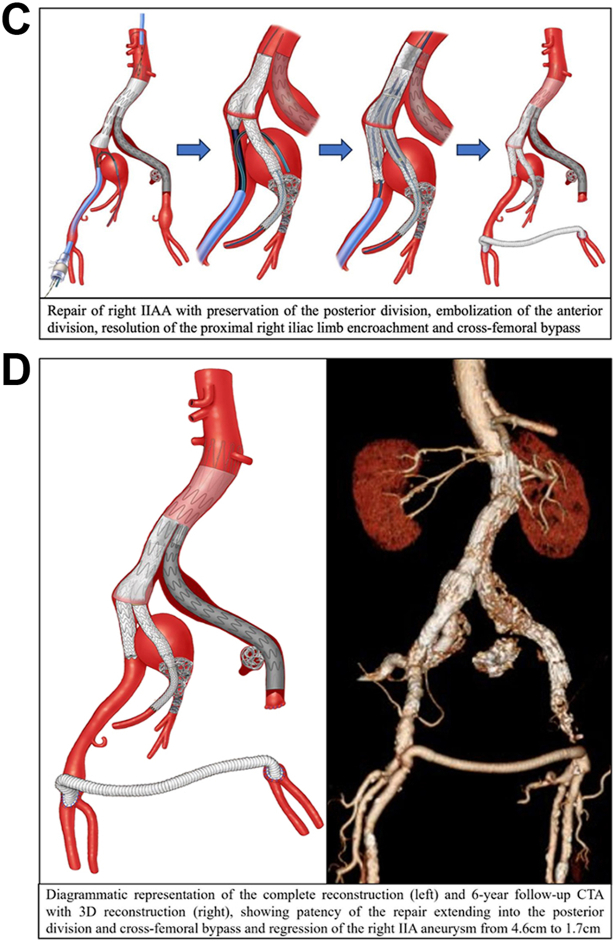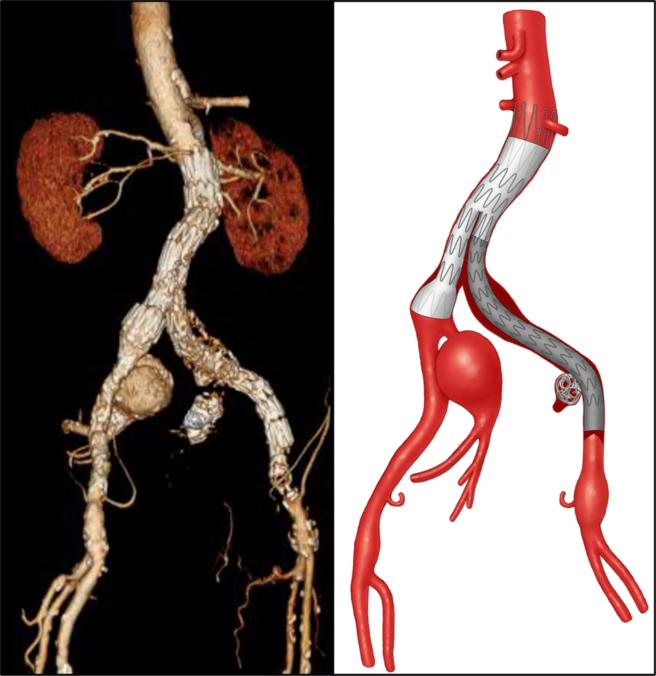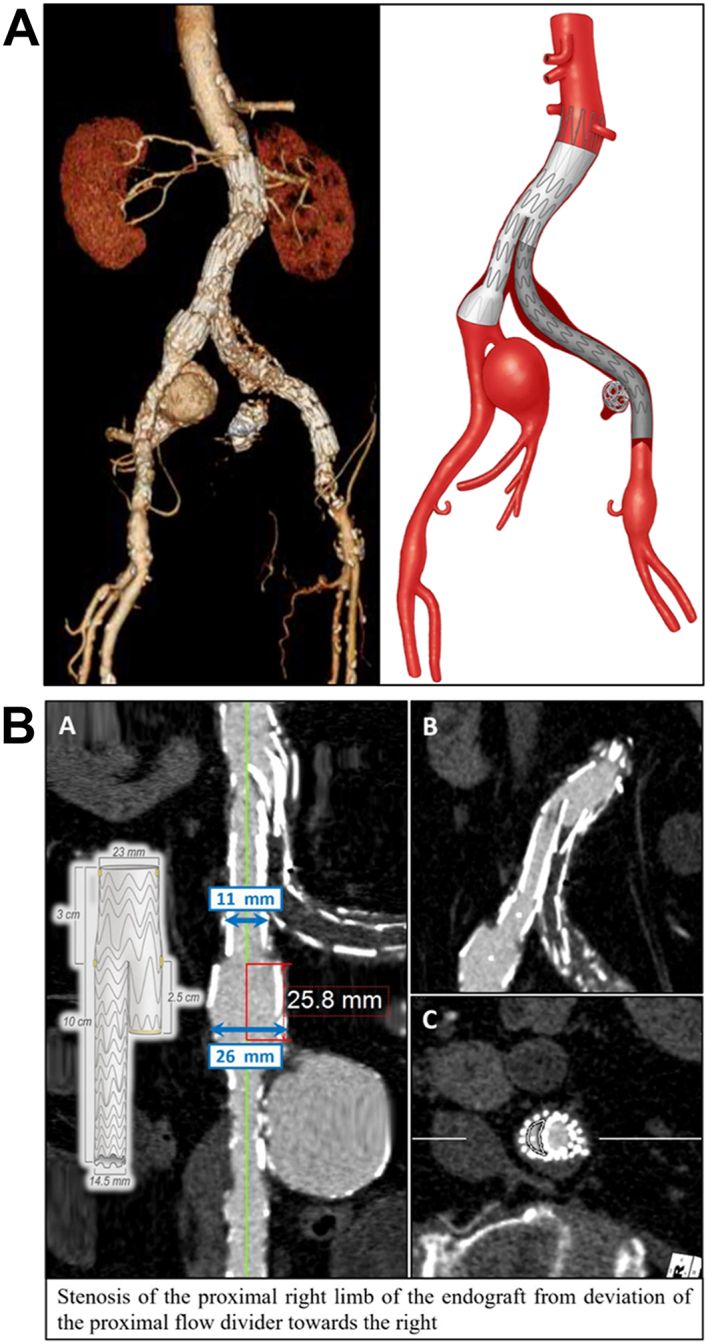
An 83-year-old man with multiple cardiovascular comorbidities presented in clinic with short-distance left calf claudication and toe ulceration 6 weeks after transurethral prostate resection for benign prostatic hyperplasia. He had a history of abdominal aortic aneurysm open repair with a tube graft 21 years previously and endovascular aneurysm repair with a Zenith endograft (Cook Medical) for a 6.4-cm left common iliac artery aneurysm with coil embolization of a 3-cm left internal iliac artery (IIA) aneurysm (IIAA) 8 years prior. Lower extremity pulses were absent on the left (ankle brachial index [ABI], 0.38) and palpable on the right (ABI, 0.99). Computed tomography angiography revealed occlusion of the endograft left limb and external iliac artery, a 4.6-cm right IIAA, and a 2-cm left common femoral artery aneurysm (A/Cover). Bilateral infrainguinal runoff was patent. The flow divider encroached on the proximal right limb, causing stenosis (B). Under general anesthesia, through a 22F right femoral sheath and left brachial cutdown, through-and-through access was obtained. The 11-mm segment of the endograft right limb was ballooned to 18 mm, and a 23-mm by 14.5-mm by 10-cm Gore iliac branch endoprosthesis (IBE; W.L. Gore & Associates) was introduced and deployed. The reconstruction was extended from the brachial access into the IIA posterior division using a 9-mm by 10-cm Viabahn stent (W.L. Gore & Associates) and a 13-mm IBE internal iliac limb as bridging stents. Coaxially, a 5F sheath was introduced into the right IIA anterior division, two 8-mm Amplatzer plugs (Abbott Cardiovascular) and coils were placed distally to occlude the anterior division branches, and the reconstruction was completed from the arm. The IBE external iliac component was deployed, followed by kissing balloon angioplasty. Two 10 by 38-mm iCast stents (Getinge) were placed in the stenosed proximal right limb and postdilated to 14 mm. Cone-beam computed tomography confirmed technical success. Finally, right-to-left femoral–femoral bypass was performed with 8-mm Dacron, excluding the left common femoral artery aneurysm (C). The procedural duration was 390 minutes and required 1.37 Gy of radiation. His postoperative course was uneventful, the left ABI normalized (ABI, 0.97), and his symptoms resolved. After 6 years, the patient is asymptomatic, with a patent reconstruction and right IIAA shrinkage (D). He provided written informed consent for publication. This case demonstrates long-term patency of an IBE placed within a previous endovascular aneurysm repair limb to preserve IIA flow1,2 in the setting of an occluded Zenith endograft limb.3
Disclosures
None.
Footnotes
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
Appendix
Cover image.
References
- 1.D'Oria M., Mastrorilli D., DeMartino R., Lepidi S. Current status of endovascular preservation of the internal iliac artery with iliac branch devices (IBD) Cardiovasc Intervent Radiol. 2019;42:935–948. doi: 10.1007/s00270-019-02199-5. [DOI] [PubMed] [Google Scholar]
- 2.Wang S.K., Miladore J.N., Yee E.J., Liao J.L., Donde N.N., Motaganahalli R.L. Combined transbrachial and transfemoral strategy to deploy an iliac branch endoprosthesis in the setting of a pre-existing endovascular aortic aneurysm repair. J Vasc Surg Cases Innov Tech. 2019;5:305–309. doi: 10.1016/j.jvscit.2019.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Urlings T.A., de Vries A.C., de Mol van Otterloo J.C., Eefting D., van der Linden E. Thromboembolic complications after Zenith® low profile endovascular graft for infrarenal abdominal aneurysms. Cardiovasc Intervent Radiol. 2015;38:600–605. doi: 10.1007/s00270-014-0972-4. [DOI] [PubMed] [Google Scholar]