Abstract
Background
The relationship between education and cardiometabolic biomarkers is contextually dependent on both inter-country and intra-country factors. This study aimed to examine educational differences in cardiometabolic biomarkers among middle-aged and older adults in the US, Mexico, China, and India, and whether this relationship is modified by urbanicity of residence.
Methods
Data were from contemporary cross-sectional waves of the US Health and Retirement Study (HRS; 2016/17, n = 19,608), the Mexican Health and Aging Study (MHAS; 2015, n = 12,356), the China Health and Retirement Longitudinal Study (CHARLS; 2015/16, n = 13,268), and the Longitudinal Aging Study in India (LASI; 2017/19, n = 47,838). To account for substantial variations in educational distribution across the four countries, we measured education attainment in two ways: by categorizing education levels into binary classifications (‘lower education: lower secondary education or below' vs. 'higher education: upper secondary education or above') to assess absolute education attainment, and by using within-country percentile ranks to capture relative education attainment. We assessed educational differences in four cardiometabolic biomarkers: body mass index (BMI), systolic blood pressure (SBP), glycated haemoglobin (HbA1c), and total cholesterol. We tested whether urbanicity of residence modified the relationship between education and these cardiometabolic biomarkers.
Results
The proportion of individuals with higher education was 82.6% in the US, 15.6% in Mexico, 10.6% in China, and 16.8% in India. In the US, higher education was associated with lower SBP (−2.74 mmHg, 95% CI: −3.62, −1.86) and HbA1c (−0.14%, 95% CI: −0.20, −0.08), but higher total cholesterol (3.33 mg/dL, 95% CI: 1.41, 5.25). In Mexico, higher education was associated with lower BMI only (−0.51 kg/m2, 95% CI: −0.76, −0.26). In China, higher education was not associated with any biomarker. In India, higher education was associated with higher BMI (1.61 kg/m2, 95% CI: 1.49, 1.73), SBP (1.67 mmHg, 95% CI: 1.16, 2.18), and HbA1c (0.35%, 95% CI: 0.19, 0.51). The association between education and cardiometabolic biomarkers was modified by urbanicity in China and India but not in the US or Mexico. In both China and India, relationships between education and cardiometabolic biomarkers were stronger among rural residents compared to those among urban residents. Results based on relative education attainment showed similar patterns in terms of the direction of the effect estimates, despite some discrepancies in statistical significance.
Interpretation
There is a complex relationship between education and cardiometabolic biomarkers across countries and by urbanicity of residence. This complexity underscores the importance of accounting for contextual factors when devising strategies to enhance cardiometabolic health in various settings.
Highlights
-
•
The study examines relationships between education and cardiometabolic biomarkers among aging populations in four countries.
-
•
The relationships between education and different cardiometabolic biomarkers vary across four countries.
-
•
Urbanicity modifies education-cardiometabolic biomarker associations in China and India, but not in the US or Mexico.
-
•
Contextual factors are important for complex education-cardiometabolic biomarker relationships within and across countries.
1. Introduction
Cardiometabolic diseases are prevalent at older age and lead to heavy financial burdens, compromised quality of life, and high risks of morbidity and mortality (Miranda et al., 2019; Pongiglione et al., 2022; Roth et al., 2020; Xu et al., 2022). Despite persistent prevention efforts for decades, high-income countries (HICs) have long observed a high prevalence of cardiometabolic conditions, including obesity, hypertension, diabetes, and dyslipidemia (Miranda et al., 2019; Schultz et al., 2018). For example, in the United States (US) and Europe, large-scale public health initiatives like the Million Hearts Initiative and NHS Health Check have been launched decades ago to reduce cardiometabolic risk factors (Blue et al., 2023; Chang et al., 2015; Frieden & Berwick, 2011). However, these initiatives face persistent challenges due to lifestyle factors, aging populations, and evolving health risks.
Since the 1980s, with the emerging global obesity epidemic, low- and middle-income countries (LMICs) also have observed a surge in the number of people living with adverse cardiometabolic conditions (Allen et al., 2017; Miranda et al., 2019; Schultz et al., 2018). The rapid increase in cardiometabolic diseases in LMICs is primarily driven by modern lifestyle changes. These include factors such as the reduced cost of food, a diet rich in processed foods, and decreased physical activity, all of which are further compounded by economic development and urbanization (Mills et al., 2020; Miranda et al., 2019; Sattar et al., 2020; Valenzuela et al., 2023). For example, as LMICs develop economically, food becomes more accessible, especially processed and packaged; in addition, urbanization leads to sedentary lifestyles and easier access to processed foods in urban areas, contributing to the increase in cardiometabolic diseases (Goryakin & Suhrcke, 2014; Westbury et al., 2021). In these regions, prevention efforts have focused on strengthening primary healthcare systems and implementing community-based interventions, often with limited resources and infrastructure (Maria et al., 2021; Sacks et al., 2018). Despite these challenges, there have been persistent and ongoing efforts in both HICs and LMICs to mitigate the growing burden of cardiometabolic diseases.
Socioeconomic conditions, widely recognized as fundamental determinants of health, have been extensively linked to cardiometabolic health, yet exhibiting substantial variation in associations across different countries (Allen et al., 2017; Clark et al., 2009; Miranda et al., 2019; Rosengren et al., 2019; Schultz et al., 2018). For example, in HICs, adverse cardiometabolic conditions are more likely to occur among people of low socioeconomic status (SES) (Pongiglione et al., 2022; Schultz et al., 2018). In contrast, in LMICs, while these conditions are more common among people with high SES, they are rapidly proliferating among those with low SES (Dinsa et al., 2012; Hu et al., 2017; Lamb et al., 2021; Miranda et al., 2019). This pattern, where associations between SES and cardiometabolic health diverge in different directions across populations from countries at varying stages of economic development, is known as the ‘reversal hypothesis’ (Kirschbaum et al., 2022; Pampel et al., 2012). One possible explanation is that the proximate mediators of the relationship between SES and cardiovascular health differ between HICs and LMICs. For example, in HICs, high SES may contribute to healthy eating and regular exercise, whereas in LMICs, it may enable the consumption of high-calorie foods and the avoidance of physically demanding work (Clark et al., 2009; Kirschbaum et al., 2022; Pampel et al., 2012). This demonstrates that the relationship between SES and cardiometabolic health evolves alongside social and economic progression.
Education, an important marker of SES, has shown heterogeneous associations with cardiometabolic health across countries (Hill-Briggs et al., 2020; Leng et al., 2015; Williams et al., 2018). In the US and Mexico, many studies have reported negative associations between education attainment and certain cardiometabolic biomarkers, such as body size index, blood pressure, and glucose levels (Addey et al., 2023; Kubota et al., 2017). However, findings from China present a mixed picture, depending on the population being studied (Bi et al., 2015; Hu et al., 2017; Kodali et al., 2023; Li et al., 2018; Li & Lumey, 2019a; Ruan et al., 2018; Zaman et al., 2012). In India, most studies report positive associations between education and cardiometabolic health indicators (Corsi & Subramanian, 2019; Lee et al., 2022; Subramanian et al., 2013). Economic developments and epidemiological transitions of these countries provide a backdrop to these inconsistencies in associations. For example, while the US began its epidemiologic transition before the mid-20th century with cardiometabolic diseases taking precedence(Omran, 1977), Mexico's transition began around the 1980s (Stevens et al., 2008). In comparison, China and India started their epidemiologic transitions even later, in the 1990s and 2000s, respectively (Li et al., 2019; Li, ÓGráda, & Lumey, 2024; Li & Lumey, 2017; Nations within a nation, 2017; Yang et al., 2013). Given the large and growing populations of older adults in China and India, these shifts warrant attention as they are critical to forecasting population health trends globally in the coming decades (Hu et al., 2017).
Within countries, the relationship between education and cardiometabolic health can be modified by country-specific contextual factors, such as urbanicity of residence (i.e., rural vs. urban residence). Urbanicity, especially in LMICs, serves as an indicator of economic progress, and rural and urban regions can greatly differ in terms of environment, diet, lifestyle, and healthcare access (Neuman et al., 2013; Rosengren et al., 2019). A recent nationwide study in India reported that the positive association between obesity and education is stronger among rural residents compared to urban residents (Barua, 2023). Such intra-country variations in the relationship between education and cardiometabolic health have also been documented in many other countries (Rosengren et al., 2019; Zhang, 2020; Zimmer & Kwong, 2004). However, the influence of urbanicity on the education-cardiometabolic health relationship may not be consistent across countries, as the contrasts between rural and urban areas can differ markedly from one country to another. For example, in the US, rural residents have more limited access to healthy food options and tend to consume more ultra-processed food and sugar-sweetened beverages compared to their urban counterparts (Losada-Rojas et al., 2021; McCullough et al., 2022; Sharkey et al., 2011; Trivedi et al., 2015). Conversely, in countries like Mexico, China, and India, rural residents are less likely to consume ultra-processed food and sugar-sweetened beverages compared to urban dwellers (Lara-Castor et al., 2023; López-Olmedo et al., 2018; Mathur et al., 2020; Navarro-Meza et al., 2014; Zou et al., 2015). This urban-rural divide, marked by differences in economic and social development, creates distinct environments that may modify the relationship between education and cardiometabolic health, leading to country-specific variations.
The above examples underscore the importance of contextualizing both inter-country and intra-country factors when studying the interplay between education and cardiometabolic health. In this study, we leveraged four population-based studies of middle-aged and older adults in the US, Mexico, China, and India to examine the relationships between education and four measured cardiometabolic biomarkers, including body mass index (BMI), blood pressure, glucose, and lipids (Perianayagam et al., 2022; Sonnega et al., 2014; Wong et al., 2017; Zhao et al., 2014). We first compared educational differences in cardiometabolic biomarkers in each country. Subsequently, we examined whether these differences varied by urbanicity of residence. By comparing educational differences in cardiometabolic biomarkers across countries and within urban and rural settings, we aim to explore how contextual factors might influence these relationships. Understanding these patterns can provide preliminary insights into potential mechanisms, thereby informing the development of more targeted and effective public health strategies.
2. Methods
2.1. Data and sample
Data were used from the cross-sectional waves of the 2016-17 US Health and Retirement Study (HRS), the 2015 Mexican Health and Aging Study (MHAS), the 2015-16 China Health and Retirement Longitudinal Study (CHARLS), and the 2017-19 Longitudinal Aging Study in India (LASI) (Perianayagam et al., 2022; Sonnega et al., 2014; Wong et al., 2017; Zhao et al., 2014). The four studies are independently conducted, and are harmonized international partner studies of the US HRS, each with its own schedule of data collection. While the years of data collection are not identical across all studies, we have selected waves that fall within a roughly similar time frame (2015–2019) to facilitate comparisons (Gross et al., 2023; Li, Liu, et al., 2024; Varghese et al., 2023). The 2017-19 LASI wave is the first publicly available wave for India, making it necessary to select the 2015 MHAS, 2016 HRS, and 2015 CHARLS waves as they are the closest in terms of data availability. This approach allows us to draw the most meaningful comparisons across countries.
We selected these studies because they were conducted in countries at varying stages of economic development and epidemiologic transitions. According to the World Bank, since the post-World War II introduction of country classifications by income levels, the US has been categorized as a high-income country; Mexico achieved upper-middle income status in 1990; China in 2010; and India was classified as a lower-middle income country in 2007 (Country and Lending Groups, 2023). To provide further information on the socioeconomic and epidemiologic conditions of these countries during the study period, we summarized several key indicators including GDP per capita, urban/rural population ratio, prevalence of chronic conditions, and leading causes of death for each country between 2015 and 2020 (Supplementary Table 1). (World Bank Open Data, 2023; Global burden of 369 diseases, 2020; revision of world urbanization prospects, 2018) For example, the table shows a stark contrast in GDP per capita, ranging from $59,800 in the United States to $2100 in India. Additionally, the prevalence of obesity varies widely, with the US having the highest prevalence of 40.0% compared to 3.4% in India.
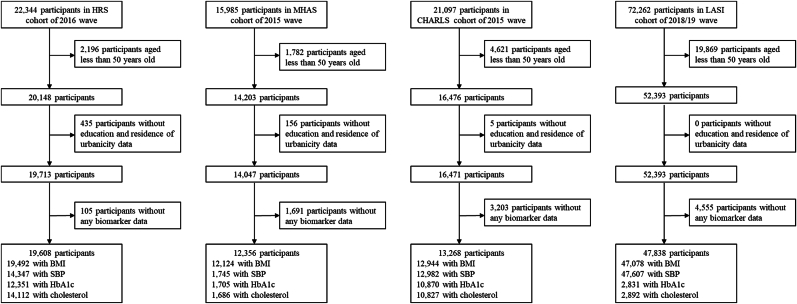
All four studies recruited middle-aged and older adults using sampling strategies to make their samples nationally representative. They administered similar designs and questionnaires (Supplementary Table 2). The HRS and MHAS surveyed individuals aged 50 and above, and their spouses irrespective of age. The CHARLS and LASI surveyed individuals aged 45 and above, and their spouses regardless of age. To facilitate cross-national comparison studies, we used harmonized variables constructed by the Gateway to the Global Aging Data. The harmonized data contain ready-to-use measures that are comparable between different countries’ studies. We included participants aged 50 and over in each of the four studies (Fig. 1). There were 20,148, 14,203, 16,476, and 52,393 participants aged 50 years and over in these selected cross-sectional waves of HRS, MHAS, CHARLS, and LASI, respectively. We further restricted our analysis to participants with complete information on education, residence of urbanicity, and at least one of the four selected cardiometabolic biomarkers described in the next section. This led to the inclusion of 19,608, 12,356, 13,268, and 47,838 participants for each of the four studies, respectively.
Fig. 1.
Flow diagram across countries.
2.2. Measures
Cardiometabolic biomarkers. Cardiometabolic health encompasses a variety of interrelated anthropometric and blood biomarkers such as adiposity, blood pressure, blood glucose, and lipid profiles (O'Hearn et al., 2022). We selected four biomarkers that represent essential and distinct aspects of cardiometabolic health: body mass index (BMI, kg/m2), systolic blood pressure (SBP, mmHg), glycated haemoglobin (HbA1c, %), and total cholesterol (mg/dL). (O'Hearn et al., 2022; Castelli et al., 1992; Sarwar et al., 2010; Dudina et al., 2011; Ettehad et al., 2016).
For the HRS, biomarker data in 2014 and 2016 were combined to maximize the sample size because HRS collects anthropometric measures and dried blood spots (DBS) biomarkers from half of its sample each wave (Sonnega et al., 2014). MHAS collected anthropometric measures from a subsample of 13,064 participants in 2015 and other biomarkers from a random subsample of 2089 participants in 2012 (Wong et al., 2017). CHARLS collected anthropometric measures from a subsample of 16,234 participants and blood samples from an overlapping subsample of 13,013 participants in 2015 (Chen et al., 2019). While LASI assessed anthropometric and blood pressure measures from over 66,000 participants, additional blood biomarkers of HbA1c and total cholesterol were only accessible for 3000 participants through an ancillary study, the LASI-DAD (Lee et al., 2019). Details on the measurement of these biomarkers are described below and summarized in Supplementary Table 3.
BMI is a crude measure of body fat based on height and weight (Amato et al., 2013). Specifically, weight was measured using a Healthometer 830 KL scale in HRS, Omron HN-286 scale in CHARLS, and a SECA 803 digital weighing scale in LASI. Height was measured by trained interviewers using a tape while the respondent was standing against the wall without shoes in HRS, a SecaTM213 stadiometer in CHARLS, and a standardized stadiometer in LASI. In MHAS, both weight and height were self-reported, which has been validated in this cohort (Avila et al., 2021; Avila-Funes et al., 2004).
SBP measures the pressure in arteries when the heart beats, which is a useful predictor of cardiovascular and renal events, especially among people aged 50 years and over (Franklin et al., 2001; Mourad, 2008). Blood pressure was measured three times during each visit in HRS, CHARLS, and LASI, and was measured twice in MHAS using different validated versions of Omron blood pressure monitors. If there were three valid SBP measurements, we calculated the mean of the second and third measurements. If there were two valid SBP measurements, SBP was calculated as the mean of both measurements. In CHARLS, the SBP of 35 participants from one residence community was recorded as lower than their diastolic blood pressure (DBP), which was rectified by switching these records.
HbA1c reflects the average blood glucose level over the past two to three months. In HRS, the Bio-Rad Laboratories Variant II High Pressure Liquid Chromatography (HPLC) System was utilized for HbA1c measurements, which were converted into NHANES (National Health and Nutrition Examination Survey) equivalents (Crimmins et al., 2013; Kim et al., 2023). In MHAS, the A1CNOW device was employed for assays (Jiang et al., 2014; Wong et al., 2015). In CHARLS, KingMed Diagnostics performed the assays using venous blood samples, with daily quality checks by the provider and weekly assessments by the CHARLS research team (Chen et al., 2019). In LASI, the Bio-Rad D10 was utilized for HbA1c measurements, with consistent daily quality control maintained at the Delhi Metropolis laboratory (Lee et al., 2020).
Total cholesterol, which indicates the entirety of cholesterol circulating in the bloodstream, serves as a critical cardiovascular disease risk factor (Peters et al., 2016). In both HRS and CHARLS, total cholesterol was measured in a similar way as HbA1c (Chen et al., 2019; Crimmins et al., 2013). In MHAS and LASI, total cholesterol was measured using Architect equipment (Lee et al., 2020; Wong et al., 2015). Most of these studies also collected and provided data on high-density lipoproteins (HDL) and low-density lipoproteins (LDL), except for LDL in the MHAS study. These two biomarkers were used in sensitivity analyses to complement findings based on total cholesterol. We examined the distribution of each biomarker among men and women separately from each country and further set the lower and upper thresholds at 1% and 99% levels to reduce the influence of extreme data. We also examined the correlation between each pair of biomarkers.
To aid in the interpretation of our study results, we provided a classification of these biomarkers. BMI was classified as underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), and overweight/obese (≥25.0 kg/m2) (Obesity Preventing 2000). SBP was categorized as normal (<120 mmHg), elevated (120–129 mmHg), and hypertensive (≥130 mmHg) (Whelton et al., 2017). HbA1c was categorized as normal (<5.7%), prediabetic (5.7–6.4%), and diabetic (≥6.5%) (WHO Guidelines Approved by the Guidelines Review Committee, 2011). Total cholesterol was classified as desirable (<200 mg/dL), borderline high (200–239 mg/dL), and high (≥240 mg/dL) (Third Report of the National Cholesterol Education Program (NCEP and), 2002). It is important to note that these cut-offs do not account for population differences, such as varying BMI thresholds for overweight and obesity between Asian and Western populations (Appropriate body, 2004).
Education attainment. Across the four studies, education was reported as the highest level attained based on country-specific response categories. Given the varying distributions of education attainment across countries, we employed two methods to measure both absolute and relative education attainment. Results from both methods were presented as the main results to provide a comprehensive understanding of the relationship between education and cardiometabolic biomarkers.
First, to measure absolute education attainment, we harmonized levels of education based on the 2011 International Standard Classification of Education (ISCED) and categorized participants into two groups: 'lower secondary education or below' (‘lower education’) and 'upper secondary education or above' (‘higher education’) (Gross et al., 2023; International Standard Classification of Education, 2012). Dichotomizing education in this way allows us to create a harmonized measure across the four countries, addressing issues of sparse data at the lower and upper ends of the distribution of education attainment in different countries. This method also allows for the examination and comparison of absolute differences in binary education levels and their relationships with cardiometabolic biomarkers across countries. Second, we assessed individuals' relative education attainment within their country-specific contexts by creating a percentile rank of education attainment within each country. This method captures participants' relative education attainment within each country.
Urbanicity of residence. Across countries, urbanicity of residence was dichotomized into urban and rural areas. Each study employed specific criteria to categorize residences. In HRS, the residence was coded based on Beale Rural Urban 2013 coding. (Service UER) It distinguishes metropolitan counties by the population size of their metro area, and nonmetropolitan counties by the degree of urbanization and adjacency to a metro area. In MHAS, residence was coded based on the standard values used by the Mexican Statistical Bureau (INEGI) (Inform á et al). It classifies areas with ≥15,000 residents as urban areas and less than this cutoff as rural areas. In CHARLS, the residence was determined based on the National Bureau of Statistics in China in 2011, where the distinction between urban and rural areas is largely based on a combination of administrative criteria and population size and density (Qin & Zhang, 2014). In LASI, residence was classified as urban or rural based on the Census of India in 2011 (Goel & Gross, 2019). According to the Indian census, a town is labeled as ‘statutory’ if it has a municipality, corporation, cantonment board, or a notified town area committee. It was designated a non-statutory in case it did not have any of the above but had at least 5000 people, 75% of its male residents were engaged in non-agricultural pursuits, and the density of population was at least 400 habitants per square kilometer. Other areas were considered rural. Despite the variations in urban classification across these studies, a shared theme is the consideration of development level and population size in defining urban and rural areas.
Covariates. We included covariates that could be confounders (common causes) of associations between education and cardiometabolic biomarkers. These included age at the time of survey (in years), gender (men, women), highest level of parental education (lower education: lower secondary education or below, higher education: upper secondary education or above), and height (in meters with two decimal places). Although our study is cross-sectional, we prioritized covariates that reflect potential confounders established earlier in life to avoid introducing mediators that could obscure the direct relationship between education and cardiometabolic health. The highest level of parental education was coded as the highest of paternal or maternal education levels. Height was used as a proxy for net nutritional status during childhood (Perkins et al., 2016). It was used as a covariate in regression models for the above selected cardiometabolic biomarkers, except for BMI. In HRS, self-reported race/ethnicity was included (non-Hispanic white, non-Hispanic black, Hispanic, and other). In China, Hukou registration status was included (agricultural or non-agricultural). In India, caste was included (general or none or other backward caste, scheduled caste, or scheduled tribe). The covariate with the highest amount of missing data was the highest level of parental education, with a missingness proportion reaching 19.67% in the HRS, as indicated in Supplementary Table 4. To account for missing data, we used multiple imputation by chained equations considering all the covariates used in the main analysis (Cho et al., 2023; Li, Liu, et al., 2024; Varghese et al., 2023).
2.3. Statistical analysis
We examined the distribution of demographic characteristics and cardiometabolic biomarkers across countries. Within each country, we utilized multiple linear regression models to examine the association between education and each of the four cardiometabolic biomarkers. Models were adjusted for urbanicity of residence, age, gender, the highest level of parental education, height (except for models of BMI), and the country-specific covariate. We added an interaction term between education and urbanicity of residence to examine whether urbanicity modifies the association between education and each of the cardiometabolic biomarkers. Analyses based on both absolute and relative education attainments were conducted.
We performed four sets of sensitivity analyses to assess their robustness and provide a more comprehensive understanding of our findings. First, we re-ran our analyses using HDL and LDL as separate outcomes in each country where these data were available, complementing the findings based on total cholesterol. Second, we re-ran our analyses using covariates before imputation to assess the impact of imputation on findings. Third, we further added a three-way interaction term for education, urbanicity of residence, and gender, alongside all lower-order two-way interactions, to examine if there were gender-specific patterns in the above results. Fourth, to determine if there are differences across countries, we conducted a pooled analysis, modeling each cardiometabolic biomarker as a function of education, urbanicity of residence, shared covariates, country fixed effects, and a three-way interaction between education, urbanicity, and country along with the corresponding two-way interaction terms (Li, Liu, et al., 2024; Varghese et al., 2023). Since the results based on both absolute and relative education attainments showed similar patterns, with consistent directions of effect estimates despite some discrepancies in statistical significance, we reported only the results based on absolute education attainment in the sensitivity analyses for simplicity. All analyses were conducted using R version 4.2.
3. Results
Our analysis included 19,608 participants from the US, 12,356 participants from Mexico, 13,268 participants from China, and 47,838 participants from India (Table 1). The distribution of education varied notably among these countries. In the USA, 82.6% of participants had achieved an education level of upper secondary or higher. In contrast, in Mexico, China, and India, the proportions with an upper secondary education or higher were 15.6%, 10.6%, and 16.8%, respectively. In each country, urban residents were more likely to have an upper secondary education or above compared to their rural counterparts, except for the US (Supplementary Table 5).
Table 1.
Summary of sociodemographic characteristics and cardiometabolic biomarkers by urbanicity of residence and countries.
| US (HRS 2016/17) |
Mexico (MHAS 2015) |
China (CHARLS 2015/16) |
India (LASI 2017/19) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Rural | Urban | Total | Rural | Urban | Total | Rural | Urban | Total | Rural | Urban | |
| Sample size, N | 19,608 | 4539 | 15,069 | 12,356 | 3358 | 8998 | 13,268 | 8261 | 5007 | 47,838 | 31,460 | 16,378 |
| Age (years) | 66.55 (11.21) | 68.34 (11.18) | 66.01 (11.16) | 66.60 (9.73) | 66.40 (10.10) | 66.68 (9.58) | 62.87 (8.85) | 62.93 (8.80) | 62.77 (8.93) | 62.90 (9.30) | 63.04 (9.36) | 62.63 (9.19) |
|
Gender, N and % |
||||||||||||
| Men | 8268 (42.17) | 1903 (42.23) | 6365 (41.93) | 5494 (44.46) | 1654 (49.26) | 3840 (42.68) | 6389 (48.15) | 4027 (48.75) | 2362 (47.17) | 22,389 (46.80) | 14,905 (47.38) | 7484 (45.69) |
| Women | 11,340 (57.83) | 2636 (57.76) | 8704 (58.07) | 6862 (55.54) | 1704 (50.74) | 5158 (57.32) | 6879 (51.85) | 4234 (51.25) | 2645 (52.83) | 25,449 (53.20) | 16,555 (52.62) | 8894 (54.30) |
|
Education, N and % |
||||||||||||
| Lower secondary and below | 3408 (17.38) | 768 (16.92) | 2640 (17.52) | 10,435 (84.45) | 3047 (94.75) | 7159 (80.37) | 11,864 (89.42) | 7716 (93.40) | 4148 (82.84) | 39,793 (83.18) | 28,401 (90.28) | 11,392 (69.56) |
| Upper secondary and above | 16,200 (82.62) | 3771 (83.07) | 12,429 (82.48) | 1921 (15.55) | 169 (5.25) | 1749 (19.63) | 1404 (10.58) | 545 (6.60) | 859 (17.16) | 8045 (16.82) | 3059 (9.72) | 4986 (30.44) |
|
Parental education, N and % |
||||||||||||
| Lower secondary and below | 7677 (39.15) | 1894 (41.73) | 5783 (38.38) | 11,105 (89.88) | 3241 (96.52) | 7864 (87.40) | 12,785 (96.36) | 8079 (97.80) | 4706 (93.99) | 45,021 (94.11) | 30,562 (97.15) | 14,459 (88.28) |
| Upper secondary and above | 11,931 (60.85) | 2645 (58.27) | 9286 (61.62) | 1251 (10.12) | 117 (3.48) | 1134 (12.60) | 483 (3.64) | 182 (2.20) | 301 (6.01) | 2817 (5.89) | 898 (2.85) | 1919 (11.72) |
| BMI (kg/m2) | 29.41 (6.34) | 29.56 (6.39) | 29.36 (6.32) | 27.42 (4.79) | 26.93 (4.85) | 27.60 (4.76) | 23.69 (3.62) | 23.31 (3.59) | 24.31 (3.58) | 22.59 (4.60) | 21.58 (4.23) | 24.52 (4.68) |
| SBP (mmHg) | 128.05 (18.93) | 128.78 (18.98) | 127.84 (18.83) | 138.94 (20.52) | 138.79 (20.43) | 139.27 (20.75) | 128.84 (19.86) | 128.47 (20.01) | 129.47 (19.58) | 130.58 (19.10) | 129.62 (19.36) | 132.41 (18.46) |
| HbA1c (%) | 6.01 (1.05) | 6.02 (1.01) | 6.01 (1.07) | 6.84 (1.84) | 6.82 (1.80) | 6.85 (1.85) | 6.01 (0.90) | 5.96 (0.83) | 6.09 (0.99) | 6.28 (1.48) | 6.10 (1.32) | 6.62 (1.70) |
| Total cholesterol (mg/dL) | 190.53 (41.55) | 191.18 (42.28) | 190.33 (41.31) | 201.79 (39.95) | 199.62 (39.71) | 202.74 (40.04) | 184.85 (34.98) | 186.53 (35.30) | 183.82 (34.75) | 183.72 (41.10) | 182.68 (39.76) | 185.61 (43.40) |
Summary statistics for the four primary cardiometabolic biomarkers, including BMI, SBP, HbA1c, and total cholesterol, are also presented in Table 1. A clear gradient in average BMI across countries was observed in line with its economic development and stage in the epidemiologic transition: the US (29.41 kg/m2), and then in Mexico (27.42 kg/m2), China (23.69 kg/m2), and India (22.59 kg/m2). The distributions of the four main cardiometabolic biomarkers, including BMI, SBP, HbA1c, and total cholesterol, among men and women in each country are in Supplementary Fig. 1. Women had consistently higher levels of total cholesterol across all countries, while the distributions of the other three biomarkers tended to overlap between men and women. In each country, most of the four cardiometabolic biomarkers correlated with each other except for Mexico (Supplementary Table 6).
3.1. Associations of absolute education attainment with cardiometabolic biomarkers
Regression models that did not include the interaction term between absolute education attainment and urbanicity of residence showed the relationship between education and each of the four cardiometabolic biomarkers (Table 2 Models A). In the US, higher education (upper secondary education or above) was associated with lower SBP (−2.74 mmHg, 95% CI: −3.62, −1.86), lower HbA1c (−0.14%, 95% CI: −0.20, −0.08), and higher total cholesterol (3.33 mg/dL, 95% CI: 1.41, 5.25), but not with BMI. In Mexico, higher education was associated with lower BMI (−0.51 kg/m2, 95% CI: −0.76, −0.26) but not with SBP, HbA1c, and total cholesterol. In China, higher education was not associated with any of these biomarkers. In India, higher education was associated with higher BMI (1.61 kg/m2, 95% CI: 1.49, 1.73), higher SBP (1.67 mmHg, 95% CI: 1.16, 2.18), and higher HbA1c (0.35%, 95% CI: 0.19, 0.51), but not with total cholesterol.
Table 2.
Regression analysis of the association between absolute education attainment and cardiometabolic biomarkers.
| US (HRS 2016/17) | Mexico (MHAS 2015) | China (CHARLS 2015/16) | India (LASI 2017/19) | ||
|---|---|---|---|---|---|
| Estimate (95% CI) | Estimate (95% CI) | Estimate (95% CI) | Estimate (95% CI) | ||
| Models A. No interaction term between education and residence added | |||||
| BMI (kg/m2) | |||||
| Education | Lower secondary and below | Ref | Ref | Ref | Ref |
| Upper secondary and above | −0.03 (−0.28, 0.22) | −0.51 (-0.76, -0.26) | 0.19 (−0.02, 0.40) | 1.61 (1.49, 1.73) | |
| SBP (mmHg) | |||||
| Education | Lower secondary and below | Ref | Ref | Ref | Ref |
| Upper secondary and above | −2.74 (-3.62, -1.86) | 0.01 (−3.03, 3.05) | −0.49 (−1.65, 0.67) | 1.67 (1.16, 2.18) | |
| HbA1c (%) | |||||
| Education | Lower secondary and below | Ref | Ref | Ref | Ref |
| Upper secondary and above | −0.14 (-0.20, -0.08) | −0.17 (−0.44, 0.10) | 0.02 (−0.04, 0.08) | 0.35 (0.19, 0.51) | |
| Total cholesterol (mg/dL) | |||||
| Education | Lower secondary and below | Ref | Ref | Ref | Ref |
| Upper secondary and above | 3.33 (1.41, 5.25) | 0.21 (−5.92, 6.34) | −0.19 (−2.44, 2.06) | 0.27 (−2.91, 3.45) | |
| Models B. Interaction term between education and residence added | |||||
| BMI (kg/m2) | |||||
| Education | Lower secondary and below | Ref | Ref | Ref | Ref |
| Upper secondary and above | 0.00 (−0.49, 0.49) | 0.18 (−0.55, 0.91) | 0.52 (0.21, 0.83) | 2.11 (1.93, 2.29) | |
| Residence | Rural | Ref | Ref | Ref | Ref |
| Urban | −0.59 (-1.10, -0.08) | 0.78 (0.58, 0.98) | 0.76 (0.60, 0.92) | 2.47 (2.37, 2.57) | |
| Interaction | Upper × Urban | −0.05 (−0.60, 0.50) | −0.77 (−1.55, 0.01) | −0.57 (-0.98, -0.16) | −0.90 (-1.12, -0.68) |
| SBP (mmHg) | |||||
| Education | Lower secondary and below | Ref | Ref | Ref | Ref |
| Upper secondary and above | −4.16 (-5.89, -2.45) | −4.66 (−12.21, 2.89) | 1.09 (−0.63, 2.81) | 3.19 (2.46, 3.92) | |
| Residence | Rural | Ref | Ref | Ref | Ref |
| Urban | −2.60 (-4.36, -0.84) | −1.02 (−3.23, 1.19) | 1.86 (1.06, 2.66) | 3.29 (2.88, 3.70) | |
| Interaction | Upper × Urban | 1.88 (−0.04, 3.80) | 5.49 (−2.62, 13.60) | −2.77 (-5.00, -0.54) | −2.78 (-3.72, -1.84) |
| HbA1c (%) | |||||
| Education | Lower secondary and below | Ref | Ref | Ref | Ref |
| Upper secondary and above | −0.07 (−0.17, 0.03) | 0.02 (−0.67, 0.71) | 0.11 (0.03, 0.19) | 0.49 (0.27, 0.71) | |
| Residence | Rural | Ref | Ref | Ref | Ref |
| Urban | −0.01 (−0.11, 0.09) | 0.14 (−0.08, 0.36) | 0.10 (0.06, 0.14) | 0.47 (0.33, 0.61) | |
| Interaction | Upper × Urban | −0.10 (−0.22, 0.02) | −0.21 (−0.95, 0.53) | −0.16 (-0.28, -0.04) | −0.27 (−0.56, 0.02) |
| Total cholesterol (mg/dL) | |||||
| Education | Lower secondary and below | Ref | Ref | Ref | Ref |
| Upper secondary and above | 1.52 (−2.11, 5.15) | 2.90 (−12.45, 18.25) | −0.80 (−4.19, 2.59) | 8.37 (2.33, 14.41) | |
| Residence | Rural | Ref | Ref | Ref | Ref |
| Urban | −3.63 (−7.41, 0.15) | 1.36 (−3.05, 5.77) | 1.22 (−0.35, 2.79) | 2.06 (−1.45, 5.57) | |
| Interaction | Upper × Urban | 2.42 (−1.70, 6.54) | −3.17 (−19.69, 13.35) | 1.07 (−3.30, 5.44) | −9.47 (-17.43, -1.51) |
Footnote: All models were adjusted for age, gender, residence, education, and parental education. All models except those using BMI as the outcome were also adjusted for height.
Regression models that included the interaction term between absolute education attainment and urbanicity of residence further showed how urbanicity of residence might modify the relationship between education and each cardiometabolic biomarker (Table 2 Models B). In the US and Mexico, the interaction terms were not statistically significant, suggesting no evidence of differential educational effects on the cardiometabolic biomarkers based on urbanicity of residence. However, in China and India, statistically significant interaction terms were observed. Specifically, in China, higher education was associated with smaller reductions in BMI, SBP, and HbA1c among urban residents compared to rural ones, with interaction term estimates of −0.57 kg/m2 (95% CI: −0.98, −0.16) for BMI, −2.77 mmHg (95%CI: −5.00, −0.54) for SBP, and −0.16% (95% CI: −0.28, −0.04) for HbA1c. In India, the interaction term estimates were −0.90 kg/m2 (95% CI: −1.12, −0.68) for BMI, −2.78 mmHg (95% CI: −3.72, −1.84) for SBP, and −9.47 mg/dL (95% CI: −17.43, −1.51) for total cholesterol.
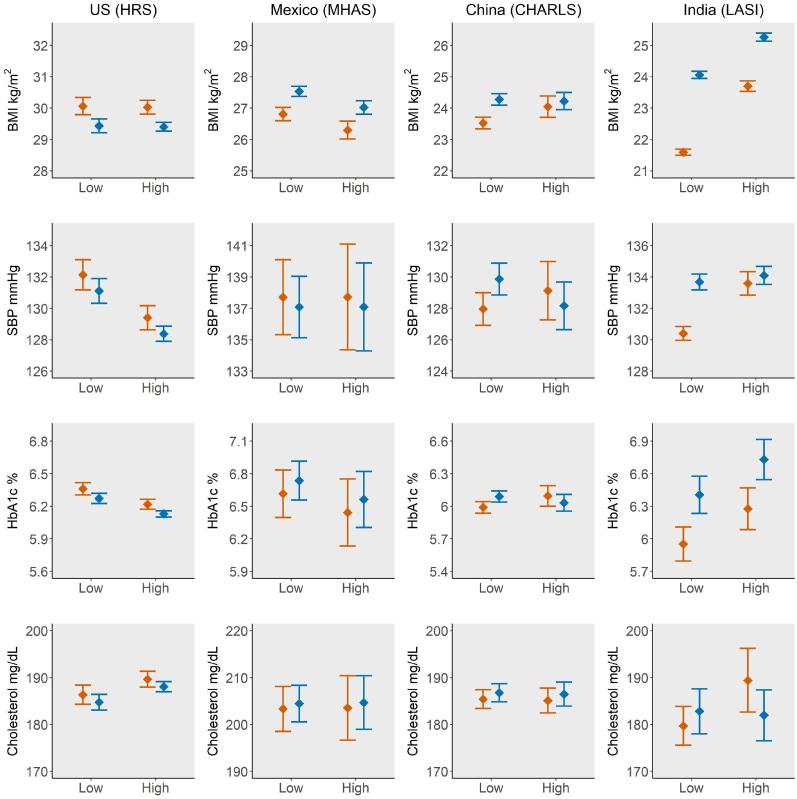
Fig. 2 shows the estimated mean and 95% CI for cardiometabolic biomarkers by absolute education attainment (higher vs. lower education) and urbanicity of residence across countries. In the US and Mexico, higher education was generally associated with lower levels of cardiometabolic biomarkers, regardless of urbanicity of residence. In contrast, in China and India, higher education was generally associated with higher levels of cardiometabolic biomarkers, and educational differences of these biomarkers were less pronounced among urban residents. In addition, the figure shows that rural residents in the US have higher levels of cardiometabolic biomarkers when compared to their urban counterparts, a trend that is reversed in Mexico, China, and India.
Fig. 2.
Estimated mean and 95% CI of cardiometabolic biomarkers by education and urbanicity of residence across countries.
Footnote: 1. Low: lower secondary education and below; High: upper secondary education and above.
2. Orange: rural residents; Blue: urban residents.
3. Estimated marginal means of cardiometabolic biomarkers were generated based on results of Models A and B in Table 2. When no interaction between education and urbanicity of residence was observed, results of Models A were used. Otherwise, results of Models B were used.
3.2. Associations of relative education attainment with cardiometabolic biomarkers
Results from regression models using relative education attainment, without and with the interaction term between education and urbanicity, are generally consistent with those based on absolute education attainment (Table 3). However, two major discrepancies are apparent when comparing these results to those based on absolute education attainment. First, regression models without the interaction term showed that in the US, each 10-percentile higher level of education was associated with lower BMI (−0.08 kg/m2, 95% CI: −0.11, −0.05), while in China, each 10-percentile higher level of education was associated with higher BMI (0.04 kg/m2, 95% CI: 0.02, 0.06). Second, in regression models with an interaction term between education and urbanicity, an interaction was found for BMI in Mexico (−0.23 kg/m2, 95% CI: −0.39, −0.07), but not for SBP in China (−0.20 mmHg, 95% CI: −0.44, 0.03). Importantly, the directions of these effect estimates were consistent between relative and absolute education attainment.
Table 3.
Regression analysis of the association between relative education attainment and cardiometabolic biomarkers.
| US (HRS 2016/17) | Mexico (MHAS 2015) | China (CHARLS 2015/16) | India (LASI 2017/19) | ||
|---|---|---|---|---|---|
| Estimate (95% CI) | Estimate (95% CI) | Estimate (95% CI) | Estimate (95% CI) | ||
| Models A. No interaction term between education and residence added | |||||
| BMI (kg/m2) | |||||
| Education | Increase by 10 percentiles | −0.08 (-0.11, -0.05) | −0.04 (-0.07, -0.01) | 0.04 (0.02, 0.06) | 0.25 (0.24, 0.27) |
| SBP (mmHg) | |||||
| Education | Increase by 10 percentiles | −0.48 (-0.59, -0.37) | −0.11 (−0.47, 0.24) | −0.04 (−0.17, 0.04) | 0.28 (0.22, 0.33) |
| HbA1c (%) | |||||
| Education | Increase by 10 percentiles | −0.03 (-0.04, -0.02) | −0.02 (−0.06, 0.01) | 0.00 (0.00, 0.01) | 0.04 (0.02, 0.06) |
| Total cholesterol (mg/dL) | |||||
| Education | Increase by 10 percentiles | 0.47 (0.23, 0.70) | 0.24 (−0.47, 0.96) | 0.20 (−0.06, 0.45) | 1.11 (0.62, 1.59) |
| Models B. Interaction term between education and residence added | |||||
| BMI (kg/m2) | |||||
| Education | Increase by 10 percentiles | −0.08 (-0.14, -0.02) | 0.15 (0.08, 0.22) | 0.06 (0.03, 0.09) | 0.27 (0.25, 0.28) |
| Residence | Rural | Ref | Ref | Ref | Ref |
| Urban | −0.58 (-0.91, -0.26) | 1.26 (1.00, 1.52) | 0.87 (0.65, 1.09) | 2.22 (2.09, 2.34) | |
| Interaction | Increase × Urban | 0.00 (−0.07, 0.07) | −0.23 (-0.39, -0.07) | −0.05 (-0.09, -0.01) | −0.04 (-0.06, -0.02) |
| SBP (mmHg) | |||||
| Education | Increase by 10 percentiles | −0.53 (-0.75, -0.31) | −0.14 (−0.88, 0.61) | 0.04 (−0.12, 0.20) | 0.35 (0.29, 0.42) |
| Residence | Rural | Ref | Ref | Ref | Ref |
| Urban | −1.09 (−2.21, 0.04) | −0.53 (−3.44, 2.37) | 2.47 (1.26, 3.68) | 3.35 (2.78, 3.91) | |
| Interaction | Increase × Urban | 0.06 (−0.18, 0.31) | 0.03 (−0.79, 0.84) | −0.20 (−0.44, 0.03) | −0.21 (-0.31, -0.11) |
| HbA1c (%) | |||||
| Education | Increase by 10 percentiles | −0.02 (-0.03, -0.01) | −0.02 (−0.09, 0.05) | 0.01 (0.00, 0.02) | 0.05 (0.02, 0.07) |
| Residence | Rural | Ref | Ref | Ref | Ref |
| Urban | −0.05 (−0.11, 0.02) | 0.14 (−0.12, 0.40) | 0.14 (0.08, 0.20) | 0.46 (0.28, 0.65) | |
| Interaction | Increase × Urban | −0.01 (−0.02, 0.01) | 0.00 (−0.07, 0.07) | −0.02 (-0.03, 0.00) | −0.01 (−0.04, 0.02) |
| Total cholesterol (mg/dL) | |||||
| Education | Increase by 10 percentiles | 0.02 (−0.46, 0.50) | 0.81 (−0.68, 2.31) | 0.26 (−0.04, 0.57) | 1.51 (0.91, 2.10) |
| Residence | Rural | Ref | Ref | Ref | Ref |
| Urban | −3.71 (-6.14, -1.28) | 2.46 (−3.31, 8.23) | 1.88 (−0.44, 4.21) | 3.93 (−0.90, 8.77) | |
| Interaction | Increase × Urban | 0.57 (−0.01, 1.14) | −0.71 (−2.34, 0.93) | −0.15 (−0.60, 0.29) | −1.01 (-1.89, -0.12) |
Footnote: The effect estimates for education should be interpreted as every 10 percentiles increase in education attainment. All models were adjusted for age, gender, residence, education, and parental education. All models except those using BMI as the outcome were also adjusted for height.
3.3. Sensitivity analyses
Results from four sets of sensitivity analyses are presented in this section. First, the findings from regression models using HDL and LDL as separate outcomes are shown in Supplementary Table 7. Results of regression models without interaction term between absolute education attainment and urbanicity of residence show that in the US, higher education was associated with higher levels of both HDL and LDL; in China, higher education was associated with a lower level of HDL; in Mexico and India, no associations were observed. Results of regression models with interaction term showed that urbanicity modified the relationship between education and LDL in India. However, no such interaction was observed in the US, Mexico, and China.
Second, the association estimates based on the non-imputed data closely matched those based on the imputed data set (Supplementary Fig. 2). Third, no three-way interaction of education, urbanicity of residence, and gender was statistically significant for most biomarkers, except for BMI in China and India (Supplementary Table 8). Therefore, gender-specific patterns in the relationship between education, urbanicity of residence, and BMI in China and India are shown in Supplementary Fig. 3. Fourth, in pooled analyses, likelihood ratio tests comparing two nested models with and without the three-way interaction term involving education, urbanicity, and country showed that the interaction term was statistically significant for most cardiometabolic biomarkers except for HbA1c. Detailed results on how education and urbanicity are related to cardiometabolic biomarkers are summarized in Supplementary Table 9.
4. Discussion
In this large cross-national study, we had two main findings about the relationship between education and cardiometabolic biomarkers. First, the association between education and specific cardiometabolic biomarkers is not uniform, the direction and magnitude of which varies across countries. This heterogeneity could be driven by country-level differences in social and economic contexts. Second, urbanicity of residence modifies the associations between education and cardiometabolic biomarkers in China and India, but not in the US or Mexico. These varying patterns show that how education relates to cardiometabolic health extends beyond biology and is shaped by social and economic environments. Therefore, the mechanisms linking education to these interrelated biomarkers may differ across countries, reflecting the evolving meaning of education and the socioeconomic contexts and epidemiologic landscapes of these countries.
This study is unique in its use of high-quality harmonized population survey data from the US, Mexico, China, and India to examine educational differences in multiple cardiometabolic biomarkers. The substantial differences in economic development and epidemiologic transition stages across these four populous countries are evidenced by the observed variations in educational achievement and BMI (Barro & Lee, 2013; Omran, 1971). In our study, the proportion of participants with upper secondary education or higher in the USA (82.6%) was significantly higher than those of Mexico (15.6%), China (10.6%), and India (16.8%). In addition, rural-urban differences in education attainment were much higher in Mexico, China, and India than in the US. Therefore, rural residence may be less of a barrier to education resources in the US than in the other three countries, indicating access to education is less meritorious than in the US. (Ulubaşoğlu and Cardak, 2007) The notably high BMI among middle-aged and older adults in the US and Mexico underscores the health risks associated with obesity (DiBonaventura et al., 2018; Dinsa et al., 2012; Trivedi et al., 2015).
Within each country, our findings on the relationship between education and cardiometabolic biomarkers show major variations. Each biomarker had a unique association with education based on either absolute education attainment (binary education: higher vs. lower education) or relative education attainment (percentile rank education). For example, in the US, while binary education was not associated with BMI, it had a negative association with SBP and HbA1c, and a positive association with total cholesterol. These varying associations suggest that the mechanisms linking education to these biomarkers are multifaceted, despite the interrelations of these biomarkers (Kim et al., 2018). It is noteworthy that findings based on the absolute education attainment for BMI in the US suggest no association between education and BMI. While this is in contrast to some other studies in the US(An, 2015; Crane et al., 2023; Sobal & Stunkard, 1989), a negative association was observed when relative education attainment was used. An analogous inconsistency in the relationship between education and BMI was also observed in China using absolute and relative education attainment. The use of absolute education in our study allows for comparisons of education levels and their relationships with cardiometabolic biomarkers across countries (Hummer & Hernandez, 2013). However, this measure can also obscure associations by reducing education attainment to only two levels. By using both absolute and relative education measures, we can capture different dimensions of education attainment and its relationship with health, thereby providing a more nuanced understanding of how education may relate to health outcomes across diverse country contexts (Montez & Zajacova, 2013).
The positive association between education and total cholesterol in the US is not intuitive, in contrast to other biomarkers. One possible explanation is that individuals with higher education might have dietary patterns that include more cholesterol-rich foods, possibly due to higher income (Wilcox et al., 2020). Additionally, although they may lead healthier lifestyles in some respects, these behaviors might not effectively manage cholesterol levels. It is also important to consider the distinction between 'good' (HDL) and 'bad' (LDL) cholesterol (Millán et al., 2009; Virani et al., 2023). In our sensitivity analyses of HDL and LDL, we observed that higher education was associated with increased levels of both types in the US. These associations between education and cardiometabolic biomarkers vary in each of the other three countries as well. Therefore, measuring cardiometabolic risk as a composite score might overlook the specific details of each biomarker (Kamel et al., 2018).
Across countries, the relationship between education and all four cardiometabolic biomarkers displays differences in both direction and magnitude. This indicates that education's implications and effects on cardiometabolic health can vary significantly by country (Schultz et al., 2018). This difference is particularly notable when comparing findings in the US with those in India, where many observed associations are in opposing directions. In high-income countries (HIC) including the US, individuals with higher education often possess better health awareness, behaviors, and healthcare access, typically leading to improved cardiometabolic health (Cutler & Lleras-Muney, 2010; Jehn, 2022). However, in low- and middle-income countries (LMIC), while those with higher education may possess increased health awareness and knowledge, they are also more likely to adopt a Westernized lifestyle (Dinsa et al., 2012). This lifestyle is characterized by reduced physical activity and a diet rich in high-energy, processed foods, which might explain the prevalence of adverse cardiometabolic conditions among more educated individuals in these countries. Additionally, early-life undernutrition or exposure to environmental shocks in many LMICs will further complicate these relationships (Ke et al., 2022; Li et al., 2019, 2024a; Li and Lumey, 2019b, 2022). The findings from all four countries generally align with results from other studies examining the ‘reversal hypothesis’ and highlight the importance of considering each country's level of economic development and stage of epidemiologic transition (Jaacks et al., 2019; Kirschbaum et al., 2022; Pampel et al., 2012).
We noted rural-urban differences in cardiometabolic biomarkers across the four countries. The nature of these disparities varied, especially when comparing the US to the other three countries. In the US, urban residents had lower levels of cardiometabolic biomarkers than rural residents. This observation might be explained by the fact that urban residents in the US generally have more access to social and health services, superior educational resources, and better employment opportunities compared to their rural counterparts, all of which can promote cardiometabolic health (Cross et al., 2020; Groenewegen et al., 2020; MacKinnon et al., 2023). In contrast, urban residents in Mexico, China, and India had higher levels of cardiometabolic biomarkers than their rural counterparts. This finding is consistent with prior evidence indicating that urban populations in these countries were more likely to adopt a Westernized lifestyle compared to their rural counterparts (Dinsa et al., 2012; Gong et al., 2012). Collectively, these findings suggest that rural-urban disparities might lessen or even reverse as nations develop and navigate their epidemiologic transitions (Goldstein, 1990; Moore et al., 2003).
Urbanicity of residence can further modify the relationship between education and cardiometabolic biomarkers depending on the country. In the US and Mexico, we observed no interactions between education and urbanicity of residence. In China and India, we found that educational differences among urban residents were generally smaller than those among rural residents. These findings highlight that urbanicity of residence may also serve as an indicator for levels of economic development and stages of epidemiologic transition within a country, especially in LMICs. This observation is reinforced by the pronounced rural-urban disparities evident in India compared to the other countries, reminiscent of trends reported in studies from China during the 1990s and 2000s when it was less economically developed (Gu et al., 2005; Hou, 2008).
The three-way interaction of education, urbanicity of residence, and gender that was observed for BMI in China and India shows the importance of taking gender into consideration. This may be explained by the differential impacts of education and urbanicity of residence on BMI comparing women to men. Additionally, pooled analyses across countries showed that the three-way interaction term involving education, urbanicity of residence, and country was statistically significant for most cardiometabolic biomarkers, except for HbA1c. These findings suggest that the relationship between education and cardiometabolic health is not uniform across urban and rural settings, and that this relationship varies by country. Future research should further explore these interactions to better understand the pathways through which education and urbanicity relate to cardiometabolic outcomes in diverse populations.
There are multiple strengths of our study. We included high-quality survey data from countries at different levels of economic development and stages of epidemiological transition. This enabled us to examine how the relationship between education and cardiometabolic health may differ across countries. Moreover, the surveys used in our study adopted harmonized designs and questionnaires and encompassed a range of comparable cardiometabolic biomarkers, which enabled cross-national comparisons. This strength is especially pertinent as many prior studies depended on self-reported statuses of cardiometabolic diseases, which can vary based on the country and residence type. We also used both absolute and relative measures of education attainment to capture the complexities of education attainment and their relationships with health outcomes across different national contexts. Another strength is these surveys had a large sample size of middle-aged and older adults from both rural and urban areas, which made it possible to examine the relationships between education and cardiometabolic health across and within countries.
However, our study also has several limitations. First, the cross-sectional design, with data gathered between 2015 and 2019 across the four countries, does not allow causal inferences. As more survey waves are under collection or planned for each of these four studies, we will have an opportunity to examine changes in cardiometabolic biomarkers over time according to education levels and potential mechanisms. Second, although we harmonized education across countries based on the 2011 International Standard Classification of Education (ISCED), equivalent education attainments might hold different implications and significances across nations, and education quality can also vary across and within countries. However, we also created relative education attainment in each country and observed similar findings based on this variable, suggesting that our findings were robust. Third, we adopted each country's classification of rural or urban residency. This approach allowed us to use contextually specific definitions of urbanicity that were relevant in each country, but it may lead to inconsistencies in the definition of urbanicity. Fourth, the cardiometabolic biomarkers that were available, their collection methodologies, and the accuracy and consistency of measurement devices varied across countries. However, measurement variation does not systematically bias country-specific estimates, which was the main objective of this study. Last, we observed differential missingness in biomarkers, education, and urbanicity of residence across countries, which could affect the representativeness of our analytical samples from these countries and introduce bias. Future research should take this limitation into account and explore methods to mitigate its potential impact on sample representativeness and cross-national comparisons.
In conclusion, we found that the association of education and cardiometabolic biomarkers varies across middle-aged and older populations in the US, Mexico, India, and China, aligning with each country's current economic development and stage of epidemiological transition. Our interaction analyses of education and urbanicity of residence showed that educational differences in cardiometabolic biomarkers are similar among rural and urban residents in the US and Mexico. However, in contrast, these educational differences are less pronounced among urban residents compared to rural residents. These findings underscore the importance of considering both inter-country and intra-country contextual factors in developing initiatives and policies aimed at improving cardiometabolic health, particularly in the context of the rising global burden of poor cardiometabolic health.
CRediT authorship contribution statement
Chihua Li: Writing – review & editing, Writing – original draft, Visualization, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Yuan Zhang: Writing – review & editing, Writing – original draft, Supervision, Methodology, Funding acquisition, Formal analysis, Data curation, Conceptualization. Grace Noppert: Writing – review & editing, Writing – original draft, Supervision, Funding acquisition, Conceptualization. Adina Zeki Al Hazzouri: Writing – review & editing, Methodology, Investigation, Conceptualization. Alden Gross: Writing – review & editing, Writing – original draft, Supervision, Methodology, Funding acquisition, Formal analysis, Data curation, Conceptualization. Lindsay Kobayashi: Writing – review & editing, Writing – original draft, Supervision, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Conceptualization.
Ethics approval and consent to participate
All participants gave written informed consent before participation. We were exempted from ethical approval for the secondary data analysis.
Data availability
The Gateway to Global Aging Data website provides documentation and code for the harmonized datasets used here, with links to the parent cohort data: https://g2aging.org/downloads. The HRS and HRS-HCAP data are available at: https://hrs.isr.umich.edu/data-products. The MHAS and MexCog data are available at: https://www.mhasweb.org/DataProducts/Home.aspx. The CHARLS data are available at: https://charls.charlsdata.com/pages/data/111/en.html. The LASI data are available at: https://iipsindia.ac.in/content/LASI-data. The LASI-DAD data are available at: https://lasi-dad.org/access-data. The LASI and LASI-DAD data are also available at: https://g2aging.org/downloads.
Funding
Chihua Li was supported by the National Institute on Aging (NIA) R01AG070953 and R01AG075719. Yuan Zhang was supported by NIA R00AG070274. Grace Noppert was supported by NIA R00AG062749 and R01AG075719. Adina Zeki Al Hazzouri was supported by R01AG072681. Alden Groos and Lindsay Kobayashi were supported by NIA R01AG070953.
Declaration of competing interest
None declared.
Acknowledgements
We thank the participants and enumerators of the Health and Retirement Study, Mexican Health and Aging Study, China Health and Retirement Longitudinal Study, and Longitudinal Aging Study in India. We thank the Gateway to Global Aging Data Team for preparing the harmonized data. During the preparation of this work, the author Chihua Li used ChatGPT-3.5 to check grammar and revise some sentences, which aimed to improve readability and language. After using this tool, the author reviewed and edited the content as needed and takes full responsibility for the content of the publication.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2024.101716.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Data availability
The data is publicly avaliable but the authors are not allowed to share them. The data can be applied from each cohort used in this manuscript.
References
- 2018 revision of world urbanization prospects. United Nations; 2018. [Google Scholar]
- Addey T., Alegre-Díaz J., Bragg F., et al. Educational and social inequalities and cause-specific mortality in Mexico City: a prospective study. The Lancet Public Health. 2023;8(9):e670–e679. doi: 10.1016/S2468-2667(23)00153-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen L., Williams J., Townsend N., et al. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: A systematic review. The Lancet Global Health. 2017;5(3):e277–e289. doi: 10.1016/S2214-109X(17)30058-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amato M.C., Guarnotta V., Giordano C. Body composition assessment for the definition of cardiometabolic risk. Journal of Endocrinological Investigation. 2013;36(7):537–543. doi: 10.3275/8943. [DOI] [PubMed] [Google Scholar]
- An R. Educational disparity in obesity among U.S. adults, 1984-2013. Annals of Epidemiology. 2015;25(9):637–642.e5. doi: 10.1016/j.annepidem.2015.06.004. [DOI] [PubMed] [Google Scholar]
- Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- Avila J.C., Samper-Ternent R., Wong R. Malnutrition risk among older Mexican adults in the Mexican health and aging study. Nutrients. 2021;13(5) doi: 10.3390/nu13051615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avila-Funes J.A., Gutiérrez-Robledo L.M., Ponce De Leon Rosales S. Validity of height and weight self-report in Mexican adults: Results from the national health and aging study. The Journal of Nutrition, Health & Aging. 2004;8(5):355–361. [PubMed] [Google Scholar]
- Barro R.J., Lee J.W. A new data set of educational attainment in the world, 1950–2010. Journal of Development Economics. 2013;104:184–198. [Google Scholar]
- Barua S. Spatial inequality and explaining the urban-rural gap in obesity in India: Evidence from 2015-16 population-based survey. PLoS One. 2023;18(1) doi: 10.1371/journal.pone.0279840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bi Y., Jiang Y., He J., et al. Status of cardiovascular health in Chinese adults. Journal of the American College of Cardiology. 2015;65(10):1013–1025. doi: 10.1016/j.jacc.2014.12.044. [DOI] [PubMed] [Google Scholar]
- Blue L., Kranker K., Markovitz A.R., et al. Effects of the million hearts model on myocardial infarctions, strokes, and medicare spending: A randomized clinical trial. JAMA. 2023;330(15):1437–1447. doi: 10.1001/jama.2023.19597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castelli W.P., Anderson K., Wilson P.W., Levy D. Lipids and risk of coronary heart disease. The Framingham Study. Annals of Epidemiology. 1992;2(1–2):23–28. doi: 10.1016/1047-2797(92)90033-m. [DOI] [PubMed] [Google Scholar]
- Chang K.C., Soljak M., Lee J.T., et al. Coverage of a national cardiovascular risk assessment and management programme (NHS Health Check): Retrospective database study. Preventive Medicine. 2015;78:1–8. doi: 10.1016/j.ypmed.2015.05.022. [DOI] [PubMed] [Google Scholar]
- Chen X., Crimmins E., Hu P.P., et al. Venous blood-based biomarkers in the China health and retirement longitudinal study: Rationale, design, and results from the 2015 wave. American Journal of Epidemiology. 2019;188(11):1871–1877. doi: 10.1093/aje/kwz170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho T.C., Yu X., Gross A.L., et al. Negative wealth shocks in later life and subsequent cognitive function in older adults in China, england, Mexico, and the USA, 2012-18: A population-based, cross-nationally harmonised, longitudinal study. The Lancet Healthy Longevity. 2023;4(9):e461–e469. doi: 10.1016/S2666-7568(23)00113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark A.M., DesMeules M., Luo W., Duncan A.S., Wielgosz A. Socioeconomic status and cardiovascular disease: Risks and implications for care. Nature Reviews Cardiology. 2009;6(11):712–722. doi: 10.1038/nrcardio.2009.163. [DOI] [PubMed] [Google Scholar]
- Corsi D.J., Subramanian S.V. Socioeconomic gradients and distribution of diabetes, hypertension, and obesity in India. JAMA Network Open. 2019;2(4) doi: 10.1001/jamanetworkopen.2019.0411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Country and lending groups. World Bank; 2023. [Google Scholar]
- Crane B.M., Nichols E., Carlson M.C., Deal J.A., Gross A.L. Body mass index and cognition: Associations across mid- to late life and gender differences. The Journals of Gerontology: Series A. 2023;78(6):988–996. doi: 10.1093/gerona/glad015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins E., Faul J., Kim J.K., et al. Survey Research Center University of Michigan; Ann Arbor, MI: 2013. Documentation of biomarkers in the 2006 and 2008 health and retirement study. [Google Scholar]
- Cross S.H., Mehra M.R., Bhatt D.L., et al. Rural-urban differences in cardiovascular mortality in the US, 1999-2017. JAMA. 2020;323(18):1852–1854. doi: 10.1001/jama.2020.2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler D.M., Lleras-Muney A. Understanding differences in health behaviors by education. Journal of Health Economics. 2010;29(1):1–28. doi: 10.1016/j.jhealeco.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiBonaventura M.D., Meincke H., Le Lay A., Fournier J., Bakker E., Ehrenreich A. Obesity in Mexico: Prevalence, comorbidities, associations with patient outcomes, and treatment experiences. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. 2018;11:1–10. doi: 10.2147/DMSO.S129247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinsa G.D., Goryakin Y., Fumagalli E., Suhrcke M. Obesity and socioeconomic status in developing countries: A systematic review. Obesity Reviews. 2012;13(11):1067–1079. doi: 10.1111/j.1467-789X.2012.01017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dudina A., Cooney M.T., Bacquer D.D., et al. Relationships between body mass index, cardiovascular mortality, and risk factors: A report from the SCORE investigators. European Journal of Cardiovascular Prevention & Rehabilitation. 2011;18(5):731–742. doi: 10.1177/1741826711412039. [DOI] [PubMed] [Google Scholar]
- Ettehad D., Emdin C.A., Kiran A., et al. Blood pressure lowering for prevention of cardiovascular disease and death: A systematic review and meta-analysis. Lancet. 2016;387(10022):957–967. doi: 10.1016/S0140-6736(15)01225-8. [DOI] [PubMed] [Google Scholar]
- Franklin S.S., Larson M.G., Khan S.A., et al. Does the relation of blood pressure to coronary heart disease risk change with aging? The framingham heart study. Circulation. 2001;103(9):1245–1249. doi: 10.1161/01.cir.103.9.1245. [DOI] [PubMed] [Google Scholar]
- Frieden T.R., Berwick D.M. The "Million Hearts" initiative--preventing heart attacks and strokes. New England Journal of Medicine. 2011;365(13):e27. doi: 10.1056/NEJMp1110421. [DOI] [PubMed] [Google Scholar]
- Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: A systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goel A., Gross A. Differential item functioning in the cognitive screener used in the Longitudinal Aging Study in India. International Psychogeriatrics. 2019;31(9):1331–1341. doi: 10.1017/S1041610218001746. [DOI] [PubMed] [Google Scholar]
- Goldstein G. Urbanization, health and well-being: A global perspective. Journal of the Royal Statistical Society. Series D. 1990;39(2):121–133. [Google Scholar]
- Gong P., Liang S., Carlton E.J., et al. Urbanisation and health in China. Lancet. 2012;379(9818):843–852. doi: 10.1016/S0140-6736(11)61878-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goryakin Y., Suhrcke M. Economic development, urbanization, technological change and overweight: What do we learn from 244 demographic and health surveys? Economics and Human Biology. 2014;14:109–127. doi: 10.1016/j.ehb.2013.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groenewegen P.P., Bosmans M.W.G., Boerma W.G.W., Spreeuwenberg P. The primary care workforce in Europe: A cross-sectional international comparison of rural and urban areas and changes between 1993 and 2011. The European Journal of Public Health. 2020;30(Suppl_4):iv12–i17. doi: 10.1093/eurpub/ckaa125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross A.L., Li C., Briceño E.M., et al. Harmonisation of later-life cognitive function across national contexts: Results from the harmonized cognitive assessment protocols. The Lancet Healthy Longevity. 2023;4(10):e573–e583. doi: 10.1016/S2666-7568(23)00170-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu D., Reynolds K., Wu X., et al. Prevalence of the metabolic syndrome and overweight among adults in China. Lancet. 2005;365(9468):1398–1405. doi: 10.1016/S0140-6736(05)66375-1. [DOI] [PubMed] [Google Scholar]
- Hill-Briggs F., Adler N.E., Berkowitz S.A., et al. Social determinants of health and diabetes: A scientific review. Diabetes Care. 2020;44(1):258–279. doi: 10.2337/dci20-0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou X. Urban-rural disparity of overweight, hypertension, undiagnosed hypertension, and untreated hypertension in China. Asia-Pacific Journal of Public Health. 2008;20(2):159–169. doi: 10.1177/1010539507312306. [DOI] [PubMed] [Google Scholar]
- Hu P., Wang S., Lee J. Socioeconomic gradients of cardiovascular risk factors in China and India: Results from the China health and retirement longitudinal study and longitudinal aging study in India. The Internet Journal of Public Health. 2017;62(7):763–773. doi: 10.1007/s00038-017-0968-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummer R.A., Hernandez E.M. The effect of educational attainment on adult mortality in the United States. Population Bulletin. 2013;68(1):1–16. [PMC free article] [PubMed] [Google Scholar]
- Informática INdEGe. Tabulados básicos población. http://www.inegi.gob.mx/est/librerias/tabulados.asp?tabulado (accessed 11/16/2023).
- International standard classification of education ISCED 2011. The United Nations Educational, Scientific and Cultural Organization (UNESCO); 2012. [Google Scholar]
- Jaacks L.M., Vandevijvere S., Pan A., et al. The obesity transition: Stages of the global epidemic. Lancet Diabetes & Endocrinology. 2019;7(3):231–240. doi: 10.1016/S2213-8587(19)30026-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jehn A. The relationship between postsecondary education and adult health behaviors. SSM Popul Health. 2022;17 doi: 10.1016/j.ssmph.2021.100992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang F., Hou X., Lu J., et al. Assessment of the performance of A1CNow(+) and development of an error grid analysis graph for comparative hemoglobin A1c measurements. Diabetes Technology & Therapeutics. 2014;16(6):363–369. doi: 10.1089/dia.2013.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamel M., Smith B.T., Wahi G., Carsley S., Birken C.S., Anderson L.N. Continuous cardiometabolic risk score definitions in early childhood: A scoping review. Obesity Reviews. 2018;19(12):1688–1699. doi: 10.1111/obr.12748. [DOI] [PubMed] [Google Scholar]
- Ke C., Narayan K.M.V., Chan J.C.N., Jha P., Shah B.R. Pathophysiology, phenotypes and management of type 2 diabetes mellitus in Indian and Chinese populations. Nature Reviews Endocrinology. 2022;18(7):413–432. doi: 10.1038/s41574-022-00669-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J.K., Faul J., Weir D.R., Crimmins E.M. Dried blood spot based biomarkers in the health and retirement study: 2006 to 2016. American Journal of Human Biology. 2023 doi: 10.1002/ajhb.23997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim M.K., Han K., Park Y.M., et al. Associations of variability in blood pressure, glucose and cholesterol concentrations, and body mass index with mortality and cardiovascular outcomes in the general population. Circulation. 2018;138(23):2627–2637. doi: 10.1161/CIRCULATIONAHA.118.034978. [DOI] [PubMed] [Google Scholar]
- Kirschbaum T.K., Sudharsanan N., Manne-Goehler J., et al. The association of socioeconomic status with hypertension in 76 low- and middle-income countries. Journal of the American College of Cardiology. 2022;80(8):804–817. doi: 10.1016/j.jacc.2022.05.044. [DOI] [PubMed] [Google Scholar]
- Kodali N.K., Bhat L.D., Phillip N.E., Koya S.F. Prevalence and associated factors of cardiovascular diseases among men and women aged 45 years and above: Analysis of the longitudinal ageing study in India, 2017-2019. Indian Heart Journal. 2023;75(1):31–35. doi: 10.1016/j.ihj.2022.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubota Y., Heiss G., MacLehose R.F., Roetker N.S., Folsom A.R. Association of educational attainment with lifetime risk of cardiovascular disease: The atherosclerosis risk in communities study. JAMA Internal Medicine. 2017;177(8):1165–1172. doi: 10.1001/jamainternmed.2017.1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López-Olmedo N., Popkin B.M., Taillie L.S. The socioeconomic disparities in intakes and purchases of less-healthy foods and beverages have changed over time in urban Mexico. The Journal of Nutrition. 2018;148(1):109–116. doi: 10.1093/jn/nxx007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamb K.E., Crawford D., Thornton L.E., Shariful Islam S.M., Maddison R., Ball K. Educational differences in diabetes and diabetes self-management behaviours in WHO SAGE countries. BMC Public Health. 2021;21(1):2108. doi: 10.1186/s12889-021-12131-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara-Castor L., Micha R., Cudhea F., et al. Sugar-sweetened beverage intakes among adults between 1990 and 2018 in 185 countries. Nature Communications. 2023;14(1):5957. doi: 10.1038/s41467-023-41269-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J., Banerjee J., Khobragade P.Y., Angrisani M., Dey A.B. LASI-DAD study: A protocol for a prospective cohort study of late-life cognition and dementia in India. BMJ Open. 2019;9(7) doi: 10.1136/bmjopen-2019-030300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J., Khobragade P.Y., Banerjee J., et al. Design and methodology of the longitudinal aging study in India-diagnostic assessment of dementia (LASI-DAD) Journal of the American Geriatrics Society. 2020;68(3):S5–s10. doi: 10.1111/jgs.16737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J., Wilkens J., Meijer E., Sekher T.V., Bloom D.E., Hu P. Hypertension awareness, treatment, and control and their association with healthcare access in the middle-aged and older Indian population: A nationwide cohort study. PLoS Medicine. 2022;19(1) doi: 10.1371/journal.pmed.1003855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leng B., Jin Y., Li G., Chen L., Jin N. Socioeconomic status and hypertension: A meta-analysis. Journal of Hypertension. 2015;33(2):221–229. doi: 10.1097/HJH.0000000000000428. [DOI] [PubMed] [Google Scholar]
- Li C., Liu C., Ye C., Lian Z., Lu P. Education, gender, and frequent pain among middle-aged and older adults in the United States, England, China, and India. Pain. 2024 doi: 10.1097/j.pain.0000000000003349. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- Li C., Lumey L.H. Exposure to the Chinese famine of 1959-61 in early life and long-term health conditions: A systematic review and meta-analysis. International Journal of Epidemiology. 2017;46(4):1157–1170. doi: 10.1093/ije/dyx013. [DOI] [PubMed] [Google Scholar]
- Li C., Lumey L.H. Impact of disease screening on awareness and management of hypertension and diabetes between 2011 and 2015: Results from the China health and retirement longitudinal study. BMC Public Health. 2019;19(1):421. doi: 10.1186/s12889-019-6753-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C., Lumey L.H. Interaction or mediation by adult obesity of the relation between fetal famine exposure and type 2 diabetes? International Journal of Epidemiology. 2019;48(2):654–656. doi: 10.1093/ije/dyy293. [DOI] [PubMed] [Google Scholar]
- Li C., Lumey L.H. Early-life exposure to the Chinese famine of 1959-1961 and type 2 diabetes in adulthood: A systematic review and meta-analysis. Nutrients. 2022;14(14) doi: 10.3390/nu14142855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C., Ó Gráda C., Lumey L.H. Famine mortality and contributions to later-life type 2 diabetes at the population level: A synthesis of findings from Ukrainian, Dutch and Chinese famines. BMJ Global Health. 2024;9(8) doi: 10.1136/bmjgh-2024-015355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C., Tobi E.W., Heijmans B.T., Lumey L.H. The effect of the Chinese Famine on type 2 diabetes mellitus epidemics. Nature Reviews Endocrinology. 2019;15(6):313–314. doi: 10.1038/s41574-019-0195-5. [DOI] [PubMed] [Google Scholar]
- Li C., Young B.R., Jian W. Association of socioeconomic status with financial burden of disease among elderly patients with cardiovascular disease: Evidence from the China health and retirement longitudinal survey. BMJ Open. 2018;8(3) doi: 10.1136/bmjopen-2017-018703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losada-Rojas L.L., Ke Y., Pyrialakou V.D., Konstantina G. Access to healthy food in urban and rural areas: An empirical analysis. Journal of Transport & Health. 2021;23 [Google Scholar]
- MacKinnon N.J., Emery V., Waller J., et al. Mapping health disparities in 11 high-income nations. JAMA Network Open. 2023;6(7) doi: 10.1001/jamanetworkopen.2023.22310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maria J.L., Anand T.N., Dona B., Prinu J., Prabhakaran D., Jeemon P. Task-sharing interventions for improving control of diabetes in low-income and middle-income countries: A systematic review and meta-analysis. The Lancet Global Health. 2021;9(2):e170–e180. doi: 10.1016/S2214-109X(20)30449-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathur M.R., Nagrath D., Malhotra J., Mishra V.K. Determinants of sugar-sweetened beverage consumption among Indian adults: Findings from the national family health survey-4. Indian Journal of Community Medicine. 2020;45(1):60–65. doi: 10.4103/ijcm.IJCM_201_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullough M.L., Chantaprasopsuk S., Islami F., et al. Association of socioeconomic and geographic factors with diet quality in US adults. JAMA Network Open. 2022;5(6) doi: 10.1001/jamanetworkopen.2022.16406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millán J., Pintó X., Muñoz A., et al. Lipoprotein ratios: Physiological significance and clinical usefulness in cardiovascular prevention. Vascular Health and Risk Management. 2009;5:757–765. [PMC free article] [PubMed] [Google Scholar]
- Mills K.T., Stefanescu A., He J. The global epidemiology of hypertension. Nature Reviews Nephrology. 2020;16(4):223–237. doi: 10.1038/s41581-019-0244-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda J.J., Barrientos-Gutiérrez T., Corvalan C., et al. Understanding the rise of cardiometabolic diseases in low- and middle-income countries. Nature Medicine. 2019;25(11):1667–1679. doi: 10.1038/s41591-019-0644-7. [DOI] [PubMed] [Google Scholar]
- Montez J.K., Zajacova A. Explaining the widening education gap in mortality among U.S. white women. Journal of Health and Social Behavior. 2013;54(2):166–182. doi: 10.1177/0022146513481230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore M., Gould P., Keary B.S. Global urbanization and impact on health. International Journal of Hygiene and Environmental Health. 2003;206(4–5):269–278. doi: 10.1078/1438-4639-00223. [DOI] [PubMed] [Google Scholar]
- Mourad J.J. The evolution of systolic blood pressure as a strong predictor of cardiovascular risk and the effectiveness of fixed-dose ARB/CCB combinations in lowering levels of this preferential target. Vascular Health and Risk Management. 2008;4(6):1315–1325. doi: 10.2147/vhrm.s4073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nations within a nation Variations in epidemiological transition across the states of India, 1990-2016 in the Global Burden of Disease Study. Lancet. 2017;390(10111):2437–2460. doi: 10.1016/S0140-6736(17)32804-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navarro-Meza M., Moreno A.G.M., López-Espinoza A., López-Uriarte P., Gómez M.R.B. Comparison in food intake of adults residing in a rural and urban area of Jalisco, Mexico. Revista Mexicana de Trastornos Alimentarios. 2014;5(1):11–19. [Google Scholar]
- Neuman M., Kawachi I., Gortmaker S., Subramanian S.V. Urban-rural differences in BMI in low- and middle-income countries: The role of socioeconomic status. The American Journal of Clinical Nutrition. 2013;97(2):428–436. doi: 10.3945/ajcn.112.045997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Hearn M., Lauren B.N., Wong J.B., Kim D.D., Mozaffarian D. Trends and disparities in cardiometabolic health among U.S. Adults, 1999-2018. Journal of the American College of Cardiology. 2022;80(2):138–151. doi: 10.1016/j.jacc.2022.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obesity Preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:1–253. [PubMed] [Google Scholar]
- Omran A.R. The epidemiologic transition. A theory of the epidemiology of population change. Milbank Memorial Fund Quarterly. 1971;49(4):509–538. [PubMed] [Google Scholar]
- Omran A.R. A century of epidemiologic transition in the United States. Preventive Medicine. 1977;6(1):30–51. doi: 10.1016/0091-7435(77)90003-2. [DOI] [PubMed] [Google Scholar]
- Pampel F.C., Denney J.T., Krueger P.M. Obesity, SES, and economic development: A test of the reversal hypothesis. Social Science & Medicine. 2012;74(7):1073–1081. doi: 10.1016/j.socscimed.2011.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perianayagam A., Bloom D., Lee J., et al. Cohort profile: The longitudinal ageing study in India (LASI) International Journal of Epidemiology. 2022;51(4):e167–e176. doi: 10.1093/ije/dyab266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins J.M., Subramanian S.V., Davey Smith G., Özaltin E. Adult height, nutrition, and population health. Nutrition Reviews. 2016;74(3):149–165. doi: 10.1093/nutrit/nuv105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters S.A., Singhateh Y., Mackay D., Huxley R.R., Woodward M. Total cholesterol as a risk factor for coronary heart disease and stroke in women compared with men: A systematic review and meta-analysis. Atherosclerosis. 2016;248:123–131. doi: 10.1016/j.atherosclerosis.2016.03.016. [DOI] [PubMed] [Google Scholar]
- Pongiglione B., Ploubidis G.B., Dowd J.B. Older adults in the United States have worse cardiometabolic health compared to england. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2022;77(Suppl_2):S167–s176. doi: 10.1093/geronb/gbac023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin B., Zhang Y. Note on urbanization in China: Urban definitions and census data. China Economic Review. 2014;30:495–502. [Google Scholar]
- Rosengren A., Smyth A., Rangarajan S., et al. Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: The prospective urban rural epidemiologic (PURE) study. The Lancet Global Health. 2019;7(6):e748–e760. doi: 10.1016/S2214-109X(19)30045-2. [DOI] [PubMed] [Google Scholar]
- Roth G.A., Mensah G.A., Johnson C.O., et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: Update from the GBD 2019 study. Journal of the American College of Cardiology. 2020;76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruan Y., Guo Y., Zheng Y., et al. Cardiovascular disease (CVD) and associated risk factors among older adults in six low-and middle-income countries: Results from SAGE wave 1. BMC Public Health. 2018;18(1):778. doi: 10.1186/s12889-018-5653-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks E., Morrow M., Story W.T., et al. Beyond the building blocks: Integrating community roles into health systems frameworks to achieve health for all. BMJ Global Health. 2018;3(Suppl 3) doi: 10.1136/bmjgh-2018-001384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarwar N., Gao P., Seshasai S.R., et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: A collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375(9733):2215–2222. doi: 10.1016/S0140-6736(10)60484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sattar N., Gill J.M.R., Alazawi W. Improving prevention strategies for cardiometabolic disease. Nature Medicine. 2020;26(3):320–325. doi: 10.1038/s41591-020-0786-7. [DOI] [PubMed] [Google Scholar]
- Schultz W.M., Kelli H.M., Lisko J.C., et al. Socioeconomic status and cardiovascular outcomes: Challenges and interventions. Circulation. 2018;137(20):2166–2178. doi: 10.1161/CIRCULATIONAHA.117.029652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Service UER. Rural-Urban Continuum Codes. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/(accessed 11/16/2023).
- Sharkey J.R., Johnson C.M., Dean W.R. Less-healthy eating behaviors have a greater association with a high level of sugar-sweetened beverage consumption among rural adults than among urban adults. Food & Nutrition Research. 2011;55 doi: 10.3402/fnr.v55i0.5819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobal J., Stunkard A.J. Socioeconomic status and obesity: A review of the literature. Psychological Bulletin. 1989;105(2):260–275. doi: 10.1037/0033-2909.105.2.260. [DOI] [PubMed] [Google Scholar]
- Sonnega A., Faul J.D., Ofstedal M.B., Langa K.M., Phillips J.W., Weir D.R. Cohort profile: The health and retirement study (HRS) International Journal of Epidemiology. 2014;43(2):576–585. doi: 10.1093/ije/dyu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens G., Dias R.H., Thomas K.J., et al. Characterizing the epidemiological transition in Mexico: National and subnational burden of diseases, injuries, and risk factors. PLoS Medicine. 2008;5(6):e125. doi: 10.1371/journal.pmed.0050125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian S.V., Corsi D.J., Subramanyam M.A., Smith G.D. Jumping the gun: The problematic discourse on socioeconomic status and cardiovascular health in India. International Journal of Epidemiology. 2013;42(5):1410–1426. doi: 10.1093/ije/dyt017. [DOI] [PubMed] [Google Scholar]
- Third Report of the National Cholesterol Education Program (NCEP) Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation. 2002;106(25):3143–3421. [PubMed] [Google Scholar]
- Trivedi T., Liu J., Probst J., Merchant A., Jhones S., Martin A.B. Obesity and obesity-related behaviors among rural and urban adults in the USA. Rural and Remote Health. 2015;15(4):3267. [PubMed] [Google Scholar]
- Ulubaşoğlu M.A., Cardak B.A. International comparisons of rural–urban educational attainment: Data and determinants. European Economic Review. 2007;51(7):1828–1857. [Google Scholar]
- Valenzuela P.L., Carrera-Bastos P., Castillo-García A., Lieberman D.E., Santos-Lozano A., Lucia A. Obesity and the risk of cardiometabolic diseases. Nature Reviews Cardiology. 2023;20(7):475–494. doi: 10.1038/s41569-023-00847-5. [DOI] [PubMed] [Google Scholar]
- Varghese J.S., Lu P., Choi D., et al. Spousal concordance of hypertension among middle-aged and older heterosexual couples around the world: Evidence from studies of aging in the United States, england, China, and India. Journal of American Heart Association. 2023;12(24) doi: 10.1161/JAHA.123.030765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virani S.S., Aspry K., Dixon D.L., et al. The importance of low-density lipoprotein cholesterol measurement and control as performance measures: A joint clinical perspective from the national lipid association and the American society for preventive cardiology. Journal of Clinical. 2023;13 doi: 10.1016/j.ajpc.2023.100472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westbury S., Ghosh I., Jones H.M., et al. The influence of the urban food environment on diet, nutrition and health outcomes in low-income and middle-income countries: A systematic review. BMJ Global Health. 2021;6(10) doi: 10.1136/bmjgh-2021-006358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whelton P.K., Carey R.M., Aronow W.S., et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American college of cardiology/American heart association task force on clinical practice guidelines. Journal of the American College of Cardiology. 2017;71(19):e127–e248. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- WHO Guidelines Approved by the Guidelines Review Committee . World Health Organization; Geneva: 2011. Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus: Abbreviated report of a WHO consultation. [PubMed] [Google Scholar]
- Wilcox S., Sharpe P.A., Liese A.D., Dunn C.G., Hutto B. Socioeconomic factors associated with diet quality and meeting dietary guidelines in disadvantaged neighborhoods in the Southeast United States. Ethnicity and Health. 2020;25(8):1115–1131. doi: 10.1080/13557858.2018.1493434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams J., Allen L., Wickramasinghe K., Mikkelsen B., Roberts N., Townsend N. A systematic review of associations between non-communicable diseases and socioeconomic status within low- and lower-middle-income countries. Journal of Global Health. 2018;8(2) doi: 10.7189/jogh.08.020409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong R., Michaels-Obregón A., Palloni A., et al. Progression of aging in Mexico: The Mexican health and aging study (MHAS) 2012. Salud Publica de Mexico. 2015;57(0 1):S79–S89. doi: 10.21149/spm.v57s1.7593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong R., Michaels-Obregon A., Palloni A. Cohort profile: The Mexican health and aging study (MHAS) International Journal of Epidemiology. 2017;46(2):e2. doi: 10.1093/ije/dyu263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank open data. World Bank; 2023. [Google Scholar]
- Xu C., Zhang P., Cao Z. Cardiovascular health and healthy longevity in people with and without cardiometabolic disease: A prospective cohort study. EClinicalMedicine. 2022;45 doi: 10.1016/j.eclinm.2022.101329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang G., Wang Y., Zeng Y., et al. Rapid health transition in China, 1990-2010: Findings from the global burden of disease study 2010. Lancet. 2013;381(9882):1987–2015. doi: 10.1016/S0140-6736(13)61097-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaman M.J., Patel A., Jan S., et al. Socio-economic distribution of cardiovascular risk factors and knowledge in rural India. International Journal of Epidemiology. 2012;41(5):1302–1314. doi: 10.1093/ije/dyr226. [DOI] [PubMed] [Google Scholar]
- Zhang N. Urban–rural disparities in cardiovascular disease risks among middle-aged and older Chinese: Two decades of urbanisation. Ageing and Society. 2020;40(7):1405–1427. [Google Scholar]
- Zhao Y., Hu Y., Smith J.P., Strauss J., Yang G. Cohort profile: The China health and retirement longitudinal study (CHARLS) International Journal of Epidemiology. 2014;43(1):61–68. doi: 10.1093/ije/dys203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmer Z., Kwong J. Socioeconomic status and health among older adults in rural and urban China. Journal of Aging and Health. 2004;16(1):44–70. doi: 10.1177/0898264303260440. [DOI] [PubMed] [Google Scholar]
- Zou Y., Zhang R., Zhou B., et al. A comparison study on the prevalence of obesity and its associated factors among city, township and rural area adults in China. BMJ Open. 2015;5(7) doi: 10.1136/bmjopen-2015-008417. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The Gateway to Global Aging Data website provides documentation and code for the harmonized datasets used here, with links to the parent cohort data: https://g2aging.org/downloads. The HRS and HRS-HCAP data are available at: https://hrs.isr.umich.edu/data-products. The MHAS and MexCog data are available at: https://www.mhasweb.org/DataProducts/Home.aspx. The CHARLS data are available at: https://charls.charlsdata.com/pages/data/111/en.html. The LASI data are available at: https://iipsindia.ac.in/content/LASI-data. The LASI-DAD data are available at: https://lasi-dad.org/access-data. The LASI and LASI-DAD data are also available at: https://g2aging.org/downloads.
The data is publicly avaliable but the authors are not allowed to share them. The data can be applied from each cohort used in this manuscript.