Abstract
Objective: Previous studies suggest older patients with multiple health conditions and medications may experience adverse interactions, leading to negative outcomes. However, there’s limited research on this in older adults receiving home medical care. This study assesses whether polypharmacy is linked to falls or other clinical outcomes. Methods: The study population included 217 participants, aged ≥65 years, receiving home medical care, who consented to participate in the Osaka Home Care Registry (OHCARE) study in Japan. The survey examined the association between polypharmacy and clinical outcomes. We defined “polypharmacy” as six or more medications taken regularly. Results: Of the participants, 135 (62.6%) had polypharmacy and were significantly more likely to have hypertension or diabetes. Common medications included those for hypertension, diabetes, and mental disorders. Participants with polypharmacy experienced significantly more falls. Multivariate analysis showed an association between polypharmacy and falls (odds ratio: 2.81, 95% confidence interval [1.34, 5.92]). Conclusion: Even in older patients receiving home health care, the use of six or more medications poses a risk of falls. Careful observations and life support by medical stuffs are necessary to prevent falls in older patients with polypharmacy receiving home medical care.
Keywords: home medical care, older patients, polypharmacy, falls
Introduction
The population in Japan is rapidly aging. Japan has the highest rates of aging and declining birthrate in the world and is a leading super-aged society. Therefore, a community-based comprehensive care system (Kamide et al., 2021) is vital to create an environment where older people can live in their homes and familiar neighborhoods and receive home medical care with peace of mind without having to be hospitalized or admitted to an institution.
Older patients receiving home medical care often have multiple illnesses, each of which is often severe, and therefore tend to regularly take six or more medications at the same time (or polypharmacy). Home medical care older patients may have different medical and activities of daily living (ADL) characteristics from older patients in inpatient and outpatient settings. About half of the patients receiving home medical care do so because their declining physical functions, or they are unable to visit the hospital due to limited ADL levels (Ministry of Health, Labour and Welfare, 2015). In comparison to inpatients, where medical care is close at hand, home medical care does not always allow for older patients to receive immediate care from their visiting medical team to address sudden changes (e.g., heart failure, stroke) to a patient’s condition in their home. But little research has been conducted about how adverse medication use at home and limitations to their care may lead to negative health outcomes. For these reasons, it is critical to address this gap and build the evidence for improving these issues facing older patients receiving home medical care.
Compared with younger people, older people are more likely to have persistent chronic conditions such as hypertension, diabetes, and bone and joint diseases. Because they have multiple comorbidities, they are more likely to have polypharmacy or regularly take six or more medications due in part to having to regularly visit multiple healthcare facilities for their health conditions and receiving different treatment or prescriptions from each facility they visit (Kozono et al., 2016). Older people are also more prone to adverse drug events from polypharmacy due to having decreased systemic physiological functions from aging, and physiological dysfunctions becoming more pronounced upon the interaction with a wide variety of drugs (Akishita, 2018).
It is a major concern that many adverse drug events are associated with polypharmacy among older people in the community (Akishita, 2018), but polypharmacy should not necessarily be regarded as negative. For some old people, polypharmacy is essential, such as those with numerous comorbidities. However, it may be important to avoid negative drug interactions from multidrug use. There is a growing need to build further evidence about polypharmacy and examine the strategies needed to avoid negative drug interactions or unnecessary medication use.
Concerning the few prior studies on polypharmacy and in-hospital events clinical outcomes, the following findings have been reported: increased risk of falls in older outpatients (Kojima et al., 2011, 2012; Masumoto et al., 2018; Trevisan et al., 2017) or inpatients (Kozono et al., 2016; Li et al., 2022), hospitalization in older patients (Shin et al., 2020), increased incidence of adverse events in acute care hospitalized older patients (Nobili et al., 2011), prolonged length of stay and increased risk of in-patient mortality in hospitalized older patients (Nobili et al., 2011) in other countries. There are also previous studies assessing the association between polypharmacy and falls in the general community and in institutional residents (Dhalwani et al., 2017; Kayyali et al., 2020; Müller et al., 2020). In older patients receiving home medical care, previous studies have examined the factors associated with polypharmacy (Komiya et al., 2017) and inappropriate prescribing (Huang et al., 2019). However, no studies based on objective data from medical records have analyzed the association between polypharmacy and various clinical outcomes (falls, hospitalizations, and deaths) in older patients receiving home medical care. Therefore, there is a major research gap in understanding the impact of polypharmacy on those older people receiving home medical care. In home medical care, the visiting doctor or pharmacist is responsible for administering medications. However, in home medical care settings, there are many patients with polypharmacy due to their multimorbidity.
In public health, falls in older people have long been considered problematic because of the complex factors involved (Tinetti et al., 1988). There have been systematic reviews of fall risk (Ambrose et al., 2013; Ganz et al., 2007). Therefore, the purpose of this study was to address whether polypharmacy further increase the risk of falls in home medical care settings where many patients were in a state of physical frailty or mental and neurological frailty. It was to find out.
Methods
Study Participants
The Osaka Home Care Registry (OHCARE) study is an ongoing prospective cohort study involving older patients receiving home medical care in nine home medical care clinics of Osaka and Hyogo Prefectures in Western Japan. The OHCARE study aims to investigate factors associated with prognosis and functional decline among older patients receiving home medical care and to establish evidence-based home medical care (Koujiya et al., 2020; Murakami et al., 2024; Yamamoto et al., 2019). The study started in January 2015, and we collected and analyzed information from medical records and visiting nurse records every 6 months to 1 year. The study was conducted in January 2015 and is still entering study enrollees, and the participants have been followed up every 6 months to a year since they entered the study.
At each collaborating institution, participants receiving home medical care were briefed on the study by a physician at the collaborating institution. Participants were assigned as research subjects if they provided written consent to participate in the study, either by themselves or by proxies. Information on the research participants collected at each collaborating institution was anonymized and entered into an electronic file for information collection and accumulation. This study was approved by the relevant institutional review boards (14498(310)-5).
Of the 327 participants enrolled in the study, we excluded 18 individuals who were under 65 years old and 92 individuals who could not be followed up for 1 year, resulting in an analysis cohort of 217 participants. The study population included 217 Japanese patients aged ≥65 years who were followed for 1 year. The follow-up period was set to 1 year to avoid the influence of changes in prescriptions. A longitudinal analysis was conducted by dividing patients into two groups with or without polypharmacy. The follow-up period was set at 1 year to account for changes in prescriptions.
Data and Collection
Basic information, laboratory data, nursing and care data, and emergency events were collected from the subject’s medical records, attending physician opinion forms, medical information forms, and home nursing records. Investigators with registered nurse or public health nurse licenses visited each collaborating institution and conducted surveys. Regarding information with unknown details, we interviewed the attending physicians and nurses at each research partner institution.
Measurements
Operative Definition of the Term “Polypharmacy”
In Japan, receiving six or more regular oral medications is often defined as polypharmacy (Akishita, 2018), and in a previous study in Japan that investigated the association between the number of medications and adverse events in older hospitalized patients, the frequency of adverse drug events was particularly increased with six or more medications (Japan Medical Association, 2017; Kojima, 2019; The Japan Geriatrics Society, 2015). Based on these findings, we used “more than six regular oral medications” as the operative definition of “polypharmacy” in this study. In addition, external medications (e.g., poultices and inhalers) and injectable medications (e.g., insulin) were excluded, and compounded tablets were counted and analyzed by type of medication. As for how many oral medications are defined as polypharmacy, reports differ, and previous studies analyzing the concept of polypharmacy in older people have shown that multidrug use varies from four or more to 10 or more (Ishizumi & Tsukamoto, 2017; Mortazavi et al., 2016).
Operative Definition of the Term “Clinical Outcomes”
The primary outcome of this study was new clinical outcomes during the follow-up period, defined as follows: new falling events including all falls during the follow-up period after the initial survey regardless of the presence or absence or degree of injury caused by the fall, hospitalization including general or emergency admission excluding respite care for the convenience of the caregiver, and not necessarily fractures or deterioration of the patient’s condition; and death between the baseline and follow-up survey. Hospitalization history at baseline was defined as hospital admissions occurring within 5 years prior to the baseline survey. This criterion was chosen because hospitalizations from several decades ago may not accurately reflect the current health status of participants due to significant changes over time.
Statistical Analysis
Basic information were collected from the medical records of the study subjects, and basic attributes were classified by comparing the two groups with or without polypharmacy. For comparisons between the two groups for categorical variables, the χ2 test and Fisher’s exact establishment test were used, and the Mann–Whitney U test for non-normal distribution was employed for comparisons between two continuous variables. From there, the χ2 test was used to assess the association between polypharmacy and clinical outcomes, and logistic regression analysis was calculated to analyze factors associated with falls. All analyses were performed with SPSS version 25.0.
Results
At the end of March 2022, 217 subjects in the OHCARE study who were aged ≥65 years and for whom information on clinical outcomes could be collected were included in the present analysis. The median follow-up period was 374 days (range: 329–440 days). 62.6% of the participants received polypharmacy. The basic characteristics of the study subjects classified with or without polypharmacy are shown (Table 1). The median age of all subjects was over 85 years, and 56 (25.8%) were over 90 years old. There were significantly more subjects with hypertension and diabetes in the group with polypharmacy than in the group without polypharmacy.
Table 1.
Participants’ Baseline Characteristics With or Without Polypharmacy.
| Indicators | All participants n = 217 | Participants with polypharmacy n = 135 | Participants without polypharmacy n = 82 | p |
|---|---|---|---|---|
| Age | 85 (78–89) | 85 (78–89) | 87 (80–90) | .131 |
| Gender | ||||
| Female | 132 (60.8) | 82 (60.7) | 50 (61.0) | .973 |
| Disease | ||||
| Hypertension | 158 (72.8) | 106 (78.5) | 52 (63.4) | .015 |
| Diabetes mellitus | 49 (22.6) | 40 (29.6) | 9 (11.0) | .001 |
| Dyslipidemia | 77 (35.5) | 50 (37.0) | 27 (32.9) | .540 |
| Cancer | 51 (23.5) | 31 (23.0) | 20 (24.4) | .810 |
| Dementia | 64 (29.5) | 35 (25.9) | 29 (35.4) | .139 |
| Cerebrovascular disease | 65 (30.0) | 38 (28.1) | 27 (32.9) | .456 |
| Cardiac disease (excluding hypertension) | 114 (52.5) | 76 (56.3) | 38 (46.3) | .154 |
| Respiratory disease | 72 (33.2) | 49 (36.3) | 23 (28.0) | .211 |
| Locomotor system disease | 119 (54.8) | 74 (54.8) | 45 (54.9) | .993 |
| Gastrointestinal disease | 118 (54.4) | 73 (54.1) | 45 (54.9) | .908 |
| Renal urinary disease | 42 (19.4) | 29 (21.5) | 13 (15.9) | .309 |
| Residential structure | ||||
| Living with family | 124 (57.1) | 71 (52.6) | 53 (64.6) | |
| Living alone | 40 (18.4) | 30 (22.2) | 10 (12.2) | .151 |
| Residential facility | 37 (17.1) | 22 (16.3) | 15 (18.3) | |
| Care need level | ||||
| Severe (needs nursing care 3 times or more) | 110 (50.7) | 66 (48.9) | 44 (53.7) | .537 |
| Bedridden † | ||||
| Severe (Rank B or higher) | 100 (46.1) | 61 (45.2) | 39 (47.6) | .660 |
| Dementia independence | ||||
| Severe (Rank III or higher) | 57 (26.3) | 32 (23.7) | 25 (30.5) | .542 |
| Social support | ||||
| Frequency of Home medical + care | ||||
| Less than 1 time/month | 38 (17.5) | 21 (15.6) | 17 (20.7) | .152 |
| 2 times/month | 124 (57.1) | 84 (62.2) | 40 (48.8) | |
| More than 3 times/month | 55 (25.3) | 30 (22.2) | 25 (30.5) | |
| Home nursing care | 120 (55.3) | 80 (59.3) | 40 (48.8) | .132 |
| Home care | 78 (35.9) | 54 (40.0) | 24 (29.3) | .192 |
| Laboratory data | ||||
| Nutritional status | ||||
| TP (g/dL) | 6.8 (6.4–7.3) | 6.8 (6.4–7.4) | 6.6 (6.4–7.3) | .537 |
| Alb (g/dL) | 3.7 (3.4–4.1) | 3.7 (3.4–4.1) | 3.6 (3.3–4.1) | .456 |
| Hb (g/dL) | 12.1 (11.2–13.3) | 12.0 (11.1–13.3) | 12.3 (11.2–13.3) | .464 |
| Renal function | ||||
| Cr (mg/dL) | 0.77 (0.59–1.00) | 0.80 (0.63–1.07) | 0.68 (0.56–0.96) | .065 |
| eGFR (mL/min/1.73 m2) | 61.3 (43.8–81.1) | 57.9 (42.1–73.4) | 66.9 (48.9–87.0) | .045 |
| Liver function | ||||
| AST (IU/L) | 20 (16–25) | 21 (16–25) | 20 (16–26) | .960 |
| ALT (IU/L) | 12 (9–19) | 12 (8–18) | 12 (9–19) | .692 |
| γ-GTP (IU/L) | 21 (13–32) | 23 (14–31) | 18 (12–33) | .235 |
| Blood pressure | ||||
| sBP (mmHg) | 122 (112–135) | 122 (114–135) | 123 (110–135) | .487 |
| dBP (mmHg) | 70 (60–76) | 70 (60–74) | 70 (60–78) | .801 |
Note. Continuous variables are expressed as the median (interquartile range). Categorical variables are expressed as the number (%). χ2 test, Fisher’s exact test (two-sided test), Mann–Whitney U test. sBP = systolic blood pressure; dBP = diastolic blood pressure.
Bedridden degree: the degree of independent living for older adults and the disabled.
The types of medications that were significantly more common in the group with polypharmacy than in the group without polypharmacy included antihypertensives, antidiabetic agents, dyslipidemia agents, hypnotics and anxiolytics, anti-thrombotic agents, cardiovascular agents (excluding antihypertensives), digestive enzymes, and urology and chronic renal failure agents (Table 2).
Table 2.
Participants’ Regular Oral Medication at Baseline.
| Indicators | All participants n = 217 | Participants with polypharmacy n = 135 | Participants without polypharmacy n = 82 | p |
|---|---|---|---|---|
| Number of types | 6 (5–9) | 8 (7–11) | 4 (3–5) | <.001 |
| Types of oral medications | ||||
| Antihypertensive | 138 (63.6) | 100 (72.5) | 38 (27.5) | <.001 |
| Antidiabetic agent | 32 (14.7) | 28 (20.7) | 4 (4.9) | .001 |
| Dyslipidemia agent | 38 (17.5) | 30 (22.2) | 8 (9.8) | .019 |
| Drowsy/anxiolytic medications | 62 (28.6) | 49 (36.3) | 13 (15.9) | .001 |
| Dementia medication | 27 (12.4) | 16 (11.9) | 11 (13.4) | .735 |
| Anti-thrombotic agent | 80 (36.9) | 58 (43.0) | 22 (26.8) | .017 |
| Cardiovascular agent (excluding antihypertensive) | 25 (11.5) | 21 (15.6) | 4 (4.9) | .017 |
| Digestive enzyme | 175 (80.6) | 116 (85.9) | 59 (72.0) | .012 |
| Respiratory active agent | 42 (19.4) | 31 (23.0) | 11 (13.4) | .084 |
| Antipyretic analgesic | 36 (16.6) | 26 (19.3) | 10 (12.2) | .175 |
| Urology/chronic renal failure agent | 25 (11.5) | 22 (16.3) | 3 (3.7) | .005 |
Note. Continuous variables are expressed as the median (interquartile range). Categorical variables are expressed as the number (%). Mann–Whitney U test, χ2 test, Fisher’s exact establishment test.
The polypharmacy group had a significantly more frequent incidence of falls during the follow-up survey than the group without polypharmacy. In the group with polypharmacy, 10 of 46 subjects (21.7%) with falls during the follow-up period were 90 years of age or older. In the group without polypharmacy, 6 of 13 subjects (46.1%) who fell were 90 years of age or older. No significant correlation was noted between hospitalization and death in the two groups (Table 3).
Table 3.
Association Between Polypharmacy and Clinical Outcomes (Falls, Hospitalizations, and Deaths).
| Indicators | All participants n = 217 | Participants with polypharmacy n = 135 | Participants without polypharmacy n = 82 | p |
|---|---|---|---|---|
| Baseline | ||||
| Falls (in the past) | 63 (29.0) | 43 (31.9) | 20 (24.4) | 0.240 |
| Hospitalizations (in the past) | 60 (27.6) | 36 (26.7) | 24 (29.3) | 0.678 |
| Deaths | — | — | — | — |
| Follow-up | ||||
| Falls | 59 (27.2) | 46 (34.1) | 13 (15.9) | 0.003 |
| Hospitalizations | 163 (75.1) | 97 (71.9) | 66 (80.5) | 0.154 |
| Deaths | 12 (5.5) | 8 (5.9) | 4 (4.9) | 0.743 |
Note. Data are expressed as the number (%). χ2 test.
Logistic regression analysis was performed to examine factors associated with falls. Univariate analysis was performed with polypharmacy, antihypertensives, antidiabetic agents, hypnotics, and anxiolytic agents as independent variables, and occurrence of falls as a dependent variable. The results were significantly correlated with polypharmacy (odds ratio: 2.74, 95% confidence interval [1.37, 5.48]). Next, a multivariate analysis of these results showed a negative association in the presence of polypharmacy (odds ratio: 2.81, 95% confidence interval [1.34, 5.92]; Table 4).
Table 4.
Relative Risk of Falls.
| Risk factor (reference) | Univariate odds ratio [95% CI] | p | Multivariate odds ratio [95% CI] | p |
|---|---|---|---|---|
| Polypharmacy (ref: none) | 2.74 [1.37, 5.48] | .004 | 2.81 [1.34, 5.92] | .006 |
| Antihypertensive (ref: none) | 0.63 [0.33, 1.20] | .157 | 0.81 [0.41, 1.61] | .553 |
| Antidiabetic agent (ref: none) | 0.67 [0.30, 1.49] | .325 | 0.93 [0.40, 2.14] | .858 |
| Hypnotics and anxiolytics (ref: none) | 1.24 [0.63, 2.45] | .531 | 1.57 [0.77, 3.18] | .213 |
Note. Logistic regression analysis.
In addition, a breakdown of 59 subjects with falls in the follow-up survey showed that about half of the subjects with new falls took 6 to 10 oral medications (Figure 1).
Figure 1.
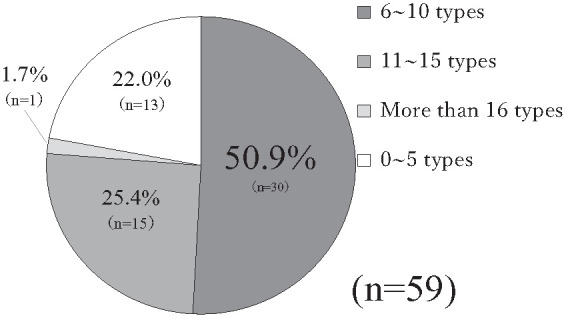
Number of types of oral medications among subjects with falls.
Discussion
This study examined the association between multiple drug use and clinical outcomes in older patients receiving home medical care. Although several studies examined the adverse effects of multiple drug use in older outpatients (Kojima et al., 2011, 2012; Masumoto et al., 2018; Trevisan et al., 2017), inpatients (Kozono et al., 2016; Li et al., 2022; Nobili et al., 2011), and community-dwelling older people (Dhalwani et al., 2017; Kayyali et al., 2020; Müller et al., 2020), very few studies focused on older patients receiving home medical care. Compared to the previous study on home medical care (Huang et al., 2019; Komiya et al., 2017), the present study included older more older subjects, including many in their 90s. In Japan, older adults who are certified as requiring long-term care are assessed based on their physical and cognitive functions, which may decline due to disease or aging. They are also evaluated for mental health issues such as depression. Consequently, older adults with long-term care certification are inherently at risk of falls. In this study, about half of the patients in both groups had severe care need levels. As a detail, half of older patients receiving home medical care have a long-term care level of 3 or higher, making them a particularly high-risk group for falls and a suitable subject for analysis. Therefore, this study may be very important, as it provides new findings on multidrug use in home medical care.
Concerning the basic attributes of the subjects at the time of the initial survey regarding diseases, the prevalence of multiple medications in subjects with hypertension and/or diabetes was more common than in subjects without such lifestyle-related diseases (Table 1). It was considered that multiple medications might be prescribed to achieve good control of lifestyle-related diseases such as hypertension and/or diabetes, resulted in polypharmacy (Japan Medical Association, 2017; The Japan Geriatrics Society, 2015).
Regarding the type of medications, antihypertensive, hypoglycemic, and drowsy/anxiolytic medications were significantly more common among those with multiple medications in patients with polypharmacy than in patients without it (Table 2). This could be a possible reason related to the result of more falls in those with multiple medications (Moon & Mikami, 2009; The Japan Geriatrics Society, 2015; Woolcott et al., 2009) because antihypertensive medications cause hypotension, hypoglycemic medications might cause hypoglycemia, and hypnotic and anxiolytic medications might cause drowsiness. No significant associations were found for diseases other than hypertension and diabetes. Even though there were no significant differences other than these two lifestyle-related diseases, subjects in the group with polypharmacy were taking more different types of oral medications than in the group without polypharmacy (Table 2). Drugs for hypertension and/or diabetes may cause the fall in home medical care. In addition, median age in the group without polypharmacy was significantly older (Table 1). Since higher age is one of strong risk for the fall (Tinetti et al., 1988), number of falls in patients with polypharmacy may be more common than in patients without polypharmacy. Another possibility of this result is that visiting physicians reduced or adjusted medications for the older subjects in home medical care. Therefore, the avoidance of polypharmacy may have resulted in fewer falls in the group without polypharmacy.
Only falls were associated with the results with or without polypharmacy in this study. The results were similar to previous studies regarding the association between polypharmacy and falls (Berdot et al., 2009; Dhalwani et al., 2017; Kayyali et al., 2020; Kojima et al., 2011, 2012; Li et al., 2022; Masumoto et al., 2018; Morita et al., 2014; Müller et al., 2020; Trevisan et al., 2017). Previous studies (Berdot et al., 2009; Moon & Mikami, 2009; Woolcott et al., 2009) and Japanese guidelines (Japan Medical Association, 2017; The Japan Geriatrics Society, 2015) have pointed to the risk of falls associated with drowsy/anxiolytic, antihypertensive, and hypoglycemic drugs, which older patients commonly take. In the case of drowsy / anxiolytic drugs, the risk of falls has been reported not only for benzodiazepines, but also for non-benzodiazepines. In addition, in the Guidelines for Safe Pharmacotherapy in the Elderly 2015 (The Japan Geriatrics Society, 2015), nonbenzodiazepines are also listed as drugs that should be administered with particular caution because they are primarily intended for frail older patients aged ≥ 75.
Furthermore, in home medical care, an association between benzodiazepine sleeping pills and anxiolytics and falls in homebound older patients has been reported. With regard to antidiabetic agents, previous studies reported that aging and hypoglycemia are associated with an increased risk of falls (Moon & Mikami, 2009), and in relation to antihypertensive agents, a history of hypertension has also been reported as a risk factor for falls among older people living in the community (Woolcott et al., 2009). In the present study, almost all drugs, including drowsy / anxiolytic medications, antihypertensive medications, and antidiabetic agents, were prescribed more frequently in the polypharmacy group, and it is possible that the effects of these drugs led to fall-related events (Table 2).
However, as independent variables, logistic regression analysis was performed with variables that could increase the risk of falls. In both uni- and multivariate analyses, neither drowsy/anxiolytics, antihypertensive medications, nor antidiabetic agents showed any association. This suggests that the risk of falling is not increased by taking drowsy/anxiolytics, antihypertensive agents, or antidiabetic agents, but rather by taking a variety of medications, that is, multiple medications, in older patients receiving home medical care (Table 2).
Two factors were considered responsible for the fact that falls were the only event related to polypharmacy in this study: low nutritional status and poor physical function. About half of the subjects in this study needed marked nursing care and had advanced malnutrition and physical function decline. Although there was no difference in background disease between patients with or without polypharmacy, it is possible that the patients with polypharmacy were more severely ill. Their malnutrition and physical deterioration were likely to be more advanced. However, clinical information on these factors is difficult to collect. This should be examined in detail using nutrition-related index data (height and weight for calculating BMI) and motor function indices (objective indices such as muscle mass and balance function), which are not easily measured or implemented in home medical health care settings. However, we believe that this difficulty limits our ability to identify the cause of the disease. Previous studies in other countries reported that frailty is a risk factor for adverse health outcomes such as falls in old age, hospitalization, and admission requiring long-term care, disability, and death (Fried et al., 2001; Woods et al., 2005).
In this study, six or more regular medications were defined as polypharmacy. Still, it is possible that a larger number of medications may further increase the risk of falls or that characteristics of medications may influence falls. We need to analyze how many oral medications increase the risk of falls and to analyze each detailed type of oral medication (e.g., antihypertensive, antidiabetic agent, hypnotics, and anxiolytic, etc.) to elucidate new indicators of multidrug use related to the risk of falls.
We need to continue our analysis to establish a definition of multidrug use, focusing on each type of disease. For example, many older patients with coronary artery disease after stenting take two anticoagulants and have hypertension, dyslipidemia, or diabetes as pre-existing conditions. It is difficult to avoid the use of multiple drugs for such patients. However, a previous study reported that in patients with cardiovascular disease, polypharmacy is not necessarily relevant, and that there is no association between cardiovascular disease and vascular risk factor-controlled drugs and death (Mortazavi et al., 2016).
Finally, drug interactions are a problem in polypharmacy, and many previous studies (Dhalwani et al., 2017; Kojima et al., 2011, 2012; Mortazavi et al., 2016) and some guidelines (Japan Medical Association, 2017; The Japan Geriatrics Society, 2015) have noted drug adverse events due to polypharmacy. Even though prescriptions are minimized to reduce adverse drug events in home medical care, multiple prescriptions are inevitably required, and drug interactions may cause an increase in falls. Therefore, it is considered a novel finding of this study to clarify that polypharmacy may be a cause of falls even in older patients receiving home medical care.
This was a prospective cohort study of home medical care for older patients at multiple clinics that provide home medical care. This is considered to provide an accurate picture of the actual conditions among homebound older patients. In addition, information was collected from highly accurate sources such as patients’ medical records and test results. The data were highly reliable because they were collected directly by licensed or public health nurses. The present study was also novel in that it included a large number of subjects over 90 years of age. On the other hand, however, there were several limitations of this study.
The first limitation was the lack of analysis of the number and quality of comorbidities and polypharmacy, and the lack of analysis of the type of medications. For those without a primary care physician’s opinion form, the information was mainly collected from diseases listed under the name on insurance forms when collecting information on main and pre-existing diseases, making it difficult to classify and evaluate.
Another limitation was that the details of some cases of falls were unknown. In previous studies, falls among community-dwelling older people were more common outdoors than indoors (Kato et al., 2012) and were also analyzed with respect to the location of the fall and environment. Because there is no detailed description about the time and place of the fall, environmental and psychological factors in the medical records, it was difficult to analyze the data. Since falls are caused by a complex combination of a wide range of factors, it is necessary to continue collecting and analyzing information from various sources to elucidate the factors that contribute to falls.
As the final limitation, the sample size and number of events in this study were limited. Therefore, only confounding factors that were considered particularly important were considered. However, even when gender and age were considered in the multivariate analysis as sub analysis, polypharmacy was the only factor that was a risk for falls and falls. Further analysis with a larger sample size, more confounding factors, and more detailed data is warranted in the future.
In conclusion, the results showed that polypharmacy was possibly associated with falls even in older patients receiving home medical care. This suggests the need to pay attention to observation, lifestyle support, and nursing care interventions to prevent falls and worsening of ADL.
Acknowledgments
We express our sincere gratitude to all the home care patients and their families who cooperated in the OHCARE study and the staff of the collaborating facilities.
Footnotes
Author Contributions: NM, MK (Mai Kabayama), HR, and KK conceptualized the study. NM was involved in the methodology, writing the original draft, data visualization, data validation, and reviewing and editing of the manuscript. MK (Mai Kabayama), KG, MK (Michiko Kido), and KK were involved in project administration and supervised the study. NM was responsible for the data curation and formal analysis. MK (Mai Kabayama), KG, MK (Michiko Kido), and KK contributed to study conceptualization. MK (Mai Kabayama), TY, CN, YF, CM, WF, YN, KG, MK (Michiko Kido), WT, and KK contributed to the study. TN, AH, TF, MT, YO (Yoshinari Okuda), MI, YB, MN, and YN were responsible for data collection. NM, TY, CN, YF, CM, WF, YN, YO (Yuki Omichi), EK, KG and MK (Michiko Kido) had access to the raw data. The corresponding author has the final responsibility of submitting this manuscript for publication. NM had full access to and verified the data.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported in part by grants-in-aid from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (K.K.:2510211, 15K08910, Mai Kabayama.:16K12336, and T.Y.: 20K10975) and Support for Pioneering Research Initiated by the Next Generation (N.M.: JPMJSP2138). Osaka University International Joint Research Promotion Program Support Type A.
ORCID iD: Naoko Murakami  https://orcid.org/0009-0005-3988-5795
https://orcid.org/0009-0005-3988-5795
References
- Akishita M. (2018). Challenges of pharmacotherapy for the elderly. Nihon Naika Gakkai Zasshi, 107, 110–114. [Google Scholar]
- Ambrose A. F., Paul G., Hausdorff J. M. (2013). Risk factors for falls among older adults: A review of the literature. Maturitas, 75(1), 51–61. 10.1016/j.maturitas.2013.02.009 [DOI] [PubMed] [Google Scholar]
- Berdot S., Bertrand M., Dartigues J. F., Fourrier-Réglat A., Tavernier B., Ritchie K., Alpérovitch A. (2009). Inappropriate medication use and risk of falls—A prospective study in a large community-dwelling elderly cohort. BMC Geriatrics, 9, 30. 10.1186/1471-2318-9-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhalwani N. N., Fahami R., Sathanapally H., Seidu S., Davies M. J., Khunti K. (2017). Association between polypharmacy and falls in older adults: A longitudinal study from England. BMJ Open, 7(10), e016358. 10.1136/bmjopen-2017-016358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried L. P., Tangen C. M., Walston J., Newman A. B., Hirsch C., Gottdiener J., Seeman T., Tracy R., Kop W. J., Burke G., McBurnie M. A. (2001). Frailty in older adults: Evidence for a phenotype. Journal of Gerontology: Biological Sciences and Medical Sciences, 56(3), 146–156. 10.1093/gerona/56.3.m146 [DOI] [PubMed] [Google Scholar]
- Ganz D. A., Bao Y., Shekelle P. G., Rubenstein L. Z. (2007). Will my patient fall? JAMA, 297(1), 77–86. 10.1001/jama.297.1.77 [DOI] [PubMed] [Google Scholar]
- Huang C. H., Umegaki H., Watanabe Y., Kamitani H., Asai A., Kanda S., Miyamoto A., Sato T., Kuzuya M. (2019). Potentially inappropriate medications according to STOPP-J criteria and risks of hospitalization and mortality in elderly patients receiving home-based medical services. PLoS One, 14(2), e0211947. 10.1371/journal.pone.0211947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishizumi R., Tsukamoto Y. (2017). A concept analysis of polypharmacy in the elderly. Hokkaido University of Medical Sciences Academic Repository, 24, 7–15. [Google Scholar]
- Japan Medical Association. (2017). A guide to appropriate prescribing for family physicians in a super-aging society. Retrieved August 16, 2024, from https://www.med.or.jp/doctor/sien/s_sien/008610.html
- Kamide K., Tseng W., Kabayama M. (2021). Health promotion for older population in Japan: Importance of preventive care and successful assisted living. Gerontology and Geriatric Research, 7(3), 1061. 10.26420/gerontolgeriatrres.2021.1061 [DOI] [Google Scholar]
- Kato R., Takagi C., Sakurai N., Hoshi T. (2012). Risk factors for falls and survival after falling in elderly people in a community. Nihon Koshu Eisei Zasshi, 59, 305–314. https://www.jstage.jst.go.jp/article/jph/59/5/59_305/_pdf [PubMed] [Google Scholar]
- Kayyali R., Funnell G., Odeh B., Owusu K., Sharma A., Katsaros Y., Nebhani-Gebara S., Persionek B., Wells J., Chang J. (2020). Investigating the characteristics and needs of frequently admitting hospital patients: A cross-sectional study in the UK. BMJ Open, 10, e035522. 10.1136/bmjopen-2019-035522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kojima T. (2019). Basic concepts and resolution for polypharmacy. Nihon Ronen Igakkai Zasshi, 56(4), 442–448. 10.3143/geriatrics.56.442 [DOI] [PubMed] [Google Scholar]
- Kojima T., Akishita M., Nakamura T., Nomura K., Ogawa S., Iijima K., Eto M., Ouchi Y. (2011). Association of polypharmacy with fall risk among geriatric outpatients. Geriatrics & Gerontology International, 11(4), 438–444. 10.1111/j.1447-0594.2011.00703.x [DOI] [PubMed] [Google Scholar]
- Kojima T., Akishita M., Nakamura T., Nomura K., Ogawa S., Iijima K., Eto M., Ouchi Y. (2012). Polypharmacy as a risk for fall occurrence in geriatric outpatients. Geriatrics & Gerontology International, 12(3), 425–430. 10.1111/j.1447-0594.2011.00783.x [DOI] [PubMed] [Google Scholar]
- Komiya H., Umegaki H., Asai A., Kanda S., Maeda K., Shimojima T., Nomura H., Kuzuya M. (2017). Factors associated with polypharmacy in elderly home-care patients. Geriatrics & Gerontology International, 18(1), 33–41. 10.1111/ggi.13132 [DOI] [PubMed] [Google Scholar]
- Koujiya E., Kabayama M., Yamamoto M., Akiyama M., Higami Y., Kodama K., Mukai S., Yano T., Nako Y., Nakamura T., Hirotani A., Fukuda T., Tamatani M., Okuda Y., Ikushima M., Baba Y., Nagano M., Rakugi H., Kamide K. (2020). Associations of blood pressure levels with clinical events in older patients receiving home medical care. Hypertension Research, 44(2), 197–205. 10.1038/s41440-020-00538-5 [DOI] [PubMed] [Google Scholar]
- Kozono A., Isami K., Shiota K., Tsumagari K., Nagano M., Inoue D., Adachi R., Hiraki Y., Nakagawa Y., Kamimura H., Yamamichi K. (2016). Relationship of prescribed drugs with the risk of fall in inpatients. Yakugaku Zasshi, 136, 769–776. 10.1248/yakushi.15-00245 [DOI] [PubMed] [Google Scholar]
- Li S. J., Hwang H. F., Yu W. Y., Lin M. R. (2022). Potentially inappropriate medication use, polypharmacy, and falls among hospitalized patients. Geriatrics & Gerontology International, 22(10), 857–864. 10.1111/ggi.14473 [DOI] [PubMed] [Google Scholar]
- Masumoto S., Sato M., Maeno T., Ichinohe Y., Maeno T. (2018). Potentially inappropriate medications with polypharmacy increase the risk of falls in older Japanese patients: 1-year prospective cohort study. Geriatrics & Gerontology International, 18(7), 1064–1070. 10.1111/ggi.13307 [DOI] [PubMed] [Google Scholar]
- Ministry of Health, Labour and Welfare. (2015). Central social insurance medical council home healthcare (Part 1). Retrieved August 16, 2024, from https://www.mhlw.go.jp/file/05-Shingikai-12404000-Hokenkyoku-Iryouka/0000074433.pdf
- Moon J. S., Mikami H. (2009). Comparison of factors of falls between ethnic Korean and Japanese older residents in an urban community in Japan. Nihon Ronen Igakkai Zasshi, 46, 232–238. 10.3143/geriatrics.46.232 [DOI] [PubMed] [Google Scholar]
- Morita S. S., Takanashi S., Yamaguchi N., Shimizu T., Hara Y., Takamura A. (2014). Characteristics of elderly diabetic patients with a history of falls. Nihon Tentou Yobou Gakkaishi, 1, 37–43. [Google Scholar]
- Mortazavi S. S., Shati M., Keshtkar A., Malakouti S. K., Bazargan M., Assari S. (2016). Defining polypharmacy in the elderly: A systematic review protocol. BMJ Open, 6, e010989. 10.1136/bmjopen-2015-010989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Müller B. S., Uhlmann L., Ihle P., Stock C., von Buedingen F., Beyer M., Gerlach F. M., Perera R., Valderas J. M., Glasziou P., van den Akker M., Muth C. (2020). Development and internal validation of prognostic models to predict negative health outcomes in older patients with multimorbidity and polypharmacy in general practice. BMJ Open, 10, e039747. 10.1136/bmjopen-2020-039747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murakami N., Kabayama M., Yano T., Nakamura C., Fukata Y., Morioka C., Fang W., Nako Y., Omichi Y., Koujiya E., Godai K., Kido M., Tseng W., Wada T., Nakamura T., Hirotani A., Fukuda T., Tamatani M., Okuda Y., . . . Kamide K. (2024). Actual conditions for returning home after hospitalization among older patients receiving home medical care in Japan: OHCARE study. Geriatrics & Gerontology International, 24, 320–326. 10.1111/ggi.14802 [DOI] [PubMed] [Google Scholar]
- Nobili A., Licata G., Salerno F., Pasina L., Tettamanti M., Franchi C., De Vittorio L., Marengoni A., Corrao S., Iorio A., Marcucci M., Fortino I., & SIMI Investigators. (2011). Polypharmacy, length of hospital stay, and in-hospital mortality among elderly patients in internal medicine wards: The REPOSI study. European Journal of Clinical Pharmacology, 67, 507–519. 10.1007/s00228-010-0977-0 [DOI] [PubMed] [Google Scholar]
- Shin J., Han S. H., Choi J., Kim Y. S., Lee J. (2020). Importance of geriatric syndrome screening within 48 hours of hospitalization for identifying readmission risk: A retrospective study in an acute-care hospital. Annals of Geriatric Medicine and Research, 24(2), 83–90. 10.4235/agmr.20.0017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Japan Geriatrics Society. (2015). Guidelines for safe medication for the elderly. https://www.jpn-geriat-soc.or.jp/info/topics/pdf/20170808_01.pdf
- Tinetti M. E., Speechley M., Ginter S. F. (1988). Risk factors for falls among elderly persons living in the community. New England Journal of Medicine, 319(26), 1701–1707. 10.1056/NEJM198812293192604 [DOI] [PubMed] [Google Scholar]
- Trevisan C., Di Gregorio P., Debiasi E., Pedrotti M., La Guardia M., Manzato E., Sergi G. March, A. (2017). Factors influencing short-term outcomes for older patients accessing emergency departments after a fall: The role of fall dynamics. Gait & Posture, 58, 463–468. 10.1016/j.gaitpost.2017.09.011 [DOI] [PubMed] [Google Scholar]
- Woods N. F., LaCroix A. Z., Gray S. L., Aragaki A., Cochrane B. B., Brunner R. L., Masaki K., Murray A., Newman A. B. (2005). Frailty: Emergence and consequences in women aged 65 and older in the Women’s Health Initiative Observational Study. Journal of the American Geriatrics Society, 53, 1321–1330. 10.1111/j.1532-5415.2005.53405.x [DOI] [PubMed] [Google Scholar]
- Woolcott J. C., Richardson K. J., Wiens M. O., Patel B., Marin J., Khan K. M., Marra C. A. (2009). Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Archives of Internal Medicine, 169, 1952–1960. 10.1001/archinternmed.2009.357 [DOI] [PubMed] [Google Scholar]
- Yamamoto M., Kabayama M., Koujiya E., Huang Y., Akiyama M., Higami Y., Kodama K., Nakamura T., Hirotani A., Fukuda T., Tamatani M., Okuda Y., Ikushima M., Baba Y., Nagano M., Rakugi H., Kamide K. (2019). Factors associated with changes of care needs level in disabled older adults receiving home medical care: Prospective observational study by Osaka Home Care Registry (OHCARE). Geriatrics & Gerontology International, 19(12), 1198–1205. 10.1111/ggi.13790 [DOI] [PubMed] [Google Scholar]


