Abstract
BACKGROUND
Though endometrial carcinomas are a relatively common cancer of the female genitourinary tract, they rarely metastasize. Similarly, clival metastases make up a tiny fraction of all brain metastases. To the authors’ knowledge, an endometrial carcinoma clival metastasis has never been described in the literature; therefore, the authors present the following unusual case of a 69-year-old female with a history of an initially grade 2 endometrial adenocarcinoma that metastasized to her clivus.
OBSERVATIONS
Endometrial carcinoma has the potential to metastasize to the clivus.
LESSONS
Endometrial carcinoma, even when initially low grade, can metastasize intracranially. Prompt diagnosis with tissue biopsy and radiation is the mainstay of treatment, although the prognosis remains poor.
Keywords: skull base neoplasm, clivus tumor, endometrial carcinoma, malignant epithelial neoplasms, neoplasm metastases
ABBREVIATIONS: MRI = magnetic resonance imaging.
The clivus is an important landmark within the skull base with a close relationship to vascular structures, cranial nerves, and the brainstem. Clival metastases are an exceedingly rare subtype of intracranial tumors, accounting for a mere 0.02% of cases.1 As many tumors in this region remain asymptomatic until they have grown substantially, they are often discovered incidentally on imaging. Furthermore, clival metastases are often difficult to distinguish from other clival pathologies such as chordomas or chondrosarcomas.1 The time of presentation of these tumors also varies considerably. Some case reports have described clival metastases as occurring soon after initial disease presentation, others as the only sign of primary disease, and still others occurring multiple years after the diagnosis of established primary cancers.1, 2
The most common primary cancers metastasizing to the clivus are prostate, gastrointestinal tract, lung, and kidney, though cases of tonsillar carcinoma, hepatocellular carcinoma, bladder carcinoma, cervical carcinoma, and intraductal breast carcinoma have also been reported.1, 3, 4 To our knowledge, there have been no reports of endometrial carcinoma metastasizing to the clivus. Endometrial carcinoma is the most common cancer of the female genital tract, yet metastatic lesions occur in less than 5% of cases and brain metastases account for approximately 0.6% of these lesions.5, 6 While lymphatics are the main form of metastatic spread, endometrial carcinoma can also disseminate hematogenously to distant sites such as the lungs or bone.6 Here, we report an aggressive case of endometrial carcinoma metastasizing to the clivus.
Illustrative Case
A 69-year-old female presented to the neurosurgery clinic following the incidental discovery of an erosive clival lesion on surveillance brain magnetic resonance imaging (MRI; Fig. 1). Her medical history was significant for endometrial adenocarcinoma, for which she had undergone a hysterectomy, bilateral salpingo-oopherectomy, and pelvic lymph node dissection 2 years earlier, as well as a remote history of thyroid cancer with a thyroidectomy. The right-sided pelvic nodes returned positive for adenocarcinoma, and she was subsequently treated with local radiation and an antiestrogenic progestin derivative with good tumor control. Initial systemic imaging revealed no evidence of distant metastases.
FIG. 1.
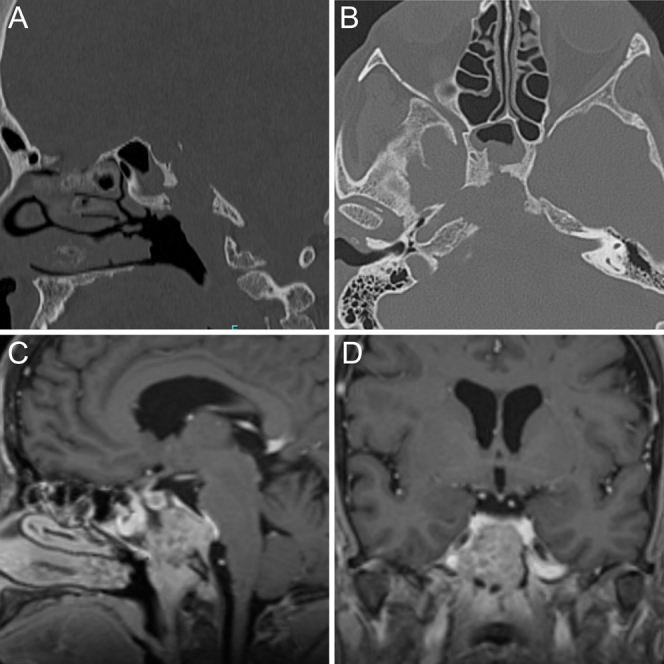
Preoperative sagittal (A) and axial (B) head computed tomography demonstrates an erosive clival lesion with superior extension to the dorsum sellae as well as to the right, eroding the bone around the lacerum segment of the right internal carotid artery. The posterior table of the clivus has been eroded. Sagittal (C) and coronal (D) postcontrast T1-weighted MRI demonstrates an enhancing lesion with encroachment upon the lacerum segment of the right internal carotid artery. Posteriorly, there is mild effacement of the basilar artery and ventral pons.
A neurosurgery consultation was ordered, given the discovery of a small heterogeneously enhancing mass within the clivus on MRI of the brain, which had been performed because of a new posterior headache. A small amount of erosion of the anterior clival cortex was noted (Fig. 1). The differential diagnosis at the time included chordoma, plasmacytoma, and metastasis. Additional workup via computed tomography of the chest had shown lung nodules that were biopsied but returned benign. Shortly after, she developed diplopia from a complete right abducens nerve palsy. Imaging showed rapid expansion of the clival mass, prompting urgent resection via an endoscopic endonasal transclival approach (Fig. 2). A near-total resection was achieved, with portions of the tumor left behind that were densely adherent to the clival dura and the right internal carotid artery (Fig. 3). Final pathology was consistent with endometrial adenocarcinoma (Fig. 4). Adjuvant stereotactic radiation therapy was planned.
FIG. 2.
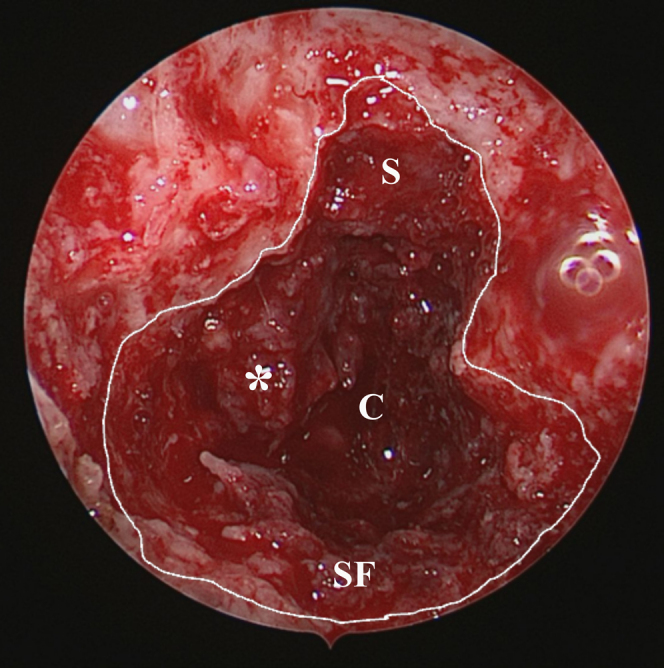
Endoscopic endonasal view of the sphenoid sinus and clivus with the resection cavity outlined in white, revealing the tumor tissue. Skeletonized lacerum segment (proximal paraclival) of the right internal carotid artery (asterisk). C = clivus dura; S = sella; SF = sphenoid sinus floor.
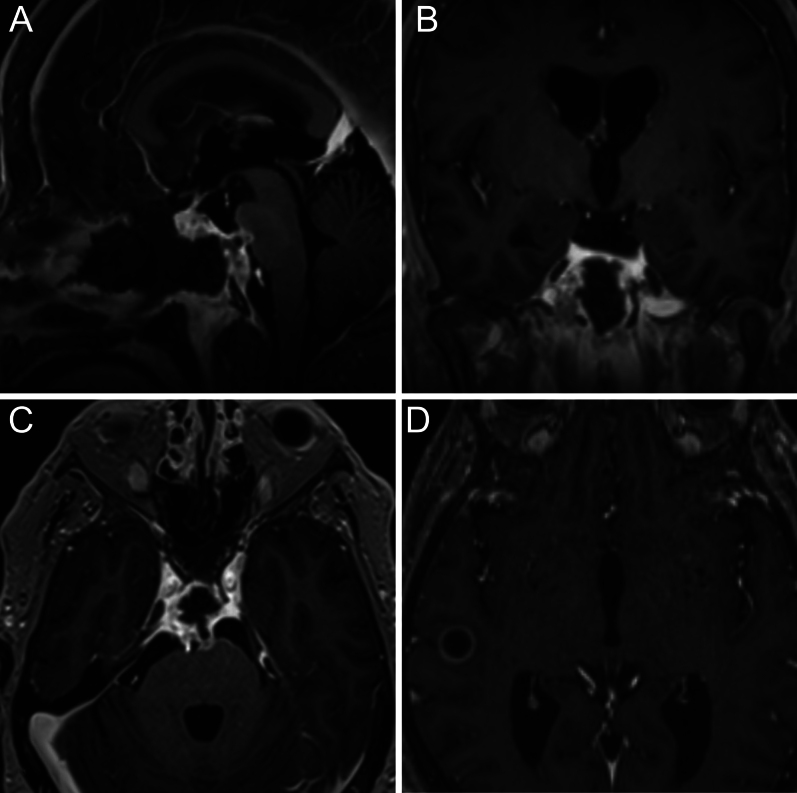
FIG. 3.
Postoperative sagittal (A), coronal (B), and axial (C) postcontrast T1-weighted MRI demonstrating near-total resection of an invasive clival metastatic mass. A small amount of residual tumor is seen around the lacerum and paraclival right internal carotid artery as well as adjacent to the right Dorello’s canal. The tumor was densely adherent to the clival dura. Two weeks postoperatively, a new right temporal lobe metastasis was seen, demonstrating the aggressive nature of the tumor (D).
FIG. 4.
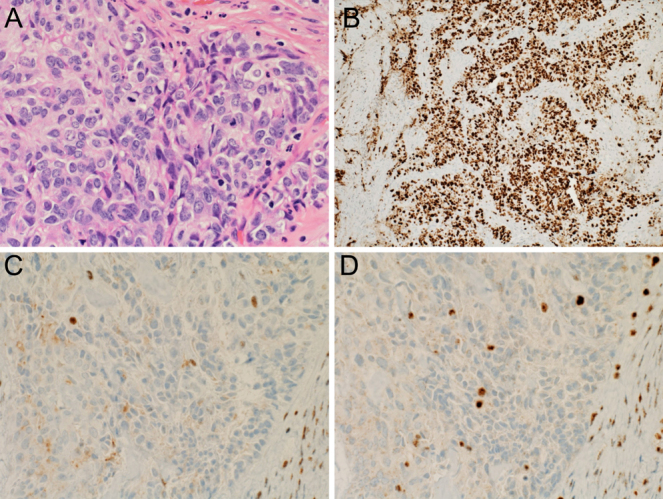
A: Microscopic hematoxylin and eosin evaluation showed a poorly differentiated neoplasm composed of sheets and nests of cells with ample, eosinophilic cytoplasm and large, pleomorphic nuclei, with frequent mitoses present. B: The Ki-67 proliferation rate is approximately 80% within the malignant cells. C: Expression of MLH-1, a protein in mismatch repair, is lost in malignant cells. D: Expression of PMS-2, a protein in mismatch repair, is lost in malignant cells. Original magnification ×400 (A, C, and D); ×100 (B).
Postoperatively, she did well overall but did not have improvement in her abducens nerve palsy, despite receiving dexamethasone as well, presumably because of continued compression of the abducens nerve in the vicinity of Dorello’s canal due to an inability to safely remove this portion of the tumor. She was discharged home on postoperative day 1 but returned 2 weeks later because she experienced a seizure from a newly discovered right temporal lobe intra-axial tumor (Fig. 3). Repeat brain MRI at this time demonstrated progressive enlargement and midline dural invasion of the residual clival tumor with effacement of the ventral pons. She was placed on levetiracetam and underwent urgent stereotactic radiation therapy. However, she returned to the emergency department 2 weeks later for dysphagia and asymmetric weakness, which, as revealed via imaging, were related to infarcts in the left frontal lobe and left anterior pons. Ultimately, she was transitioned to hospice and died of her illness.
Patient Informed Consent
The necessary patient informed consent was obtained in this study.
Discussion
Observations
The present case is unusual, if not unprecedented, according to our review of the literature. Endometrial carcinoma is relatively common. However, metastatic lesions occur < 5% of the time, with only 1.4% of those occurring in the brain.7, 8 They often portend a bleak prognosis. One systematic review determined that patients with metastases to the clivus died a mean of 9.4 months after initial presentation.3 The rapid expansion of the clival lesion and presentation of a new temporal lobe mass, as demonstrated on our patient’s imaging after her first seizure, certainly support the importance of early recognition. For these reasons, we will review salient clinical manifestations and future considerations for early diagnosis of these lesions.
Lessons
The majority of symptomatic clival lesions present with headache and diplopia attributable to an abducens nerve palsy.1, 4 The petrosal process of the sphenoid bone is the superolateral portion of the clivus, which comprises the inferomedial portion of Dorello’s canal, where this nerve traverses, beneath the petrosphenoidal ligament.9 An abducens nerve palsy is often the sole abnormality appreciated on physical examination, which, in combination with its rarity, makes it a rare entity to diagnose.1, 3 Unsurprisingly, with a larger tumor burden, combinations of presenting signs are described, with the involvement of multiple cranial nerves, including optic, trigeminal, and vagal palsies.3 There also appears to be a slight male predominance, ranging from 55% to 67.2%.3, 4 As mentioned previously, cancers that commonly metastasize to the bone (including breast and prostate) are most commonly the source of clival metastases, though the case presented here demonstrates an exception.
One of the more unusual features of this clival metastasis was its aggression. The patient received prompt treatment with resection via an endonasal endoscopic approach, generally accepted as the safest way to approach these lesions, as well as stereotactic radiation surgery.10, 11 However, the patient’s time from incidental discovery of the clival mass to death was just under 1 year. The period from the onset of symptoms attributable to the intracranial metastasis to her death was just under 3 months. Radiation targeted to the clivus has been shown to be helpful in prostate cancer, breast cancer, and multiple myeloma, though early detection is essential and the overall prognosis remains dismal.1, 4, 11 Examples of endometrial cancer metastasizing to the clivus are not documented in the literature, and several mechanisms that portend radioresistance in some tumors have been identified.12
The pathology of our patient’s tumor is consistent with an aggressive clinical course. The patient’s primary tumor, removed approximately 2 years prior, was a grade 2 endometrioid adenocarcinoma and showed extensive invasion, including > 90% of myometrial depth, involvement of the lymphovascular system, and favored involvement of soft tissue. Evaluation of the tumor metastatic to the clivus showed a poorly differentiated neoplasm invading bone and soft tissue with a Ki-67 proliferation rate of 80% (Fig. 4A and B). Molecular testing performed on this specimen revealed high microsatellite instability and defective mismatch repair, with loss of expression of MLH-1 and PMS-2 (Fig. 4C and D). High microsatellite instability is associated with characteristics related to more aggressive disease, including deep myometrial invasion, lymphovascular invasion, greater histological grade, and later-stage disease.13, 14
In the case of an unusually aggressive progression as in our patient, the likelihood of an underlying genetic mutation should be considered. Cowden syndrome is an autosomal dominant syndrome that predisposes affected individuals to a variety of benign and cancerous conditions, including thyroid and endometrial cancers. It was first described in 1963 and was not associated with the tumor suppressor phosphatase and tensin homolog (PTEN) gene until 1997.15, 16 Women with abnormalities in PTEN have twice the risk of developing cancer compared to men with the condition.17 Guidelines delineating appropriate clinical circumstances for initiating the complicated genetic testing needed to diagnose Cowden syndrome have been established by the National Comprehensive Cancer Network, but considerable heterogeneity in presentations and underlying mechanisms have been described.16, 18, 19 As the technology surrounding genetic testing continues to improve, so too might the potential for early screening and diagnosis, leading to earlier treatment of aggressive cancers attributable to genetic conditions.
Even if it is initially low grade, endometrial carcinoma can metastasize intracranially and portends a poor prognosis. Though seldom high in our differential diagnosis, an isolated abducens nerve palsy should alert one to the possibility of a clival lesion, as it is the most frequent presenting symptom. Treatment should be considered promptly for the best outcomes.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Avery, Samargandy. Acquisition of data: Avery, Sheldon, Riordan, Fallahi, Samargandy. Analysis and interpretation of data: Sheldon, Samargandy. Drafting the article: Avery, Sheldon, Riordan, Fallahi, Samargandy. Critically revising the article: Avery, Sheldon, Riordan, Le. Reviewed submitted version of manuscript: Avery, Sheldon, Riordan, Le. Approved the final version of the manuscript on behalf of all authors: Avery. Administrative/technical/material support: Samargandy. Study supervision: Avery, Sheldon.
Correspondence
Michael B. Avery: University of Arizona, Tucson, AZ. mbavery@arizona.edu.
References
- 1.Pallini R, Sabatino G, Doglietto F, Lauretti L, Fernandez E, Maira G. Clivus metastases: report of seven patients and literature review. Acta Neurochir (Wien). 2009;151(4):291-296. [DOI] [PubMed] [Google Scholar]
- 2.Altman KW, Mirza N, Philippe L. Metastatic follicular thyroid carcinoma to the paranasal sinuses: a case report and review. J Laryngol Otol. 1997;111(7):647-651. [DOI] [PubMed] [Google Scholar]
- 3.Jozsa F, Das JM. Metastatic lesions of the clivus: a systematic review. World Neurosurg. 2022;158:190-204. [DOI] [PubMed] [Google Scholar]
- 4.Sturgis R, Mack A, Kim S, Maier J, Heath EI. Symptom outcomes of cancer patients with clival metastases treated with radiotherapy: a study of 44 patients. Anticancer Res. 2021;41(10):5001-5006. [DOI] [PubMed] [Google Scholar]
- 5.Piura E, Piura B. Brain metastases from endometrial carcinoma. ISRN Oncol. 2012;2012:581749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kato MK, Tanase Y, Uno M, Ishikawa M, Kato T. Brain metastases from uterine cervical and endometrial cancer. Cancers (Basel). 2021;13(3):519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kouhen F, Afif M, El Kabous M, et al. Brain metastasis of endometrial cancer: report of a case and review of literature. Pan Afr Med J. 2015;20:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martínez-Mañas RM, Brell M, Rumià J, Ferrer E. Brain metastases in endometrial carcinoma. Gynecol Oncol. 1998;70(2):282-284. [DOI] [PubMed] [Google Scholar]
- 9.Doniz-Gonzalez A, Vigo V, Nunez MA, et al. Microsurgical anatomy and the importance of the petrosal process of the sphenoid bone in endonasal surgery. J Neurosurg. 2022;137(5):1431-1442. [DOI] [PubMed] [Google Scholar]
- 10.Vellutini A, Balsalobre L, Hermann DR, Stamm AC. The endoscopic endonasal approach for extradural and intradural clivus lesions. World Neurosurg. 2014;82(6suppl):S106-S115. [DOI] [PubMed] [Google Scholar]
- 11.Cathel A, Khan YR, Blais D, Mahato B, Mahato D. Metastatic disease to clivus: biopsy or not? Cureus. 2019;11(9):e5658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sorolla MA, Parisi E, Sorolla A. Determinants of sensitivity to radiotherapy in endometrial cancer. Cancers (Basel). 2020;12(7):1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.An HJ, Kim KI, Kim JY, et al. Microsatellite instability in endometrioid type endometrial adenocarcinoma is associated with poor prognostic indicators. Am J Surg Pathol. 2007;31(6):846-853. [DOI] [PubMed] [Google Scholar]
- 14.Bell DW, Ellenson LH. Molecular genetics of endometrial carcinoma. Annu Rev Pathol. 2019;14:339-367. [DOI] [PubMed] [Google Scholar]
- 15.Lloyd KM, Dennis M. Cowden’s disease. A possible new symptom complex with multiple system involvement. Ann Intern Med. 1963;58:136-142. [DOI] [PubMed] [Google Scholar]
- 16.Liaw D, Marsh DJ, Li J, et al. Germline mutations of the PTEN gene in Cowden disease, an inherited breast and thyroid cancer syndrome. Nat Genet. 1997;16(1):64-67. [DOI] [PubMed] [Google Scholar]
- 17.Bubien V, Bonnet F, Brouste V, et al. High cumulative risks of cancer in patients with PTEN hamartoma tumour syndrome. J Med Genet. 2013;50(4):255-263. [DOI] [PubMed] [Google Scholar]
- 18.Pilarski R, Burt R, Kohlman W, Pho L, Shannon KM, Swisher E. Cowden syndrome and the PTEN hamartoma tumor syndrome: systematic review and revised diagnostic criteria. J Natl Cancer Inst. 2013;105(21):1607-1616. [DOI] [PubMed] [Google Scholar]
- 19.Yehia L, Ni Y, Sesock K, et al. Unexpected cancer-predisposition gene variants in Cowden syndrome and Bannayan-Riley-Ruvalcaba syndrome patients without underlying germline PTEN mutations. PLoS Genet. 2018;14(4):e1007352. [DOI] [PMC free article] [PubMed] [Google Scholar]