Abstract
AIM
To understand the current situation of parental perspectives, knowledge, and practices concerning myopia prevention and control for both pre- and school-aged children.
METHODS
This study was a cross-sectional survey that involved children aged 0 to 15y and their parents. Participants were required to respond to an online questionnaire by scanning a quick response (QR) code. The questionnaire consisted of 25 tick-box questions and was open to response from December 22, 2022, to January 5, 2023. The dioptric traits of the children, the visual status and educational background of the parents, the parental perspectives towards myopia and its risks, and the parents' knowledge and practices related to myopia prevention and control were recorded and measured. The Chi-square test and binomial logistic regression were used for statistics.
RESULTS
Totally 350 parents responded to the questionnaire. The prevalence and severity of myopia among the surveyed children exhibited a positive correlation with advancing age (P<0.001 and P=0.004, respectively). Nearly half of parents with myopic children considered myopia did not pose any health threat and could be effectively corrected (P<0.001). Parents who held master's or doctoral degree demonstrated a better understanding of children's vision standards for each age group (P=0.001), and 31.63% of them could undergo initial vision screening for their children during the age of 0 to 3y while parents with bachelor's degree (34.04%) and below (32.43%) mainly initiated the vision examination for their children at the age of 4 to 6y (P=0.05). Parents with master's or doctoral degree also exhibited more rational practices concerning outdoor time (P=0.048) and sleep time (P=0.044). No other significant discrepancy among the different educational groups in additional conceptions of myopia, such as hyperopia reserve, axis length, and corneal curvature alterations. Most parents preferred to employ conventional interventions, such as enhancing indoor lighting condition (80.00%) and ensuring appropriate reading posture and distance (71.71%).
CONCLUSION
The current status of parental knowledge and practices about myopia prevention and control remains outdated and deficient. The administrative department should implement efficacious and adaptable measures to enhance parental awareness and foster their commitment towards myopia prevention and control.
Keywords: myopia, myopia prevention and control, parental perspectives, pre- and school-aged children
INTRODUCTION
Myopia is widely acknowledged as a significant public health concern due to its escalating global prevalence. According to the World Health Organization, it is projected that nearly 5 billion individuals worldwide may be myopic by 2050[1]. This refractive error is particularly prevalent in China and other Asian countries[2]–[3], with a higher incidence observed during childhood and adolescence. Epidemiological investigations have revealed that in 2020, the overall prevalence of myopia among children and adolescents in China was 52.7%, with approximately 10% classified as highly myopia, as reported in an official online publication[4]. Singaporean school children also have experienced a notable surge in myopia, with a significant incidence rate of 62% at the age of 12[5]. Worse, a lower age of myopia onset has been observed in recent years[4], resulting in an extended duration for the progression of myopia. Considering the potential complications of high myopia such as fundus retinopathy and maculopathy, which can lead to severe irreversible visual impairment and even blindness[6]–[7], the presence of myopia in pre- and school-aged children is a major medical and societal issue that requires immediate attention and control.
Currently, the remarkable prevalence of myopia among school-aged children has garnered great attention from the pertinent Chinese authorities. A collaborative effort has consequently been made to establish a network system for myopia prevention and control within the hospital-school-community framework[8]–[9]. However, it is disheartening to note that there is a lack of parental awareness and comprehension regarding visual health in their pre- or school-aged children in recent initiatives aimed at controlling myopia. Given these limitations among parents, there may be a diminished emphasis on modifying myopic behavior and accepting optical and pharmacological interventions to mitigate the progression of myopia. Considering the significant influence parents have on the lifestyle choices of children, it should not underestimate the importance of parents in the prevention and control of early-stage myopia. The present research suggests that the attitudes and behavior of parents can have a subtle impact on children's visual care and the risk of developing myopia. Liu et al[10] found that detecting myopia in children prompted parents to adopt beneficial behaviors to prevent it from worsening. Other studies have shown that parents with myopia or who viewed myopia as a health risk were more likely to limit their children's screen time[11], and children whose parents ensured them sufficient sleep had a reduced risk of developing myopia[12]. Furthermore, according to the findings of a cross-sectional study conducted by He et al[13], left-behind children exhibited a greater prevalence of vision-threatening behaviors compared to their counterparts residing with their parents.
The role of parental influence was emphasized during the COVID-19 pandemic[14], as home confinement measures restricted children's access to outdoor activities, resulting in prolonged periods of online learning. Without adequate parental intervention to adjust their children's reading habits and encourage visual health exercises, there is a notable risk of an increase in the prevalence or advancement of myopia. Zhang et al[15] observed a consistent myopia prevalence among 20 527 screened children aged 6 to 8y in Hong Kong from 2015 to 2019. However, in 2020 and 2021, the prevalence notably escalated to 28.8% and 36.2% respectively. Similarly, Wang et al[16] discovered a substantial increase in the mean spherical equivalent refraction of 325 443 children aged 6 to 8y in 2021 compared to the previous year.
Parents should be the first line of defense for the prevention and control of myopia. The significance of parental involvement in the prevention and control of myopia is paramount and irreplaceable by governmental, medical, or educational entities. To a great extent, parents' cognition of myopia determines the prevention and cure strategy of children's myopia. However, the widespread implementation of family-based myopia prevention and control education in China faces challenges due to the disparities of region, educational attainment, socioeconomic status, and other pertinent factors. Li et al[17] employed mobile phone short messaging service, a widely used communication tool, to remind parents about the importance of controlling children's myopia. This approach introduces a novel avenue for remotely managing myopia in school-aged children during non-school hours, but the lack of pertinent knowledge has hindered the full mobilization of parental involvement. Existing researches on myopia prevention and control among school-aged children were either geographically restricted or lacked a comprehensive perspective[18]–[19]. Furthermore, there is a dearth of surveys investigating parents' understanding and implementation of strategies for managing children's myopia.
To thoroughly evaluate the current level of parental understanding and implementation of knowledge and strategies related to myopia prevention and control, with the objective of efficiently disseminating tailored information to parents, a survey was conducted among parents in China.
SUBJECTS AND METHODS
Ethical Approval
The present study received approval from the Ethical Committee of the Beijing Hospital of Traditional Chinese Medicine (No.2022BL05-001-01) and adhered to the principles outlined in the Declaration of Helsinki. Before participation, participants were provided with a comprehensive explanation regarding the nature and objectives of the research, and their informed consent was obtained through an online platform. Furthermore, participants were guaranteed anonymity in completing the questionnaire, and strict confidentiality measures were implemented to safeguard their individual results.
Questionnaires and Participants
This was a cross-sectional study in which parents of children aged 0 to 15y were recruited as the respondents, and an online survey questionnaire was distributed from December 22, 2022, to January 5, 2023. The questionnaire was designed by ophthalmology clinicians, drawing upon previous clinical data and literature. To facilitate participation, a quick response (QR) code was generated through an online questionnaire platform (https://www.wjx.cn) and widely disseminated among social media groups of parents for online responses. The survey encompassed four primary sections: the dioptric traits of the children, the visual status and educational background of the parents, the parental perspectives towards myopia and its risks, and the parents' knowledge and practices related to myopia prevention and control. The questionnaire consisted of a total of 25 tick-box questions. To ensure the quality of the questionnaire, careful evaluation and optimization were conducted to eliminate leading, confusing, or double-barreled questions. Furthermore, each question was made mandatory to guarantee complete data collection, and the survey system restricted the use of the same IP address to only one submission.
Parents of 0- to 15-year-old children who had digital devices that could scan the QR code online and were willing to participate were enrolled in our research. The exclusion criteria were 1) parents who live in different places with their children for a long time (more than half a year); 2) parents with severe mental disorders and who could not have access to smartphones; 3) parents who did not consent to participate.
Statistical Analysis
In this study, the survey data were exported as Microsoft EXCEL sheets and screened for evident errors. Data analysis was conducted using IBM SPSS 29.0. The counting data were expressed as n (%), and univariate analysis of categorical variables was performed using the R×C contingency table of the Chi-square test. The correlation between the current status of myopia in pre- and school-aged children and parental knowledge and practices of myopic control was examined through binomial logistic regression. The values of relevant research factors can be found in Table 1. A significance level of P<0.05 was utilized for all statistical analyses conducted.
Table 1. Valuation of factors related to myopia prevention and control knowledge and practices.
| Factors | Valuation |
| Is your child presently experiencing myopia? (Children with myopia) |
No=0; Yes=1. |
| In your option, is myopia detrimental to the visual health of children? (Parents attitudes towards myopia risks) |
Indeed, it poses significant risks, particularly in cases of high myopia, which may lead to retinopathy, maculopathy, and even blindness (It poses significant risks + high myopia may lead to irreversible fundus lesions) =0; Indeed, there are certain risks involved, although myopia correction surgery can serve as a potential “cure” (It poses certain risks + could be “cured”) =1; No, it does not entail any risks and can be easily rectified through the use of spectacles (It does not pose any risks) =2. |
| Have you ever actively pursued knowledge regarding the prevention and control of myopia in children? | Demonstrate a strong commitment to acquiring knowledge on myopia prevention and control through extensive engagement with ophthalmology books, articles, pictures, videos, and seeking professional consultations =0; Possess limited knowledge and have not actively sought to understand =1; Lack any knowledge or understanding in this area =2. |
| Do you know the visual acuity standard of each age group? | Yes=0; No=1. |
| Can you differentiate between myopia and “pseudomyopia”? | Yes=0; No=1. |
| Have you ever closely monitored the developmental progression of your children's axis length and corneal curvature? (Attention to children's axis length development and corneal curvature changes) |
Devoted significant attention and conducted regular examinations (Paid significant attention) =0; Paid minimal attention, only conducting examinations upon the recommendation of a doctor (Paid minimal attention) =1; Neglected to pay attention altogether =2. |
| Are you familiar with the concept of hyperopia reserve? | I possess a thorough understanding of it =0; I have some knowledge about it =1; I have heard of it before, but do not possess a comprehensive understanding =2; I am entirely unfamiliar with it =3. |
| When did you first bring your child for a visual examination or optometry? (The age at which child's vision examination or optometry was first performed) |
0-3y =0; 4-6y =1; 7-9y =2; 10-15y =3; No initiative examination besides the school-organized =4. |
| Do you consistently bring your child for routine visual examinations or optometry? (Have regular vision examinations or optometry for children or not) |
Consistently undergo examinations and establish a dioptric development profile (Have regular examination + established a dioptric development profile) =0; Consistently undergo examinations without establishing a dioptric development profile (Have regular examination without a dioptric development profile) =1; Only check if the child experiences a decline in vision =2; Have never taken your child for a visual examination or optometry appointment (Have never taken their child for a visual examination) =3. |
| What is the cumulative duration of your child's engagement with digital devices on a daily basis, excluding online educational activities? (The total duration of digital devices for children per day, except for e-learning) |
No additional usage =0; <1h=1; 1-3h=2; >3h=3. |
| What is the total duration of time that your child spends engaged in outdoor activities on a daily basis? (The total duration of outdoor activities for children per day) |
>3h=0; 1-3h=1; <1h=2. |
| What is the total duration of sleep for your child within a 24-hour period? (The total duration of sleep for children per day) |
>10h=0; 9-10h=1; 8-9h=2; <8h=3. |
The italic text in parentheses is an abbreviation of the sentence and is intended to be better illustrated in Figure 2 forest plot.
RESULTS
Demographic Characteristics of Study Participants
The survey yielded a total of 350 valid questionnaires completed by parents or guardians. Among these questionnaires, it indicated that approximately 69.14% of communities or schools had implemented scientific dissemination initiatives to promote knowledge regarding myopia prevention and control. Among the households surveyed, there were a total of 198 boys and 152 girls. Of these, 73.43% were primarily cared for by their parents, while 23.43% received care from their grandparents and 3.14% were attended to by nurses or other family members when their parents work away from home in the daytime. The predominant age group of the children was 7 to 9y, comprising 161 individuals. Additionally, there were 114 preschool-aged children (including 27 children aged 0 to 3y and 87 children aged 4 to 6y) and 75 higher grade school children (consisting of 30 children aged 10 to 12y and 45 children aged 13 to 15y). Totaly 81 children (23.14%) in this survey exhibited myopia according to their parents' responses.
For the parents of children, a mere 64 individuals (18.29%) were nonmyopic, while the remaining parents, either singularly or collectively, were myopic, with proportions of 53.71% and 28.00% respectively. Out of the total 350 parents who participated in this study, 31.71% possessed a high school education or lower, 40.29% held a bachelor's degree, and 28.00% possessed a master's or doctoral degree. The baseline characteristics of both the children and parents involved in this study are presented in Table 2.
Table 2. Demographic characteristics of study participants.
| Characteristics | Numbers (n=350) |
| Gender of children | |
| Male | 198 (56.57) |
| Female | 152 (43.43) |
| Age group of children | |
| 0-3y | 27 (7.71) |
| 4-6y | 87 (24.86) |
| 7-9y | 161 (46) |
| 10-12y | 30 (8.57) |
| 13-15y | 45 (12.86) |
| Family caretaker for children | |
| Parents | 257 (73.43) |
| Grandparents | 82 (23.43) |
| Nurses or other family members | 11 (3.14) |
| Children with myopia | |
| Yes | 81 (23.14) |
| No | 269 (76.86) |
| Parents with myopia, n | |
| 0 | 64 (18.29) |
| 1 | 188 (53.71) |
| 2 | 98 (28.00) |
| Parents' educational level | |
| High school or below | 111 (31.71) |
| Bachelor's degree | 141 (40.29) |
| Master's or doctoral degree | 98 (28.00) |
n (%)
Visual Status and Myopia Correction of Children in Pre- and School-age
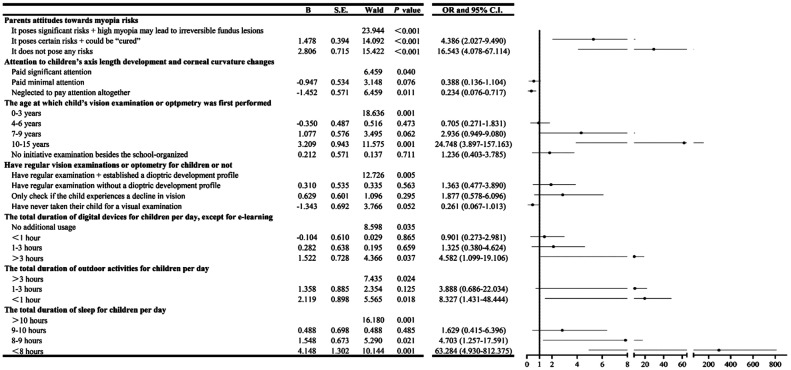
There was a significant difference in myopia prevalence among different age groups of children (P<0.001), with rates increasing as age increased. The highest rate was seen in children aged 13 to 15y (about 88.89%). The severity of myopia also increased with age (P=0.004; Table 3), and the age at which myopia first appeared was getting younger (Figure 1). Regarding myopia correction for children, a majority of parents (55.56%) still favored conventional spectacles as their first choice. Meanwhile, there has been a growing adoption of alternative methods such as defocus incorporated multiple segments (DIMS) spectacles and orthokeratology lenses (OK lenses), albeit in smaller proportions (20.99% and 4.94% respectively). It is noteworthy that 18.52% of parents expressed reluctance in providing glasses for their myopic children with diopters ranging from -0.50 to -3.00 D (Table 3). During the COVID-19 Era, about 53.71% of children encountered diverse levels of visual acuity impairment, among which 11.43% experienced significant vision deterioration, with a particular concentration observed among school-aged children aged 6y and above (Table 3).
Table 3. Visual status and myopia correction of children in pre- and school-age.
| Myopia status of pre- and school-age children | Age group |
Total | χ 2 | P | ||||
| 0-3y | 4-6y | 7-9y | 10-12y | 13-15y | ||||
| Children with myopia | 158.916 | <0.001 | ||||||
| Yes | 0 | 4 (4.94)b | 21 (25.93)b | 16 (19.75)b | 40 (49.38)b | 81 (23.14)a | ||
| No | 27 (10.04)c | 83 (30.86)c | 140 (52.04)c | 14 (5.20)c | 5 (1.86)c | 269 (76.86)a | ||
| Dioptric level of myopia, D | 19.343 | 0.004 | ||||||
| -0.50 to -3.00 | — | 4 (100.00)d | 20 (95.24)d | 14 (87.50)d | 22 (55.00)d | 60 (74.07)b | ||
| -3.25 to -6.00 | — | 0 | 1 (4.76)d | 2 (12.50)d | 13 (32.50)d | 16 (19.75)b | ||
| >-6.00 | — | 0 | 0 | 0 | 5 (12.50)d | 5 (6.17)b | ||
| Correction of myopia refraction error | 28.908 | <0.001 | ||||||
| OK lenses | — | 3 (75.00)e | 0 | 1 (25.00)e | 0 | 4 (4.94)b | ||
| DIMS spectacles | — | 0 | 6 (35.29)e | 3 (10.34)e | 8 (47.06)e | 17 (20.99)b | ||
| Ordinary spectacles | — | 0 | 9 (20.00)e | 8 (17.78)e | 28 (62.22)e | 45 (55.56)b | ||
| Uncorrected | — | 1 (6.67)e | 6 (40.00)e | 4 (26.67)e | 4 (26.67)e | 15 (18.52)b | ||
| Vision decline during COVID-19 pandemic | 51.605 | <0.001 | ||||||
| No discernible decline | 21 (77.78)d | 50 (57.47)d | 80 (49.69)d | 7 (23.33)d | 4 (8.89)d | 162 (46.29)a | ||
| Slight decline | 6 (22.22)d | 30 (34.48)d | 66 (40.99)d | 16 (53.33)d | 30 (66.67)d | 148 (42.29)a | ||
| Substantial decline | 0 | 7 (8.05)d | 15 (9.32)d | 7 (23.33)d | 11 (24.44)d | 40 (11.43)a | ||
aA proportion of all 350 surveyed children; bA proportion of all 81 children with myopia; cA proportion of all 269 children without myopia; dA proportion in each age group; eA proportion in each “correction of myopia refraction error” group. OK lenses: Orthokeratology lenses; DIMS spectacles: Defocus incorporated multiple segments spectacles.
n (%)
Figure 1. The age of myopia onset in pre- and school-aged children.
Parental Perspectives on Myopia and Myopic Risk in Children of Pre- and School-Age
A Chi-square test was conducted to investigate the correlation between the myopic status of children or parents and the parental attitude towards myopia and myopic risk. It revealed that most parents exhibited a heightened concern towards myopia, irrespective of whether their children or they themselves were myopic. There was no statistical difference (P=0.144 and P=0.703, respectively). Interestingly, a majority of parents (78.81%) with nonmyopic children held the belief that myopia posed a potential risk to their children's visual health, while nearly half of parents with myopic children expressed the view that myopia did not pose any health threat and could be effectively corrected through the use of corrective measures such as glasses, contact lenses, or laser refractive surgery (P<0.001). Such a significant difference was not seen between each parent's myopic status cohort (P=0.183; Table 4).
Table 4. Parental perspectives on myopia and myopic risk in children of pre- and school-age.
| Relevant status of children or parents | Increase concern about your child's vision health |
Total (n=350) | χ2 | P | Awareness of myopia risk |
Total (n=350) | χ 2 | P | |||
| Yes | No | It poses significant risks +high myopia may lead to irreversible fundus lesions | It poses certain risks + could be “cured” | It does not pose any risks | |||||||
| Children with myopia | 2.137 | 0.144 | 25.107 | <0.001 | |||||||
| Yes | 75 (92.59) | 6 (7.41) | 81 (23.14) | 43 (53.09) | 27 (33.33) | 11 (13.58) | 81 (23.14) | ||||
| No | 261 (97.03) | 8 (2.97) | 269 (76.86) | 212 (78.81) | 49 (18.22) | 8 (2.97) | 269 (76.86) | ||||
| Parents with myopia, n | 0.704 | 0.703 | 6.231 | 0.183 | |||||||
| 0 | 3 (4.69) | 61 (95.31) | 64 (18.29) | 46 (71.87) | 12 (18.75) | 6 (9.38) | 64 (18.29) | ||||
| 1 | 6 (3.19) | 182 (96.81) | 188 (53.71) | 134 (71.27) | 42 (22.35) | 12 (6.38) | 188 (53.71) | ||||
| 2 | 5 (5.10) | 93 (94.90) | 98 (28.00) | 75 (76.53) | 22 (22.45) | 1 (1.02) | 98 (28.00) | ||||
n (%)
Correlation Between Myopia of Children and Parental Myopia Prevention and Control Knowledge and Practices
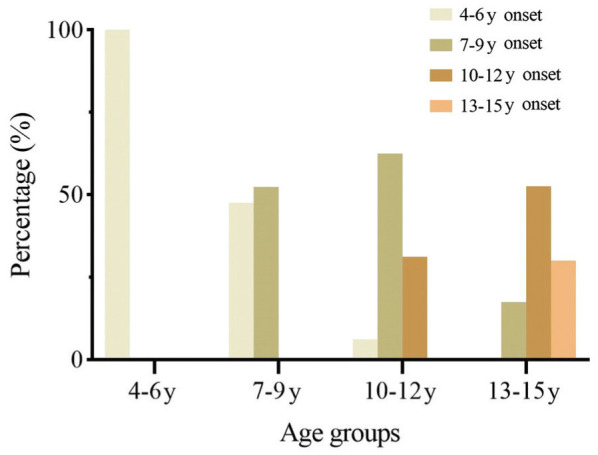
A binary logistic regression model was employed to examine the association between myopia in pre- and school-aged children and parental knowledge and practices regarding myopia prevention and control. A total of seven factors, selected from a pool of twelve related factors (Table 1), were considered for analysis. Subsequently, a regression forest plot was generated, as depicted in Figure 2. It indicated that compared to those lacking knowledge and awareness, parents who had a clear understanding of the risk of myopia, paid more attention to the changes in children's axis length and corneal curvature, advanced the age of children's visual examination, regularly monitored children's dioptric development, limited the screen time of digital products, ensured outdoor activity time and sufficient sleep time could effectively control the incidence of myopia in their pre- and school-aged children.
Figure 2. Correlation between myopia of children and parental myopia prevention and control knowledge and practices.
Myopia Prevention and Control Knowledge and Practices Among Parents Vary Across Different Levels of Education
Additionally, we conducted a hierarchical study to examine the comprehension of parents with varying levels of education regarding the prevention and control of myopia. This study categorized parents' educational attainment into three distinct classes: 1) completion of high school education or lower, 2) attainment of a bachelor's degree, 3) acquisition of a master's or doctoral degree.
The study revealed that there was a correlation between the education level of parents and the prevalence of childhood-onset myopia, with lower rates observed among parents with higher education levels (27.03%, 23.40%, and 18.37% for different education levels. This correlation, however, did not reach statistical significance (P=0.332). Interestingly, there was a slight decrease in parents' attention to their children's visual health, with the improvement in education level, as evidenced by percentages of 98.20%, 95.03%, and 94.90% (P=0.359). But there was a more comprehensive awareness of myopic vision impairment, particularly high myopia, with percentages of 69.37%, 74.47%, and 74.49%. Nevertheless, the difference was also not statistically significant (P=0.056).
Through the analysis of the myopia prevention and control knowledge and practices among parents with varying levels of education, several noteworthy conclusions have been derived, warranting further exploration: 1) In terms of the knowledge of myopia prevention and control, parents holding a master's or doctoral degree exhibited a superior understanding of the visual standards for children across various age groups (P=0.001). However, the parental awareness and understanding of certain concepts such as the distinction between myopia and “pseudomyopia (the ciliary muscle modulation spasm)”, the development of children's axis length, the alterations in corneal curvature, and the concept of children's hyperopia reserve were generally inadequate. There was no significant disparity observed among the three groups (Table 5). 2) In terms of the practices of myopia prevention and control, 31.63% of parents holding a master's or doctoral degree could undergo initial vision screening for their children during the age of 0 to 3y, while parents with a bachelor's degree (34.04%) and below (32.43%) predominantly initiated the vision examination for their children at the age of 4 to 6y; this result was borderline significant (P=0.05). Furthermore, there was still a considerable proportion (nearly 30%) of parents in each group who had not taken their children for a visual examination, except for the school-organized. The majority of parents in these three groups were able to regulate their children's screen time on digital devices, limiting it to 1-3h or even prohibiting usage except online classes (P=0.598). Moreover, it was observed that parents who held master's or doctoral degrees exhibited more effective regulation of their children's outdoor time and sleep duration. This regulation resulted in a higher likelihood of their children engaging in 1 to 3h of outdoor activities (72.45%, P=0.048) and obtaining more than 9 to 10h of sleep per day (41.84%, P=0.044). Conversely, parents with varying levels of education had a low awareness of establishing the dioptric development profiles for their children, with only 16.22%, 12.77%, and 16.33% of parents at different education levels respectively acknowledging this need (P=0.613). The adoption rate of myopia prevention and control products in the market exhibited a generally low level, with no statistically significant variation observed among the three educational cohorts (P=0.724). In contrast, a greater proportion of parents express a preference for employing traditional measures to safeguard their children's visual health. These measures include enhancing the indoor lighting conditions within the reading environment (80.00% of parents), maintaining appropriate reading posture and distance (71.71% of parents), regulating reading duration and incorporating eye relaxation techniques (40.57% of parents), and adhering to prescribed eye exercises (39.43% of parents). A minority of parents also opted for traditional Chinese medicine (TCM) treatment regimens (4.57%), including ear pressure pills, plum needles, and moxibustion, as well as the pharmacological treatment regimens (6.29%), such as low-concentration atropine, for the purpose of preventing and managing myopia (Table 6).
Table 5. Myopia prevention and control knowledge of parents in different educational levels.
| Myopia control knowledge | High school and below | Bachelor's degree | Master's or doctor's degree | Total | χ 2 | P |
| Parents take the initiative to learn about myopia control | 2.467 | 0.651 | ||||
| Learn with a variety of materials actively | 26 (23.42) | 25 (17.73) | 17 (17.35) | 68 (19.43) | ||
| Possess limited knowledge + have not actively sought to learn | 73 (65.77) | 98 (69.50) | 72 (73.47) | 243 (69.43) | ||
| Lack any knowledge or understanding | 12 (10.81) | 18 (12.77) | 9 (9.18) | 39 (11.14) | ||
| Parents attitudes towards myopia risks | 9.221 | 0.056 | ||||
| It poses significant risks + cause irreversible fundus lesions | 77 (69.37) | 105 (74.47) | 73 (74.49) | 255 (72.86) | ||
| It poses certain risks + can be “cured” | 22 (19.82) | 32 (22.69) | 22 (22.45) | 76 (21.71) | ||
| It does not pose any risks | 12 (10.81) | 4 (2.84) | 3 (3.06) | 19 (5.43) | ||
| Know the visual acuity standard of each age group or not | 14.864 | <0.001 | ||||
| Yes | 50 (45.05) | 82 (58.16) | 70 (71.43) | 148 (42.29) | ||
| No | 61 (54.95) | 59 (41.84) | 28 (28.57) | 202 (57.71) | ||
| Able to distinguish between myopia and “pseudomyopia” or not | 1.983 | 0.371 | ||||
| Yes | 44 (42.86) | 65 (46.10) | 48 (48.98) | 157 (44.86) | ||
| No | 67 (57.14) | 76 (53.90) | 50 (51.02) | 193 (55.14) | ||
| Attention to children's axis length development and corneal curvature changes | 7.088 | 0.131 | ||||
| Pay significant attention + have a periodic examination | 21 (18.92) | 17 (12.06) | 16 (16.33) | 54 (15.43) | ||
| Pay minimal attention + only examine when doctor think it is necessary | 26 (23.42) | 45 (31.91) | 37 (37.76) | 108 (30.86) | ||
| Neglect to pay attention altogether | 64 (57.66) | 79 (56.03) | 45 (45.92) | 188 (53.71) | ||
| Knowledge of the hyperopia reserve | 6.885 | 0.332 | ||||
| Possess a thorough understanding of it | 5 (4.50) | 8 (5.67) | 8 (8.61) | 21 (6.00) | ||
| Have some knowledge about it | 22 (19.82) | 26 (18.44) | 27 (27.55) | 75 (21.83) | ||
| Have heard before, but do not possess a comprehensive understanding | 34 (30.63) | 53 (37.59) | 26 (26.53) | 113 (32.29) | ||
| Be entirely unfamiliar with it | 50 (45.05) | 54 (38.30) | 37 (37.76) | 141 (40.29) |
n (%)
Table 6. Myopia prevention and control practices of parents in different educational levels.
| Myopia control practices | High school and below | Bachelor's degree | Master's or doctor's degree | Total | χ2 | P |
| The age at which the child's vision examination was first performed | 15.512 | 0.050 | ||||
| 0-3y | 17 (15.32) | 26 (18.44) | 31 (31.63) | 74 (21.14) | ||
| 4-6y | 36 (32.43) | 48 (34.04) | 28 (28.57) | 112 (32.00) | ||
| 7-9y | 17 (15.32) | 18 (12.77) | 6 (6.12) | 41 (11.71) | ||
| 10-15y | 8 (7.21) | 5 (3.55) | 2 (2.04) | 15 (4.29) | ||
| No initiative examination besides the school-organized | 33 (29.73) | 44 (31.21) | 31 (31.63) | 108 (30.86) | ||
| Have regular vision examinations or optometry for children or not | 4.475 | 0.613 | ||||
| Consistently undergo examinations and have established a refractive profile | 18 (16.22) | 18 (12.77) | 16 (16.33) | 52 (14.86) | ||
| Consistently undergo examinations without establishing a refractive profile | 34 (30.63) | 43 (30.50) | 29 (29.59) | 106 (30.29) | ||
| Only check if the child experiences a decline in vision | 27 (24.32) | 29 (20.57) | 15 (15.31) | 71 (20.29) | ||
| Have never taken their child for a visual examination | 32 (28.83) | 51 (36.71) | 38 (38.78) | 121 (34.57) | ||
| The total duration of digital devices for children per day, except for e-learning | 4.583 | 0.598 | ||||
| No additional usage | 14 (12.61) | 13 (9.33) | 13 (13.27) | 40 (11.43) | ||
| <1h | 49 (44.14) | 72 (51.06) | 48 (48.98) | 169 (48.29) | ||
| 1-3h | 33 (29.73) | 42 (29.79) | 31 (31.63) | 106 (30.29) | ||
| >3h | 15 (13.51) | 14 (9.93) | 6 (6.12) | 35 (10.00) | ||
| The total duration of outdoor activities for children per day | 9.580 | 0.048 | ||||
| >3h | 11 (9.91) | 10 (7.09) | 13 (13.27) | 34 (9.71) | ||
| 1-3h | 71 (63.96) | 88 (62.41) | 71 (72.45) | 230 (65.71) | ||
| <1h | 29 (26.13) | 43 (30.50) | 14 (14.29) | 86 (24.57) | ||
| The total duration of sleep for children per day | 12.913 | 0.044 | ||||
| >10h | 14 (12.61) | 18 (12.77) | 21 (21.43) | 53 (15.14) | ||
| 9-10h | 36 (32.43) | 52 (36.88) | 41 (41.84) | 129 (36.86) | ||
| 8-9h | 53 (47.75) | 67 (47.52) | 35 (35.71) | 155 (44.29) | ||
| <8h | 8 (7.21) | 4 (2.84) | 1 (1.02) | 13 (3.71) | ||
| Use myopia prevention and control products or not | 0.647 | 0.724 | ||||
| Yes | 19 (17.12) | 23 (16.31) | 13 (13.27) | 55 (15.71) | ||
| No | 92 (82.88) | 118 (83.69) | 85 (86.73) | 295 (84.29) | ||
| Myopia control practices parents have implemented for their children | 23.171 | 0.058 | ||||
| No practices have been undertaken | 13 (11.71) | 14 (9.93) | 6 (6.12) | 33 (9.43) | ||
| Enhancing the indoor lighting of the reading environment | 85 (76.58) | 109 (77.30) | 86 (87.76) | 280 (80.00) | ||
| Maintaining proper reading posture and distance (>33 cm) | 80 (72.07) | 111 (78.72) | 70 (71.43) | 251 (71.71) | ||
| Appropriate duration of proximal reading (within 30min) and eye relaxation (2-3min) | 44 (39.64) | 56 (39.72) | 42 (42.86) | 142 (40.57) | ||
| Consistent adherence to eye exercises | 54 (48.65) | 60 (42.55) | 24 (24.49) | 138 (39.43) | ||
| Utilization of TCM treatments | 3 (2.70) | 11 (7.80) | 2 (2.04) | 16 (4.57) | ||
| Low-concentration atropine | 2 (1.80) | 3 (2.13) | 5 (5.10) | 10 (2.86) | ||
| Other practices | 3 (2.70) | 13 (9.22) | 6 (6.12) | 22 (6.29) |
TCM: Traditional Chinese medicine.
n (%)
DISCUSSION
The issue of myopia in pre- and school-aged children is a significant societal concern. The statistical findings of this study indicate a positive correlation between age and the incidence and sever of myopia in pre- and school-aged children. Additionally, the age at which myopia onsets inclines to be younger compared with the past, which is consistent with previous analyses of large-scale domestic data[4],[20].
In China, apart from acknowledged risk factors associated with myopia[21], such as genetic predisposition and excessive near work, the pervasive educational anxiety[22] and parental unawareness regarding myopia prevention and control are also exerting indirect influences on the visual health of children. Typical instances include providing preschool education or early interest-based training for children, as well as introducing electronic devices to children at a young age. These factors may potentially contribute to the depletion of children's reserves of hyperopia. Previous research indicated that a considerable proportion of preschool children had insufficient hyperopia reserve. Sun et al[23] discovered that approximately 88.57% of 6-year-old children in Guangdong Province, China had experienced a depletion of their hyperopia reserves. Furthermore, a refractive screening of 4411 primary school students in Chongqing, China revealed that only 6.10% of children aged 6 to 7y possessed sufficient hyperopia reserves[24]. This concerning trend is not limited to China, but similar patterns have also been observed in other Asian countries[25]–[26]. Hence, it is crucial to start myopia prevention and control measures in children at an earlier age. Our investigation, however, revealed that merely about 50% of parents were able to successfully conduct the initial vision screening for their offspring before the age of six, with roughly 30% of parents never proactively seeking vision examinations for their children. The preschool stage is a critical period for the prevention of myopia, requiring parents to have a thorough understanding of the visual development characteristics of children during this phase and to provide timely support in fostering appropriate habits.
From a public health policy standpoint, the effective implementation of any myopia prevention and control strategy is contingent upon parental involvement. However, due to varying levels of education and socioeconomic status among families, the extent of parental control over their children's extracurricular tutoring is inconsistent, leading to the potential polarization of either excessive leniency or excessive strictness[27]–[28]. This presents numerous challenges in promoting myopia prevention and control strategies among parents.
It is worth mentioning that the COVID-19 era has witnessed a notable prevalence of myopia in children as a result of such parental education strategies. A part of parents believed that the period of home confinement provided a favorable opportunity for their children to acquire knowledge and devised comprehensive study schedules; Some parents disregarded the supervision of their children, leading to unregulated utilization of electronic products[29]. As a result, such intensive online learning, accompanied by high levels of recreational screen time, has resulted in the emergence of diverse eye health issues among children, including eye strain, dry eyes, and myopia[30]–[32]. Our findings indicated that a majority of children (53.71%) experienced visual decline during the COVID-19 lockdown, with a subset (11.43%) exhibiting significant visual decline. Interestingly, despite the notable prevalence of myopia, there is a dearth of published research exploring parental attitudes and practices regarding myopia and its management within the household. The existing research has primarily concentrated on the extent of parental knowledge regarding the occurrence of digital eye strain among children participating in online classes during this period[14],[30]. This prompts further contemplation regarding the appropriate actions that parents should adopt to safeguard their children's visual well-being in the context of prolonged isolation necessitated by situations like COVID-19.
Most families in this research still exhibited a persisting adherence to traditional notions of myopia correction. Specifically, 18.52% of parents believed that as long as the degree of myopia was not severe, corrective eyewear was unnecessary and a significant proportion of parents (55.56%) continued to opt for conventional spectacles. The utilization of DIMS lenses and OK lenses, which possess myopia prevention and control functionalities, was limited due to parents' insufficient understanding of their underlying principles. Consequently, these lenses were not favored unless specifically recommended by optometrists. In addition, the exorbitant cost and frequent ocular examinations also impose limitations on the target audience to some degree.
Parents also have limited knowledge about various aspects of myopia, including children's visual acuity at different age groups, hyperopia reserve, axis length and corneal curvature development. In clinical practice, a number of parents (21.71% in our study) mistakenly believe that myopia correction surgery can completely eradicate myopia. Moreover, parents with lower levels of education often lack sufficient awareness regarding the detrimental consequences of myopia, such as high-myopic retinopathy. Unlike our conventional cognition, certain parents with elevated educational attainment exhibit limited concern for their children's visual well-being, potentially due to their prioritization of fostering their children's cultural knowledge. Jiang et al[19] conducted a survey in Wenzhou, China, to examine the eye health care knowledge and behavior of parents with junior primary school students. The findings revealed that 70.0% of the surveyed parents possessed a bachelor's degree or higher, and a majority of these well-educated parents lacked clarity regarding the appropriate eye healthcare practices. Furthermore, over half of the parents were unaware of their children's dioptric status, suggesting a lack of attention towards their children's eye hygiene despite their educational background.
In contrast to the limited comprehension of myopia-related concepts, parents exhibit greater engagement in the implementation of myopia prevention and control measures. The findings of this study indicate that approximately 50% of parents proactively engage in regular assessments of their children's visual acuity and diopter status, while 14.86% of parents have established a dioptric development profile for their children. Furthermore, the findings suggest a positive correlation between parental education levels and the age at which children undergo their first vision screening, as well as the establishment of more appropriate outdoor activity and sleep routines. Despite the different educational backgrounds, a large majority of parents (90.00%) acknowledged the potential adverse effects of digital technology on their children's eyes and consequently imposed strict limitations on their children's usage of digital devices. In conjunction with traditional preventive and control measures, such as the rectification of reading and writing habits, enhancement of indoor lighting, and adherence to eye exercises, a growing number of individuals presently exhibit a preference for receiving TCM therapy and pharmacological interventions, including the administration of low-concentration atropine.
Through the utilization of binary logistic regression analysis, our study has demonstrated a strong correlation between the implementation of diverse strategies within families for disseminating myopia prevention and control knowledge and a significant decrease in the prevalence of myopia among preschoolers and school-aged children. These strategies include emphasizing the detrimental effects of myopia, monitoring alterations in children's axis length and corneal curvature, initiating visual examinations at an earlier age, regularly monitoring dioptric development, restricting the usage of digital devices, promoting outdoor activities, and ensuring adequate sleep duration. Hence, with regard to familial education for myopia prevention and control, it is imperative to enhance the aforementioned seven aspects, while also recognizing that diverse family education backgrounds warrant distinct comprehensive strategies.
Our study is subject to several limitations. First, selection bias may have occurred due to the relatively small sample size. Second, the survey was shared in parents' social media groups, but it is unclear if all participants were actually parents or guardians of pre- and school-aged children. Our questionnaire restricts one response per IP address, but we cannot prevent a single parent from using different IP addresses to submit multiple responses. Third, the information regarding myopia in both parents and children was collected through questionnaires, lacking objective and quantitative measurements. This reliance on self-reported data introduces the potential for recall biases, as parents may provide ideal responses rather than accurate ones.
In conclusion, this survey advances our knowledge of myopia status in pre- and school-aged children and parental attitudes, knowledge, and practices in relation to myopia. Despite the widespread concern among parents regarding the visual health of pre- and school-aged children, there remains a dearth of up-to-date and comprehensive knowledge and strategies about myopia prevention and control. The diverse socioeconomic statuses and cultural backgrounds of parents further complicate the dissemination of reliable and systematic information on myopia prevention and control. Thus, popularization for families is still difficult. In forthcoming times, the government ought to implement efficacious and adaptable strategies to enhance parental awareness and foster their commitment towards myopia prevention and control, thereby establishing a collaborative effort for the betterment of children's visual health across society.
Footnotes
Authors' contributions: Li TT and Fang ZS were responsible for questionnaire design, publication, and original draft preparation. Xue YX and Chen SJ were responsible for data analysis. Yang YX was responsible for the evaluation and optimization of the questionnaire content, and revision of the manuscript. Li TJ, Yang Y, and Wu Y participated in the design of the questionnaire content. All authors reviewed the manuscript.
Foundation: Supported by the National Natural Science Foundation of China (No.82205196).
Conflicts of Interest: Li TT, None; Fang ZS, None; Xue YX, None; Chen SJ, None; Yang YX, None; Li TJ, None; Yang Y, None; Wu Y, None.
REFERENCES
- 1.Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 2.Hopf S, Pfeiffer N. Epidemiology of myopia. Ophthalmologe. 2017;114(1):20–23. doi: 10.1007/s00347-016-0361-2. [DOI] [PubMed] [Google Scholar]
- 3.Wu PC, Huang HM, Yu HJ, Fang PC, Chen CT. Epidemiology of myopia. Asia Pac J Ophthalmol (Phila) 2016;5(6):386–393. doi: 10.1097/APO.0000000000000236. [DOI] [PubMed] [Google Scholar]
- 4.The Overall Myopia Rate of Children and Adolescents in China was 52.7% in 2020, and the Problem of Myopia at a Younger age is still prominent. In: The State Council of the People's Republic of China. 2021 http://www.gov.cn/xinwen/2021-07/13/content_5624709.htm. Accessed on Jul 13, 2021. [Google Scholar]
- 5.Ding BY, Shih YF, Lin LLK, Hsiao CK, Wang IJ. Myopia among schoolchildren in East Asia and Singapore. Surv Ophthalmol. 2017;62(5):677–697. doi: 10.1016/j.survophthal.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 6.Li SM, Wei SF, Atchison DA, Kang MT, Liu LR, Li H, Li SY, Yang Z, Wang YP, Zhang FJ, Wang NL. Annual incidences and progressions of myopia and high myopia in Chinese schoolchildren based on a 5-year cohort study. Invest Ophthalmol Vis Sci. 2022;63(1):8. doi: 10.1167/iovs.63.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jonas JB, Ang M, Cho P, Guggenheim JA, He MG, Jong M, Logan NS, Liu M, Morgan I, Ohno-Matsui K, Pärssinen O, Resnikoff S, Sankaridurg P, Saw SM, Smith EL, III, Tan DTH, Walline JJ, Wildsoet CF, Wu PC, Zhu XY, Wolffsohn JS. IMI prevention of myopia and its progression. Invest Ophthalmol Vis Sci. 2021;62(5):6. doi: 10.1167/iovs.62.5.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhu ZT, Chen YX, Tan Z, Xiong RL, McGuinness MB, Müller A. Interventions recommended for myopia prevention and control among children and adolescents in China: a systematic review. Br J Ophthalmol. 2023;107(2):160–166. doi: 10.1136/bjophthalmol-2021-319306. [DOI] [PubMed] [Google Scholar]
- 9.Morgan IG, Jan CL. China turns to school reform to control the myopia epidemic: a narrative review. Asia Pac J Ophthalmol (Phila) 2022;11(1):27–35. doi: 10.1097/APO.0000000000000489. [DOI] [PubMed] [Google Scholar]
- 10.Liu YL, Jhang JP, Hsiao CK, Tsai TH, Wang IJ. Influence of parental behavior on myopigenic behaviors and risk of myopia: analysis of nationwide survey data in children aged 3 to 18y. BMC Public Health. 2022;22(1):1637. doi: 10.1186/s12889-022-14036-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McCrann S, Flitcroft I, Lalor K, Butler J, Bush A, Loughman J. Parental attitudes to myopia: a key agent of change for myopia control? Ophthalmic Physiol Opt. 2018;38(3):298–308. doi: 10.1111/opo.12455. [DOI] [PubMed] [Google Scholar]
- 12.Zhou S, Yang LH, Lu BL, Wang HX, Xu T, Du DD, Wu SQ, Li XX, Lu MX. Association between parents' attitudes and behaviors toward children's visual care and myopia risk in school-aged children. Medicine (Baltimore) 2017;96(52):e9270. doi: 10.1097/MD.0000000000009270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.He AQ, Liu SA, He SY, Yao H, Chen P, Li Y, Qiu J, Yu KM, Zhuang J. Investigation of children's habits of smartphone usage and parental awareness of myopia control in underdeveloped areas of China. Int J Ophthalmol. 2022;15(10):1691–1698. doi: 10.18240/ijo.2022.10.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaur K, Kannusamy V, Gurnani B, Mouttapa F, Balakrishnan L. Knowledge, attitude, and practice patterns related to digital eye strain among parents of children attending online classes in the COVID-19 era: a cross-sectional study. J Pediatr Ophthalmol Strabismus. 2022;59(4):224–235. doi: 10.3928/01913913-20211019-01. [DOI] [PubMed] [Google Scholar]
- 15.Zhang XJ, Zhang YZ, Kam KW, Tang FY, Li Y, Ng MPH, Young AL, Ip P, Tham CC, Chen LJ, Pang CP, Yam JC. Prevalence of myopia in children before, during, and after COVID-19 restrictions in Hong Kong. JAMA Netw Open. 2023;6(3):e234080. doi: 10.1001/jamanetworkopen.2023.4080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang JX, Han YJ, Musch DC, Li Y, Wei N, Qi XL, Ding G, Li X, Li J, Song LL, Zhang Y, Ning YX, Zeng XY, Li YL, Sun L, Hua N, Li S, Jardines S, Qian XH. Evaluation and follow-up of myopia prevalence among school-aged children subsequent to the COVID-19 home confinement in Feicheng, China. JAMA Ophthalmol. 2023;141(4):333–340. doi: 10.1001/jamaophthalmol.2022.6506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li SM, Ran AR, Kang MT, Yang XY, Ren MY, Wei SF, Gan JH, Li L, He X, Li H, Liu LR, Wang YP, Zhan SY, Atchison DA, Morgan I, Wang NL, Anyang Childhood Eye Study Group Effect of text messaging parents of school-aged children on outdoor time to control myopia: a randomized clinical trial. JAMA Pediatr. 2022;176(11):1077–1083. doi: 10.1001/jamapediatrics.2022.3542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang HW, Zhang XN, JI Y, Xie LJ, Long X, Cao RX. Analysis on the awareness and influencing factors of myopia prevention and control among the parents of 339 lower grade primary school students. Capital Journal of Public Health. 2020;14(06):291–293. [Google Scholar]
- 19.Jiang DD, Deng RZ, Zheng DD, Chen YY. A cross-sectional study on eye health care knowledge and behavior among parents of low-grade students. Chin J Sch Health. 2016;37(10):1473–1475. [Google Scholar]
- 20.Chinese Optometric Association, Chinese Ophthalmological Society, Ophthalmology and Optometry Committee, Ophthalmologists Association, Chinese Doctor Association, Ophthalmology and Optometry Group, Ophthalmologic Committee, Chinese Non-government Medical Institutions Association, Eye Refractive error prevtenion and control Group of the Cross-Straits Medical Exchange Association (SMEA), Commission of Ophthalmology, Ophthalmology Branch of Chinese Geriatrics Society (CGS) Expert Consensus on Myopia Management White Paper (2022) Chin J Optom Ophthalmol Vis Sci. 2022;24(9):641–648. [Google Scholar]
- 21.Landreneau JR, Hesemann NP, Cardonell MA. Review on the myopia pandemic: epidemiology, risk factors, and prevention. Mo Med. 2021;118(2):156–163. [PMC free article] [PubMed] [Google Scholar]
- 22.Peng W, Zhang ZK, Wang F, Sun SM, Sun YN. Association of educational environment with the prevalence of myopia: a cross-sectional study in Central China. Front Public Health. 2023;11:1188198. doi: 10.3389/fpubh.2023.1188198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sun Y, Lin R, Xiong LH, Chen SY, Chen KC, Wu DP, Liu WJ. Status and influencing factors of insufficient hyperopia reserve among children without myopia in Guangzhou in 2021. Chin J Dis Control & Prev. 2023;27(3):368–372. [Google Scholar]
- 24.Yue Y, Liu XM, Yi S, Liu B, Yi H, Li H. High prevalence of myopia and low hyperopia reserve in 4411 Chinese primary school students and associated risk factors. BMC Ophthalmol. 2022;22(1):212. doi: 10.1186/s12886-022-02436-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grzybowski A, Kanclerz P, Tsubota K, Lanca C, Saw SM. A review on the epidemiology of myopia in school children worldwide. BMC Ophthalmol. 2020;20(1):27. doi: 10.1186/s12886-019-1220-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cohen Y, Iribarren R, Ben-Eli H, Massarwa A, Shama-Bakri N, Chassid O. Light intensity in nursery schools: a possible factor in refractive development. Asia Pac J Ophthalmol (Phila) 2022;11(1):66–71. doi: 10.1097/APO.0000000000000474. [DOI] [PubMed] [Google Scholar]
- 27.Chen GY, Oubibi M, Liang AN, Zhou YL. Parents' educational anxiety under the “double reduction” policy based on the family and students' personal factors. Psychol Res Behav Manag. 2022;15:2067–2082. doi: 10.2147/PRBM.S370339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saw SM, Hong RZ, Zhang MZ, Fu ZF, Ye M, Tan D, Chew SJ. Near-work activity and myopia in rural and urban schoolchildren in China. J Pediatr Ophthalmol Strabismus. 2001;38(3):149–155. doi: 10.3928/0191-3913-20010501-08. [DOI] [PubMed] [Google Scholar]
- 29.Dong CM, Cao SM, Li H. Young children's online learning during COVID-19 pandemic: Chinese parents' beliefs and attitudes. Child Youth Serv Rev. 2020;118:105440. doi: 10.1016/j.childyouth.2020.105440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mohan A, Sen P, Shah C, Jain E, Jain S. Prevalence and risk factor assessment of digital eye strain among children using online e-learning during the COVID-19 pandemic: digital eye strain among kids (DESK study-1) Indian J Ophthalmol. 2021;69(1):140–144. doi: 10.4103/ijo.IJO_2535_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wong CW, Tsai A, Jonas JB, Ohno-Matsui K, Chen J, Ang M, Ting DSW. Digital screen time during the COVID-19 pandemic: risk for a further myopia boom? Am J Ophthalmol. 2021;223:333–337. doi: 10.1016/j.ajo.2020.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hu Y, Zhao F, Ding XH, Zhang S, Li ZY, Guo YF, Feng ZB, Tang XH, Li Q, Guo L, Lu CY, Yang X, He MG. Rates of myopia development in young Chinese schoolchildren during the outbreak of COVID-19. JAMA Ophthalmol. 2021;139(10):1115–1121. doi: 10.1001/jamaophthalmol.2021.3563. [DOI] [PMC free article] [PubMed] [Google Scholar]