Extract
The World Health Organization (WHO) hosted an expert committee on chronic cor pulmonale in Geneva, Switzerland, from 10 to 15 October 1960. In the introduction of the report [1], the authors underscored that the attention of the Director General of the WHO had been drawn to the fact that, while the lung diseases causing pulmonary heart disease (corresponding to the exact translation of the term cor pulmonale in original Latin) had been studied in detail, there was little reliable information concerning the incidence of important secondary effects on the pulmonary circulation and right ventricle. Importantly, the authors made it clear that the term “chronic” indicated that the report intended to exclude secondary effects on the right heart arising in the course of a few days or weeks from acute pulmonary disorders [1]. The objectives of this report were to define chronic cor pulmonale, to provide a tentative classification of diseases which might cause the syndrome, to describe its pathophysiology and to establish criteria for diagnosis [1].
Shareable abstract
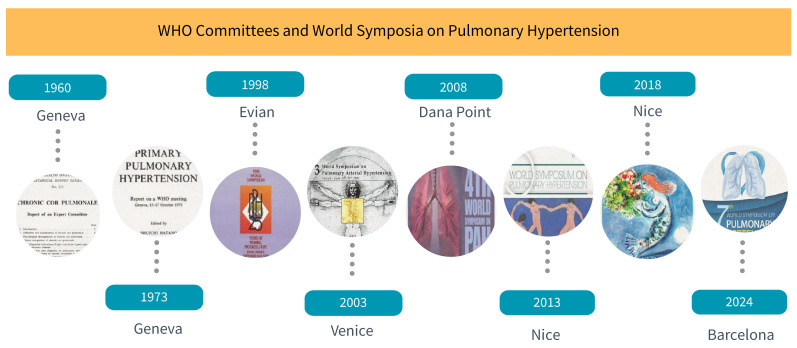
Since 1960, pulmonary hypertension has been the focus of WHO committee reports and World Symposia proceedings. The conclusions from the 7th World Symposium on Pulmonary Hypertension are now published in the European Respiratory Journal. https://bit.ly/4ePMZ6H
Cor pulmonale: WHO, Geneva, Switzerland (October 1960)
The World Health Organization (WHO) hosted an expert committee on chronic cor pulmonale in Geneva, Switzerland, from 10 to 15 October 1960. In the introduction of the report [1], the authors underscored that the attention of the Director General of the WHO had been drawn to the fact that, while the lung diseases causing pulmonary heart disease (corresponding to the exact translation of the term cor pulmonale in original Latin) had been studied in detail, there was little reliable information concerning the incidence of important secondary effects on the pulmonary circulation and right ventricle. Importantly, the authors made it clear that the term “chronic” indicated that the report intended to exclude secondary effects on the right heart arising in the course of a few days or weeks from acute pulmonary disorders [1]. The objectives of this report were to define chronic cor pulmonale, to provide a tentative classification of diseases which might cause the syndrome, to describe its pathophysiology and to establish criteria for diagnosis [1].
This WHO expert committee report represents the basis of the modern age of our field and contains key statements. First, the authors clearly stated that three broad groups of diseases would lead to excess load on the right ventricle: diseases primarily affecting the ventilatory and respiratory function of the lungs, diseases that act directly on the pulmonary vessels, and primary cardiac diseases. Of note, the authors indicated that the vascular changes in the lungs and in the clinical presentation of some cases of mitral stenosis or congenital heart disease with left-to-right shunting were similar to diseases directly affecting the pulmonary vessels. However, the committee decided to exclude primary cardiac diseases to conform with contemporary cardiological practice. After discussion, it was decided to give an anatomical definition corresponding to hypertrophy of the right ventricle resulting from diseases affecting the function and/or structure of the lung, except when these pulmonary alterations are the results of left heart or congenital heart disease. A first attempt to classify the causes was proposed. At that time, physiological derangements in chronic cor pulmonale were described in detail, with an emphasis on disturbances in the respiratory circulation on one hand and alterations in the haemodynamics of the pulmonary circulation on the other, including chronic thromboembolic pulmonary disease and the debated concept of primary pulmonary hypertension caused by primary lesion of the pulmonary arterial wall.
It is fascinating to read the meticulous description of the clinical and diagnostic approach to the condition. The upper limits of normal values of haemodynamic measures were described with a reference point 10 cm above the level of the back in supine position. The authors stated at that time that pulmonary hypertension is usually considered to be present when the mean pressure in the pulmonary artery exceeds 25 mmHg at rest, but that in many instances of pulmonary heart disease this value will not be exceeded at rest. Therapy was in its infancy, with an emphasis on prevention and treatment of the underlying pulmonary diseases and the resulting cardiac failure.
The report contained suggestions for future research and recommendations: training of investigators with multidisciplinary backgrounds, hosting regular meetings to further discuss advances in the field, disseminating information, supporting postgraduate education and using WHO as a platform for coordinating research, and promoting and disseminating refinements in the definition and classification of disease [1].
Primary pulmonary hypertension: WHO, Geneva, Switzerland (October 1973)
In the following decade an intense interest was given to pulmonary hypertension, due to a sudden increase in the number of patients diagnosed in Switzerland, Germany and Austria in the context of the intake of an anorexic agent, aminorex fumarate. The lungs of patients with anorexigen-associated pulmonary hypertension showed a morphological picture identical with that seen in so-called primary pulmonary hypertension without an underlying known cause. It was emphasised that this condition was a rare disease recognised in a small number of patients worldwide. The outbreak of cases associated with the intake of anorexic agents generated interest in primary pulmonary hypertension, and the WHO convened another meeting in Geneva, Switzerland, from 15 to 17 October 1973, in order to review its causes and mechanisms [2]. On this occasion, the committee decided to exclude the most common forms of pulmonary hypertension secondary to chronic pulmonary and heart disease, and the report started with a statement that the cause of some cases of pulmonary hypertension was “unknown”.
Interestingly, the term primary pulmonary hypertension was a source of debate and the authors clarified that it was used in the report to describe pulmonary hypertension of unknown cause. The report sequentially addressed the control of the pulmonary circulation, the morphology of primary pulmonary hypertension, its pathogenesis, the pharmacology of the pulmonary circulation, the clinical attributes of primary pulmonary hypertension and its epidemiology and natural history. At that time, it was proposed that the empirical upper limits of normal mean pulmonary artery pressure were 25 mmHg with a borderline range of 15–25 mmHg. In the annex, it is reminded that the normal mean pulmonary artery pressure never exceeds 20 mmHg, but that hypertension is definitely present if the pressure exceeds 25 mmHg [2]. Although patients with primary pulmonary hypertension presented with much higher values, the authors insisted that the pulmonary artery pressure of such patients may have been a great deal closer to the normal range during the early stages of the disease. The need to develop noninvasive diagnostic techniques to perform serial measurements and identify early disease or follow relatives in familial forms was underscored. A key consequence of the report was the launch of a National Institute of Health Registry in the 1980s [3].
World Symposium on Primary Pulmonary Hypertension: co-sponsored by WHO, Evian, France (September 1998)
The next quarter of a century witnessed progress in the field of chronic pulmonary vascular disease, with better understanding of risk factors and associated conditions, localisation of the main disease-causing gene on chromosome 2q31–32, better tools for noninvasive early diagnosis and screening led by echocardiography with Doppler and other imaging techniques (computed tomography of the chest and magnetic resonance imaging), simplified exercise testing (6-min walk test), and identification of a subgroup of patients showing acute and long-term response to vasodilator agents [4]. An updated diagnostic classification introduced the term pulmonary arterial hypertension, which could be associated or not with other conditions (sporadic or familial primary pulmonary hypertension, and pulmonary arterial hypertension related to connective tissue disorders, congenital systemic to pulmonary shunts, portal hypertension, HIV infection, and drugs and toxins). The most common causes of pulmonary hypertension associated with heart, lung or thromboembolic pulmonary disease were kept in discrete groups. The idea was that the different groups gathered patients with broadly similar mechanisms and management. Calcium channel blockers and prostacyclins were proposed for the treatment of primary pulmonary hypertension and pulmonary arterial hypertension. These agents were primarily vasodilators and future research on antiproliferative agents was proposed. Surgical and interventional techniques were in rapid development, such as atrial septostomy and lung and heart–lung transplantation.
The Third World Symposium on Pulmonary Arterial Hypertension: Venice, Italy (June 2003)
In the following 5 years, the volume and speed of discoveries in the field warranted a “third” World Symposium (assuming that the first two were held in 1973 and 1998, this symposium was held in Venice, Italy, on 23–25 June 2003. The clinical classification was refined and a better understanding of the cellular and molecular drivers of pulmonary arterial hypertension benefited from significant technological advances [5]. Not long before the conference, heterozygous mutations in the bone morphogenetic protein receptor type II gene (BMPR2) were identified as the leading causes of familial or heritable pulmonary arterial hypertension. While the transforming growth factor beta superfamily was demonstrated as a major player in pulmonary vascular homeostasis, other important studies clearly identified treatable pathways and supported the development of several medications with properties targeting the dysfunctional endothelin, nitric oxide and prostacyclin pathways. This resulted in the publication of an evidence-based treatment algorithm, with levels of evidence to guide treating clinicians on the best practice options for patients with pulmonary arterial hypertension [5]. Interventional and surgical modalities were proposed for the treatment of pulmonary arterial hypertension (atrial septostomy and lung and heart–lung transplantation) and chronic thromboembolic pulmonary hypertension (pulmonary endarterectomy).
The Fourth World Symposium on Pulmonary Arterial Hypertension: Dana Point, USA (February 2008)
The next World Symposium was organised for the first time in the USA (Dana Point, CA; 11–14 February 2008). The purpose of the symposium was to review the progresses made in diagnosing and treating pulmonary hypertension, describe the rationale for ongoing research and formulate proposals for new investigative paths that may translate into a better future for patients [6]. Novel genetic causes of pulmonary arterial hypertension were discovered beyond BMPR2, but many pointed to the key role of the transforming growth factor beta superfamily in the pathobiology of the disease. Modalities for diagnosing the disease and predicting outcomes were analysed in great detail, with an emphasis on haemodynamic and echocardiographic measures, as well as biomarkers led by brain natriuretic protein. An updated treatment algorithm reflected the best evidence available for the appropriate treatment of patients. Sequential combination therapies were proposed for patients with pulmonary arterial hypertension. The benefits and drawbacks of a variety of clinical trial end-points and designs were proposed to determine the most interpretable and clinically relevant randomised controlled trials [6].
The Fifth World Symposium on Pulmonary Hypertension: Nice, France (February 2013)
The Fifth World Symposium was organised in Nice, France from 27 February to 1 March 2013 [7]. The ongoing clinical and translational research of our community led to more discoveries and the proactive support to setting ambitious risk assessment and treatment goals of pulmonary hypertension. This allowed the emergence of novel treatment strategies such as initial combination therapy in pulmonary arterial hypertension and balloon pulmonary angioplasty in inoperable chronic thromboembolic pulmonary hypertension [7].
The Sixth World Symposium on Pulmonary Hypertension: Nice, France (February 2018)
The Sixth World Symposium was organised in Nice, France from 27 February to 1 March 2018 [8, 9]. A dedicated session on patients’ perspectives emphasised the importance of patients’ empowerment and partnership with researchers, clinicians and healthcare providers. The impressive developments in the understanding of the pathology, pathobiology, genetics and genomics of pulmonary hypertension further highlighted emerging pathways which could be the target of novel therapeutic interventions. Careful analysis of large databases resulted in precisely defining the upper limit of normal pulmonary artery pressure as 20 mmHg. This led to the end of the empirical and erroneous value of 25 mmHg to define pulmonary hypertension, and an updated definition of pulmonary hypertension was proposed. This approach was a first step to considering a revision of cut-off values for all haemodynamic parameters, including pulmonary vascular resistance and pulmonary artery wedge pressure. In terms of therapy, accumulation of novel clinical data firmly established initial and sequential combination therapy in pulmonary arterial hypertension. Moreover, the respective roles of medical therapy, balloon pulmonary angioplasty and pulmonary endarterectomy were then better understood in chronic thromboembolic pulmonary hypertension.
The Seventh World Symposium on Pulmonary Hypertension: endorsed by Alliance for Pulmonary Hypertension, ERN-LUNG, ERS, ISHLT, PHA Europe, PHA Japan, PHA Korea, PHA Latin America, PHA UK, PHA USA, and SPLF, Barcelona, Spain (June 2024)
The COVID-19 pandemic hit us badly in the subsequent few years, widening the interval between the Sixth and the Seventh World Symposia by one year, but it did not slow innovation in our field. The Seventh World Symposium has just been held in Barcelona, Spain, from 29 June to 1 July 2024. It was endorsed by several patients' organisations (Alliance for Pulmonary Hypertension, Pulmonary Hypertension Association (PHA) Europe, PHA Japan, PHA Korea, PHA Latin America, PHA UK, PHA USA), the European Respiratory Society, the International Society for Heart and Lung Transplantation, the Société de Pneumologie de Langue Française and the European Reference Network for Rare Lung Diseases (ERN-LUNG). In recent years, the European Commission has launched ambitious programmes for a higher level of research, education and care in the field of rare diseases that are of such low prevalence (fewer than 1 in 2000 people) that special combined efforts are needed to address them. The ERN-LUNG is patient-centric and the organising committee of the Seventh World Symposium share the same priority. Symbolically, the 2024 Symposium started for the first time with the patients’ perspective, showing the respect and importance given to patients’ priorities. The translational aspects of modern pulmonary vascular research have been highlighted by the development of novel treatment approaches directly targeting the basic drivers of pulmonary vascular remodelling through activin signalling inhibition [10] and the updated evidence-based treatment algorithm benefiting from improved risk stratification tools and ambitious treatment goals. Similarly, refined treatment approaches for chronic thromboembolic pulmonary hypertension highlighted the complementarity of the different treatment modalities targeting different mechanisms of the disease. Transplantation, bridging and support technologies, palliative care, management of pregnant women with pulmonary hypertension, and specificities of paediatric care were discussed extensively. Emerging multimodality imaging techniques and novel technologies enabled a better understanding of right ventricular and pulmonary vascular interactions.
The growing interest in pulmonary hypertension is confirmed by the presence of an increasing number of specialists at the World Symposia. The 1960 and 1973 WHO Committees were attended by 14 and 22 participants, respectively. These numbers rose steadily in the following years, culminating in Barcelona, where 1700 attendees contributed to the open programme (figure 1).
FIGURE 1.
Historical perspective of the World Health Organization (WHO) Committees and World Symposia on Pulmonary Hypertension (1960–2024).
Shareable PDF
Footnotes
Conflict of interest: M. Humbert reports grants from Gossamer and Merck, consultancy fees from 35 Pharma, Aerovate, AOP Orphan, Chiesi, Ferrer, Gossamer, Janssen, Keros, Liquidia, Merck, Novartis, Respira, Roivant and United Therapeutics, payment or honoraria for lectures, presentations, manuscript writing or educational events from Janssen and Merck, and participation on a data safety monitoring board or advisory board with 35 Pharma, Aerovate, Janssen, Keros, Merck, Novartis and United Therapeutics. N. Galiè reports grants from Janssen, Actelion and Merck, consultancy fees and payment or honoraria for lectures, presentations, manuscript writing or educational events from Janssen, Actelion, Chiesi and Ferrer, support for attending meetings from Dompe, and participation on a data safety monitoring board or advisory board with Janssen, Actelion and Ferrer. L.J. Rubin reports consultancy fees from Gossamer and SoniVie, payment for expert testimony from Sandoz, and is a member of the Organizing and Founders Committees, WSPH. G. Simonneau has no potential conflicts of interest to disclose. V.V. McLaughlin reports grants from Aerovate, Gossamer-Bio, Janssen, Keros, Merck and Sonovie, and consultancy fees from 35Pharma, Aerami, Aerovate, Caremark, L.L.C., Corvista, Gossamer Bio, Janssen, Keros, Merck, Riovant and United Therapeutics.
Support statement: M. Humbert is supported by state funding managed by the National Research Agency according to the Investments for the Future programme integrated into France 2030, under the reference ANR-18-RHUS-0006 (DESTINATION 2024).
References
- 1.World Health Organization. Report of the WHO Expert Committee on Chronic Cor Pulmonale. WHO Technical Report Series, Number 213. Geneva, WHO, 1961. [PubMed]
- 2.Hatano S, Strasser T, eds. Primary Pulmonary Hypertension. Report on a WHO Meeting. Geneva, World Health Organization, 1975; pp. 7–45. [Google Scholar]
- 3.Rich S, Dantzer DR, Ayres SM, et al. Primary pulmonary hypertension: a national prospective study. Ann Intern Med 1987; 107: 216–228. doi: 10.7326/0003-4819-107-2-216 [DOI] [PubMed] [Google Scholar]
- 4.Rich S, ed. Executive Summary from the World Symposium – Primary Pulmonary Hypertension. www.wsphassociation.org/wp-content/uploads/2019/04/Primary-Pulmonary-Hypertension-Evian-1998.pdf
- 5.Galiè N, Rubin LJ. Introduction: new insights into a challenging disease; a review of the third World Symposium on Pulmonary Arterial Hypertension. J Am Coll Cardiol 2004; 43: 2S–4S. doi: 10.1016/j.jacc.2004.03.019 [DOI] [PubMed] [Google Scholar]
- 6.Humbert M, McLaughlin VV. The 4th World Symposium on Pulmonary Hypertension. J Am Coll Cardiol 2009; 54: Suppl., S1–S2. doi: 10.1016/j.jacc.2009.04.013 [DOI] [PubMed] [Google Scholar]
- 7.Galiè N, Simonneau G. The fifth World Symposium on Pulmonary Hypertension. J Am Coll Cardiol 2013; 62: Suppl. 25, D1–D3. doi: 10.1016/j.jacc.2013.10.030 [DOI] [PubMed] [Google Scholar]
- 8.Galiè N, McLaughlin VV, Rubin LJ, et al. An overview of the 6th World Symposium on Pulmonary Hypertension. Eur Respir J 2019; 53: 1802148. doi: 10.1183/13993003.02148-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Humbert M, Galiè N, McLaughlin VV, et al. An insider view on the World Symposium on Pulmonary Hypertension. Lancet Respir Med 2019; 7: 484–485. doi: 10.1016/S2213-2600(19)30111-0 [DOI] [PubMed] [Google Scholar]
- 10.Humbert M. Viewpoint: activin signalling inhibitors for the treatment of pulmonary arterial hypertension. Eur Respir J 2023; 62: 2301726. doi: 10.1183/13993003.01726-2023 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This one-page PDF can be shared freely online.
Shareable PDF ERJ-01222-2024.Shareable (283.8KB, pdf)