data analysis only.
Contributor Information
Jacob Stein, Division of Oncology, Department of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA; University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC, USA; Lineberger Comprehensive Cancer Center, Chapel Hill, NC, USA.
Alexis Wardell, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC, USA; Lineberger Comprehensive Cancer Center, Chapel Hill, NC, USA.
Dawn M Ritzwoller, Department of Maternal and Child Health, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
Catherine Swift, Lineberger Comprehensive Cancer Center, Chapel Hill, NC, USA; Adolescent and Young Adult Cancer Program, Comprehensive Cancer Support Program, Department of Psychiatry, University of North Carolina, Chapel Hill, NC, USA.
Melissa Matson, Lineberger Comprehensive Cancer Center, Chapel Hill, NC, USA; Adolescent and Young Adult Cancer Program, Comprehensive Cancer Support Program, Department of Psychiatry, University of North Carolina, Chapel Hill, NC, USA.
Hannah C Winslow, Lineberger Comprehensive Cancer Center, Chapel Hill, NC, USA; Adolescent and Young Adult Cancer Program, Comprehensive Cancer Support Program, Department of Psychiatry, University of North Carolina, Chapel Hill, NC, USA.
Hrishika Muthukrishnan, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC, USA.
Austin R Waters, Department of Health Policy and Management, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
Emily R Haines, Adolescent and Young Adult Cancer Program, Comprehensive Cancer Support Program, Department of Psychiatry, University of North Carolina, Chapel Hill, NC, USA; Department of Implementation Science, Wake Forest University School of Medicine, Winston-Salem, NC, USA.
Lauren Lux, Lineberger Comprehensive Cancer Center, Chapel Hill, NC, USA; Adolescent and Young Adult Cancer Program, Comprehensive Cancer Support Program, Department of Psychiatry, University of North Carolina, Chapel Hill, NC, USA.
Andrew B Smitherman, Lineberger Comprehensive Cancer Center, Chapel Hill, NC, USA; Adolescent and Young Adult Cancer Program, Comprehensive Cancer Support Program, Department of Psychiatry, University of North Carolina, Chapel Hill, NC, USA; Division of Hematology/Oncology, Department of Pediatrics, University of North Carolina, Chapel Hill, NC, USA.
Data availability
We will share aggregated and de-identified data with any interested researchers or regulatory bodies upon request and explanation of their plans for data use and protection. We do not publicly release electronic health record and cancer registry data given the potential for breach of confidentiality.
Author contributions
Jacob Stein, MD, MPH (Conceptualization; Data curation; Funding acquisition; Investigation; Methodology; Project administration; Resources; Supervision; Validation; Visualization; Writing—original draft; Writing—review & editing), Alexis Wardell, MS (Conceptualization; Data curation; Formal analysis; Methodology; Writing—original draft; Writing—review & editing), Dawn M. Ritzwoller, MPH (Data curation; Project administration; Writing—original draft; Writing—review & editing), Catherine Swift, LCSW (Conceptualization; Methodology; Resources; Writing—review & editing), Melissa Matson, MSN, RN (Conceptualization; Methodology; Resources; Writing—review & editing), Hannah C. Winslow, MSW, MPH (Project administration; Writing—original draft; Writing—review & editing), Hrishika Muthukrishnan, BS (Writing—original draft; Writing—review & editing), Austin R. Waters, PhD (Conceptualization; Methodology; Writing—original draft; Writing—review & editing), Emily R. Haines, PhD (Conceptualization; Methodology; Writing—review & editing), Lauren Lux, LCSW (Conceptualization; Methodology; Resources; Writing—review & editing), and Andrew B. Smitherman, MD, MSc (Conceptualization; Writing—original draft; Writing—review & editing).
Funding
This work was supported by a UNC Lineberger Comprehensive Cancer Center Developmental Award, which is supported in part by P30 CA016086 Cancer Center Core Support Grant.
Conflicts of interest
None of the authors have any relevant conflicts of interest, including financial interest with any company or financial connection that might raise the question of bias in the published work.
References
- 1. American Cancer Society. Cancer Treatment & Survivorship Facts & Figures 2019-2021. American Cancer Society; 2019. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2019.html. Accessed March 15, 2024. [Google Scholar]
- 2. Coccia PF. Overview of adolescent and young adult oncology. J Oncol Pract. 2019;15(5):235-237. doi: 10.1200/JOP.19.00075 [DOI] [PubMed] [Google Scholar]
- 3. Keegan THM, Ries LAG, Barr RD, et al. ; National Cancer Institute Next Steps for Adolescent and Young Adult Oncology Epidemiology Working Group. Comparison of cancer survival trends in the United States of adolescents and young adults with those in children and older adults. Cancer. 2016;122(7):1009-1016. doi: 10.1002/cncr.29869 [DOI] [PubMed] [Google Scholar]
- 4. Dyson GJ, Thompson K, Palmer S, Thomas DM, Schofield P.. The relationship between unmet needs and distress amongst young people with cancer. Support Care Cancer. 2012;20(1):75-85. doi: 10.1007/s00520-010-1059-7 [DOI] [PubMed] [Google Scholar]
- 5. Zebrack BJ, Block R, Hayes-Lattin B, et al. Psychosocial service use and unmet need among recently diagnosed adolescent and young adult cancer patients. Cancer. 2013;119(1):201-214. doi: 10.1002/cncr.27713 [DOI] [PubMed] [Google Scholar]
- 6. Coccia PF, Pappo AS, Beaupin L, et al. Adolescent and young adult oncology, version 2.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2018;16(1):66-97. doi: 10.6004/jnccn.2018.0001 [DOI] [PubMed] [Google Scholar]
- 7. Zebrack B, Mathews-Bradshaw B, Siegel S; LIVESTRONG Young Adult Alliance. Quality cancer care for adolescents and young adults: A position statement. J Clin Oncol. 2010;28(32):4862-4867. doi: 10.1200/JClinOncol.2010.30.5417 [DOI] [PubMed] [Google Scholar]
- 8. Smith AW, Seibel NL, Lewis DR, et al. Next steps for adolescent and young adult oncology workshop: an update on progress and recommendations for the future. Cancer. 2016;122(7):988-999. doi: 10.1002/cncr.29870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ferrari A, Stark D, Peccatori FA, et al. Adolescents and young adults (AYA) with cancer: A position paper from the AYA Working Group of the European Society for Medical Oncology (ESMO) and the European Society for Paediatric Oncology (SIOPE). ESMO Open. 2021;6(2):100096. doi: 10.1016/j.esmoop.2021.100096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kirchhoff AC, Waters AR, Chevrier A, Wolfson JA.. Access to care for adolescents and young adults with cancer in the united states: State of the literature. J Clin Oncol. 2024;42(6):642-652. doi: 10.1200/JClinOncol.23.01027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Haines E, Asad S, Lux L, et al. Guidance to support the implementation of specialized adolescent and young adult cancer care: a qualitative analysis of cancer programs. J Clin Oncol Oncol Pract. 2022;18(9):e1513-e1521. doi: 10.1200/OP.22.00063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Haines ER, Lux L, Stein J, et al. Developing a Comprehensive Adolescent and Young Adult Cancer Program: Lessons Learned from 7 Years of Growth and Progress. J Adolesc Young Adult Oncol. 2023;12(6):868-878. doi: 10.1089/jayao.2023.0015 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
We will share aggregated and de-identified data with any interested researchers or regulatory bodies upon request and explanation of their plans for data use and protection. We do not publicly release electronic health record and cancer registry data given the potential for breach of confidentiality.