Abstract
Most longitudinal studies of healthcare workers’ mental health during COVID-19 end in 2021. We examined trends in hospital workers eight times, ending in 2023. A cohort of healthcare workers at one organization was surveyed at 3-month intervals until Spring 2022 and re-surveyed in Spring 2023 using validated measures of common mental health problems. Of 538 workers in the original cohort, 289 (54%) completed the eighth survey. Repeated-measures ANOVA revealed significant changes in psychological distress (F = 7.4, P < .001), posttraumatic symptoms (F = 14.1, P < .001), and three dimensions of burnout: emotional exhaustion (F = 5.7, P < .001), depersonalization (F = 2.7, P = .01), and personal accomplishment (F = 2.8, P = .008). Over time, psychological distress and depersonalization increased, posttraumatic symptoms and personal accomplishment decreased, and emotional exhaustion fluctuated significantly without net change. Most measures did not improve significantly in the year prior to the declaration of the pandemic’s end. The lack of improvement in psychological distress, emotional exhaustion, depersonalization, and personal accomplishment during the period in which COVID-19 case rates declined and public health measures were relaxed is a concerning indication of the chronicity of the impact of the pandemic on healthcare workers.
Subject terms: Occupational health, Human behaviour, Viral infection
Introduction
Hospital-based healthcare workers experience occupational stressors which increase the risk of many harms, including reduced job satisfaction, burnout, depressive and anxiety symptoms, poor perceived physical health, poor quality of life, and thoughts of suicide1–5. These harms affect healthcare organizations through absenteeism and workforce turnover6–9, increases in medical errors, and reduced patient satisfaction10–13. It has been widely documented that working during the COVID-19 pandemic increased the psychological burden of healthcare work14–16, but little is known about which pandemic-related effects were transient and which are likely to endure beyond the pandemic.
While the literature on the mental health impact of COVID-19 on healthcare workers is huge, with a few exceptions which extend into mid-202217–19, most longitudinal studies track the well-being of health care workers no further than 2021. However, the first wave of cases with the omicron variant, which peaked early in 2022, was the pandemic wave with by far the highest case rate20. Since cases rates have been in decline since, with a concomitant relaxing of public measures, leading to the official declaration of the end of the pandemic in May 202321, longitudinal measures that extend beyond 2022 are needed to determine if the occupational effects of the pandemic on healthcare workers are resolving over time. Knowledge of long-term trends is particularly important currently because shortages in the healthcare workforce have been described as a crisis22,23, so effective management of occupational harms is crucial not only for the well-being of healthcare workers and patients, but also for recruitment and retention of healthcare workers.
We have previously reported on trends in emotional exhaustion in hospital workers at one urban hospital at quarterly intervals starting in the fall of 2020, with the seventh measurement in the spring of 202224–26. We found that severity of emotional exhaustion tended to rise and fall with local case rates and differed by occupational group, with the greatest severity in nurses. The purpose of this report is to extend those observations by reporting on a broader range of mental health impacts and extending the period of observation with a 1-year follow-up in the spring of 2023. The follow-up measure occurred at a time when COVID-19 case rates were lower and the pandemic was officially declared over, and so provides an opportunity to observe if there was an improvement in measures of occupational stress when the acute impact of the pandemic was receding.
Methods
Setting, participants, and survey design
The study was conducted at Sinai Health, which is comprised of two sites, an acute care teaching hospital and a rehabilitation hospital, with a combined staff of over 6000, in Toronto, Canada. All hospital staff, aged 18 years or older, including hospital employees, physicians, learners, volunteers, and employees of third parties (e.g. retail employees) were invited via posters and hospital emails to participate in a longitudinal survey, distributed quarterly from the fall 2020 until spring 2022, with a follow-up measure in the spring of 2023, eight surveys in all.
Surveys were completed using online software (Alchemer, Louisville, CO) that adheres to privacy standards in Ontario, Canada (Personal Health Information Protection Act). All participants completed measures of emotional exhaustion and psychological distress at all time points, and of posttraumatic (PTSD) symptoms at T1, T3, T5, T7 and T8. Measures of depersonalization and personal accomplishment were also completed at all time points, but only by the 50% of participants randomly selected for a longer version of the survey. Scores for depersonalization and personal accomplishment were only included in the analysis for healthcare professionals (nurses, doctors, and members of other regulated healthcare professionals and their students) because nonprofessional participants requested a “not applicable” option for items on these scales after the T1 survey, and subsequently often used this option. For the first five surveys, participants received a gift card at the end of each completed survey valued at $15 US converted to Canadian currency. For surveys six to eight, the value of the gift card was increased to $20 US.
This study was approved by the Sinai Health Research Ethics Board (20-0084-E). All survey participants provided informed consent. All procedures were performed in accordance with relevant guidelines and regulations.
During the recruitment phase, 884 potential participants consented to receive surveys. Of these, 538 (61%) completing the first survey (T1, conducted September 21-November 15, 2020) which included the baseline measure of emotional exhaustion. These 538 formed the cohort for further follow-up. The participation rate at subsequent time points, with the numerator comprised of those participants who completed a valid measure of emotional exhaustion, psychological distress, or both was T2: 485/538 (90%), T3: 424/538 (79%), T4: 409/538 (76%), T5: 395/538 (73%), T6: 372/538 (69%), T7: 350/538 (65%), T8:289/538 (54%). The latter 289 participants were included in the current analysis.
Instruments
Emotional exhaustion, depersonalization and personal accomplishment were measured with the Maslach Burnout Inventory: Human Services Survey for Medical Personnel25. The emotional exhaustion (nine items), depersonalization (five items), and personal accomplishment (eight items) were each calculated as the sum of items scored 0 to 6. Across time points, Cronbach’s alpha ranged from 0.94 to 0.96 (emotional exhaustion, n = 289), 0.84-0.90 (depersonalization, n = 82), and 81-0.89 (personal accomplishment, n = 82).
Psychological distress, which is comprised of depressive and anxiety symptoms, was measured with the Kessler K6, which has 6 items scored from 0 to 4, yielding a range of 0–24 [27]. The K6 strongly discriminates between community cases and non-cases of psychiatric disorders diagnosed by structured interview [27] and has acceptable sensitivity and specificity [28]. In this cohort Cronbach’s alpha across time-points ranged from 0.85 to 0.90 (n = 289).
Posttraumatic symptoms were measured with the Impact of Events Scale-Revised (IES-R) [29], a 22-item measure that assesses hyperarousal, avoidance, and intrusion caused by traumatic events. Respondents are asked to identify a stressful life event (in this case specified as “working during COVID-19”) and then to rate how much they were bothered by 22 types of difficulty in the past 7 days (each scored from 0 to 4). The Cronbach’s alpha for the full scale at each time-point this measure was used (T1, T3, T5, T7, T8) ranged from 0.94 to 0.96 (n = 289).
Analysis
Descriptive statistics were used to characterize the sample. Participants were sorted into four categories of job-type as previously described24: nurses, other healthcare professionals, other personnel with patient contact, and other personnel without patient contact. Patient contact was determined by participants’ endorsement of the statement that “in the past month, my work has involved direct contact (within 2 metres for more than 15 minutes) with” patients.
To make the scales of various measures directly comparable, scores on all measures at all time points were converted to standardized scores (0 = full group mean at T1, units = standard deviations from T1 mean).
Changes over time, differences in scores by occupational group and the interaction of these variables were tested by repeated measures analysis of variance (ANOVA) with participants who did not provide valid measures at each time point excluded. The Greenhouse-Geisser correction was applied to tests of within-subjects effects when Mauchly’s test of sphericity indicated that sphericity could not be assumed. Standardized scores were plotted by occupational group at each time point in order to interpret significant results from ANOVA.
To test if the Spring 2023 (T8) value of each measure differed from the T7 measure (representing potential improvement as case rates declined and public health measures were relaxed) or differed from T1 (representing potential improvement from the early impact of the pandemic effects), difference scores were calculated: T8 – T7 and T8 – T1. Confidence intervals on difference scores were calculated to determine if they differed from zero, indicating change over time. All analyses were carried out using IBM SPSS Statistics 28 (Armonk, New York).
Results
The characteristics of the 289 hospital workers who participated in the survey in Spring 2023 (T8) are described in Table 1. Compared to 247 T1 participants who did not complete the T8 survey, the 289 participants reported on here did not differ with respect to occupation category, age, or education. Compared to nonparticipants, participants at T8 differed by gender (χ2 (df2) = 18.1, p < .001) in that they were more likely to be female (83% vs. 74%) and less likely to report gender as other or “prefer not to say” (2% vs. 10%). T8 participants and nonparticipants did not differ in T1 levels of emotional exhaustion or psychological distress. In contrast, T8 nonparticipants had higher levels of PTSD symptoms (mean 24.9, SD 16.6) at T1 than T8 participants (mean 20.7, SD 15.1, t = 3.1, p = .002). To understand if high PTSD symptoms at T1 was associating with becoming lost to follow-up throughout the longitudinal course of the study, we identified participants who stopping completing surveys completely, starting at a timepoint from T2 to T7. There were 186 such participants. Those lost to follow up had significantly higher T1 IES-R scores than those not lost to follow-up (25.6 vs. 21.1, t = 2.93, p = .003).
Table 1.
Characteristics of 289 participants at T8.
| Characteristic | n | % |
|---|---|---|
| Occupational Role1 | ||
| Nursing | 70 | 24.2 |
| Other Clinical Professionals | 85 | 29.4 |
| Other Clinical Personnel | 46 | 15.9 |
| Non-Clinical Personnel | 88 | 30.4 |
| Age (missing 3) | ||
| 18–30 | 78 | 27.0 |
| 31–40 | 79 | 27.3 |
| 41–50 | 79 | 27.3 |
| Over 50 | 50 | 17.3 |
| Gender | ||
| Female | 239 | 82.7 |
| Male | 44 | 15.3 |
| Other/prefer not to say | 6 | 2.0 |
| Education | ||
| High School or less | 3 | 1.0 |
| College Diploma | 39 | 13.5 |
| Undergraduate Degree | 95 | 32.9 |
| Professional or Graduate Degree | 152 | 52.6 |
| Marital Status | ||
| Married/Common-law | 173 | 59.9 |
| Single | 106 | 36.7 |
| Divorced/Separated/Widowed | 10 | 3.4 |
| Ethnicity | ||
| African/Black | 12 | 4.2 |
| Asian | 89 | 30.8 |
| South Asian | 17 | 5.9 |
| European/White | 144 | 49.8 |
| Hispanic | 4 | 1.4 |
| Other | 23 | 8.0 |
1. Most common occupation types by category (in descending order of numbers, with occupations with two or fewer participants not shown).
Other clinical professionals: physician, occupational therapist, physiotherapist, dietician, resident, clinical manager, social worker, speech language pathologist, respiratory therapist, pharmacist.
Other clinical positions: administrative assistant, medical imaging technologist.
Non-clinical position: research staff, research scientist, laboratory technician, administrative assistant, nonclinical manager, administrator, and clerk.
Some roles appear in both clinical and non-clinical lists as determined by patient contact as described by participant.
At the first measurement point, in Fall 2020, the mean values ± standard deviations of psychological measures for T8 participants were: psychological distress (K6) 6.0 ± 4.4, PTSD symptoms (IES-R) 20.8 ± 15.0, emotional exhaustion (MBI-EE) 25.0 ± 12.7, depersonalization (MBI-DP) 4.1 ± 5.1, and personal accomplishment (MBI-PA) 34.7 ± 11.3. To make the scales of various measures directly comparable, scores on all measures at all time points were converted to standardized scores (0 = full group mean at T1, units = standard deviations from T1 mean).
Analysis of changes in psychological measures over time, compared by occupational group, are provided in Table 2. There were significant changes over time in all variables, with significant differences by job type in each variable except depersonalization (for which p = .06). Interactions between changes over time and occupational group were not statistically significant, indicating that the trajectory of change did not differ by occupational group.
Table 2.
Results of repeated measures ANOVA assessing psychological variables over time by occupational group.
| Within Subjects | Between Subjects | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Time | Time X Job type | Job type | ||||||||
| N | df | F | Sig | df | F | Sig | df | F | Sig | |
| Psychological distress1 | 228 | 6.2 | 7.4 | < 0.001 | 18.5 | 0.4 | 0.99 | 3 | 4.6 | 0.004 |
| Posttraumatic symptoms | 248 | 4 | 14.1 | < 0.001 | 12 | 1.1 | 0.34 | 3 | 5.3 | 0.001 |
| Burnout – Emotional Exhaustion1 | 227 | 5.4 | 5.7 | < 0.001 | 16.1 | 1.3 | 0.22 | 3 | 8.9 | < 0.001 |
| Burnout – Depersonalization1,2 | 60 | 5.4 | 2.7 | 0.01 | 5.4 | 1.4 | 0.31 | 1 | 3.8 | 0.06 |
| Burnout – Personal Accomplishment2 | 54 | 7 | 2.8 | 0.008 | 7 | 0.7 | 0.71 | 1 | 6.7 | 0.01 |
1. Greenhouse Geiser corrected values used because sphericity assumption was violated.
2. Analyzed for nurses and other healthcare professionals only.
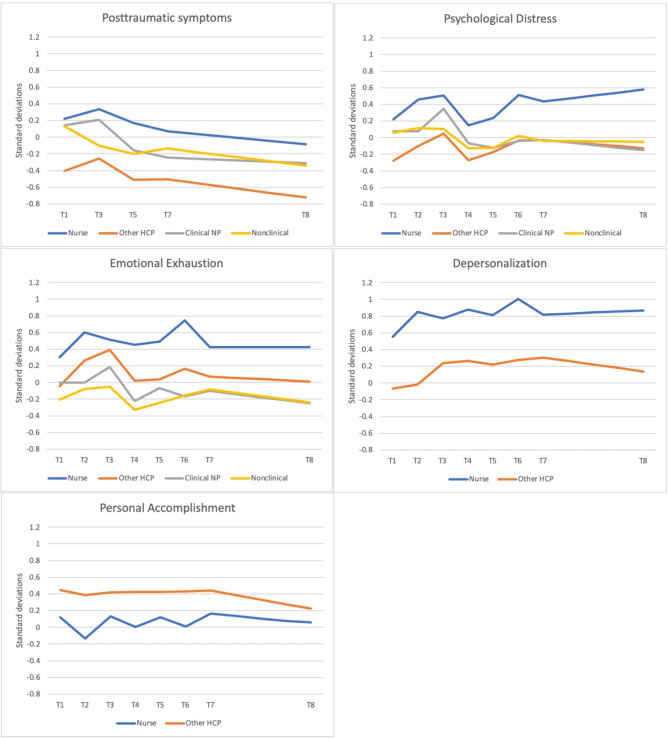
Changes in standardized variables over time by occupational group were plotted to visualize the differences identified in the repeated measures ANOVA (Fig. 1). These figures demonstrate that the most consistent difference between job types is that compared to other occupational groups, nurses were experiencing higher psychological distress, posttraumatic symptoms, emotional exhaustion, depersonalization, and less perceived personal accomplishment at all time points. Trends in changes over time differed by variable. Posttraumatic symptoms decreased over time after T3 (Spring 2021). Psychological distress and emotional exhaustion appear to have risen and fallen in a pattern that roughly corresponds that roughly corresponds to the rise and fall of local COVID-19 case rates, which peaked in January 2022 (near T6).
Fig. 1.
Trends in standardized psychological variables over time by occupational group.
When we tested whether the mean severity of these variables differed from the first measurement to the last (T1 to T8, Table 3) we found that over the period of study there was a significant increase in psychological distress and depersonalization and a significant decrease in perceived personal accomplishment. Emotional exhaustion, though it varied significantly over time (Table 2), did not differ significantly between the first and last measurement. Posttraumatic symptoms significantly declined over the time of the study. When we tested whether the mean severity of these variable differed over the final year of follow-up (T7 to T8, Table 3) we found that the only significant changes in this period were decreases in personal accomplishment and posttraumatic symptoms.
Table 3.
Changes in mental health variables from T1 to T8 and from T7 to T8.
| Difference T1 to T8 | Difference T7 to T8 | |||||||
|---|---|---|---|---|---|---|---|---|
| n | Mean | 95% CI | n | Mean | 95% CI | |||
| Lower | Upper | Lower | Upper | |||||
| Posttraumatic symptoms | 280 | − 0.27 | − 0.40 | − 0.15 | 268 | − 0.15 | − 0.26 | − 0.04 |
| Psychological Distress | 280 | 0.16 | 0.05 | 0.28 | 272 | 0.00 | − 0.10 | 0.11 |
| Emotional Exhaustion | 284 | 0.00 | − 0.11 | 0.11 | 267 | − 0.03 | − 0.12 | 0.06 |
| Personal Accomplishment | 72 | − 0.19 | − 0.28 | − 0.09 | 67 | − 0.15 | − 0.27 | − 0.03 |
| Depersonalization | 75 | 0.38 | 0.15 | 0.62 | 71 | − 0.05 | − 0.23 | 0.14 |
Units of means are standard deviations at T1.
Changes which are significantly different than zero are bolded.
HCP: healthcare professional, NP: non-professional, T1: Fall 2020, T2-T7: quarterly intervals to Spring 2022, T8: Spring 2023.
Units are in standard deviations (full cohort, T1), varying from 0 (full cohort mean at T1).
Discussion
This report advances previous studies of the impact of the COVID-19 pandemic on hospital-based health care workers by describing changes in several measures of mental health at intervals from the first year of the pandemic until shortly before it was declared over in 2023. We found that the pattern of change over time varied in different measures of mental health and that most measures of mental health were not improving in the year prior to the declaration of the end of the pandemic, even as the rate of hospitalized cases greatly decreased27.
For the emotional exhaustion dimension of burnout, from the first measurement in the Fall of 2020 (T1) to the seventh quarterly measurement in the Spring of 2022 (T7), the mean severity of emotional exhaustion tended to rise and fall in approximate synchrony with the rise and fall of case rates. However, in the following year there was no significant improvement in emotional exhaustion, despite declining cases of hospitalizations for COVID-19. From the perspectives of staff well-being and the ability of hospitals to recruit and retain healthcare professionals, it is a concern that emotional exhaustion did not decrease as case rates declined in the year leading up to the end of the pandemic. This suggests that case rates were not the most important determinant of late-pandemic emotional exhaustion. There are many potential contributors to emotional exhaustion at the levels of healthcare organizations and the broader healthcare system28. It is possible that rather than the acute stresses associated with case rates of COVID-19, emotional exhaustion later in the pandemic was driven by the chronic stresses of a depleted health care workforce22,23, and the accumulated impact of working through an extraordinarily stressful three-year period.
Psychological distress also tended to rise and fall in approximate synchrony with the rise and fall of case rates in the period between Fall of 2020 (T1) and the Spring of 2022 (T7). However, of concern, there was an overall increase in psychological distress over this period, and no significant decrease during the year prior to the pandemic being declared over (indeed the trend in nurses appears to be a further increase). Since psychological distress is comprised of depressive and anxiety symptoms and can be used as a screening test for possible cases of diagnosable depressive and anxiety disorders29, rising psychological distress over time may be due to the development of longer-term mental health problems in some hospital-based staff, perhaps secondary to the impact of chronic stress and exhaustion.
In contrast to the longitudinal patterns observed for emotional exhaustion and psychological distress, posttraumatic symptoms peaked in the first year of the pandemic and declined after that. The difference in trajectories for psychological distress and posttraumatic symptoms in the current study is consistent with a systematic review of long-term trajectories of mental health symptoms after disasters and pandemics, which found that posttraumatic symptoms tended to gradually improve while depression and anxiety symptoms remained stable over months and years30. This would suggest that, for most hospital workers in our cohort, working during the pandemic was not experienced as a psychological trauma after the pandemic’s first year. On the other hand, it is noteworthy that high posttraumatic symptoms at the first measurement point (T1) were found to predict subsequent drop-out from the cohort, so it is also possible that the improvement in posttraumatic symptoms over time in the cohort studied in this report (the subset of the initial cohort who did not drop out) is not representative of the whole cohort.
Two variables were measured only in healthcare professionals, depersonalization and diminished sense of personal accomplishment. As with all mental health variables tested, diminished sense of personal accomplishment varied significantly over time (Table 2). Overall, sense of personal accomplishment declined over the course of the study (T1 to T8) as well as declining significantly in the year prior to the pandemic’s end (T7 to T8).
Depersonalization increased overall over the course of the study and there was no significant improvement in the year before the pandemic’s end. It is noteworthy that in the context of professional burnout, depersonalization represents distancing emotionally from one’s work and from patients, adopting an attitude of indifference or callousness. This is similar to a pattern of “numbing of their moral sensitivity and a withdrawal from involvement in ethically challenging patient situations” combined with lack of feeling, which has been described as a response to repeated episodes of moral distress31—a common experience for hospital workers during the COVID-19 pandemic. We previously described a vicious circle in this cohort in which depersonalization amplifies the experience of moral distress, which in turn contributes to further subsequent depersonalization32. This finding provides support for attributing the rise in depersonalization over the course of the pandemic, in part, to repeated experiences of moral distress.
Overall, except for posttraumatic symptoms, we found that mental health symptoms did not improve in health care workers in this cohort in the final year before the declaration that the pandemic had ended, despite decreasing cases, relaxing of public health measures, and decreased public attention to healthcare workers. Moreover, trends toward overall increasing depersonalization, decreasing perceived personal satisfaction, increasing emotional exhaustion and increasing psychological distress are a cause for concern. Potential explanations for the persistent mental health impact of the pandemic for hospital-based workers are long-term depletion of individual-level coping resources because of extended extraordinary stress, persistent and potentially increasing occupational stress as a result of workforce depletion, and persistent tensions and moral distress in the workplace. These results support the need for interventions at the level of health care organizations and systems28 to support the well-being and resilience of healthcare workers, including the support of trainable skills to enhance resilience33,34 such as mentalizing capacities35.
It is a strength of this study that a cohort of hundreds of health care workers provided longitudinal data over 2.5 years in the context of the COVID-19 pandemic, and that these measurements extend into 2023, making this a unique dataset that provides a window onto the long-term impact of the pandemic for hospital workers. Weaknesses include the attrition of the cohort to 54% of its original size by the eighth measurement point, which while understandable in this context, nonetheless threatens the representativeness of the remaining cohort. It is noteworthy, however, that aside from PTSD symptoms at the first measurement point, few differences between those who dropped out and those who continued were found. The representativeness of the cohort that was assembled for the first measurement in the Fall of 2020 is also limited by the method of recruitment through advertising to all hospital staff rather than with a more targeted sampling strategy. It is possible that findings in a single hospital organization are not generalizable to other hospital organizations, but we argue that the known differences between this hospital and others, favour a bias towards better outcomes in the current hospital, if there is a bias. This suggestion is based on two possible differences between the site of this study and other hospitals. First, this hospital has achieved Magnet™ Recognition from the American Nurses Credentialing Center, the only hospital in Canada to have done so at the time of this study. Magnet™ hospitals have been found to have better work environments, more highly educated nurses, less job dissatisfaction, and less burnout than non-magnet hospitals36. Second, during the phases of pandemic in which some hospitals in Ontario were overwhelmed with COVID-19 patients requiring admission or intensive care, inter-hospital transfers were common. The hospital organization in this study was often a recipient of such patient transfers but rarely if ever a source of patients needing transfer. This indicates that this hospital was relatively less overwhelmed by COVID-19 admissions than other hospitals. Given these differences, it is possible that the long-terms trends found here are under-estimates of the impact of the pandemic on workers in other hospitals.
This study adds to the evidence that hospital-based healthcare workers have not recovered quickly from pandemic-related effects on mental health indices. Ongoing monitoring and support of the wellness of hospital-based healthcare workers is critical not only for individual well-being but also for the recruitment and retention of staff that is necessary for the well-being of the healthcare system.
Author contributions
Study conception: RGM; Data analysis: RGM, NDH; Data illustration: RGM, NDH; Interpretation of Results and Discussion: RGM, NDH, LPJ, LAW, JJH; First draft: RGM; Contribution to and approval of final draft: RGM, NDH, LPJ, LAW, JJH.
Funding
This work was funded by a CIHR Canadian 2019 Novel Coronavirus (COVID-19)nRapid Research Grant (FRN OV7 170642).
Data availability
De-identified data is available from the corresponding author on reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Williams, E. S., Rathert, C. & Buttigieg, S. C. The Personal and Professional consequences of Physician Burnout: a systematic review of the literature. Med. Care Res. Rev. 77 (5), 371–386 (2020). [DOI] [PubMed] [Google Scholar]
- 2.Dyrbye, L. N. et al. Burnout and suicidal ideation among U.S. medical students. Ann. Intern. Med. 149 (5), 334–341 (2008). [DOI] [PubMed] [Google Scholar]
- 3.Dewa, C. S., Loong, D., Bonato, S., Thanh, N. X. & Jacobs, P. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv. Res. 14 (1), 325 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bianchi, R., Schonfeld, I. S. & Laurent, E. Burnout-depression overlap: a review. Clin. Psychol. Rev. 36, 28–41 (2015). [DOI] [PubMed] [Google Scholar]
- 5.Dutheil, F. et al. Suicide among physicians and health-care workers: a systematic review and meta-analysis. PLoS One. 14 (12), e0226361 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dall’Ora, C. et al. Association of 12 h shifts and nurses’ job satisfaction, burnout and intention to leave: findings from a cross-sectional study of 12 European countries. BMJ Open. 5 (9), e008331 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grossman, Z. et al. Burnout and intentions to quit the practice among community pediatricians: associations with specific professional activities. Isr. J. Health Policy Res. ; 8(1). (2019). [DOI] [PMC free article] [PubMed]
- 8.Moloney, W., Boxall, P., Parsons, M. & Cheung, G. Factors predicting registered nurses’ intentions to leave their organization and profession: a job demands-resources framework. J. Adv. Nurs. 74 (4), 864–875 (2018). [DOI] [PubMed] [Google Scholar]
- 9.Heinen, M. M. et al. Nurses’ intention to leave their profession: a cross sectional observational study in 10 European countries. Int. J. Nurs. Stud. 50 (2), 174–184 (2013). [DOI] [PubMed] [Google Scholar]
- 10.Azam, K., Khan, A., Alam, M. T. & Toqeer, M. INTRODUCTION causes and adverse impact of Physician Burnout: a systematic review. J. Coll. Physicians Surg. Pakistan. 27 (8), 495–501 (2017). [PubMed] [Google Scholar]
- 11.HallLH, Johnson, J., Watt, I., Tsipa, A. & O’Connor, D. B. (ed Harris, F.) Healthcare Staff Wellbeing, Burnout, and Patient Safety: a systematic review. PLoS One. 11 7 e0159015 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Panagioti, M. et al. Association between Physician Burnout and Patient Safety, Professionalism, and patient satisfaction. JAMA Intern. Med. 178 (10), 1317 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 13.Shanafelt, T. D. et al. Burnout and medical errors among American surgeons. Ann. Surg. 251 (6), 995–1000 (2010). [DOI] [PubMed] [Google Scholar]
- 14.Ching, S. M. et al. Psychological distress among healthcare providers during COVID-19 in Asia: Systematic review and meta-analysis. PLoS One [Internet]. 2021 Oct 1 [cited 2023 Mar 19];16(10):e0257983. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0257983 [DOI] [PMC free article] [PubMed]
- 15.Blasco-Belled, A., Tejada-Gallardo, C., Fatsini-Prats, M. & Alsinet, C. Mental health among the general population and healthcare workers during the COVID-19 pandemic: A meta-analysis of well-being and psychological distress prevalence. Current Psychology [Internet]. 2022 Mar 1 [cited 2024 Apr 15];43(9):8435–46. https://link.springer.com/article/10.1007/s12144-022-02913-6 [DOI] [PMC free article] [PubMed]
- 16.Salazar de Pablo, G. et al. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. J. Affect. Disord. 275, 48–57 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fattori, A. et al. Long-Term Trajectory and Risk Factors of Healthcare Workers’ Mental Health during COVID-19 Pandemic: A 24 Month Longitudinal Cohort Study. Int J Environ Res Public Health [Internet]. 2023 Mar 1 [cited 2024 May 1];20(5):4586. https://www.mdpi.com/1660-4601/20/5/4586/htm [DOI] [PMC free article] [PubMed]
- 18.Leung, H. T., Lim, M., Lim, W. O., Lee, S. A. & Lee, J. Psychological well-being of healthcare workers during COVID-19 in a mental health institution. PLoS One [Internet]. 2024 Mar 1 [cited 2024 May 1];19(3):e0300329. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0300329 [DOI] [PMC free article] [PubMed]
- 19.Bellehsen, M. H. et al. Adapting the Stress First Aid Model for Frontline Healthcare Workers during COVID-19. International Journal of Environmental Research and Public Health 2024, Vol 21, Page 171 [Internet]. 2024 Feb 1 [cited 2024 May 1];21(2):171. https://www.mdpi.com/1660-4601/21/2/171/htm [DOI] [PMC free article] [PubMed]
- 20.Coronavirus Graphs. Worldwide Cases and Deaths - Worldometer [Internet]. [cited 2024 May 2]. https://www.worldometers.info/coronavirus/worldwide-graphs/#total-cases
- 21.WHO chief declares end to COVID. -19 as a global health emergency | UN News [Internet]. [cited 2024 May 2]. https://news.un.org/en/story/2023/05/1136367
- 22.Baumann, A. & Crea-Arsenio, M. The Crisis in the Nursing Labour Market: Canadian Policy Perspectives. Healthcare. Vol 11, Page 1954 [Internet]. 2023 Jul 6 [cited 2024 May 1];11(13):1954. (2023). https://www.mdpi.com/2227-9032/11/13/1954/htm [DOI] [PMC free article] [PubMed]
- 23.Looi, M. K. The European healthcare workforce crisis: how bad is it? BMJ [Internet]. Jan 19 [cited 2024 May 1];384. (2024). https://www.bmj.com/content/384/bmj.q8 [DOI] [PubMed]
- 24.Maunder, R. G. et al. Psychological impact of the COVID-19 pandemic on hospital workers over time: Relationship to occupational role, living with children and elders, and modifiable factors. Gen Hosp Psychiatry [Internet]. 2021/05/11. ;71:88–94. (2021). https://www.ncbi.nlm.nih.gov/pubmed/33971518 [DOI] [PMC free article] [PubMed]
- 25.Maunder, R. G. et al. Trends in burnout and psychological distress in hospital staff over 12 months of the COVID-19 pandemic: a prospective longitudinal survey. Journal of Occupational Medicine and Toxicology 2022 17:1 [Internet]. 2022 May 25 [cited 2022 Jul 26];17(1):1–11. https://occup-med.biomedcentral.com/articles/10.1186/s12995-022-00352-4 [DOI] [PMC free article] [PubMed]
- 26.Maunder, R. G. et al. Randomized trial of personalized psychological feedback from a longitudinal online survey and simultaneous evaluation of randomized stepped wedge availability of in-person peer support for hospital staff during the COVID-19 pandemic. Gen. Hosp. Psychiatry. 84, 31–38 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.COVID-19 epidemiology update. Current situation — Canada.ca [Internet]. [cited 2024 Jul 2]. https://health-infobase.canada.ca/covid-19/current-situation.html?stat=num&measure=deaths_weekly↦=pt#a2
- 28.Maunder, R. G. et al. Burnout in Hospital-Based Healthcare Workers during COVID-19. 2021 Oct 7 [cited 2021 Oct 24]; https://covid19-sciencetable.ca/sciencebrief/burnout-in-hospital-based-healthcare-workers-during-covid-19
- 29.Kessler, R. C., Andrews, G., Colpe, L. J. & Mroczek, D. K. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. [cited 2021 Nov 4]; (2002). https://www.researchgate.net/publication/11174017 [DOI] [PubMed]
- 30.Newnham, E. A. et al. Long term mental health trajectories after disasters and pandemics: a multilingual systematic review of prevalence, risk and protective factors. Clin. Psychol. Rev. 97, 102203 (2022). [DOI] [PubMed] [Google Scholar]
- 31.Epstein, E. G. & Hamric, A. B. Moral distress, moral residue, and the crescendo effect [Internet]. 2009 [cited 2022 Nov 29]. https://philpapers.org/rec/EPSMDM [PubMed]
- 32.Maunder, R. G. et al. The relationship between moral distress, burnout, and considering leaving a hospital job during the COVID-19 pandemic: a longitudinal survey. BMC Nurs [Internet]. 2023 Dec 1 [cited 2024 Jul 2];22(1):1–10. https://link.springer.com/articles/10.1186/s12912-023-01407-5 [DOI] [PMC free article] [PubMed]
- 33.Winwood, P. C., Colon, R. & McEwen, K. A practical measure of workplace resilience: developing the resilience at work scale. J Occup Environ Med [Internet]. 2013;55(10):1205–12. (2013). /09/26 https://www.ncbi.nlm.nih.gov/pubmed/24064782 [DOI] [PubMed]
- 34.Maunder, R. G. et al. Relationship between three aspects of resilience—adaptive characteristics, withstanding stress, and bouncing back—in hospital workers exposed to prolonged occupational stress during the COVID-19 pandemic: a longitudinal study. BMC Health Serv Res [Internet]. 2023 Dec 1 [cited 2024 Oct 17];23(1):1–11. https://link.springer.com/article/10.1186/s12913-023-09731-x [DOI] [PMC free article] [PubMed]
- 35.Safiye, T. et al. Mentalizing, Resilience, and Mental Health Status among Healthcare Workers during the COVID-19 Pandemic: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. Vol 20, Page 5594 [Internet]. 2023 Apr 20 [cited 2024 Oct 17];20(8):5594. (2023). https://www.mdpi.com/1660-4601/20/8/5594/htm [DOI] [PMC free article] [PubMed]
- 36.Kelly, L. A., McHugh, M. D. & Aiken, L. H. Nurse outcomes in magnet® and non-magnet hospitals. Journal of Nursing Administration [Internet]. 2011 Oct [cited 2024 Jul 2];41(10):428–33. https://journals.lww.com/jonajournal/fulltext/2011/10000/nurse_outcomes_in_magnet__and_non_magnet_hospitals.9.aspx [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
De-identified data is available from the corresponding author on reasonable request.