Abstract
BACKGROUND
Gastrointestinal lymphoma typically arises in the stomach, small bowel, or colorectum and is usually a B-cell lymphoma. However, primary T-cell lymphomas originating in the stomach are particularly rare. Gastric peripheral T-cell lymphoma-not otherwise specified (PTCL-NOS) is an extremely rare subtype.
CASE SUMMARY
We report a 63-year-old male presenting with epigastric pain. Esophagogastroduodenoscopy revealed a large ulcerative lesion in the gastric cardia. Biopsy and immunohistochemical profiling confirmed PTCL-NOS. Imaging indicated stage II disease involving the stomach and intra-abdominal lymph nodes. The patient is planned to undergo cyclophosphamide, doxorubicin, vincristine, and prednisone or cyclophosphamide, doxorubicin, vincristine, prednisone, and etoposide chemotherapy.
CONCLUSION
This case highlights the necessity of considering PTCL-NOS in differential diagnoses of gastric lesions. Comprehensive histopathological and immunohistochemical analysis is crucial for accurate diagnosis and guiding treatment.
Keywords: Gastrointestinal lymphoma, Stomach, Peripheral T-cell lymphoma-not otherwise specified, Extranodal lymphoma, Case report
Core Tip: Gastrointestinal lymphoma is an extranodal malignancy primarily arising in the stomach, small intestine, or colorectum, most commonly presenting as B-cell lymphoma. In contrast, primary T-cell lymphomas of the stomach are exceedingly rare, particularly within the spectrum of T-cell lymphoma subtypes. Among these, gastric peripheral T-cell lymphoma-not otherwise specified (PTCL-NOS) is extremely rare. In this report, we present a rare case of a 63-year-old male diagnosed with gastric PTCL-NOS, along with a detailed examination of the clinicopathological features.
INTRODUCTION
Gastrointestinal (GI) lymphoma is the most common extranodular lymphoma, accounting for 30%-40% of all extranodular lymphoma, and has distinct clinical and pathological characteristics[1,2]. More than 80% of the GI lymphomas are B-cell lymphomas. The stomach is the most commonly affected site for GI lymphoma, followed by the small bowel, colorectum, and esophagus[3,4]. The majority of primary gastric lymphoma cases are B-cell lymphomas, while T-cell lymphomas are known to be rare. The incidence of primary gastric T-cell lymphoma (PG-TCL) is estimated to be exceptionally low, making it challenging to determine, and it is reported through documented cases[3]. Consequently, only a few cases have been reported. The T-cell lymphoma of the stomach is mainly categorized into anaplastic large cell lymphoma (ALCL), natural killer (NK)/T-cell lymphoma, or enteropathy-associated T-cell lymphoma (EATL)[5,6]. Peripheral T-cell lymphoma-not otherwise specified (PTCL-NOS) includes all T-cell lymphomas that don’t meet the diagnostic criteria of any category.
To the best of our knowledge, primary gastric PTCL-NOS have been rarely reported. Therefore, we present a gastric PTCL-NOS case and describe its clinic-pathological and endoscopic features.
CASE PRESENTATION
Chief complaints
A 63-year-old male was admitted to Kangwon National University Hospital with a 3-week history of epigastric pain.
History of present illness
The patient denied weight loss and febrile sense. Physical examination revealed that his abdomen was soft without tenderness or rebound tenderness.
History of past illness
The patient denied any significant past medical history.
Personal and family history
The patient's personal and family history had no notable findings.
Physical examination
The physical examination revealed that the patient’s abdomen was soft. It was not tender. Rebound tenderness was not observed.
Laboratory examinations
Blood test results revealed that white blood cell count, hemoglobin, and platelet count were within normal ranges. However, lactate dehydrogenase level was slightly elevated at 244 U/L (reference range: 119-229 U/L).
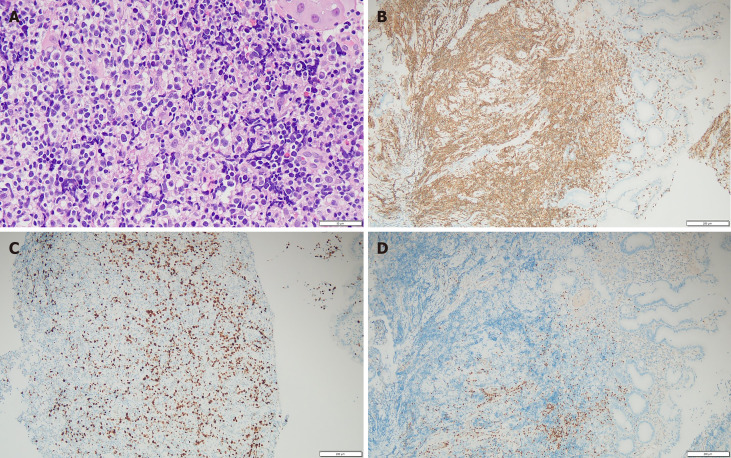
In hematoxylin and eosin staining of the stomach tissue, majority of malignant cells were intermediate to large-sized abnormal lymphoid cells. Characteristics commonly found in gastric carcinomas, such as intestinal dysplasia, cylindrical epithelial cells, and prominent intracytoplasmic mucin vacuoles, were not detected in this case. A pan-cytokeratin immunohistochemistry (IHC) test yielded a negative result, ruling out gastric carcinoma. Tests for CD20, PAX5, CD10, and Bcl-6 also returned negative results, excluding the possibility of B-cell lineage lymphoma. CD3, CD5, CD7, and CD4 were expressed positively (Figure 1). These cells also exhibited a relatively elevated Ki-67 proliferation index (30%). The T-cell receptor gamma gene rearrangement test demonstrated a positive result. Pathological findings were indicative of high-grade T-cell lymphoma. Further IHC tests were conducted to differentiate between various subtypes of T-cell lymphoma, including NK/T-cell lymphoma, EATL, monomorphic epitheliotropic intestinal T-cell lymphoma, angioimmunoblastic T-cell lymphoma, ALCL, and PTCL-NOS. However, CD30, ALK (D5F3), CD56, granzyme B, and Epstein-Barr virus all showed negative results.
Figure 1.
Histopathological findings. A: Hematoxylin and eosin staining of stomach of magnification of 400 ×; B-D: Results of immunohistochemistry revealing the tumor was CD3 positive, Ki-67 positive, and PAX positive (magnification 100 ×).
Imaging examinations
To investigate the cause of the patient's primary symptom, an esophagogastroduodenoscopy was first performed, revealing a large irregular ulcerative lesion in the gastric cardia (Figure 2). This endoscopic finding was clinically suspected as advanced gastric cancer. Thus, a biopsy was performed.
Figure 2.
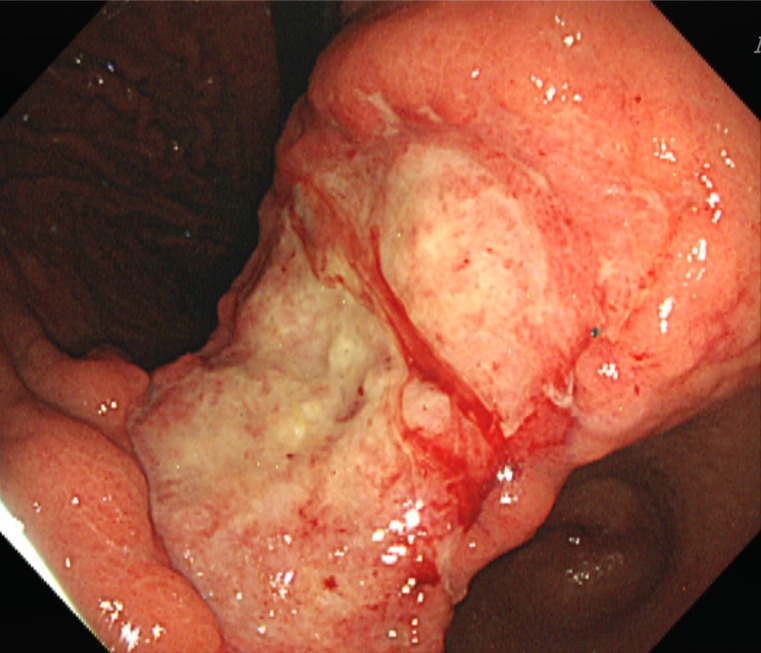
Endoscopic finding. A huge irregular ulcerative lesion in the gastric cardia.
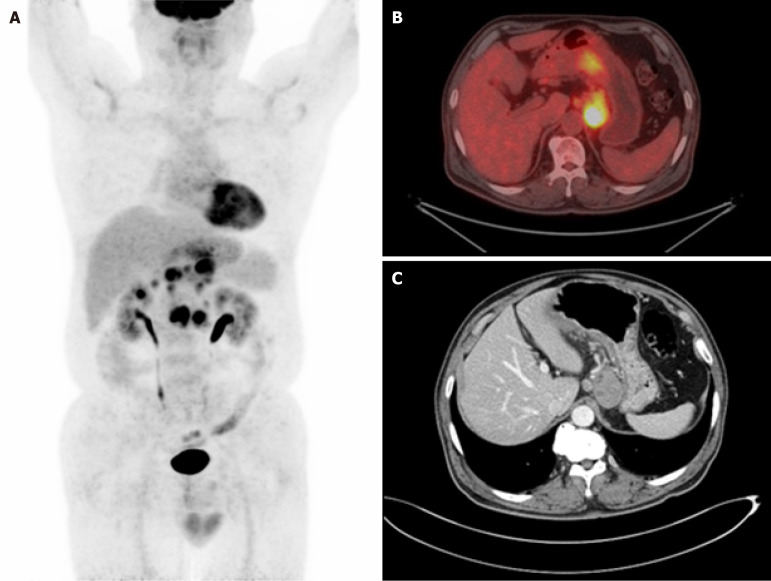
After confirmation of the biopsy result, to determine the stage of the lymphoma, the patient underwent imaging tests, including abdominal and pelvic computed tomography (CT) scans and 18F-fluorodeoxyglucose-positron emission tomography/CT scans (Figure 3). These imaging studies showed the involvement of stomach and intra-abdominal lymph nodes.
Figure 3.
Underwent imaging. A and B: Positron emission tomography showed hypermetabolic mass located in the lower body; C: Computed tomography showed diffuse wall thickening of the posterior lesser curvature of the gastric body with metastatic nodes.
FINAL DIAGNOSIS
Based on these findings, the patient received a diagnosis of PTCL-NOS, meeting the diagnostic criteria for intestinal T-cell lymphoma, not otherwise specified based on the revised World Health Organization 2018 classification.
TREATMENT
The patient underwent a bone marrow examination, which confirmed that there was no lymphoma involvement in the bone marrow. The final staging was determined to be stage II. The patient received a total of six cycles of chemotherapy with cyclophosphamide, doxorubicin, vincristine, prednisone, and etoposide.
OUTCOME AND FOLLOW-UP
The patient did not experience any significant complications or treatment-related adverse events throughout the chemotherapy. Complete remission was confirmed after six cycles of chemotherapy.
DISCUSSION
Primary gastric PTCL-NOS is a rare subtype of lymphoma. As a result, report about its prevalence is limited. Among several subtypes of T-cell lymphoma, EATL appears to be the most common subtype of gastric T-cell lymphoma according to several studies. It has been reported that EATL accounts for 12%-40% of all gastric T-cell lymphomas[6,7].
In a study on primary GI lymphoma conducted in China, 415 patients with primary GI lymphoma were identified between 1998 and 2013. Among these cases, T-cell lymphoma was reported in approximately 60 cases. Specifically, PG-TCL was reported in about 7 cases[6]. The study from China provided limited information regarding specific subtypes of T-cell lymphoma. According to SEER data analysis, from 1965 to 2016, a total of 164 patients with PG-TCL were analyzed. The age-adjusted occurrence rate of PG-TCL stood at 0.0091 per 100000 person-years and demonstrated an increase in frequency as age advanced. This incidence rate is about 1/20000 of the incidence rate of B-cell lymphoma. The present report also showed that its occurrence varied depending on ethnicity and geographic location. Patients with primary gastric PTCL-NOS showed distinctive clinical characteristics such as younger age at disease onset, higher incidence among males, less prevalence among white race, advanced disease stage, and frequent presence of symptom B. Furthermore, overall survival and cancer-specific survival rates of primary gastric PTCL-NOS patients were significantly lower than those of patients with other subtypes of gastric lymphoma[5]. Nevertheless, these two studies demonstrate that primary gastric PTCL-NOS is an exceedingly rare disease. It is important to note that endoscopic findings of primary gastric lymphoma can be nonspecific. They can resemble those of other gastric diseases such as gastric adenocarcinoma and peptic ulcer disease[8]. Therefore, histopathologic examination is required for a definitive diagnosis.
The optimal management for primary gastric PTCL-NOS has not been established yet. Although there was no specific research exclusively focusing on PTCL-NOS, retrospective studies related to the treatment of T-cell lineage gastric lymphoma indicated that the majority of patients received a combination therapy of cyclophosphamide, doxorubicin, vincristine, and prednisone[9,10]. Table 1 summarizes the studies that have investigated the treatment strategies and outcomes for patients with primary gastric PTCL-NOS. Treatment outcomes were evaluated based on disease status, with results ranging from death due to the disease to survival durations lasting from 7 months to over 83 months[5,8-10].
Table 1.
Treatment approaches and outcomes for primary gastric T-cell lymphoma: Summary of literatures
|
Ref.
|
Study period (year)
|
Study type
|
Sample size
|
Patients with gastric peripheral T-cell lymphoma-not otherwise specified
|
Patient demographics
|
Treatment
|
Outcomes
|
| Park et al[9] | 1990-2004 | Primary gastric lymphoma of T-cell origin | 17 | 7 (41.1) | Median age 49 years, male (14 : 3) | CHOP, cyclophosphamide, doxorubicin, vincristine, prednisone, and etoposide, Vanderbilt regimen, surgical resection | Median progression-free survival 10 months, median OS 12 months |
| Kim et al[8] | 1995-2008 | Endoscopic and clinical analysis of primary T-cell lymphoma of the GI tract | 36 | 5 (13.9) | Median age 50 years, male to female ratio 2.6:1 | Of the 36 patients, primary surgical resection with chemotherapy (55%), primary chemotherapy without surgery (45%) | Median OS 7.8 months, 3-year survival rate 19.4% |
| Kohri et al[10] | 2007-2018 | Peripheral T-cell lymphoma with GI involvement | 11 | 2 (2.4) | Median age 75 years, 10 males and 1 female | CHOP | OS 7 months and 83 months (2 patients) |
| Zhang et al[5] | 1975-2016 | Gastric T-cell lymphoma in the SEER program | 164 | 104 (63.4) | Median age 65 years, mostly White and male | Chemotherapy, surgery, radiotherapy | Median OS 8 months, 5-year OS 23.5% |
CHOP: Cyclophosphamide, doxorubicin, vincristine, and prednisone; GI: Gastrointestinal; OS: overall survival.
Primary gastric PTCL-NOS is rare, as it is typically found in other organs such as the small bowel rather than the stomach. B-cell lymphomas are more commonly associated with gastric involvement. However, in cases where gastric lymphoma is suspected, despite its low incidence, it is crucial to conduct appropriate testing for the diagnosis of T-cell lymphoma, known to have a poor prognosis. This approach can provide valuable insights and guide appropriate treatment decisions.
CONCLUSION
We present a case of gastric PTCL-NOS, a condition that is seldom discussed in relation to it endoscopic findings and the process of pathological differential diagnosis. This case is notable due to the rarity of gastric PTCL-NOS.
Footnotes
Informed consent statement: Informed written consent was obtained from the patient for publication of this report and any accompanying images.
Conflict-of-interest statement: The authors declare that they have no conflict of interest.
CARE Checklist (2016) statement: The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country of origin: South Korea
Peer-review report’s classification
Scientific Quality: Grade C
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade C
P-Reviewer: Liu YQ S-Editor: Luo ML L-Editor: A P-Editor: Wang WB
Contributor Information
Hee Ryeong Jang, Division of Hematology and Oncology, Department of Internal Medicine, Kangwon National University Hospital, Kangwon National University College of Medicine, South Korea.
Kyungyul Lee, Department of Pathology, Pathology Center, Seegene Medical Foundation, Seoul 61743, South Korea.
Kyu-Hyoung Lim, Division of Hematology and Oncology, Department of Internal Medicine, Kangwon National University Hospital, Kangwon National University College of Medicine, South Korea. kyuhyoung.lim@kangwon.ac.kr.
References
- 1.Bautista-Quach MA, Ake CD, Chen M, Wang J. Gastrointestinal lymphomas: Morphology, immunophenotype and molecular features. J Gastrointest Oncol. 2012;3:209–225. doi: 10.3978/j.issn.2078-6891.2012.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Groves FD, Linet MS, Travis LB, Devesa SS. Cancer surveillance series: non-Hodgkin's lymphoma incidence by histologic subtype in the United States from 1978 through 1995. J Natl Cancer Inst. 2000;92:1240–1251. doi: 10.1093/jnci/92.15.1240. [DOI] [PubMed] [Google Scholar]
- 3.Peng JC, Zhong L, Ran ZH. Primary lymphomas in the gastrointestinal tract. J Dig Dis. 2015;16:169–176. doi: 10.1111/1751-2980.12234. [DOI] [PubMed] [Google Scholar]
- 4.Morton JE, Leyland MJ, Vaughan Hudson G, Vaughan Hudson B, Anderson L, Bennett MH, MacLennan KA. Primary gastrointestinal non-Hodgkin's lymphoma: a review of 175 British National Lymphoma Investigation cases. Br J Cancer. 1993;67:776–782. doi: 10.1038/bjc.1993.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang M, Xiao F, Lin M, Chen M, Hou J, Huang H. The epidemiology and prognosis of patients with primary gastric T-cell lymphoma in the SEER program. Cancer Med. 2023;12:84–98. doi: 10.1002/cam4.4936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen Y, Chen Y, Chen S, Wu L, Xu L, Lian G, Yang K, Li Y, Zeng L, Huang K. Primary Gastrointestinal Lymphoma: A Retrospective Multicenter Clinical Study of 415 Cases in Chinese Province of Guangdong and a Systematic Review Containing 5075 Chinese Patients. Medicine (Baltimore) 2015;94:e2119. doi: 10.1097/MD.0000000000002119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tse E, Gill H, Loong F, Kim SJ, Ng SB, Tang T, Ko YH, Chng WJ, Lim ST, Kim WS, Kwong YL. Type II enteropathy-associated T-cell lymphoma: a multicenter analysis from the Asia Lymphoma Study Group. Am J Hematol. 2012;87:663–668. doi: 10.1002/ajh.23213. [DOI] [PubMed] [Google Scholar]
- 8.Kim DH, Lee D, Kim JW, Huh J, Park SH, Ha HK, Suh C, Yoon SM, Kim KJ, Choi KD, Ye BD, Byeon JS, Song HJ, Jung HY, Yang SK, Kim JH, Myung SJ. Endoscopic and clinical analysis of primary T-cell lymphoma of the gastrointestinal tract according to pathological subtype. J Gastroenterol Hepatol. 2014;29:934–943. doi: 10.1111/jgh.12471. [DOI] [PubMed] [Google Scholar]
- 9.Park YH, Kim WS, Bang SM, Lee SI, Kang HJ, Na II, Yang SH, Lee SS, Uhm JE, Kwon JM, Kim K, Jung CW, Park K, Ko YH, Ryoo BY. Primary gastric lymphoma of T-cell origin: clinicopathologic features and treatment outcome. Leuk Res. 2006;30:1253–1258. doi: 10.1016/j.leukres.2006.01.018. [DOI] [PubMed] [Google Scholar]
- 10.Kohri M, Tsukasaki K, Akuzawa Y, Tanae K, Takahashi N, Saeki T, Okamura D, Ishikawa M, Maeda T, Kawai N, Matsuda A, Arai E, Arai S, Asou N. Peripheral T-cell lymphoma with gastrointestinal involvement and indolent T-lymphoproliferative disorders of the gastrointestinal tract. Leuk Res. 2020;91:106336. doi: 10.1016/j.leukres.2020.106336. [DOI] [PubMed] [Google Scholar]