Abstract
A 64-year-old man presented with severe intermittent claudication for 4 weeks. Computed tomography angiography showed aortoiliac occlusion. Aortoiliac thrombectomy and followed by covered endovascular reconstruction of aortic bifurcation was performed successfully. On-table fenestration technique was used for preservation of inferior mesenteric artery (IMA) to minimize the risk of bowel ischemia. A follow-up computed tomography scan at 6 weeks showed aortoiliac artery and IMA were patent and patient was asymptomatic at 6 months follow-up. Comprehensive management with thrombectomy, covered endovascular reconstruction of the aortic bifurcation, and concurrent on-table fenestration for IMA preservation was an alternative novel, effective, and safe approach for treatment of complex aortoiliac occlusion.
Keywords: Aortoiliac occlusive disease, Covered endovascular reconstruction, Aortic bifurcation, Thrombectomy, On-table fenestration
Aortoiliac occlusive disease (AIOD) may present as intermittent claudication and limb-threatening ischemia. It has been treated traditionally by open surgical aortobifemoral bypass. Open surgery is recommended for Trans-Atlantic Inter-Society Consensus Document (TASC) II C and D lesions because of favorable long-term patency rates.1 However, open bypass surgery for AIOD is associated with a 30-day mortality rate of 3% and a morbidity rate of 15%.2 Currently, minimally invasive endovascular revascularization is accepted widely as the preferred treatment modality in most of patients, including TASC II C and D lesions.3, 4, 5 Endovascular treatment of the extensive occlusive lesions at the aortic bifurcation is one of the most challenging endovascular procedures. Currently, the endovascular techniques commonly used for the reconstruction of aortic bifurcation include kissing stents and covered endovascular reconstruction of the aortic bifurcation (CERAB). The CERAB technique was introduced as a novel method to treat extensive AIOD approximately 10 years ago.6 It is associated with satisfactory long-term outcomes with a reported primary patency rate of 77.5% to 83.3% at the 5-year follow-up.7,8 However, inferior mesenteric artery (IMA) and bilateral internal iliac arteries (IIAs) may have to be sacrificed by the covered stent during CERAB for AIOD. The IMA and bilateral IIAs are the main blood supply vessels to the lower abdomen and pelvis, and IMA collateralization is an important compensatory mechanism when bilateral IIAs are obstructed.
In this study, we report the treatment of a patient with subacute AIOD with coexistent IIA occlusion using a combination of CERAB technique and on-table fenestration for preservation of IMA to minimize the risk of bowel ischemia. This case report was conducted according to the CARE guidelines.9 The patient has given written consent for publication of this paper.
Case report
A 64-year-old gentleman presented to our hospital with severe debilitating intermittent claudication. He had sudden onset of weakness and pain in bilateral lower limb during physical exercise 4 weeks ago. The weakness and pain worsened progressively after walking for 10 m without rest pain or tissue loss. Past medical history was significant for hypertension, mellitus diabetes, and hyperlipidemia, and he was a heavy smoker. His vital signs were normal on admission. Upon physical examination, the bilateral lower limbs were pale and cool to the touch. There was slight sensory loss below the knee bilaterally without impairment to motor function. Bilateral femoral pulses were absent. Blood tests showed that liver and renal function were normal, except for an elevated triglyceride of 2.5 mmol/L (normal reference, <1.7 mmol/L). d-Dimer was 0.22 μg/mL (within the normal range of 0-0.5 μg/mL). Computed tomography (CT) angiography showed that the distal aorta, right common iliac artery and external iliac artery were totally occluded (Fig 1, A). Extensive stenosis was noted from the origin of the left common iliac artery to the distal external iliac artery. The right IIA was obstructed and the origin of left IIA was stenotic. Large collaterals were present from the IMA to the lower abdomen and pelvis, the diameter of IMA was measured 5 mm on a CT scan. The common, superficial, and profunda femoral arteries were patent without significant stenosis. The ankle-branchial index was 0.29 in the left side and undetectable in the right side.
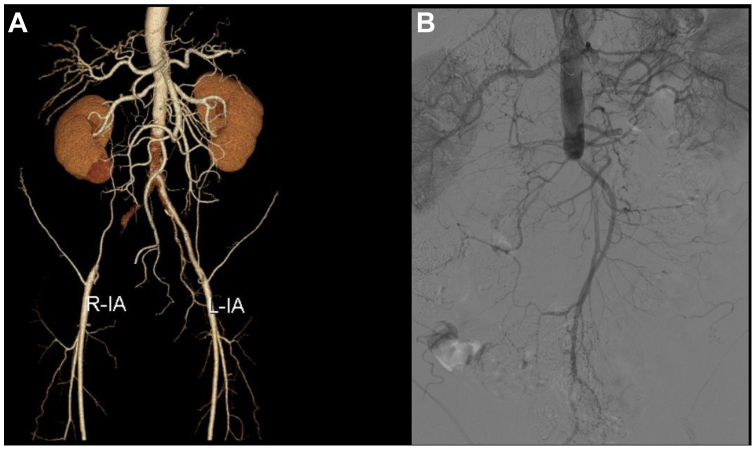
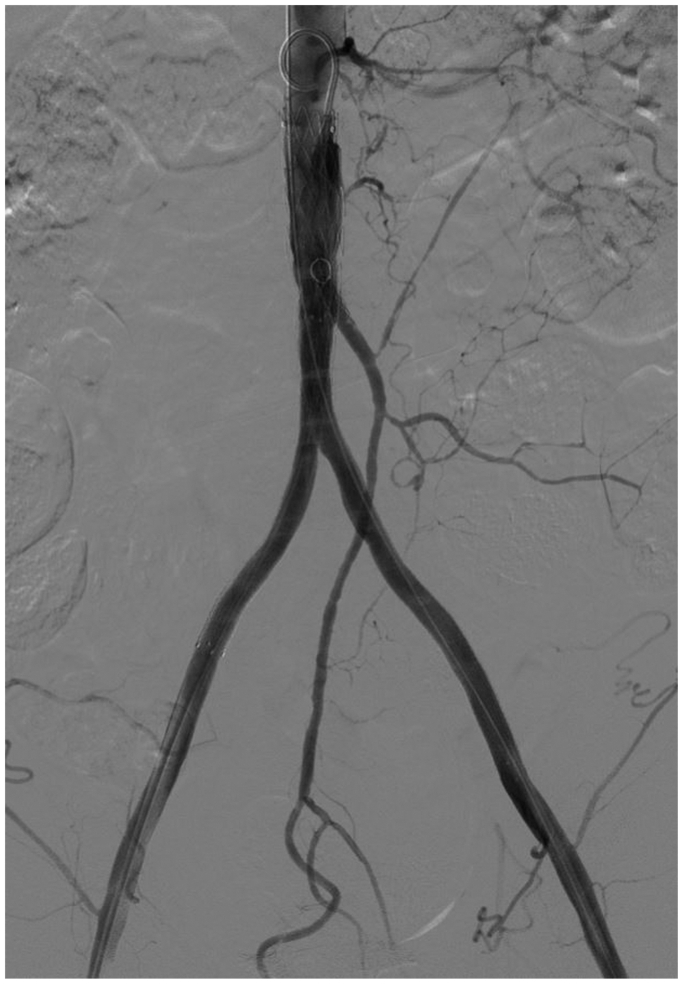
Fig 1.
(A) Computed tomography (CT) angiography showed that the distal aorta, right common iliac artery (CIA) and external iliac artery (EIA) were totally occluded. Extensive stenosis was noted from the origin of left CIA to distal EIA. Right internal iliac artery (IIA) was obstructed and the origin of left IIA was stenotic. Large collaterals were present from inferior mesenteric artery (IMA) to the lower abdomen and pelvis. (B) Angiogram showed aortic occlusion below the IMA which was consistent with the preoperative CT angiography. L-IA, Left iliac artery; R-IA, right iliac artery.
In view of his clinical presentation and aortoiliac occlusion with collaterals from the IMA, the diagnosis was suspected subacute thrombosis on chronic aortoiliac stenosis. Anticoagulation with low-molecular-weight heparin was administrated. A hybrid operation with aortoiliac thrombectomy via bilateral femoral arteries and subsequent angioplasty and placement of covered stent to reconstruct the aortic bifurcation was planned. Owing to occlusion of the right IIA, stenosis of the left IIA origin and aortic partial thrombosis at the level of IMA, there was a risk of bowel ischemia after covered stent placement. To decrease the risk of bowel ischemia, we decided to preserve the IMA using an on-table fenestration technique.
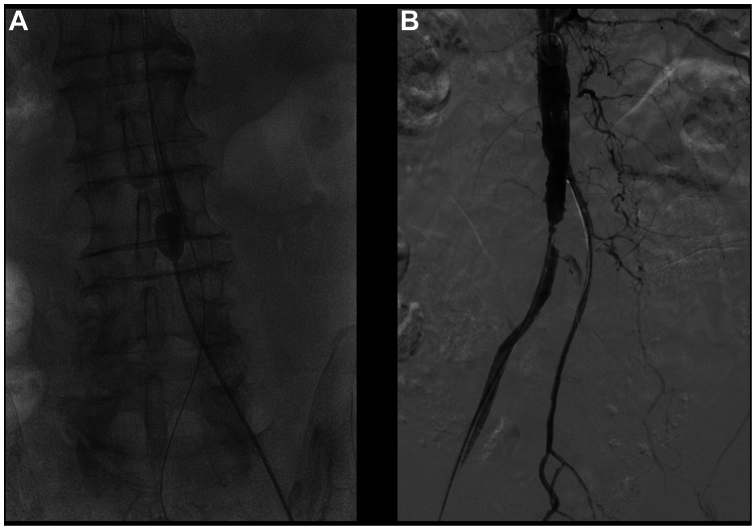
Under general anesthesia, the bilateral femoral arteries were exposed using vertical groin incisions. Left branchial artery was punctured under ultrasound guidance, a 5F sheath (Terumo, Tokyo, Japan) was inserted. A 5F pigtail catheter (Cordis, Hialeah, FL) was advanced over a 0.035″ guidewire (Terumo) and parked at the renal level of the abdominal aorta. Angiogram showed aortic occlusion below the IMA (Fig 1, B) and it was consistent with the preoperative CT angiography. After heparinization, a transverse arteriotomy was made in the anterior wall of right common femoral artery. A 0.035″ guidewire (Terumo) passed through the occlusion in the true lumen with the support of a 5F curved catheter (Cordis) and advanced into the proximal abdominal aorta. A 7F Fogarty double-lumen catheter (Edwards Lifesciences, Irvine, CA) followed, and the balloon at the tip of Fogarty catheter was inflated with contrast and thrombectomy was performed carefully under fluoroscopy (Fig 2, A). Before thrombectomy, a 4 × 40 mm balloon (Zylox, Zhuhai City, China) was selectively advanced into the IMA via the left brachial access. The balloon was inflated during thrombectomy to prevent embolism of the IMA. Thrombus was removed from the distal aorta and the right iliac artery. Using the same method, thrombectomy was also performed using the left femoral access. After thrombectomy, bilateral iliac flow was restored and common femoral arteries were closed with a running suture of 6-0 Prolene (Ethicon, Inc, Raritan, NJ). An angiogram after thrombectomy revealed the previously occluded aortoiliac bifurcation was patent; diffuse stenosis was seen from the distal aorta to the bilateral EIAs. Angioplasty was performed using a 12 × 80 mm balloon (Mustang, Boston Scientific, Marlborough, MA) for the aorta and an 8 × 80 mm balloon (Mustang, Boston Scientific) for the iliac arteries. Despite improvement of stenosis after angioplasty, residual stenosis at the aortoiliac bifurcation was noted (Fig 2, B).
Fig 2.
(A) Thrombectomy was performed using a 7F Fogarty catheter under fluoroscopy. A 4 × 40-mm balloon was selectively advanced into the inferior mesenteric artery (IMA) and this balloon was inflated during thrombectomy to prevent embolism of IMA. (B) Residual stenosis was identified at the aortoiliac bifurcation after thrombectomy and angioplasty.
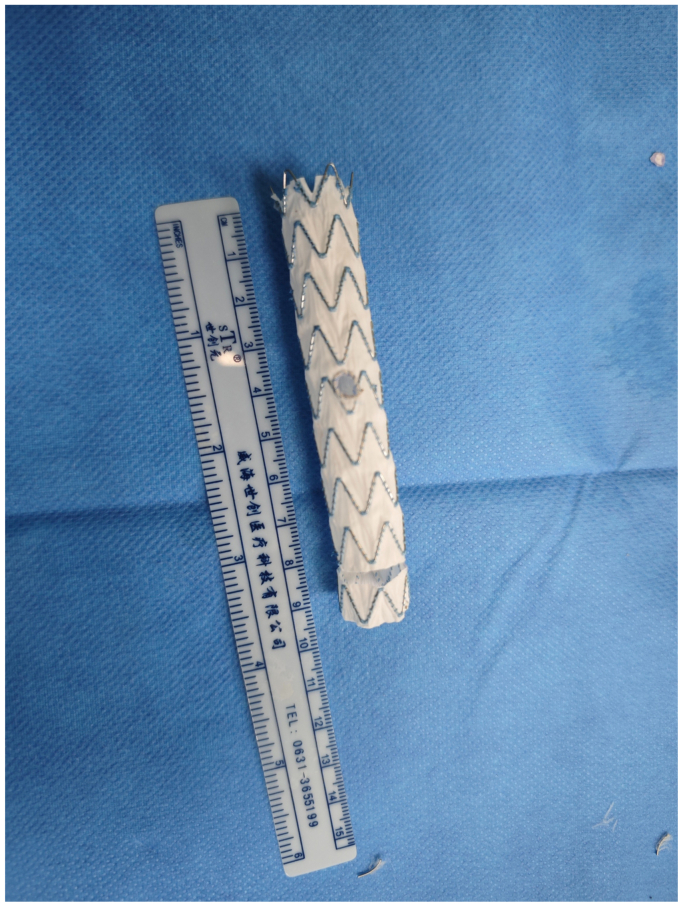
A fenestrated CERAB technique was used to resolve the stenosis. A 5-mm fenestration was made with scalpel on a 16-16-95 mm Endurant iliac extension (Medtronic, Minneapolis, MN). The tip of a 0.018″ guidewire (V18, Boston Scientific) was cut off and sutured around the fenestration using 6-0 Prolene (Ethicon) as a marker (Fig 3). The Endurant iliac limb was partially deployed in vitro, most of the stent graft remained in the sheath. After the IMA fenestration was created, the stent graft was packed using flexible small-bore transparent tubing from a butterfly cannula. During the resheathing process, great care was taken to ensure that the stent graft was not torqued or twisted and that there was a smooth pass at tip of the delivery system. The Endurant stent graft was deployed at infrarenal aorta with the fenestration toward 1 o'clock direction of the origin of IMA. The distal end of the stent graft was located just above the aortoiliac bifurcation. A 0.035″ guideline was selected into the IMA through the fenestration, a 5 × 29 mm balloon expandable covered stent (Viabahn VBX, W. L. Gore & Associates, Flagstaff, AZ) was deployed. Then, kissing covered stents were placed at the aortoiliac bifurcation. An 8 × 100 mm and 8 × 150 mm self-expanding covered stents (Viabahn, W. L. Gore & Associates) were used for right and left iliac artery, respectively. A completion angiogram showed the distal aorta, IMA, and bilateral iliac arteries were patent without any residual stenosis (Fig 4).
Fig 3.
A 5-mm fenestration was made on a 16-16-95 mm Endurant iliac extension during CERAB technique.
Fig 4.
Completion angiogram showed the distal abdominal aorta, inferior mesenteric artery (IMA) and bilateral iliac arteries were patent without any residual stenosis.
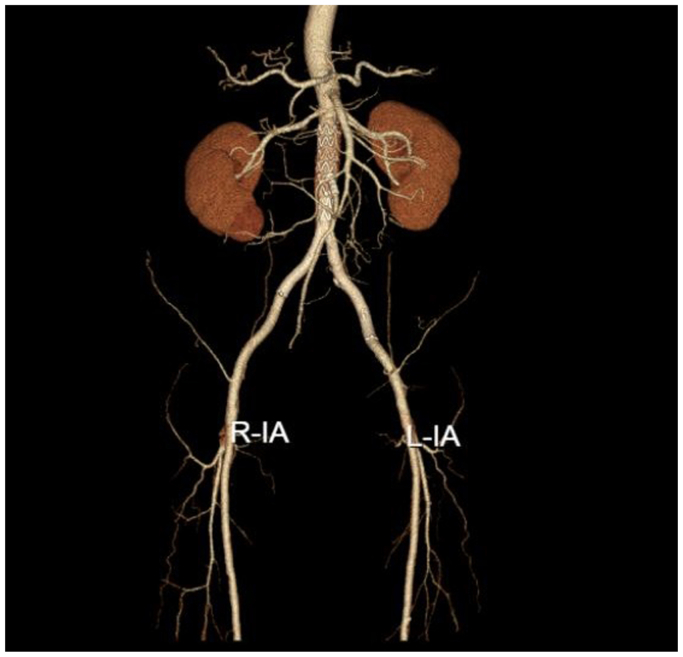
The patient's symptoms were improved after the procedure and he was on anticoagulation using low-molecular-weight heparin. The ankle-branchial index increased from 0 to 0.88 on the right side and from 0.29 to 0.85 in the left side, and both feet were pink and well-perfused. Histology of the removed blood clot was just thrombus. He recovered well and rivaroxaban (Bayer, Leverkusen, Germany) 20 mg once a day was used after discharge. The postoperative follow-up CT angiography at 6 weeks showed the distal abdominal aorta, IMA, and bilateral iliac arteries were all patent (Fig 5). He was asymptomatic at 6 months' follow-up; bilateral femoral and dorsalis pedis arterial pulses were clinically palpable. He remained on antithrombotic therapy with aspirin 100 mg and rivaroxaban 10 mg once a day after 3 months of anticoagulation.
Fig 5.
Follow-up computed tomography (CT) angiography at 6 weeks after operation showed the distal abdominal aorta, inferior mesenteric artery (IMA) and bilateral iliac arteries were patent. L-IA, Left iliac artery; R-IA, right iliac artery.
This study was carried out in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, ethical approval by institutional review board was waived.
Discussion
To the best of our knowledge, this report is the first in the contemporary literature on the use of CERAB technique with on-table fenestration to preserve IMA in the treatment of AIOD. This patient presented with disabling intermittent claudication (Rutherford classification 3, Fontaine stage IIb), and TASC II D infra-IMA aortic occlusion with IMA collateralization was identified on CT angiography. Based on the symptoms and formation of large collaterals from the IMA, acute thrombosis on chronic aortoiliac stenosis was highly suspected. Therefore, we performed aortoiliac thrombectomy through the femoral access to remove the thrombosis and expose the underlying stenotic lesion, and followed by placement of covered stent to reconstruct the aortoiliac bifurcation. In this patient, preservation of collaterals from IMA to lower abdomen and pelvis was essential to decrease the risk of bowel ischemia because the right IIA was occluded and the stenotic left IIA was covered by the iliac stent after CERAB. An on-table fenestration technique was used to preserve the IMA. A bridging balloon-expandable covered stent was deployed across the aortic fenestration and IMA.
During thrombectomy using a 7F Fogarty catheter, resistance was encountered at the distal aortic level when a Fogarty balloon catheter was withdrawn under fluoroscopy. Chronic abdominal aortic stenosis was suspected and subsequently confirmed with an angiogram after thrombectomy. Catheter-directed thrombolysis was an alternative option to decrease the burden of blood clot. However, catheter-directed thrombolysis needs close monitoring and is associated with the risk of hemorrhage and distal embolism. Minion10 reported the experience of thrombolysis and CERAB in six patients with chronic juxtarenal aortic occlusion. The thrombolytic duration was 12 to 72 hours without major complications, the patency rate was 100% at 15 months' follow-up. To prevent embolism of IMA during thrombectomy, a 4-mm balloon was parked in the proximal IMA from brachial access.
The underlying stenosis of the aortoiliac artery was identified after thrombectomy and treated with angioplasty and CERAB. Even without residual stenosis after angioplasty for the aorta and bilateral iliac arteries, stenting was absolutely indicated in this scenario. Ideally, an aortic cuff or short balloon-expandable covered stent should be used for the distal aorta during CERAB. In this patient, the diameter of the normal aorta proximal to the occlusion was 16 mm on preoperative CT scan. The minimum diameter of abdominal aortic off-the-shelf cuff is 22 mm. There are three types of balloon-expandable covered stents available in China, including the Gore Viabahn VBX, BD LifeStream, and BD Fluency with a maximum diameter of ≤13.0 mm, 12.0 mm, and 13.5 mm respectively. A commercially available aortic cuff or short balloon-expandable covered stent with a suitable size was not readily available. Therefore, we used a long iliac limb with a diameter of 16 mm for the distal aorta in this patient. Because there was thrombus surrounding the orifice of the IMA, the proximal landing zone of the aortic covered stent should be above the IMA origin. In this situation, an on-table fenestration technique was used to preserve IMA. The diameter of the IMA was measured to be 5 mm on preoperative CT image. Therefore, we used a 5 × 29 mm balloon expandable covered stent (Viabahn VBX, W. L. Gore & Associates). A snorkel/chimney technique is another viable endovascular alternative for preservation of the IMA during CERAB.11,12 Kissing stents can also be used to reconstruct the aortoiliac bifurcation. Geometrical study comparing kissing stents and CERAB supported that a CERAB configuration was a more anatomical and physiological reconstruction method.13 A recently published systematic review showed the pooled primary patency rates of CERAB were 94.4%, 84.4%, and 83.8% at 12, 24, and 36 months, respectively. The technical success and 30-day mortality and morbidity rates were 95.9%, 1.9%, and 6.4%, respectively.14
Other, more conventional treatment options can be considered. Open aortobifemoral bypass has a high primary patency rate, but carries a higher risk of perioperative mortality and morbidity.1 Extra-anatomical bypasses such as axillobifemoral bypass can be used in frail patients, but is associated with inferior long-term patency. Data from the Vascular Quality Initiative between 2009 and 2021 suggested that CERAB had a similar primary patency at 1 year compared with aortobifemoral bypass with a lower perioperative rate.15 However, the long-term outcomes of CERAB have not been well-defined because it is a relatively new technique and no randomized controlled trial comparing CERAB with aortobifemoral bypass has been conducted.
Conclusions
Our comprehensive management with thrombectomy, CERAB, and concurrent on-table fenestration for IMA preservation was an alternative novel, effective, and safe approach for the treatment of complex AIOD in this patient. This technique requires certain endovascular expertise and experience, but minimized the risk of bowel ischemia when the bilateral IIAs were occluded or covered by CERAB.
Disclosures
None.
Footnotes
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Nordanstig J., Behrendt C.A., Baumgartner I., et al. Editor's choice -- European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of asymptomatic lower limb peripheral arterial disease and intermittent claudication. Eur J Vasc Endovasc Surg. 2024;67:9–96. doi: 10.1016/j.ejvs.2023.08.067. [DOI] [PubMed] [Google Scholar]
- 2.Salem M., Hosny M.S., Francia F., et al. Management of extensive aorto-iliac disease: a systematic review and meta-analysis of 9319 patients. Cardiovasc Intervent Radiol. 2021;44:1518–1535. doi: 10.1007/s00270-021-02785-6. [DOI] [PubMed] [Google Scholar]
- 3.Piffaretti G., Fargion A.T., Dorigo W., et al. Outcomes from the Multicenter Italian Registry on primary endovascular treatment of aortoiliac occlusive disease. J Endovasc Ther. 2019;26:623–632. doi: 10.1177/1526602819863081. [DOI] [PubMed] [Google Scholar]
- 4.Amanvermez Senarslan D., Yildırım F., Bayram B., Kurdal A.T., Tetik O. Results of endovascular treatments of Trans-Atlantic Inter-Society Consensus C or D aortoiliac occlusive disease involving the aortic bifurcation. SAGE Open Med. 2023;11 doi: 10.1177/20503121231179836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Choudhry A.J., Shaw P.M. Endovascular aorto-iliac reconstruction vs. aortobifemoral bypass as first choice for a durable revascularization for aorto-iliac occlusive disease. Vasc Endovascular Surg. 2023;57:88–92. doi: 10.1177/15385744221130870. [DOI] [PubMed] [Google Scholar]
- 6.Goverde P.C., Grimme F.A., Verbruggen P.J., Reijnen M.M. Covered endovascular reconstruction of aortic bifurcation (CERAB) technique: a new approach in treating extensive aortoiliac occlusive disease. J Cardiovasc Surg. 2013;54:383–387. [PubMed] [Google Scholar]
- 7.Rouwenhorst K.B., Abdelbaqy O.M.A., van der Veen D., van Rijswijk R.E., Holewijn S., Reijnen M.M.P.J. Long-term outcomes of the covered endovascular reconstruction of the aortic bifurcation (CERAB) technique in patients with aorto-iliac occlusive disease. J Endovasc Ther. 2023 doi: 10.1177/15266028231166539. [DOI] [PubMed] [Google Scholar]
- 8.de Cort B.A., Salemans P.B., Fritschy W.M., Pierie M.E.N., Lind R.C. Long-term outcome for covered endovascular reconstruction of aortic bifurcation for aortoiliac disease: a Single-Center experience. J Endovasc Ther. 2021;28:906–913. doi: 10.1177/15266028211028210. [DOI] [PubMed] [Google Scholar]
- 9.Rison R.A., Kidd M.R., Koch C.A. The CARE (CAse REport) guidelines and the standardization of case reports. J Med Case Rep. 2013;7:261. doi: 10.1186/1752-1947-7-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Minion D.J. Lysis and covered endovascular reconstruction of the aortic bifurcation (LA CERAB) technique for chronic juxtarenal aortic occlusions. J Cardiovasc Surg. 2023;64:389–395. doi: 10.23736/S0021-9509.23.12685-1. [DOI] [PubMed] [Google Scholar]
- 11.Li W., Santana D., Phillips C. Comprehensive management of challenging recurrent aortoiliac and lower extremity occlusive disease with simultaneous modified-covered endovascular reconstruction of the aortic bifurcation, inferior mesenteric artery snorkel, and lower extremity bypass. Vascular. 2024 doi: 10.1177/17085381241245874. [DOI] [PubMed] [Google Scholar]
- 12.Chaudhuri A., Dey R. Chimney endovascular reconstruction of the aortic bifurcation (Ch-ERAB) for aorto-iliac occlusive disease allows inferior mesenteric arterial preservation. Eur J Vasc Endovasc Surg. 2017;54:404. doi: 10.1016/j.ejvs.2017.05.007. [DOI] [PubMed] [Google Scholar]
- 13.Groot Jebbink E., Grimme F.A., Goverde P.C., van Oostayen J.A., Slump C.H., Reijnen M.M. Geometrical consequences of kissing stents and the covered endovascular reconstruction of the aortic bifurcation configuration in an in vitro model for endovascular reconstruction of aortic bifurcation. J Vasc Surg. 2015;61:1306–1311. doi: 10.1016/j.jvs.2013.12.026. [DOI] [PubMed] [Google Scholar]
- 14.Bontinis V., Bontinis A., Giannopoulos A., et al. Covered endovascular reconstruction of the aortic bifurcation: a systematic review aggregated data and individual participant data meta-analysis. J Vasc Surg. 2024;79:1525–1535.e9. doi: 10.1016/j.jvs.2023.12.021. [DOI] [PubMed] [Google Scholar]
- 15.Semaan D.B., Habib S.G., Abdul-Malak O.M., et al. Aortobifemoral bypass vs covered endovascular reconstruction of aortic bifurcation. J Vasc Surg. 2024;80:459–465.e2. doi: 10.1016/j.jvs.2024.03.437. [DOI] [PubMed] [Google Scholar]