Abstract
Objective
Dysphagia is highly prevalent worldwide, causing serious complications. Video-game based rehabilitation training can increase dysphagia patient motivation and adherence. However, the acceptance of video game systems by patients and healthcare providers is still not fully explored. This study aimed to explore the acceptance of the video game swallowing training system among potential users.
Methods
The in-depth interviews were conducted face-to-face between July and October 2023 at a rehabilitation center in China, with a sample size based on the principle of information saturation. Interviews were audio-recorded and transcribed verbatim, and the data were analyzed using theory-driven thematic analysis methods based on the technology acceptance model.
Results
A total of 19 participants participated in the interviews, which included 11 hospitalized dysphagia patients, three rehabilitation therapists, one doctor, and four nurses. Three themes and seven subthemes were identified. Sufficient training content, interesting interaction between the game and the rehabilitation training, intuitive page design, and efficient training modes were related to the usefulness of the system; user-friendly page design and simple interface could make it easier for participants to use the system. Overall, the availability of the video game system for use without geographical or time limitations led to a high level of participant intention to use the system, but it is still challenging to use it in the real world.
Conclusions
The results of the study showed that participants were generally accepted and willing to use the video game system for dysphagia rehabilitation training. The video game-based swallowing function training system can be helpful in assisting with dysphagia rehabilitation.
Keywords: Video game, dysphagia, rehabilitation, qualitative study, acceptance, technology acceptance model
Introduction
Dysphagia is a clinical phenomenon in which the jaw, lips, tongue, soft palate, pharynx, esophagus, and other organs are structurally and/or functionally impaired, preventing the safe and effective delivery of food from the mouth into the stomach. 1 A United States study analyzing the 2012 National Health Interview Survey found that about 9.44 million adults had swallowing problems, accounting for 4% of the country's total population.2,3 In the Japanese community, the prevalence of dysphagia was 13.8% in community-dwelling elderly people over 65 years of age, with a high prevalence of 28.2% in those over 85 years of age. 4 Notably, a survey of 20 communities and 20 nursing homes in China showed that 19.2% of older individuals suffered from dysphagia. 5 The severity of dysphagia ranges from a complete inability to elicit a pharyngeal response or airway protection to mild discomfort when eating food and liquids, which can lead to dehydration, malnutrition, pneumonia, and other adverse effects that increase the risk of death in patients. 6 Appropriate treatment of dysphagia aim to extend patients’ life, improve the quality of life of the patient, prevent serious complications such as aspiration, aspiration pneumonia, and asphyxia, improve their health outcomes, and reduce length of hospital stay.7,8
Rehabilitation of dysphagia is a complex process, requiring a multidisciplinary team effort that involves speech-language pathologists, therapists, doctors, and nurses. They collaborate with a multidisciplinary approach that includes muscle strengthening, skill training, physical therapy, occupational therapy, compensation therapy, and nutritional support.9,10 Collaboration with patients and their families, centering on their values and needs, is crucial for successful treatment. However, current dysphagia rehabilitation methods face multiple challenges. One significant issue is the monotonous physical rehabilitation models, which can lead to reduced patient engagement and motivation.11,12 Additionally, practical constraints such as space limitations, transportation barriers, and availability of trained personnel can affect the implementation and effectiveness of these programs.10,13 These multifaceted challenges collectively contribute to low patient compliance, diminished motivation for rehabilitation participation, and increased work pressure on healthcare staff. 14
In the evolving digital age, there has been a surge in the use of video game modalities by researchers to facilitate therapeutic interventions for patients.15,16 Contemporary research has integrated gamification methods into rehabilitation frameworks, crafting virtual environments that meet patient-specific requirements, providing relevant experiential scenarios, and engaging in multisensory interactions across multiple dimensions, including visual, auditory, and tactile.17,18 This integrated approach enhances the rehabilitation paradigm, making it more immersive and accessible. As societies are aging, the number of patients with dysphagia is increasing, making the management of dysphagia rehabilitation even more important to cope with the burden of health care. 19 Video games can be a helpful but understudied clinical tool, especially in recovering populations, who are more likely to benefit from the use of video games for condition management and healthcare services. 20 Athukorala et al. conducted a study that helped patients with Parkinson's dysphagia with swallowing rehabilitation, using the surface electromyography biofeedback device and the Biofeedback in Swallowing Skill Training software. 21 The patients were given feedback about the outcome of their actions through changes in the shape of swallowing targets, such as green squares, on a computer screen during skill training. The results showed significant improvements in swallowing function and swallowing-related quality of life. Biofeedback provided through vision, auditory, or haptic sensations can complement the lack of intrinsic feedback in patients with dysphagia due to neurological impairments. 22 Biofeedback provided through gamification transforms hidden swallowing movements into user-friendly outputs, making it easier for patients to understand swallowing performance and increasing their motivation for treatment. 22
A system designed with the user-centered approach requires an evidence-based methodology based on the needs and understanding of a specific group of end-users to determine the intended use and required functionality of the system. 23 Therefore, continued interaction with potential user groups is needed to obtain feedback for better program design. Users’ full experience of the system will help to stimulate conversations and provide a deeper understanding of end-users’ needs and opinions. 24 By understanding users’ (i.e. healthcare providers and patients) perceptions of video game systems, their accessibility, acceptability, and adoption of video games can be improved. 25 Constantinescu et al. conducted interviews with users targeting home treatment adherence and game design elements in order to design an mHealth application combining surface electromyography and biofeedback for patients with dysphagia after head and neck cancer. 26 It was found that participants agreed that biofeedback should be immediate, simple, and straightforward. Participants felt that it was important to be able to notice progress over time, which helped them to build confidence and improve their adherence. Gabbas et al. conducted interviews with doctors and dysphagia patients to help design a gamified user page for dysphagia rehabilitation. 27 They combined the isotonic, isokinetic, and isometric movements of swallowing training, such as shaker training, with concentric balls of different colors, which responded to the level of difficulty of the training through changes in the transparency of the concentric balls. However, both studies only surveyed the needs of patients during the design phase of the game page and lacked feedback and suggestions from patients after the game development was completed. Rodriguez et al. developed a new system for the gamification of tongue rehabilitation based on virtual reality with head-mounted displays and tested it with three therapists to assess the usability, development cost, robustness, technical novelty, and interactivity of the gamification system. 28 However, this study lacked the test of patient usability. Therefore, there is still a lack of research on the acceptance of the new technology by potential users of the rehabilitation game once it has been developed.
The technology acceptance model (TAM) was proposed by Davis, 29 it explains and predicts individuals’ adoption or acceptance of computer information systems or information technology. The model proposes two major factors as determinants: perceived usefulness and perceived ease of use. Perceived usefulness refers to how much users believe that the use of particular system will improve their efficiency or performance, and perceived ease of use refers to how easy the user finds the system to use. 29 At the same time, perceived ease of use enhances perceived usefulness in particular situations.
Before using the video game-based swallowing training system in a clinical environment, it is important to understand the situations and factors that predict its acceptance by people who will use it. Therefore, this study aimed to explore the acceptance of the video game-based swallowing function training system among potential users, using the TAM to investigate the acceptance through face-to-face interviews with health healthcare providers (i.e. nurses and rehabilitation therapists) and patients with dysphagia.
Methods
A qualitative descriptive design approach was used for the study. Semi-structured, individual interview methods were used, which provided flexibility in data collection and produced rich narratives that allowed the researcher to analyze how participants made sense of the topic under investigation. 30 Qualitative data collection and analysis were reported following the consolidated criteria for reporting qualitative research (Supplementary File 1). 31
Video game-based swallowing function training system
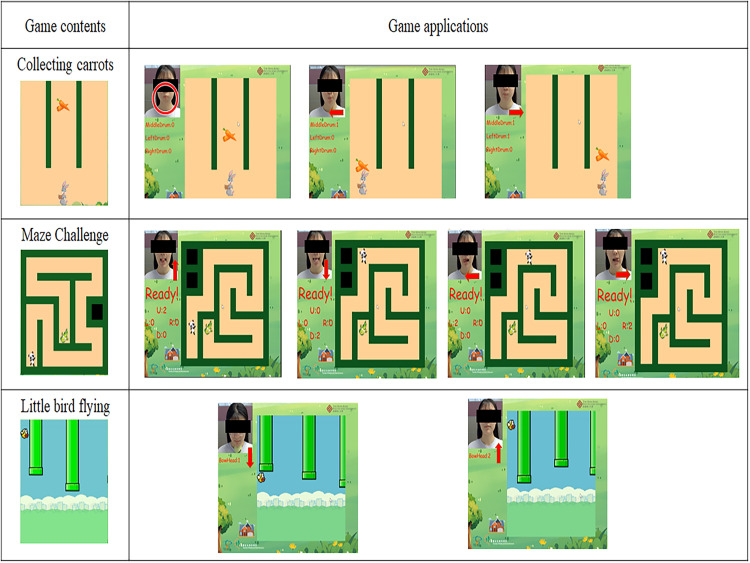
The video game-based swallowing function training system was based on the task, user, performance, and function unified usability framework, 32 designed to be patient-centered. Participants will interact with a facial recognition system utilizing MediaPipe's AI-based landmark detector to track facial expressions in real time. 33 By detecting 3D shifts in facial muscles, including the cheeks, mouth, and chin, the system allows hands-free control of therapeutic video games for dysphagia rehabilitation. The system includes three mini-games: (1) Lip exercise game where players move a rabbit character left and right by alternately activating their left and right cheeks. Kang et al. 34 showed that stroke patients with dysphagia who received oral exercises, combined with tongue, jaw, pharyngeal and respiratory exercises, were effective in improving swallowing function. Mul et al. 35 found that patients with higher cheek pressure and endurance had weaker dysphagia and that swallowing could be effectively improved by cheek or lip movements; (2) Tongue exercise game with a maze navigated by detected tongue movements up, down, left, and right. Tongue exercises are commonly recommended by clinicians for patients with dysphagia. 36 Through tongue exercises, the patient's swallowing pressure and tongue strength can be improved, effectively enhancing tongue muscle strength and muscle coordination, and improving oral transit function through tongue elevation and lateral exercises, which improves the patient's swallowing function37,38; and (3) Lower jaw exercise by lifting the chin down and squeezing the rubber ball, controls the vertical movement of a flying bird character through on-screen barriers. Chin tuck against resistance was found to be an effective training method to improve the stroke patient's swallowing function, which is to exercise the suprahyoid muscles through jaw contraction against resistance exercises39–41 (Figure 1). The biofeedback from game performance allows targeted activation of muscles involved in swallowing to strengthen them. This facial tracking system with customized games provides a patient-friendly approach to improve muscle control for swallowing disorders. The real-time quantitative feedback motivates continued engagement with the rehabilitative tasks.
Figure 1.
Game contents and applications of the video game-based swallowing function training.
Setting and participants
This study was conducted from July to October 2023 at a rehabilitation center in Beijing, China. Healthcare providers and dysphagia patients were selected as the research objects by purposive sampling method. Healthcare providers were chosen for the study because healthcare providers are also potential users and can identify possible shortcomings in the consistency of game tasks and difficulty levels with educational program practices. The sample size criterion is that the information provided by the interviewees is repeated and no new themes are presented at the time of data analysis (data saturation). 42
The inclusion criteria of healthcare providers were: (1) have worked in the rehabilitation center for 3 months at least; (2) have experience related to the treatment or care of dysphagia for at least 3 months; (3) have experienced the dysphagia training based on video game 1 week in this study; and (4) able to speak and understand Chinese.
The exclusion criteria of healthcare providers were: healthcare providers from other hospitals to study or intern healthcare providers.
The inclusion criteria of patients were: (1) hospitalized during the study period; (2) diagnosed with dysphagia by a doctor using Gugging Swallowing Screen, with no restrictions on the severity of the dysphagia; (3) aged 18 or above; (4) have experienced the dysphagia training based on video game 1 week in this study; and (5) able to speak and understand Chinese.
The exclusion criteria of patients were: (1) dysphagia caused by structural lesions (e.g. radiotherapy, previous surgery of the head and neck region such as laryngectomy and cordectomy); (2) have a significant cognitive impairment, with mini-mental state examination score <24. 43
To obtain recommendations on the acceptability of the video game system to as many potential users as possible so that we could develop a dysphagia rehabilitation system that would be applicable to users of all backgrounds, we did not screen or assess the technical experience of potential users.
Users experienced the system under the supervision of the researcher following a structured protocol: (1) first use: the researcher provided guidance and assistance to familiarize the user with the system. (2) subsequent use (second to fifth): The researchers were present but did not offer assistance. They only answered necessary questions or provided minimal guidance to encourage independent use. Besides experiencing the video game system, patients received conventional swallowing treatment, including health education, nutritional management, postural techniques and compensatory strategies, and dietary modifications as needed.
During patient interviews, family members were allowed to be present to assist with communication if necessary, particularly for patients with speech difficulties due to comorbid dysarthria. However, family members did not directly participate in the interviews, nor did they experience the video game system themselves.
Data collection
The interviews were recorded in strict accordance with the principles of audio recording, with the commitment that all audio recordings would be used for text transcription only, and that if the interviewees refused to be recorded, the researcher would conduct live transcriptions. The interview time was 30–40 minutes per interviewee. All information was transcribed and returned to the interviewees for verification. Memos were flexibly applied to record the researcher's feelings, thoughts on the research questions, and reflections while analyzing the data at any time during the interview process.
The interview outline was designed based on the literature review and the TAM, reviewed and refined by experts in dysphagia and informatics.29,44 The authors Bohan Zhang and Vivian Hui checked and improved the interview outline. During the interview study, some questions were modified (e.g. simplified wording) or added to clarify important elements that had emerged from the earlier interviews. 45 The final interview outline included the main contents: (1) “What do you think of this video game system?”; (2) “What outcomes do you think can be achieved through the use of this system?”; (3) “Do you like it? What do you like most about the system?”; (4) “Do you dislike it? What do you dislike most about the system?”; (5) “Are you interested in using the system?”; (6) “Why would you want to use it? Or why would you prefer to NOT use it?”; (7) “Would you recommend this to others? Can you suggest any changes to improve this system?”; (8) “Any other comments?” (Supplementary File 2).
Data analysis
Within 24 hours after the interview, transcriptions from the recordings were transcribed verbatim by the researcher into a transcript in Microsoft Word, and the original data in the research process will be numbered and marked for easy searching. Summarized coding using Nvivo 14 for within-case and between-case comparisons. 30
A theory-driven method of thematic analysis was used, and interview data were analyzed in terms of the TAM and the overall goals of the study. 44 Therefore, the analysis was directed to explore the usefulness of the video game system, and the ease of use for people with dysphagia, healthcare providers, and their intention to use it. Interviews and data analysis, quotes translated were conducted by the authors Bohan Zhang and Ka Po Wong, and crosschecked by the authors Vivian Hui, Yue Liu, and Jing Qin. First, the researchers repeatedly read the Chinese transcripts for meaningful information, performed initial coding, grouped comparisons, and organized the emerging themes into meaningful clusters to form an initial coding template. Throughout the analysis, an iterative approach was used to continually revisit and refine the coding. Codes were reviewed and modified based on our theoretical approach and research objectives, and finalized into themes. After completing the analysis independently by two researchers, a meeting was held to discuss the discrepancies in the hierarchy of themes until a consensus was reached. 46 The back-translation method was used to ensure the accuracy of the translation of the quotes and to preserve the original meaning. 47 After the initial translation by one researcher, a second researcher translated the English quotes into Chinese. Then these back-translations were compared with the original Chinese quotations to identify and resolve any discrepancies.
Rigor and trustworthiness
The trustworthiness of the research results was verified through the following two methods: (1) original materials: the recording materials, notes, and memos collected during the research are properly preserved. In the process of research and analysis, two researchers participated in the analysis and returned the research results to the original materials for verification; (2) feedback method: two researchers analyzed separately and compared and identified overlapping themes and sub-themes, and if there were differences, resolved them with the third researcher.
Ethical considerations
The interview time and place were agreed upon with the interviewees in the form of face-to-face. Before the interview began, the purpose and significance of the study were introduced, written informed consent was obtained from all interviewees, and the names of the interviewees were replaced with English codes and numerical ordinal numbers. The patients’ code was P and the healthcare providers’ code was M.
Results
Participant characteristics
A total of 19 participants were recruited between July and October 2023, including 8 healthcare providers and 11 patients with dysphagia. Of the healthcare providers, four were nurses, three were rehabilitation therapists, and one was a doctor. The average years of dysphagia rehabilitation work was 9.38 years. The patient participants included a total of four males and seven females with a mean age of 58.18 years. Sociodemographic details of healthcare providers are shown in Table 1, and sociodemographic characteristics of patients are shown in Table 2.
Table 1.
Healthcare providers’ sociodemographic characteristics (n = 8).
| Caregiver | Age | Gender | Educational Status | Professional Title | Duty | Work Experience of Dysphagia, Years |
|---|---|---|---|---|---|---|
| M1 | 26 | Male | Bachelor | Junior | Nurse | 5 |
| M2 | 33 | Female | Bachelor | Junior | Nurse | 2 |
| M3 | 31 | Female | Bachelor | Intermediate | Nurse | 7 |
| M4 | 36 | Female | Bachelor | Intermediate | Rehabilitation therapist | 12 |
| M5 | 38 | Female | Bachelor | Senior | Head of nurse | 8 |
| M6 | 51 | Female | Associate degree | Intermediate | Rehabilitation therapist | 31 |
| M7 | 34 | Female | Master's degree or above | Intermediate | Doctor | 9 |
| M8 | 25 | Female | Master's degree or above | Junior | Rehabilitation therapist | 1 |
Table 2.
Patients’ sociodemographic characteristics (n = 11).
| Patient | Age | Gender | Educational Status | Residence | Diagnose | Co-morbidities (Self-reported) |
|---|---|---|---|---|---|---|
| P1 | 64 | Female | High school | Urban | Stroke | Hypertension, hyperlipemia |
| P2 | 59 | Female | Junior school | Urban | Meningioma | Hyperlipemia, anemia |
| P3 | 30 | Female | Bachelor | Urban | Acoustic neuroma | NA |
| P4 | 76 | Female | Bachelor | Urban | Stroke | NA |
| P5 | 43 | Male | High school | Urban | Stroke | Hypertension, diabetes |
| P6 | 59 | Female | High school | Suburb | Stroke | Hypertension, diabetes |
| P7 | 75 | Female | High school | Urban | Alzheimer’s disease | NA |
| P8 | 78 | Female | High school | Urban | Stroke | Hypertension, diabetes |
| P9 | 71 | Male | Junior school | Urban | Guillain-barre syndrome | NA |
| P10 | 36 | Male | Bachelor | Urban | Schwannoma | NA |
| P11 | 49 | Male | High school | Urban | Stroke | Hypertension, diabetes |
By analyzing the participants’ feedback, three themes and seven sub-themes related to the video game for swallowing rehabilitation were identified (Table 3). Three thematic sections on three key factors that affect the acceptance of video games: perceived usefulness, perceived ease of use, and intention to use.
Table 3.
The main themes and sub-themes.
| Main Themes | Sub-Themes |
|---|---|
| Perceived usefulness |
|
| Perceived ease of use |
|
| Intention to use |
|
Theme 1: perceived usefulness
Sufficient training content to support the needs of patients with dysphagia
Most participants indicated that the three games of the video game-based swallowing function training system covered most of their rehabilitation training and could satisfy their daily rehabilitation needs:
… I think three games are sufficient. Because the more programs they do, the more they may forget or not understand…We need to consider the patients’ capacity for learning and their attention span (M1).
The current games can improve swallowing… Because the rehabilitation therapist provides exercises also like ‘pointing here’ or ‘pointing there’ (fingers to the face), I don’t like it. But when I use this (the video game system), I look at the character feedback to know if I've done it right or not, it's more intuitive… I think for now, I think it's good (P6).
Video games increase patient interest and initiative by providing interactive to rehabilitation
Participants reported that rehabilitation training in the form of games can enhance their interest in rehabilitation more. Because game training is something new to them, they have not experienced it before. Interacting with the game stimulates their initiative and interest in rehabilitation.
It's okay, I think it's more interesting for the patient, it's not just that we’re doing some training exercises or electrical stimulation and everyone is the same in every case. Because rehabilitation is a pretty boring process, it's more fun to have something new to add to the training. I think it's a good method (M7).
The game is pretty interesting and fun. The graphics and interactive elements really help to keep me engaged. It's a refreshing change! (P3).
Game pages allow visualization and intuitive showing of training results
The video game-based swallowing training system provides direct feedback to the participant on whether they have completed the training actions through the screen picture and sound. Participants believed that visual display of training results could also motivate patients to continue their training.
And there is feedback to them (the patient). It's more visualized. ‘Eh, I made it. Eh, I didn't make it’, that motion picture of the video-game, I think it's pretty good (M4).
It feels good to be confronted with direct evaluation… Unlike traditional therapy where progress can sometimes feel abstract, this game provides immediate feedback on my performance… It's definitely good for functional exercise as well, I'm not just completing the swallowing training, I have to understand how to play the game, and I think it's good for my cognition as well (P7).
Training can be completed efficiently
Using the video game swallowing training system can help patients to complete their rehabilitation training at home, reducing travel time. At the same time, the rehabilitation model can be changed from “one-to-one” to “one-to-many”, which saves the rehabilitation therapist's treatment time and allows them to complete their work more efficiently.
Now this kind of rehabilitation, it's a whole day's work…You have to keep talking and keep reminding him (the patient) to do it…(Using video game system) I can train several patients at the same time. At least, I can do one on two, and I can look over here and I can look over there, because I can listen to the sound. Well, I can listen to it, and if you “ding”, that means you did it, and I can focus on the patient who didn't ding over here…I don't have to focus on one patient all the time (M4).
Theme 2: perceived ease of use
Learning how to use it is easy through a user-friendly and simple interface
Participants indicated that the video game swallowing system was easy to operate, could be learned how to use quickly, and did not require much computer skills. They considered that the game page design was simple. When patients used it, they did not get dizzy when watching the computer screen, and it did not increase the burden on their eyes. The page design is simple and easy for patients to understand.
I think the ease of use is pretty high. Because there are not too many keys, if there are more keys it may be more complicated to use, but I see that (video game system) does not seem to have too many keys (M1).
It's easy to use…I have to say, even someone with less intelligence than me can use this (P9).
I can do this myself. It doesn't hurt my eyes to look at it, and I don't get dizzy when I use it (P3).
Theme 3: intention to use
High flexibility for patients without geographical and time limitations
The use of video game rehabilitation training provides a variety of options for the rehabilitation of dysphagia patients, helping them to complete their training more easily and efficiently. Patients can use the video game at home, in the community, or in the hospital, saving them traveling time. Patients can choose when and where they are most comfortable to complete their training.
After all, not all patients have a rehabilitation hospital in the neighborhood where they live. They may be traveling a long distance or they may be outpatients who have to run to the hospital every day. So, it's hard for patients to keep training. So, I think this (video game system) would be better (M3).
Patients like me, I just can't swallow and now I can't do it (rehabilitation) on an outpatient clinic…I have to be hospitalized…it's easier for me to do it myself at home like this one…there are more options (P10).
Practical use in the real world is still challenging
While there is a lot of positive feedback about video game systems, they are still challenging to apply in practice. For example, elderly patients need help from family members to use computers, the accuracy of the face recognition technology used needs to be further improved, background supervision needs to be refined, and the game needs to be set up with graded challenges to increase interest.
As long as the patient's cognition is good, they can basically cooperate, but some may have to have someone to supervise or push them. But if it's one of these cognitively problematic ones, then someone definitely has to supervise them, that is, push them to train (M7).
I'm old and may need my daughter's help to train with this, I'm not very good at using the computer. You see, I didn't grow up with all this technology…The screen, the camera, it all makes me nervous (P2).
Discussion
This study used a qualitative research methodology and included patients, family members, doctors, nurses, and rehabilitators who are potential users of this video game-based swallowing function training system. The results of this study indicated that although there are some challenges to using video games for rehabilitation in practical applications, users are confident in using video games for dysphagia rehabilitation in the future and perceive the system to be useful and easy to use.
Technology acceptance is a major challenge for designers and developers of new technologies. With the growing popularity of mobile technology in healthcare, the widespread use of invasive technologies such as sensors, face recognition, and deep learning may cause greater concern among users and reduce their intention to use new technologies. 48 In addition, the perception of technology by healthcare providers may influence the implementation of new device treatments. The TAM, which centers on perceived usefulness and perceived ease of use, significantly influences the individual's acceptance or intention to engage with technology, and TAM has been very effective in understanding how potential users perceive new technologies. 44
One recent technology is video games, which provide an interactive personal experience through computer-generated games that provide real-time feedback on the user's choices, movements, and facial expressions. 49 Fewer studies focused on user acceptance of video games and more studies have explored the physical and cognitive benefits of video games for users, such as improvements in memory function, 50 attentional, 51 perceptual, 52 depression and anxiety, 53 and pain. 54
Perceived usefulness was defined as a subjective estimate of the degree to which users improved their swallowing function after using the video game system for dysphagia rehabilitation training. 55 This study found that the video game-based swallowing function training system was perceived as useful by participants. It contained three exercises, including facial, tongue, and neck muscles, with enough training content to meet the needs of patients with dysphagia. Moreover, the video game system added an interactive element to the rehabilitation training and a visual presentation of the results, which aroused interest and increased the practice initiatives among patients in rehabilitation. Due to these reasons, swallowing training can be completed efficiently. When training with video games, the interaction between patients and computers is beneficial if it creates positive perceptions and attitudes toward adopting new learning styles, thereby increasing active engagement and enhancing the patient's ability to absorb new learning content. 56 In addition to this, unlike traditional training techniques, patients found video games very interesting because of the visualization and engaging presentation of the results pages. This finding is consistent with the results of Padilla et al. that the use of user-computer interaction leads to high perceived fun, which influences perceptions of the usefulness of video games by patients. 57
Perceived ease of use was defined as an estimate of how easy it was for the users to use the video game system for rehabilitation of swallowing function. 55 Most participants considered it very easy to learn how to use the video game system through its friendly and simple interface. The intention of users to use a particular technology is heavily influenced by the effort required to use it. 44 Consistent with previous studies, participants felt that video games need to be user-friendly, always including clean graphics and easy access to information. 58 In addition, previous research identified a key assumption of ease of use as the importance of repeated hands-on experience with the technology and user guides that can be referenced to foster comfort, especially for initially reluctant patients. 59 Demonstration of the user guide by healthcare providers and condensing it into a format that is easier for patients to understand will help improve ease of use. Further research is needed to adapt technology to meet the needs of people with severely limited cognitive function and mobility.
This study found that participants’ intention to use video game system for dysphagia rehabilitation in the future in clinical practice was high, mainly due to more flexibility in the use of video game system, which allows patients to perform rehabilitation without time and geographic limitations. This is consistent with the study by Portz et al., 25 more and more patients are interested in using new technologies to manage their health, and new technologies will particularly benefit patients who live far from their healthcare providers by improving their access to care. Once older patients are exposed to a technology, they tend to become high utilizers of that technology. 60 Healthcare providers also had a high intention to use the video game system because they believed that proper use of the system would increase their productivity, quality of service, and reduce patient commuting time. Since healthcare providers have a high awareness of healthcare practices and eHealth, their perceived usefulness and perceived ease of use of the system are also higher, which significantly influences their intention to use it. 61
However, there are some challenges to using the video game system in real-world environments. For instance, elderly patients are not competent to use computers and need help from family members, and background monitoring is required to monitor and review patients’ training process. These findings are consistent with Scott et al. 62 such as the technical skills needed to teach patients to access new technologies, the availability of technical support, and other challenges that hinder the adoption of new technologies in real-world settings. Further technological developments, in the form of increased background supervision, improved technical accuracy, patient education and counseling, and policy guideline development, could remove these barriers and stimulate the development and application of information technologies. 63
Given that conventional exercises such as muscle strengthening, skill training, and physical therapy are widely adopted in clinical practice to improve health outcomes for dysphagia, it is important to understand how gamification could enhance patient engagement in these exercises. Future work is necessary to better define the clinical benefits of these exercises in various dysphagic populations when completed in a traditional manner and via gamification. Independent of treatment efficacy, evaluating user experience adds critical value to our understanding of the treatments and can be used in combination with efficacy data to improve usability and utilization.
Strengths and limitations
The qualitative research design and thematic analysis were used to obtain multiple insights into the acceptance of the video game swallowing training system from patients, doctors, nurses, and rehabilitators. Using the initial video game system to obtain participants’ suggestions for the rehabilitation intervention development could shed light on the system’s function and design, thereby informing future swallowing rehabilitation models. Our study also identified real-world barriers to the use of the video game, such as computer accessibility limitations and background supervision needs. Overcoming these barriers in the future will allow them to play an important role in patient swallowing rehabilitation.
However, some limitations should be considered when interpreting the results of this study. First, the acceptance of the video game system only represented the opinions of participants who experienced it for 1 week, and the suggestions of long-term users were not taken into consideration. Moreover, since the intensity of effective training was not achieved, there was no data collected on the swallowing function of the patients, and no limitations on the etiology of dysphagia. Randomized controlled trials can be conducted in the future to explore the efficacy of the video game system. Second, we only interviewed one rehabilitation hospital, and opinions from other organizations or communities may be different. Third, although we recruited as many participants of all ages as possible, we did not maintain average participation in each age group. Fourth, although our interview outline was developed based on the TAM model and literature review, we did not pilot-test it in a small sample size to test validity and modify the interview outline. Finally, to ensure universality for potential users, we did not inquire about or assess participants’ technological experience, which could have influenced participants’ judgment of the perceived ease of use and perceived usefulness of the system. In future studies, participants’ technological experience could be assessed while keeping the general applicability of the system to better analyze the impact of technological experience on the acceptability of the system.
Conclusion
This study explored the acceptance of the video game-based swallowing function training system by dysphagia patients and healthcare providers. The results of the study showed that participants perceived high usefulness and ease of use of the video game and generally accepted the use of the video game for swallowing rehabilitation. As the demand for quality healthcare continues to expand, video game rehabilitation programs can be an interesting and intuitive way to improve clinical practice.
Supplemental Material
Supplemental material, sj-docx-1-dhj-10.1177_20552076241284830 for Technology acceptance of the video game-based swallowing function training system among healthcare providers and dysphagia patients: A qualitative study by Bohan Zhang, Ping Ding, Vivian Hui, Ka Po Wong and Yue Liu, Zihan Liu, Qian Xiao, Jing Qin in DIGITAL HEALTH
Supplemental material, sj-docx-2-dhj-10.1177_20552076241284830 for Technology acceptance of the video game-based swallowing function training system among healthcare providers and dysphagia patients: A qualitative study by Bohan Zhang, Ping Ding, Vivian Hui, Ka Po Wong and Yue Liu, Zihan Liu, Qian Xiao, Jing Qin in DIGITAL HEALTH
Acknowledgments
The authors thank all the patients, families, and healthcare providers who participated in the interviews.
Footnotes
Contributorship: BZ was involved in conceptualization, methodology, formal analysis, investigation, and writing—original draft. PD was involved in data curation and investigation.VH was involved in conceptualization, supervision, and writing—review and editing. KPW was involved in formal analysis and validation. YL was involved in investigation, project administration, resources, and writing—review and editing. ZL was involved in investigation and resources. QX was involved in funding acquisition, resources, supervision, and writing—review and editing. JQ was involved in supervision and writing—review and editing.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval: The study received approval from the Ethics Committee of the Beijing Xiaotangshan Hospital (LS20230720-1) and the Hong Kong Polytechnic University (HSEARS20230502007).
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Natural Science Foundation of China, (grant number No. 72174130).
Guarantor: QX.
ORCID iD: Bohan Zhang https://orcid.org/0000-0002-2165-9424
Supplemental material: Supplemental material for this article is available online.
References
- 1.Tulunay-Ugur OE, Eibling D. Geriatric dysphagia. Clin Geriatr Med 2018; 34: 183–189. [DOI] [PubMed] [Google Scholar]
- 2.Bhattacharyya N. The prevalence of dysphagia among adults in the United States. Otolaryngol Head Neck Surg 2014; 151: 765–769. [DOI] [PubMed] [Google Scholar]
- 3.Zheng M, Zhou S, Hur K, et al. Disparities in the prevalence of self-reported dysphagia and treatment among US adults. Am J Otolaryngol 2023; 44: 103774. [DOI] [PubMed] [Google Scholar]
- 4.Kawashima K, Motohashi Y, Fujishima I. Prevalence of dysphagia among community-dwelling elderly individuals as estimated using a questionnaire for dysphagia screening. Dysphagia 2004; 19: 266–271. [DOI] [PubMed] [Google Scholar]
- 5.Zhang M, Li C, Zhang F, et al. Prevalence of dysphagia in China: An epidemiological survey of 5943 participants. Dysphagia 2021; 36: 339–350. [DOI] [PubMed] [Google Scholar]
- 6.Huckabee ML, Flynn R, Mills M. Expanding rehabilitation options for dysphagia: Skill-based swallowing training. Dysphagia 2023; 38: 756–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Panebianco M, Marchese-Ragona R, Masiero S, et al. Dysphagia in neurological diseases: A literature review. Neurol Sci 2020; 41: 3067–3073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fang WJ, Zheng F, Zhang LZ, et al. Research progress of clinical intervention and nursing for patients with post-stroke dysphagia. Neurol Sci 2022; 43: 5875–5884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen KC, Jeng Y, Wu WT, et al. Sarcopenic dysphagia: A narrative review from diagnosis to intervention. Nutrients 2021; 13: 4043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones CA, Colletti CM, Ding MC. Post-stroke dysphagia: Recent insights and unanswered questions. Curr Neurol Neurosci Rep 2020; 20: 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Luker J, Lynch E, Bernhardsson S, et al. Stroke survivors’ experiences of physical rehabilitation: A systematic review of qualitative studies. Arch Phys Med Rehabil 2015; 96: 1698–1708.e10. [DOI] [PubMed] [Google Scholar]
- 12.Gustavsson M, Kjörk EK, Erhardsson M, et al. Virtual reality gaming in rehabilitation after stroke–user experiences and perceptions. Disabil Rehabil 2022; 44: 6759–6765. [DOI] [PubMed] [Google Scholar]
- 13.Nielsen AH, Kaldan G, Nielsen BH, et al. Intensive care professionals’ perspectives on dysphagia management: A focus group study. Aust Crit Care 2023; 36: 528–535. [DOI] [PubMed] [Google Scholar]
- 14.Speyer R, Sandbekkbråten A, Rosseland I, et al. Dysphagia care and management in rehabilitation: A national survey. J Clin Med 2022; 11: 5730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Griffiths MD, Kuss DJ, de Gortari ABO. Videogames as therapy: An updated selective review of the medical and psychological literature. Int J Priv Health Inf Manag 2017; 5: 71–96. [Google Scholar]
- 16.Bonnechère B, Jansen B, Omelina L, et al. The use of commercial video games in rehabilitation: A systematic review. Int J Rehabil Res 2016; 39: 277–290. [DOI] [PubMed] [Google Scholar]
- 17.Laver KE, Lange B, George S, et al. Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev 2017; 11: Cd008349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cassani R, Novak GS, Falk TH, et al. Virtual reality and non-invasive brain stimulation for rehabilitation applications: A systematic review. J Neuroeng Rehabil 2020; 17: 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baijens LW, Clavé P, Cras P, et al. European society for swallowing disorders—European union geriatric medicine society white paper: Oropharyngeal dysphagia as a geriatric syndrome. Clin Interv Aging 2016; 11: 1403–1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Melchiorre MG, Papa R, Quattrini S, et al. Integrated care programs for people with multimorbidity in European countries: eHealth adoption in health systems. BioMed Res Int 2020; 2020: 9025326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Athukorala RP, Jones RD, Sella O, et al. Skill training for swallowing rehabilitation in patients with Parkinson's disease. Arch Phys Med Rehabil 2014; 95: 1374–1382. [DOI] [PubMed] [Google Scholar]
- 22.Huckabee M-L, Mills M, Flynn R, et al. The evolution of swallowing rehabilitation and emergence of biofeedback modalities. Curr Otorhinolaryngol Rep 2023; 11: 144–153. [Google Scholar]
- 23.Calvillo-Arbizu J, Roa-Romero LM, Estudillo-Valderrama MA, et al. User-centred design for developing e-health system for renal patients at home (AppNephro). Int J Med Inf 2019; 125: 47–54. [DOI] [PubMed] [Google Scholar]
- 24.Ali EE, Chan SSL, Poh HY, et al. Design considerations in the development of app-based oral anticancer medication management systems: A qualitative evaluation of Pharmacists’ and Patients’ perspectives. J Med Syst 2019; 43: 63. [DOI] [PubMed] [Google Scholar]
- 25.Portz JD, Bayliss EA, Bull S, et al. Using the technology acceptance model to explore user experience, intent to use, and use behavior of a patient portal among older adults with multiple chronic conditions: Descriptive qualitative study. J Med Internet Res 2019; 21: e11604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Constantinescu G, Loewen I, King B, et al. Designing a mobile health app for patients with dysphagia following head and neck cancer: A qualitative study. JMIR Rehabil Assist Technol 2017; 4: e6319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gabbas M, Kim K. Gamified user interface design for dysphagia rehabilitation based on common mental models. Digital Library. https://dl.designresearchsociety.org/drs-conference-papers/drs2022/researchpapers/200/ (2022, accessed 10 December 2023).
- 28.Rodríguez A, Chover M, Boada I. Gamification and virtual reality for tongue rehabilitation. IEEE Access 2023; 11: 124975–124984. [Google Scholar]
- 29.Davis FD. A technology acceptance model for empirically testing new end-user information systems: Theory and results. Massachusetts Institute of Technology, Sloan School of Management, 1985. [Google Scholar]
- 30.McCaughan D, Sheard L, Cullum N, et al. Patients’ perceptions and experiences of living with a surgical wound healing by secondary intention: A qualitative study. Int J Nurs Stud 2018; 77: 29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007; 19: 349–357. [DOI] [PubMed] [Google Scholar]
- 32.Zhang J, Walji MF. TURF: Toward a unified framework of EHR usability. J Biomed Inform 2011; 44: 1056–1067. [DOI] [PubMed] [Google Scholar]
- 33.Zhang B, Guo C, Hui V, et al. Evaluating the effectiveness of video-game based swallowing function training in patients with dysphagia: Study protocol for a randomized controlled trial. Trials 2023; 24: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kang JH, Park RY, Lee SJ, et al. The effect of bedside exercise program on stroke patients with dysphagia. Ann Rehabil Med 2012; 36: 512–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mul K, Berggren KN, Sills MY, et al. Effects of weakness of orofacial muscles on swallowing and communication in FSHD. Neurology 2019; 92: e957–e963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carnaby GD, Harenberg L. What is “usual care” in dysphagia rehabilitation: A survey of USA dysphagia practice patterns. Dysphagia 2013; 28: 567–574. [DOI] [PubMed] [Google Scholar]
- 37.Robbins J, Kays SA, Gangnon RE, et al. The effects of lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehabil 2007; 88: 150–158. [DOI] [PubMed] [Google Scholar]
- 38.Crary MA. Chapter 10—Treatment for adults. In: Groher ME, Crary MA. (eds) Dysphagia. 2nd ed. St. Louis: Mosby, 2016, pp.207–240. [Google Scholar]
- 39.Liu J, Wang Q, Tian J, et al. Effects of chin tuck against resistance exercise on post-stroke dysphagia rehabilitation: A systematic review and meta-analysis. Front Neurol 2023; 13: 1109140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Park JS, Hwang NK. Chin tuck against resistance exercise for dysphagia rehabilitation: A systematic review. J Oral Rehabil 2021; 48: 968–977. [DOI] [PubMed] [Google Scholar]
- 41.Park J-S, An D-H, Oh D-H, et al. Effect of chin tuck against resistance exercise on patients with dysphagia following stroke: A randomized pilot study. NeuroRehabilitation 2018; 42: 191–197. [DOI] [PubMed] [Google Scholar]
- 42.Vasileiou K, Barnett J, Thorpe S, et al. Characterising and justifying sample size sufficiency in interview-based studies: Systematic analysis of qualitative health research over a 15-year period. BMC Med Res Methodol 2018; 18: 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rjoob MA, Rjoob KA. The correlation between cognitive function and dysphagia in stroke patients. Tunis Med 2022; 100: 342–345. [PMC free article] [PubMed] [Google Scholar]
- 44.Nguyen M, Fujioka J, Wentlandt K, et al. Using the technology acceptance model to explore health provider and administrator perceptions of the usefulness and ease of using technology in palliative care. BMC Palliat Care 2020; 19: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Malterud K. Qualitative research methods for medicine and health: An introduction. Oslo, Norway: University Press[Google Scholar], 2017. [Google Scholar]
- 46.Brooks J, McCluskey S, Turley E, et al. The utility of template analysis in qualitative psychology research. Qual Res Psychol 2015; 12: 202–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen HY, Boore JR. Translation and back-translation in qualitative nursing research: Methodological review. J Clin Nurs 2010; 19: 234–239. [DOI] [PubMed] [Google Scholar]
- 48.Nadal C, Sas C, Doherty G. Technology acceptance in Mobile health: Scoping review of definitions, models, and measurement. J Med Internet Res 2020; 22: e17256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang RY, Chopin A, Shibata K, et al. Action video game play facilitates “learning to learn”. Commun Biol 2021; 4: 1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yu RWL, Chan AHS. Meta-analysis of the effects of game types and devices on older adults-video game interaction: Implications for video game training on cognition. Appl Ergon 2021; 96: 103477. [DOI] [PubMed] [Google Scholar]
- 51.Peñuelas-Calvo I, Jiang-Lin LK, Girela-Serrano B, et al. Video games for the assessment and treatment of attention-deficit/hyperactivity disorder: A systematic review. Eur Child Adolesc Psychiatry 2022; 31: 5–20. [DOI] [PubMed] [Google Scholar]
- 52.Bediou B, Adams DM, Mayer RE, et al. Meta-analysis of action video game impact on perceptual, attentional, and cognitive skills. Psychol Bull 2018; 144: 77–110. [DOI] [PubMed] [Google Scholar]
- 53.Ruiz M, Moreno M, Girela-Serrano B, et al. Winning the game against depression: A systematic review of video games for the treatment of depressive disorders. Curr Psychiatry Rep 2022; 24: 23–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sajeev MF, Kelada L, Yahya Nur AB, et al. Interactive video games to reduce paediatric procedural pain and anxiety: A systematic review and meta-analysis. Br J Anaesth 2021; 127: 608–619. [DOI] [PubMed] [Google Scholar]
- 55.Lin HC, Chiu YH, Chen YJ, et al. Continued use of an interactive computer game-based visual perception learning system in children with developmental delay. Int J Med Inf 2017; 107: 76–87. [DOI] [PubMed] [Google Scholar]
- 56.Sun P-C, Tsai RJ, Finger G, et al. What drives a successful e-learning? An empirical investigation of the critical factors influencing learner satisfaction. Comput Educ 2008; 50: 1183–1202. [Google Scholar]
- 57.Padilla-Meléndez A, del Aguila-Obra AR, Garrido-Moreno A. Perceived playfulness, gender differences and technology acceptance model in a blended learning scenario. Comput Educ 2013; 63: 306–317. [Google Scholar]
- 58.Dünnebeil S, Sunyaev A, Blohm I, et al. Determinants of physicians’ technology acceptance for e-health in ambulatory care. Int J Med Inf 2012; 81: 746–760. [DOI] [PubMed] [Google Scholar]
- 59.Chock G, Perna G. Soul road: One solo doc's extensive EMR journey implementing an EMR is a long process fraught with obstacles, especially for a solo practitioner. Healthc Inform 2014; 31: 38–39. [PubMed] [Google Scholar]
- 60.Wildenbos GA, Peute L, Jaspers M. Facilitators and barriers of electronic health record patient portal adoption by older adults: A literature study. Stud Health Technol Inform 2017; 235: 308–312. [PubMed] [Google Scholar]
- 61.Rouidi M, Elouadi A, Hamdoune A. Acceptance and use of telemedicine technology by health professionals: Development of a conceptual model. Digital Health 2022; 8: 20552076221081693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Scott Kruse C, Karem P, Shifflett K, et al. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare 2018; 24: 4–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schwarz F, Ward J, Willcock S. E-Health readiness in outback communities: An exploratory study. Rural Remote Health 2014; 14: 2871. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-dhj-10.1177_20552076241284830 for Technology acceptance of the video game-based swallowing function training system among healthcare providers and dysphagia patients: A qualitative study by Bohan Zhang, Ping Ding, Vivian Hui, Ka Po Wong and Yue Liu, Zihan Liu, Qian Xiao, Jing Qin in DIGITAL HEALTH
Supplemental material, sj-docx-2-dhj-10.1177_20552076241284830 for Technology acceptance of the video game-based swallowing function training system among healthcare providers and dysphagia patients: A qualitative study by Bohan Zhang, Ping Ding, Vivian Hui, Ka Po Wong and Yue Liu, Zihan Liu, Qian Xiao, Jing Qin in DIGITAL HEALTH