Abstract
Background
Long surgical wait times have long plagued health systems in Canada and abroad. This backlog and associated strain on health human resources has been exacerbated by the COVID-19 pandemic, affecting surgeries of varying degrees of urgency across all surgical specialties, including head and neck surgery. Single-entry models (SEMs) are being increasingly studied as one possible strategy to help manage surgical wait times, and a growing number of health systems have implemented SEMs within departments such as otolaryngology—head and neck surgery. We sought to evaluate the views of head and neck surgeons at all 8 designated head and neck cancer centers across Ontario on the role of SEMs in managing surgical backlogs.
Results
We interviewed 10 Ontario head and neck surgeons on the role of SEMs in managing wait times within the field. The following themes were elicited from interview transcripts: (1) anticipated positive impact, (2) barriers to implementation, (3) patient experience, and (4) roadmap to implementation. Participants agreed that SEMs may have utility for certain types of surgeries if implemented to address local needs. They also believe this model would have the greatest impact if employed together with other approaches, such as increasing operating room time or nursing availability.
Conclusion
Our results highlighted the necessity for a nuanced approach to single-entry model implementation in head and neck surgery. While participants recognized the utility of SEMs for high-volume and low-variation surgeries, participants remained divided on the optimal approach to triaging patients necessitating more complex oncologic treatments. Deliberate collaboration among stakeholder organizations and senior surgeons will be critical if SEMs are to succeed in an intricate and political healthcare environment.
Keywords: single-entry models, health policy, surgical wait times, health services research
Graphical abstract.
Background
Excessive surgical wait times have long plagued healthcare systems in Canada and elsewhere. 1 This is thought to be due in part to Canada’s relatively unique single-payer system which does not allow for any type of non-hospital-based insured surgical care to take place, as well as a lack of human resources and funding to increase operating capacity. This problem was significantly worsened by the pause in elective surgeries during and after the COVID-19 pandemic.1,2 The backlog and associated strain on health human resources has affected surgeries of varying degrees of urgency across all surgical specialties, including head and neck surgery. 3 It will take many years before wait times are returned to their pre-pandemic levels, which many already considered unacceptably long. 4 Interestingly, wait times for urgent oncologic surgeries were the only cases with smaller backlogs than previously recorded during the pandemic, and overall wait times varied significantly by funding type.5,6 However, these wait times have risen again since the elective surgeries were resumed. 5
One strategy proposed to help manage surgical backlogs is single-entry models (SEMs). SEMs, or central-intake models, are informed by queuing theory and have demonstrated the ability to decrease wait times in various industrial sectors.7,8 They optimize the distribution and flow of patients by placing them in a common queue to see the first available surgeon. They can be organized at any level, such as among colleagues within a hospital, or at a provincial or health system level. 8 SEMs are being increasingly studied as one possible strategy to help manage surgical wait times in Canada and abroad.8-11 SEMs have been endorsed by the Canadian Medical Association as a promising strategy to improve referral triage. 12 Ontario, Canada’s most populous province, has also recently funded pilot projects to design SEMs for surgical care.13,14
A growing number of health systems have implemented SEMs within a broad range of clinical areas such as orthopedic surgery, rheumatology, and otolaryngology—head and neck surgery. 15 Head and neck oncologic care is highly specialized and regionalized beyond other areas of practice within otolaryngology—head and neck surgery. Only a small group of surgeons at 8 regional centers across Ontario are designated to perform these complex procedures. These specialized centers also contend with limited resources, emphasizing the need for efficient management of surgical waitlists. In addition, the smaller number of cases provides an opportunity to explore the effects of having a large proportion of cases enter SEMs. Wait times for treatment also directly impact patient survival, underscoring the pressing healthcare challenges faced by these subspecialists.
There is a paucity of research about SEMs for head and neck oncology specifically. Given its promise to improve access to other services, SEMs may be a suitable strategy to manage wait times in head and neck surgery, but we currently lack an understanding of stakeholder perception. Specifically, further clarity is necessary to describe the optimal structures, geographic coverage, procedure scope, funding model, and barriers to implementation in this particular subspecialty area. Without these perspectives, political and financial capital may be expended on a process that is at risk of failing before implementation. We, therefore, sought to evaluate the views of head and neck surgical oncologists at all 8 designated head and neck cancer centers across Ontario on the role of SEMs in managing surgical backlogs.
Methods
This research project received ethics approval from the Research Ethics Board at the University of Toronto (Protocol #00044197). All participating surgeons were covered by this ethics board approval.
Study Design
The qualitative method of interpretive description was used to study the perceptions of head and neck surgeons on the utility of SEMs in managing wait times. This approach allowed us to gain valuable insight from practicing surgeons to generate actionable knowledge for decision-makers, managers, and thought leaders in the field as they develop or strengthen SEMs.14,15 Interviews were conducted and transcribed with Zoom (Copyright ©2024 Zoom Video Communications, Inc., Toronto and London, Ontario). 16 This study was reported in accordance with the Consolidated Criteria for Reporting Qualitative Research.
Data Sources
We invited head and neck surgeons from all 8 head and neck cancer centers in Ontario for semi-structured interviews. We identified an initial group of prospective participants by reviewing publicly available information from hospital websites, and further study participants were contacted based on snowball and purposive sampling. 17 Purposive sampling involves study investigators selecting suitable participants, whereas snowball sampling entails having study participants identify other suitable candidates for participation. 17 Interviews were conducted by J.S. (male) and B.L. (male) between March and November 2023. There were no prior relationships between interviewers and participants. Eligibility criteria encompassed all head and neck surgeons at designated head and neck cancer centers in Ontario. Excluded were oncologists working outside these roles at the 8 centers. Participants were contacted by J.S. and interviews were scheduled. Existing research on SEMs was included in the initial contact for participants to familiarize themselves with the process and prior experiences. Recruitment concluded when saturation was achieved and interviews failed to yield novel insights as determined by study authors with expertise in qualitative methodologies (J.S., C.A., and B.L.).
Data Collection
Our team modified questions employed in a previous study led by several co-investigators on the utility of SEMs for managing surgical backlogs in general surgery. These original questions were developed from reviewing the literature, as well as consulting and piloting with content experts. 18 We used a modified Delphi approach to confirm that the adapted questions were appropriately refocused for our interviews with head and neck surgeons (Supplemental Appendix 1).1-18 We held semi-structured interviews and invited participants to read their transcripts and confirm accuracy. Interviews were transcribed by Zoom and verified with audio recordings for accuracy by one study author (S.B.).
Data Analysis
Three researchers (J.S., C.A., and B.L.) analyzed data via deductive and inductive approaches. 18 A preliminary coding framework was developed a priori based on pre-interview consultation with content experts and findings from prior SEM research. 14 NVivo was used for coding the transcript data. J.S., C.A., and B.L. iteratively triangulated findings and developed a final coding framework, from which thematic patterns were identified. Data collection concluded when we achieved saturation in terms of depth, breadth, and consistency of themes. We established validity through a data source, investigator, and theoretical triangulation. 18
Results
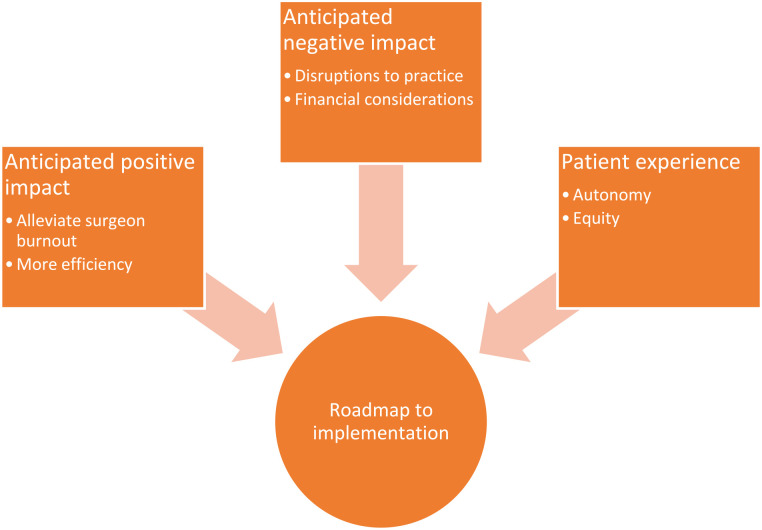
Participant demographics are provided in Table 1. We contacted 14 individuals, of whom 10 consented to be interviewed. In all, 27 surgeons worked within head and neck surgery at the 8 designated provincial cancer centers at the time this study was conducted. Nonresponders were therefore excluded from the study. One female and 9 male surgeons were interviewed for this study. Participants operate approximately 2 times per week. These surgeons represented all 8 head and neck cancer centers in Ontario (Health Sciences North/Horizon Santé-Nord, Kingston General Hospital, London Health Sciences Centre, The Ottawa Hospital, Sinai Health System, St. Joseph’s Healthcare Hamilton, Sunnybrook Health Sciences Centre, and University Health Network). Interviews lasted between 20 and 35 minutes. The following themes were derived from our interviews: (1) anticipated positive impact, (2) anticipated negative impact, (3) patient experience, and (4) roadmap to implementation (Figure 1).
Table 1.
Participant Demographics.
| Participant | Location | Institution | No. of years of experience (>20, 10-20, <10 years) | Previous, current, or no experience with SEMs |
|---|---|---|---|---|
| P1 | Hamilton | St. Joseph’s Healthcare Hamilton | <10 | Current |
| P2 | Toronto | Mount Sinai Hospital | >20 | None |
| P3 | Sudbury | Health Sciences North/Horizon Santé-Nord | <10 | None |
| P4 | Hamilton | St. Joseph’s Healthcare Hamilton | <10 | Current |
| P5 | Kingston | Kingston General Hospital | <10 | None |
| P6 | Toronto | Sunnybrook Health Sciences Centre | >20 | None |
| P7 | Toronto | Toronto General Hospital | <10 | None |
| P8 | Toronto | Toronto General Hospital | >20 | None |
| P9 | London | London Health Sciences Centre | 10-20 | Current |
| P10 | Ottawa | The Ottawa Hospital | >20 | Current |
Abbreviation: SEM, single-entry model.
Figure 1.
Relationship of study themes.
Anticipated Positive Impact
All participants were optimistic about the potential positive impact of SEMs in general and in head and neck oncology. SEMs were felt to be beneficial both on an individual surgeon level and at the systems level.
For surgeons, SEMs may alleviate burnout: “I think it will help the burgeoning waitlist and the hefty personal pressures that you feel when you’re waitlisting a patient . . . Like who wants to be a surgeon and not be allowed to operate when you need to right?” (P7). Moreover, participants suggested that SEMs would be particularly helpful for early career surgeons “who are looking to establish themselves, but maybe just aren’t getting the referrals in place so they’re kind of struggling a little bit with that” (P6).
In terms of impacting the healthcare system more broadly, many participants felt SEMs lead to better “efficiency getting patients through” (P2). “[SEMs support] better organization of OR time and utilization . . . we have a lot of wasted downtime” (P6). With SEMs, participants widely agreed that wait times would be improved overall: “the natural [benefit] would obviously be just improving our wait times” (P4); “It allows people to get in a reasonable amount of time” (P9); and “[SEMs] shorten the wait times for patients in these conditions” (P8). And more broadly, SEMs align with a growing “culture of collaboration” among surgeons (P1).
Anticipated Negative Impact
Despite the potential positive impact of SEMs, participants identified several barriers to its implementation. These were largely related to anticipated disruptions to practice and financial considerations. Many participants felt that surgeons would be reluctant to adopt SEMs, whether for reasons of pride—“there probably is some prestige to having huge wait lists for some people” (P1)—or reasons of power—“I don’t want anybody else being in control of our practice” (P2). A major concern arose around variability between surgeons and procedures. For example, “some people might be referred to a specific reconstructive surgeon because [they] have a particular experience or skill set” (P4), and so, “for subspecialisation, it becomes a little bit more difficult” (P5). Moreover, 1 participant commented on “the loss of individualized workup,” in which a patient may not be worked up “the way you would work it up” (P4), leading to discomfort proceeding with the surgery.
Another area of concern was financial. To improve capacity and implement single-entry requires funding, “a lot of money” (P4), “more OR staff, more OR efficiency” (P9), and health human resources that “the hospital doesn’t have” (P3). “There probably has to be some form of funding from the government because the hospitals do tend to respond to funding” (P1). At the individual level, surgeons may be “concerned that they’ll get a decrease in consults and patients, and this could affect their billing and bottom line” (P6). As 1 participant shared, “I think it’s a bad idea to start implementing these things because I don’t think we fully understand the problem” (P8).
Patient Experience
Participants agreed that SEMs can support patient autonomy and equity, with some caveats. The “whole goal is that people have equal waiting times” (P1) rather than “which slot did the marble go down in terms of which doctor they were referred to” (P7). In other words, “if you have a good model that’s shown to be equitable, it can only make things better” (P6). However, there was unanimous agreement that patients’ geographic location cannot be ignored. To implement SEMs at a regional or provincial level, in which patients are traveling several hours for their surgery and follow-up care, “that becomes a two-day affair where people have to take off work,” and it may be “painful to not be able to be around [family] and to be in unfamiliar places” (P3). One participant asked, “does a patient really want to travel to from Brampton to Toronto or to from Barrie to Toronto when they can get the surgery closer to home?” (P5). Some participants suggested that patient autonomy ought to be factored in, “allowing patients to have another opinion if that’s what they want” (P9), noting that “patient confidence and choice actually does play a role” (P5).
Roadmap to Implementation
Perhaps the most important task prior to implementation is to develop an informed understanding of the contemporary issues that any proposed SEM aims to solve. For example, participants voiced that not all surgeries were affected equally by the pause in elective procedures and that “malignant case wait times went down during the pandemic because there [were] no benign cases” (P1). All surgeons also emphasized the need to clarify the definition of a single-entry model, as models with different geographical scopes and surgery types would likely have a wide variety of effects, including on the level of enthusiasm among head and neck surgeons. A major recurring idea was that one must also understand the “profound effects” (P5) of the pauses in elective surgeries during the COVID-19 pandemic to comprehend the current healthcare landscape.
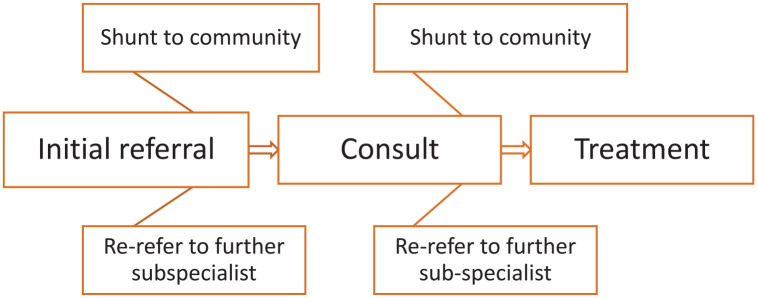
Most head and neck cancer centers have “never had too big of an issue with oncology wait times” (P3) as opposed to the backlogs for high volume “benign malignancies and [neoplasms]” (P4). Oncology wait times are meticulously monitored by provincial authorities and often come with dedicated funding, which has contributed to the relatively shorter wait times in this domain. Facilities facing extended oncology wait times might be dealing with regional or site-specific issues that may not be effectively curtailed by the implementation of SEMs alone. As such, when developing SEMs, it is important to consider the types of surgeries to be included in a model. Many participants stated that more complex oncologic cases should be excluded due to the very subspecialized nature of treatment and “logistical issues” (P3) in multidisciplinary cancer treatment. However, centers such as St. Joseph’s Healthcare Hamilton already have such a model for complex free flap surgeries which functions well in their collaborative group practice. All participants agreed that lower acuity surgeries of the head and neck lend themselves well to triage using SEMs. Multiple participants stated that the benefits of SEMs would be most fruitful “in the community” (P5). One participant queried whether we could increase case numbers in many centers even if we attempt to and whether it is accepted that “certain conditions [should] have longer wait lists than others in a resource-limited system” (P8). Many questions were posed about the best way to prioritize patients in a centralized intake model, such as by temporality, acuity, or other factors. A minimum or standardized set of criteria is crucial for “equitable distribution” (P8) and the flow of patients through the system. One participant described the potential benefits of moving “easier” (P10) cases out of head and neck surgery centers to create capacity for challenging cases. However, this was also cited as potentially “disadvantageous for resident education” (P10) if done with all low-complexity and low-variation cases. Most participants agreed that high-volume general otolaryngology procedures were particularly well-suited to SEMs as well (Figure 2).
Figure 2.
Theoretical flow through an otolaryngology SEM. SEM, single-entry model.
Iterative improvement and “maintenance” (P1) of any SEM are crucial. At 1 center, surgeons meet monthly to ensure that the cancer patients have been triaged appropriately and care is provided in a timely manner. They also adjust patients’ priority based on novel investigations that have been performed since patients were placed in the queue. Piloting models before broader implementation was also cited as very important to “[long term] scalability” (P4) and sustainability. Performance must be measured, and most surgeons believed that the “primary outcome would be wait times and secondary outcomes would be [case] volumes. . . patient satisfaction outcomes and complications” (P1).
Participants reiterated the need to identify champions for SEM implementation, such as senior surgeons or “[organizations like] the Canadian Society of Otolaryngology” (P6) or “Cancer Care Ontario” (P4). Governance considerations were emphasized, and government involvement from a funding, policy, or bureaucratic perspective can certainly galvanize or deflate a process before it has even begun. Once leaders take ownership, an important next step is to obtain buy-in and “changes in mentality” (P7) from participating surgeons. One participant proposed that having “multidisciplinary representation” (P4) in SEM management and administration, could “ensure it is patient centered” (P4). Being transparent and involving all stakeholders throughout the process was described as “important” (P8).
Multiple participants described certain strategies that they believe should be “addressed in parallel” (P7) such as engaging with “private enterprises and independent health facilities” (P7). They stated that such partnerships can reduce wait times for high-volume surgeries such as thyroidectomies. Others suggested moving large volumes of low acuity surgeries to “outpatient surgical centres” (P9) and prioritizing hospital OR time for patients who need significant management in the hospital postoperatively. Health human resource shortages are naturally a major concern to all participants, especially post-pandemic. While participants did not have a consensus on how physicians should be remunerated within a centralized referral triage system, 1 senior surgeon stated that placing participants in an alternate payment plan involving a “salary with volume incentivization” (P5) would likely increase case volumes.
Discussion
In this study, we investigated the perspectives of head and neck surgeons in Ontario on the role of SEMs in managing wait times within the field of head and neck oncology. Study participants were recruited from all 8 designated head and neck cancer surgery centers in Ontario. The following themes were elicited from our interviews: (1) anticipated positive impact, (2) anticipated negative impact, (3) patient experience, and (4) roadmap to implementation.
All participants reiterated the utility of SEMs for managing high-volume and low-variation surgeries, such as certain thyroidectomies and benign salivary neoplasms resections, which are categorized as elective according to CCO’s guidelines Target Wait Times for Cancer Surgery in Ontario. 19 Interestingly, these are cases that do not necessarily need to be managed exclusively at designated head and neck centers and could potentially be managed in community settings. Shifting these cases to the community level would create more capacity within designated centers for the complex cancer cases that require their specialized expertise and resources. However, participants were divided on whether SEMs are a useful strategy for managing more complex cancer cases. 19 A recurring theme was the collaborative nature of cancer care and its importance to the success of an SEM. Participants also felt that surgeons themselves posed the largest barrier to the implementation of SEMs. While no panacea, all participants thought they have a utility to some degree within the field. They also believe SEMs would have the greatest impact if employed together with other approaches to wait time management, such as increasing operating room time or nursing availability. These findings align with the opinions of general surgeons in a prior study. 12 Head and neck surgeons, like general surgeons, were enthusiastic about the idea of SEMs; however, they had particular concerns not raised by general surgeons regarding patient ownership and leadership of care, particularly given the multidisciplinary approach for oncologic patients.
Most research on SEMs thus far has focused on high-volume, low-variation, low-complexity, and low-acuity surgeries.7-9 SEMs have generally demonstrated positive results in terms of decreasing wait times for these procedures. However, there were very few studies investigating these models within surgical oncology of any kind, and none were identified for head and neck oncology. Interestingly, participants from certain centers, such as St Joseph’s Healthcare Hamilton and the London Health Sciences Centre already have centralized intake systems for specific types of oncologic referrals. Surgeons from these hospitals viewed their triage models positively, stating that the collaborative nature of their practice enabled such referral sharing. They believed that their team-based cultures enabled them to provide more patient-centered care. However, there was a broad objection to the idea of an SEM being established that incorporates surgeons from more than a single center. Participants felt that this would infringe on surgeon autonomy and fail to address local needs. This is congruent with past studies investigating the use of SEMs in various surgical fields.7,9
Many participants also stated that groups such as the Canadian Society of Otolaryngology—Head & Neck Surgery or the Canadian Association of Head and Neck Surgical Oncology would be ideal forums to advance the implementation of SEMs through dedicated working groups or policy positions. Endorsement by provincial groups, such as Ontario Health or analogous organizations, was deemed to be essential to successful implementation. Similar studies have likewise found that senior leaders must champion these models if they are to achieve their intended effect in a complex and political healthcare system.
Our study had several limitations. All participants work in Ontario, and as such data was situated within the context of the province’s healthcare system. However, all interviewees are actively involved in national and international subspecialty associations. Furthermore, many of them have familiarity with other healthcare systems from completing training outside of Ontario, nationally or internationally. We chose to limit our participants to solely Ontario because it is the largest Canadian province. The ability to speak with surgeons from all provincial head and neck cancer centers meant that we could attain a comprehensive understanding of the province’s approach to treating these cancers in a timely and equitable manner. Also, this study focused solely on surgeons working in major cancer centers, and these findings may not apply to those working in other domains of head and neck surgery or community settings. The number of interviewees was not large due to our provincial focus, which is common in qualitative studies. We had already interviewed 1 or more surgeons from each center at the time we concluded data collection after reaching thematic saturation. Another limitation is that surgeons were the only stakeholders consulted for this study, as opposed to patients, the public, allied healthcare workers, and policymakers. However, this is acceptable because the focus of this study is to identify surgeon concerns and opinions on SEM implementation.
Future studies could include evaluating the perspectives of other stakeholders, such as referring physicians, community otolaryngologists, patients, or others. Similar studies can also be conducted for community otolaryngology or other subspecialists, such as rhinology or pediatric otolaryngology. Crucially, quantitative data comparing wait times before and after SEM implementation in a head and neck cancer center would provide further evidence either for or against the utility of SEM implementation in the field.
Conclusion
Overall, our results highlighted the nuanced perspectives of head and neck surgeons toward SEM implementation. While participants recognized the utility of SEMs for high-volume and low-variation surgeries, participants remained divided on the optimal approach to triaging patients necessitating more complex oncologic treatments. Team-based care emerged as an indispensable requirement, and deliberate collaboration among stakeholder organizations and senior surgeons will be critical if SEMs are to succeed in an intricate and political healthcare environment. Further studies could describe the views of other stakeholders and utilize both quantitative and qualitative methods.
Supplemental Material
Supplemental material, sj-xlsx-1-ohn-10.1177_19160216241286793 for Evaluating Perceptions of Head and Neck Surgeons on the Role of Single-Entry Models in Managing Surgical Waitlists in Ontario: A Qualitative Study by Justin Shapiro, Charlotte Axelrod, Ben B. Levy, Saruchi Bandargal, Emily C. Steinberg, Emily Wener, John de Almeida, Joel Davies, Brian Rotenberg, Antoine Eskander, Janet Chung, David Urbach and Yvonne Chan in Journal of Otolaryngology - Head & Neck Surgery
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Justin Shapiro  https://orcid.org/0000-0002-6559-9515
https://orcid.org/0000-0002-6559-9515
Charlotte Axelrod  https://orcid.org/0000-0003-2688-3633
https://orcid.org/0000-0003-2688-3633
Saruchi Bandargal  https://orcid.org/0000-0003-3763-2119
https://orcid.org/0000-0003-3763-2119
Emily C. Steinberg  https://orcid.org/0009-0009-8421-5781
https://orcid.org/0009-0009-8421-5781
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Blumenthal D, Fowler EJ, Abrams M, Collins SR. Covid-19—implications for the health care system. N Engl J Med. 2020;383(15):1483-1488. [DOI] [PubMed] [Google Scholar]
- 2. Diaz A, Sarac BA, Schoenbrunner AR, Janis JE, Pawlik TM. Elective surgery in the time of COVID-19. Am J Surg. 2020;219(6):900-902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Urbach DR. Improving access to health services in Canada. Healthc Manage Forum. 2018;31(6):256-260. [DOI] [PubMed] [Google Scholar]
- 4. Wang J, Vahid S, Eberg M, et al. Clearing the surgical backlog caused by COVID-19 in Ontario: a time series modelling study. CMAJ. 2020;192(44):E1347-E1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Damani Z, Conner-Spady B, Nash T, Tom Stelfox H, Noseworthy TW, Marshall DA. What is the influence of single-entry models on access to elective surgical procedures? A systematic review. BMJ Open. 2017;7(2):e012225. doi: 10.1136/bmjopen-2016-012225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lopatina E, Damani Z, Bohm E, et al. Single-entry models (SEMs) for scheduled services: towards a roadmap for the implementation of recommended practices. Health Policy. 2017;121(9):963-970. [DOI] [PubMed] [Google Scholar]
- 7. Milakovic M, Corrado AM, Tadrous M, Nguyen ME, Vuong S, Ivers NM. Effects of a single-entry intake system on access to outpatient visits to specialist physicians and allied health professionals: a systematic review. CMAJ Open. 2021;9(2):E413-E423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Novak KL, Van Zanten SV, Pendharkar SR. Improving access in gastroenterology: the single point of entry model for referrals. Can J Gastroenterol. 2013;27(11):633-635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Damani Z, Mackean G, Bohm E, et al. The use of a policy dialogue to facilitate evidence-informed policy development for improved access to care: the case of the Winnipeg Central Intake Service (WCIS). Health Res Policy Syst. 2016;14(1):78. doi: 10.1186/s12961-016-0149-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Canadian Medical Association. Six steps to an effective central intake program [internet]. 2014. Accessed April 28, 2021. https://www.cma.ca/Assets/assets-library/document/en/advocacy/Six-steps-central-intake-2014.pdf
- 11. Ministry of Health. Ontario ramping up efforts to reduce surgical wait times [internet]. 2021. Accessed August 10, 2021. https://news.ontario.ca/en/release/1000613/ontario-ramping-up-efforts-to-reduce-surgical-wait-times?utm_source=sfmc&utm_medium=email&utm_campaign=OMA%20News%20July%2030%202021&utm_term=View%20the%20Ministry’s%20news%20release&utm_id=141463&sfmc_id=7603219
- 12. Shapiro J, Axelrod C, Levy BB, Sriharan A, Bhattacharyya OK, Urbach DR. Perceptions of Ontario health system leaders on single-entry models for managing the COVID-19 elective surgery backlog: an interpretive descriptive study. CMAJ Open. 2022;10(3):E789-E797. doi: 10.9778/cmajo.20210234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Michael Garron Hospital. Michael Garron Hospital Launches a New eReferral System and Hospital-Wide Central Intake Model [internet]. 2021. Accessed November 19, 2022. https://www.tehn.ca/about-us/newsroom/michael-garron-hospital-launches-new-ereferral-system-and-hospital-wide-central
- 14. Thorne S, Kirkham SR, Macdonald-Emes J. Interpretive description: a noncategorical qualitative alternative for developing nursing knowledge. Res Nurs Health. 1997;20(2):169-177. [DOI] [PubMed] [Google Scholar]
- 15. Archibald MM, Ambagtsheer RC, Casey MG, Lawless M. Using zoom videoconferencing for qualitative data collection: perceptions and experiences of researchers and participants. Int J Qual Methods. 2019;18:160940691987459. [Google Scholar]
- 16. Auerbach C, Silverstein L. Qualitative Data: An Introduction to Coding and Analysis. NYU Press; 2003. [Google Scholar]
- 17. Carter N, Bryant-Lukosius D, DiCenso A, Blythe J, Neville AJ. The use of triangulation in qualitative research. Oncol Nurs Forum. 2014;41(5):545-547. [DOI] [PubMed] [Google Scholar]
- 18. Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893-1907. doi: 10.1007/s11135-017-0574-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Walker MJ, Wang J, Mazuryk J, et al. Delivery of cancer care in Ontario, Canada, during the first year of the COVID-19 pandemic. JAMA Netw Open. 2022;5(4):e228855. doi: 10.1001/jamanetworkopen.2022.8855 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-xlsx-1-ohn-10.1177_19160216241286793 for Evaluating Perceptions of Head and Neck Surgeons on the Role of Single-Entry Models in Managing Surgical Waitlists in Ontario: A Qualitative Study by Justin Shapiro, Charlotte Axelrod, Ben B. Levy, Saruchi Bandargal, Emily C. Steinberg, Emily Wener, John de Almeida, Joel Davies, Brian Rotenberg, Antoine Eskander, Janet Chung, David Urbach and Yvonne Chan in Journal of Otolaryngology - Head & Neck Surgery