Abstract
[Purpose] We aimed to examine factors at admission that are related to independence in stair climbing at discharge among patients with vertebral compression fractures. [Participants and Methods] The study included 179 female patients with vertebral compression fractures. A decision tree model was created to predict independence in stair climbing at discharge based on Dementia Scale-Revised, skeletal muscle mass index body mass index, grip strength, number of vertebral fractures, and number of injuries at admission. [Results] Analysis with the decision tree model showed that skeletal muscle mass index at admission, age, and grip strength were predictors for independence in stair climbing at discharge. [Conclusion] Patients with vertebral compression fractures who have a low skeletal muscle mass index and grip strength on admission may require assistance with stair climbing upon discharge.
Keywords: Vertebral compression fracture, Stair climbing, Interrelationship
INTRODUCTION
Furthermore, among Asian countries, Japan exhibits the highest prevalence of vertebral fractures1). Vertebral compression fractures, the most prevalent fragility fracture in the elderly, have demonstrated a higher injury rate in Asia than in other countries2). The prevalence of vertebral compression fractures in our country is increasing3, 4). Therefore, the number of patients with vertebral compression fractures requiring physical therapy is expected to continuously increase. Vertebral compression fractures are related to severe post-fracture pain that limits physical activity5). Physical activity in the elderly prevents cognitive decline; hence, the ability to be active is important in patients with vertebral compression fractures. However, many older people live in older houses, and depending on their living conditions, they may have many steps and stairs at the entrance. Studies conducted on community-dwelling older adults revealed that as their ability to ascend and descend stairs declines, they are less likely to go out6), decreased opportunities to go outdoors are associated with worse depressed mood and subjective health7, 8) and increased mortality risk9). Moreover, the elderly are at higher risk of falling when ascending and descending stairs10). For these reasons, the ability to ascend and descend stairs should be a focus of physical therapy.
Initial physical therapy assessment is crucial for predicting prognosis, planning treatment programs, and helping patients return home. However, the patient’s activities are limited by severe pain when a vertebral compression fracture is sustained. These disease-specific limitations of vertebral compression fractures make proper initial physical therapy evaluation and prognosis prediction difficult.
In recent years, several predictive studies have used Classification and Regression Tree (CART) analysis, which generates an easy-to-understand prediction11,12,13).
CART analysis involves decision criteria that are expressed in the form of trees. The analysis results are arranged hierarchically, starting with the factors most strongly associated with the dependent variable, enabling an easy understanding of the interactions between each factor. Therefore, the present study used CART analysis to investigate the factors that affect the ability to ascend and descend stairs at discharge in patients with vertebral compression fractures.
The results of this study would be useful to appropriately predict ability to ascend and descend stairs at discharge, that is otherwise difficult to assess due to acute pain.
PARTICIPANTS AND METHODS
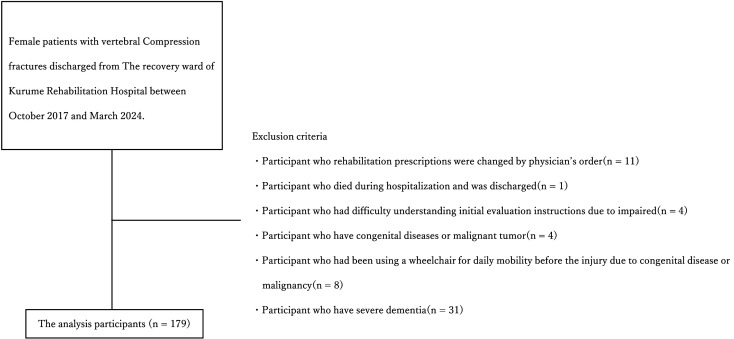
This study includes patients with vertebral compression fractures who were discharged from the recovery ward of Kurume Rehabilitation Hospital from October 2017 to March 2024. The participants were limited to females because of their higher vertebral compression fracture prevalence4). This study excluded patients who were transferred to other hospitals or wards due to the onset of severe pneumonia or cerebrovascular disease, including 11 whose rehabilitation prescriptions were changed by physician’s order, 1 who died during hospitalization and was discharged, 4 who had difficulty understanding initial evaluation instructions due to impaired consciousness or higher brain dysfunction, 4 who have congenital diseases or malignant tumors, 8 who had been using a wheelchair for daily mobility before the injury due to congenital disease or malignancy, and 31 who have severe dementia. Finally, the analysis included 179 participants (Fig. 1). Of the patients analyzed, 79 (44.1%) had vertebral compression fractures due to falls and 100 (55.9%) due to turning movements or activities of daily living (ADL). The median time from injury to hospitalization was 0–8 days (25th–75th percentile). The Ethics Committee and the Ethics Review Committee of our hospital (No. 24-003) approved this study.
Fig. 1.
Flow diagram of the study.
This retrospective cohort study obtained data, including age at admission, Hasegawa Dementia Scale-Revised (HDS-R), skeletal muscle mass index (SMI), body mass index (BMI), grip strength, number of vertebral fractures, location of vertebral fractures, and functional independence rating (FIM) at discharge, from electronic medical records.
The HDS-R is a 9-item, 30-point questionnaire, indicating higher cognitive function with higher scores and higher cognitive impairment with lower scores. The HDS-R was administered as early as possible after initiating rehabilitation, in the early hospitalization stages.
An In Body S10 (In Body, Inc., Tokyo, Japan) to measure muscle mass in the left and right upper extremities, lower extremities, and trunk SMI, calculated by dividing the sum of muscle mass in the left and right upper and lower extremities by the square of height (m), was used to measure SMI at admission. BMI was obtained by dividing weight (kg) at admission by the square of height (m).
Grip strength was measured at the time of admission using a Smedley grip strength meter (T.K.K. 5401, Takei Rika Kikai Co., Niigata, Japan). The values obtained were reliable14). Measurements were taken twice on each side in the sitting position, and the maximum value was used.
The history of vertebral compression fracture injury was categorized into those who had a first vertebral compression fracture at admission and those who had a history of vertebral compression fracture injury before admission.
The number of vertebral compression fractures was categorized into those with one vertebral compression fracture at admission and those with multiple vertebral compression fractures.
Vertebral fracture sites at admission were classified as thoracic, lumbar, and both thoracic and lumbar fractures.
The assigned physical therapist, occupational therapist, and nurse scored FIM at discharge15). Patients were categorized into two groups based on FIM staircase items at discharge for statistical analysis.
Participants who scored ≥6 points on the stairs were categorized into the independent group and those who scored ≤5 points were classified into the group requiring assistance.
Comparisons between the two groups of participants followed previous studies16).
The χ2 test was used to compares the number of vertebral compression fractures received, the number of vertebral fractures, and the location of vertebral fractures. Mann–Whitney’s U test was used to compare age at admission, HDS-R, SMI, BMI, and grip strength. Additionally, effect sizes were calculated for each item, and effect size φ was calculated in the case of the χ2 test. The effect size φ was interpreted as small, medium, and large for effect sizes of <0.1–0.3, >0.3–0.5, and >0.5, respectively. The effect size φ was interpreted as small, medium, and large at <0.1–0.3, >0.3–0.5, and >0.5, respectively. The effect size r was calculated using the test statistic Z in the case of the Mann–Whitney U test. A decision tree analysis was performed with the ability to climb stairs at discharge as the dependent variable and the items that demonstrated significant differences in the comparison of the two groups as independent variables. The Gini coefficient was utilized as the criterion for branching. The maximum depth of the tree was defined as 5, and the minimum number of cases before and after analysis was 10 and 2, respectively. Statistical Package for the Social Sciences version 28.0 (IBM, Tokyo, Japan) was used for statistical analysis, with a significance level of 5%. The results of the decision tree analysis revealed that the correct classification rate was 80.4%, with an error rate of 0.03%. Age at admission, SMI, and grip strength were identified as factors associated with independence in stair climbing at discharge. In this model, SMI at admission was the first option in the first tier and was categorized into two groups of approximately 4.48 kg/m2. Patients were divided into two groups in the second tier based on age of 90.5 years if the SMI on admission was >4.48 kg/m2.
RESULTS
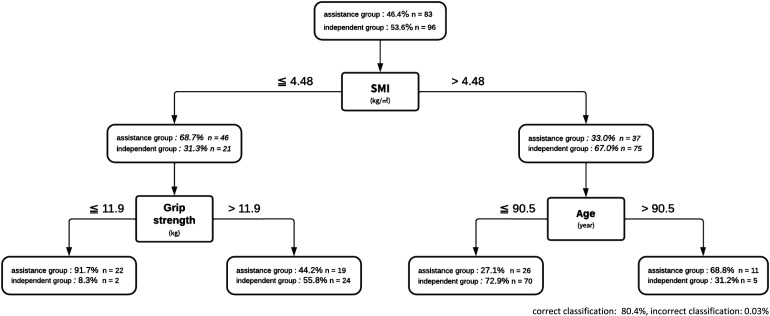
The age of 179 participants was 77.0–87.0 years (25th–75th percentile), with a median age of 85.0 years. At discharge, 96 (53.6%) patients ascend and descend stairs independently, whereas 83 (46.4%) required assistance. Comparing patients who ascend and descend stairs independently with those who required assistance, significant differences were found in age at admission, HDS-R, SMI, grip strength, and the number of vertebral compression fracture injuries (Table 1). Decision tree analysis identified age at admission, SMI, and grip strength as factors associated with independence in stair climbing at discharge. In this model, SMI at admission was the first option in tier 1, and was classified into two groups of approximately 4.48 kg/m2. If the SMI on admission was greater than 4.48 kg/m2, patients were divided into two groups based on age 90.5 years in the second tier. The correct classification rate was 80.4%, and the incorrect classification rate was 0.03%. Age at admission, SMI, and grip strength were selected as factors associated with independence in stair climbing at discharge. In this model, patients were categorized into two groups based on SMI on admission of 4.48 kg/m2. Patients were categorized into a second group based on their age on admission of 90.5 years if the SMI on admission was >4.48 kg/m2. Patients were divided into two groups based on their grip strength of 11.9 kg on admission if the SMI on admission was <4.48 kg/m2 (Fig. 2).
Table 1. Characteristics of the analyzed participants.
| Overall | Independent group | Assistance group | Effect size | |
| (n=179) | (n=96) | (n=83) | ||
| Age‡ (years) | 85.0 (80.0–89.0) | 83.0 (77.0–87.0) | 87.0 (82.0–91.0)** | −0.30 |
| HDS-R‡ (points) | 25.0 (19.0–28.0) | 26.0 (21.0–29.0) | 21.0 (18.0–26.0)** | 0.40 |
| SMI‡ (kg/m2) | 4.7 (4.1–5.4) | 5.0 (4.5–5.1) | 4.4 (3.9–5.1)** | 0.31 |
| BMI‡ (kg/m2) | 21.0 (18.7–23.6) | 21.3 (19.0–24.1) | 20.0 (18.0–22.6) | 0.11 |
| Grip strength‡ (kg) | 15.9 (12.7–19.9) | 17.6 (14.1–20.5) | 13.6 (11.3–18.4)** | 0.36 |
| History of vertebral compression fracture injury | 179 (130:49) | 96 (76:20) | 83 (54:29)* | 0.17 |
| (first fracture: re-fracture)† (n) | ||||
| Number of vertebral fractures | 179 (145:33) | 96 (80:16) | 83 (65:18) | 0.02 |
| (single: multiple)† (n) | ||||
| Vertebral fracture sites | 179 (71:90:18) | 96 (41:48:7) | 83 (30:42:11) | 0.02 |
| (cspine: lumbar spine: both thoracic and lumbar spine)† (n) |
Median (1st quartile–3rd quartile), †χ2 test, ‡Mann–Whitney U test, HDS-R: Hasegawa Dementia Scale-Revised; SMI: skeletal muscle mass index; BMI: body mass index, *p<0.05, **p<0.01.
Fig. 2.
The flowchart created by the Classification and Regression Tree (CART) analysis.
DISCUSSION
SMI, grip strength, and age at admission were as indicators of stair climbing ability at discharge in this study. On the other hand, HDS-R, BMI, number of vertebral fractures, and vertebral fracture location at admission were not selected in the decision tree analysis. In other words, these unselected factors were suggested to have low prognostic contribution for stair climbing ability at discharge. The results of this study revealed that independence in stair climbing at discharge is achieved by having an SMI of at least 4.48 kg/m2 at admission and an age of <90.5 years at admission. Conversely, approximately 70% of patients with low SMI at admission required assistance in climbing stairs at discharge. Furthermore, patients with a grip strength of <11.9 kg at admission may require assistance in ascending and descending stairs at discharge.
Daniel et al.17) reported, in a meta-analysis, that a decrease in muscle mass predicts a decrease in ADLs and instrumental ADLs. A study of male patients who had a stroke and admitted to a recovery unit revealed18) that sarcopenia at admission was associated with FIM motor items at discharge. The results of the present study are consistent with the results of these studies and indicate that SMI at admission is a predictor of functional prognosis. Chen et al.19) calculated a cut-off value for SMI, which is a measure of sarcopenia in community-dwelling older adults, as 5.7 kg/m2 for women. The criterion value for the present study was 4.48 kg/m2, which was slightly lower than the criterion value for SMI to determine sarcopenia. The study participants exhibited a median SMI of 4.7 kg/m2, which is generally low. Vertebral compression fracture injury causes severe pain that decreases activity and may present with disuse syndrome. Therefore, we infer that the SMI at admission, which was the result of this study, demonstrates a lower criterion value than in previous studies.
Furthermore, this study revealed that in addition to SMI at admission, grip strength at admission was associated with independence in stair climbing at discharge. Grip strength is an indicator of whole-body muscle strength even among the elderly20, 21) and is a predictor of physical function, risk of death, and development of complications in the elderly22). The baseline value of grip strength associated with the ability to climb stairs at discharge from the hospital was 11.9 kg. Hashimoto et al.23) revealed preoperative grip strength as a predictor of stair climbing ability in female patients with total knee replacement (mean age: 75.6 ± 7.2 years), with a cut-off value of 19.0 kg to discriminate stair climbing independence. The median grip strength of the participants in this study was 15.9 (12.7–9.9) kg, which was lower than the cut-off of Hashimoto et al. Furthermore, the median age of the participants was 85 years (77.0–87.0), slightly older than in previous studies. Moreover, participants’ SMI was lower overall, resulting in lower cut-off value for grip strength than in previous studies. However, grip strength was identified as a prognostic predictor of the ability to ascend and descend stairs, similar to previous studies.
In summary, we predicted that patients with SMI of <4.48 kg/m2 and grip strength of 11.9 kg at admission would require assistance in stair climbing at discharge. SMI indicates muscle mass in the extremities19), and grip strength is associated with muscle strength20, 21). Furthermore, progressive loss of muscle mass reduces muscle strength24). This may therefore hinder ADL improvement. Therefore, physical therapy that focuses on muscle mass and strength needs to be developed for the ability to climb stairs at discharge. Preventing disuse syndrome in patients with vertebral compression fractures is especially important, as they are prone to inactivity due to post-injury pain and activity limitation. Furthermore, early home environment investigation and considering handrail installation and step elimination will help ensure opportunities to go outside in life after discharge even if the SMI at admission is >4.48 kg/m2 and if the patient is >90 years old as well as those with low SMI and grip strength at admission. In this study, a decision tree model was obtained for patients with vertebral compression fractures to determine their independence level in stair climbing at discharge. This decision tree model selected SMI at admission at the first place, followed by age and grip strength, as the predictors of independence in stair climbing at discharge. Various factors are associated with the ability to ascend and descend stairs at discharge in patients with vertebral compression fractures. Therefore, it is significant that this study used decision tree analysis to examine factors associated with the ability to ascend and descend stairs at the time of hospital discharge.
This study has several limitations. First, psychological aspects, such as self-efficacy and pain25, 26), which were not included in the study’s endpoints, influenced stair climbing. Second, the study was conducted at a single site and warrants further validation.
Conflict of interest
No potential conflict of interest was reported by the authors.
REFERENCES
- 1.Kwok AW, Leung JC, Chan AY, et al. : Prevalence of vertebral fracture in Asian men and women: comparison between Hong Kong, Thailand, Indonesia and Japan. Public Health, 2012, 126: 523–531. [DOI] [PubMed] [Google Scholar]
- 2.Bow CH, Cheung E, Cheung CL, et al. : Ethnic difference of clinical vertebral fracture risk. Osteoporos Int, 2012, 23: 879–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kadowaki E, Tamaki J, Iki M, et al. : Prevalent vertebral deformity independently increases incident vertebral fracture risk in middle-aged and elderly Japanese women: the Japanese Population-based Osteoporosis (JPOS) Cohort Study. Osteoporos Int, 2010, 21: 1513–1522. [DOI] [PubMed] [Google Scholar]
- 4.Horii C, Asai Y, Iidaka T, et al. : Differences in prevalence and associated factors between mild and severe vertebral fractures in Japanese men and women: the third survey of the ROAD study. J Bone Miner Metab, 2019, 37: 844–853. [DOI] [PubMed] [Google Scholar]
- 5.Kendler DL, Bauer DC, Davison KS, et al. : Vertebral fractures: clinical importance and management. Am J Med, 2016, 129: 221.e1–221.e10. [DOI] [PubMed] [Google Scholar]
- 6.Edwards N, Dulai J: Examining the relationships between walkability and physical activity among older persons: what about stairs? BMC Public Health, 2018, 18: 1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fujita K, Fujiwara Y, Chaves PH, et al. : Frequency of going outdoors as a good predictors for incident disability of physical function as well as disability recovery in community-dwelling older adults in rural Japan. J Epidemiol, 2006, 16: 261–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen-Mansfield J, Shmotkin D, Hazan H: Homebound older persons: prevalence, characteristics, and longitudinal predictors. Arch Gerontol Geriatr, 2012, 54: 55–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Inoue K, Shono T, Matsumoto M: Absence of outdoor activity and mortality risk in older adults living at home. J Aging Phys Act, 2006, 14: 203–211. [DOI] [PubMed] [Google Scholar]
- 10.Startzell JK, Owens DA, Mulfinger LM, et al. : Stair negotiation in older people: a review. J Am Geriatr Soc, 2000, 48: 567–580. [DOI] [PubMed] [Google Scholar]
- 11.Skidmore ER, Rogers JC, Chandler LS, et al. : Dynamic interactions between impairment and activity after stroke: examining the utility of decision analysis methods. Clin Rehabil, 2006, 20: 523–535. [DOI] [PubMed] [Google Scholar]
- 12.Hiraoka S, Maeshima S, Okazaki H, et al. : Factors necessary for independent walking in patients with thalamic hemorrhage. BMC Neurol, 2017, 17: 211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fujita T, Ohashi Y, Kurita M, et al. : Functions necessary for gait independence in patients with stroke: a study using decision tree. J Stroke Cerebrovasc Dis, 2020, 29: 104998. [DOI] [PubMed] [Google Scholar]
- 14.Mehmet H, Yang AW, Robinson SR: Measurement of hand grip strength in the elderly: a scoping review with recommendations. J Bodyw Mov Ther, 2020, 24: 235–243. [DOI] [PubMed] [Google Scholar]
- 15.Keith RA, Granger CV, Hamilton BB, et al. : The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil, 1987, 1: 6–18. [PubMed] [Google Scholar]
- 16.Kurita M, Fujita T, Kasahara R, et al. : Cutoff value for a nutritional indicator related to gait independence in elderly fracture patients: a preliminary study. Phys Ther Res, 2021, 25: 26–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang DX, Yao J, Zirek Y, et al. : Muscle mass, strength, and physical performance predicting activities of daily living: a meta-analysis. J Cachexia Sarcopenia Muscle, 2020, 11: 3–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Matsushita T, Nishioka S, Taguchi S, et al. : Sarcopenia as a predictor of activities of daily living capability in stroke patients undergoing rehabilitation. Geriatr Gerontol Int, 2019, 19: 1124–1128. [DOI] [PubMed] [Google Scholar]
- 19.Chen LK, Woo J, Assantachai P, et al. : Asian Working Group for Sarcopenia: 2019 Consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc, 2020, 21: 300–307.e2. [DOI] [PubMed] [Google Scholar]
- 20.Meessen JM, Fiocco M, Tordoir RL, et al. : Association of handgrip strength with patient-reported outcome measures after total hip and knee arthroplasty. Rheumatol Int, 2020, 40: 565–571. [DOI] [PubMed] [Google Scholar]
- 21.Strandkvist V, Larsson A, Pauelsen M, et al. : Hand grip strength is strongly associated with lower limb strength but only weakly with postural control in community-dwelling older adults. Arch Gerontol Geriatr, 2021, 94: 104345. [DOI] [PubMed] [Google Scholar]
- 22.Bohannon RW: Hand-grip dynamometry predicts future outcomes in aging adults. J Geriatr Phys Ther, 2008, 31: 3–10. [DOI] [PubMed] [Google Scholar]
- 23.Hashimoto S, Hatayama K, Terauchi M, et al. : Preoperative hand-grip strength can be a predictor of stair ascent and descent ability after total knee arthroplasty in female patients. J Orthop Sci, 2020, 25: 167–172. [DOI] [PubMed] [Google Scholar]
- 24.Barbat-Artigas S, Rolland Y, Zamboni M, et al. : How to assess functional status: a new muscle quality index. J Nutr Health Aging, 2012, 16: 67–77. [DOI] [PubMed] [Google Scholar]
- 25.Suzuki Y, Iijima H, Aoyama T: Pain catastrophizing affects stair climbing ability in individuals with knee osteoarthritis. Clin Rheumatol, 2020, 39: 1257–1264. [DOI] [PubMed] [Google Scholar]
- 26.Whitchelo T, McClelland JA, Webster KE: Factors associated with stair climbing ability in patients with knee osteoarthritis and knee arthroplasty: a systematic review. Disabil Rehabil, 2014, 36: 1051–1060. [DOI] [PubMed] [Google Scholar]