Abstract
Introduction
Non-adherence to splint wearing following an upper limb traumatic injury is a significant medical issue. Optimal outcome following such injuries relies on people adhering to the prescribed splint, and a failure to do so can negatively impact outcome and increase healthcare burden and costs. This systematic review aims to compare and synthesise the evidence related to measuring adherence to wear recommendations and the barriers to splint wearing following upper limb trauma in adults.
Methods
Databases (EBSCO, PubMed, EMBASE and Science Direct) were systematically searched for articles that met the pre-agreed eligibility criteria between February and May 2023. Data on study characteristics and reported outcomes relating to measuring and quantifying splint adherence and barriers to adherence were extracted.
Results
A total of 16 articles were included for final review. Several methods were used to measure adherence, with no single tool used predominantly. These included patient or therapist reported data, preexisting classification systems and an electronic device. Methods used to quantify adherence was also heterogenous in nature, and a range of investigator and patient reported barriers to splint wearing were reported.
Conclusion
This review demonstrates heterogeneity in both classifying and measuring splint adherence, as well as in the barriers to splint wearing reported. Moving forward, using agreed measurement and reporting practices for splint adherence will enable researchers to complete high quality trials to determine splinting outcomes, and may ultimately enable health care professionals to improve adherence and, subsequently, outcomes in clinical practice.
Keywords: Splint, adherence, systematic review, hand therapy
Introduction
Non-adherence to treatment is a significant concern in healthcare. As well as being associated with an increasing health burden and a negative impact on health outcomes overall, non-adherence is also associated with higher healthcare costs. 1 In clinical practice, the World Health Organisation (WHO) defines adherence as “...the extent to which a person’s behaviour – taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider” (p.18). 1 Adherence is like compliance, this being previously defined as the degree to which an individual's actual medication use aligned with the regimen prescribed: however, use of the word adherence has superseded the term compliance due to the negative connotations of the latter.2,3
The multi-dimensional adherence model was developed by WHO in 2003. 1 This report identified five domains associated with non-adherence more broadly: 1) social and economic (age, gender, ethnicity, employment status, family/social dysfunction, drug/alcohol issues and education level); 2) health-care team and system (patient-provider relationship, follow up length); 3) condition related (type of injury, prognosis, co-morbidities); 4) therapy related (complexity, duration of treatment, interference with lifestyle/activities of daily living/work, immediacy of benefit, discomfort) and 5) patient related (physical factors, cognitive impairment and psychological factors). This report aimed to raise awareness of the problem, highlight the clinical and cost impact of non-adherence, and give clinicians specific guidance on how to manage non-adherence, but was primarily focussed on medication adherence. 4
Within upper limb therapy, adherence to a splint wearing regimen is of particular importance. Splinting forms a key part of the rehabilitation of most upper limb pathologies, including osteoarthritis of the hand, 5 tendon injuries of the hand and forearm, 6 bony and non-bony wrist pathology, 7 peripheral neuropathies,8,9 and post-stroke spasticity of the upper limb, 10 although the evidence base underpinning these interventions is variable. 11 Earlier publications have indicated that adherence to splinting is inconsistent, with some studies identifying non-adherence rates of up to 70%; although there are substantial differences in how this is measured in different studies, 12 and what factors influence adherence. 13 There is a wealth of data on patient adherence to pharmacological treatments,1,14,15 but much less on adherence to therapy interventions as identified by a systematic review conducted in 2010. 13 Interestingly, some studies have reported that having a poor functional baseline as well as transport burden to appointments have been identified as factors associated with poor adherence to rehabilitation regimes. 16 These are likely exacerbated by restrictions placed on mobility and driving due to the nature of the patient’s condition in these circumstances. 16
Given the near ubiquity of splinting in the management of upper limb pathology, an appreciation of adherence to treatment is vital, both to maximise patient responsiveness to therapy regimes and to identify potential behavioural study targets that could improve the use of splinting in the future. This systematic review aims to identify barriers to adherence to upper limb splints, and to compare and synthesise the evidence related to measuring and quantifying splint adherence.
Methods
This review was developed and completed using the PRISMA guidelines for reporting systematic reviews 17 and registered with PROSPERO (CRD42023403415). 18 The full details of the protocol can be viewed at: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023403415.
The terms splint, orthosis and brace are frequently used interchangeably in the literature depending on the location and the clinical background of the study team. The American Society of Hand Therapists (ASHT) specifically define an orthosis as “A rigid or semi-rigid device that supports a weak or deformed body member or restricts or eliminates motion in a diseased or injured part of the body. An orthosis can be custom fabricated, custom fit or prefabricated”. 19 In this review we will use the term ‘splint’ to reflect the commonly preferred terminology of United Kingdom (UK) based hand therapists, to represent any ‘splint’, ‘orthosis’ or ‘brace’ providing an element of immobilisation or controlled mobilisation to the affected part of the upper limb, which could be removed by the patient under the direction of their clinical team.
Search strategy
A systematic literature search was carried out to identify articles reporting on the methods used to measure adherence and the barriers to wearing splints in the upper limb following traumatic injuries. The search strategy was developed by the research team and took place between February and May 2023, and was updated in December 2023.
A systematic search of databases: MEDLINE, CINAHL (via EBSCOhost), PubMed, EMBASE, and ScienceDirect was conducted using key search terms and their related terms. Table 1 provides detail on the search terms used.
Table 1.
Literature review key search terms.
| Population | Adult* |
| AND | |
| Injur* Trauma* | |
| AND | |
| Finger* Hand* Thumb* Wrist* Upper limb* Arm* Shoulder* | |
| AND | |
| Intervention | Splint |
| Ortho* | |
| Brace | |
| AND | |
| Outcome | Compliance |
| Adherence | |
A decision to search databases from 2009 up to the current year was made because of the publication of a previous systematic review on splint adherence, 13 and a paper reviewing the methods used to measure adherence. 20 The aim of this current review therefore was to update and combine these two previously published reviews in the field of upper limb splinting, given that additional articles had been published related to splint adherence and the measurement of adherence since these publications.
Eligibility criteria
The inclusion criteria included patients 18 years and over, traumatic injuries of the upper limb and studies reporting on: splint adherence as a primary or secondary outcome OR reporting on barriers to splint adherence OR reporting on methods used to assess splint adherence.
The exclusion criteria were articles published prior to 2009, systematic or other literature reviews, articles relating to chronic long-term conditions e.g., rheumatoid arthritis, case series, cadaveric or other non-human studies and non-English articles. Full eligibility criteria can be seen in Table 2.
Table 2.
Eligibility criteria.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Date of publications | |
| • Articles published from 2009 until Dec 2023 | • Articles published prior to 2009 as previous reviews have reported on these |
| Population | |
| • Adults over 18 years | • Acquired or chronic long term conditions e.g rheumatoid arthritis, neurological conditions etc. |
| • Any type of traumatic injury/injuries of the digits, hand, wrist forearm, arm, upper limb or shoulder that required immobilisation or control of movement of the affected body part with a splint/orthosis or brace | |
| Article type | |
| • Primary quantitative or qualitative studies reporting on barriers to splint adherence AND/OR reporting on splint adherence as a primary or secondary outcome AND/OR reporting on methods used to assess splint adherence | • Systematic or other literature reviews were excluded, along with case series, opinion pieces, proof on concept articles and cadaveric or other non-human studies |
| • Non-English articles were also excluded | |
Screening and article selection
The initial search of the databases was carried out by the primary author (EB) and all articles were exported to Rayyan.ai (https://www.rayyan.ai), reference management software. Table 2 provides full details of the search strategy used. Once all articles had been exported, duplicate articles were removed. The remaining titles and abstracts were then screened for eligibility according to the inclusion and exclusion criteria by three reviewers (EB, JM, IS). The full texts of eligible studies were retrieved, and subject to screening independently by three reviewers (EB, JM, IS) against the full inclusion and exclusion criteria. Any uncertainties were initially discussed within the screening team, and a fourth assessor was used to resolve any discrepancies (AS). Finally, the reference lists of the full text articles included in this review were hand searched for any additional articles of interest. These papers were then subject to screening (EB, JM, IS), and any eligible articles added for final review if they satisfied the inclusion and exclusion criteria.
Data extraction
A standardised data extraction pro-forma was developed by the study team (EB, JM, IS) and data was extracted and inputted systematically by the individual reviewing each paper using this pro-forma (EB, JM, IS, AS). Data capture included: demographic data, study design, country of study, study duration, sample size, study population (diagnosis, age, and sex), type of splint, duration of wear, and barriers to splint wearing (including patient reported barriers and patterns observed by the study teams). The method of recording adherence was also captured.
Due to the heterogeneity of the studies, quantitative analysis was not possible, therefore synthesis of extracted data was narrative.
Quality assessment
The quality of the studies being reviewed was assessed using Version 2 of the Cochrane risk-of-bias tool for randomised trials (RoB 2) 21 for the three RCTs,22–24 and the critical appraisal skills programme (CASP) checklist appropriate for the type of study being reviewed e.g. qualitative study, cohort study etc 25 for the remaining studies. All studies were evaluated by individual reviewers (EB, JM, IS) and an appropriate form was completed for each assessment.
Results
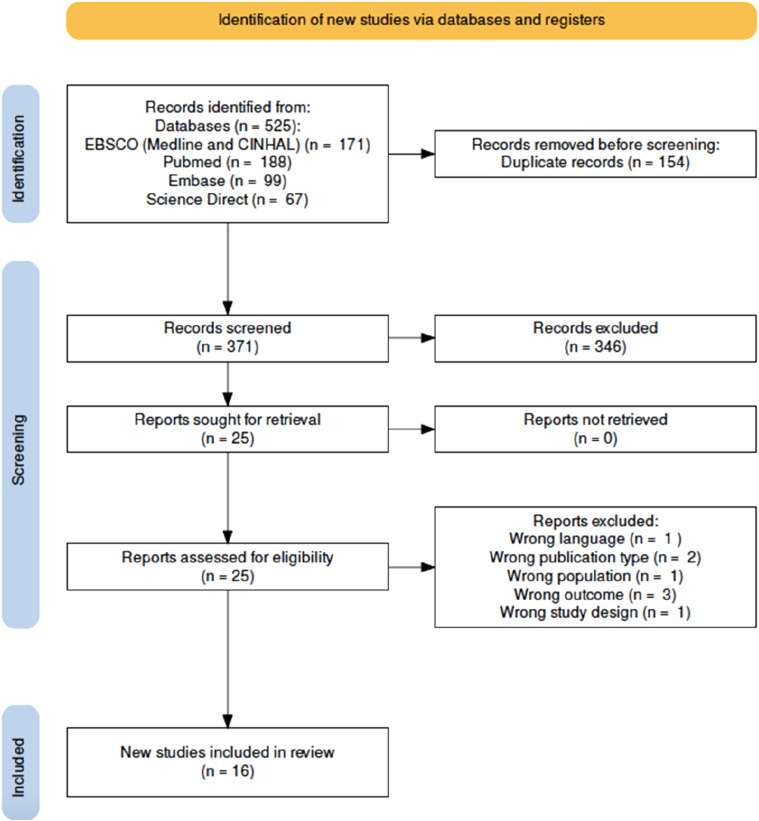
A total of 525 records were identified from the original search with 371 records remaining after removal of duplicates. Of these, 25 full texts were then screened for eligibility, of which 16 satisfied the inclusion and exclusion criteria and were subject to full review. A total of 16 articles were included in the final review. These included articles that measured adherence (n = 14), quantified adherence (n = 10) or barriers to adherence (n = 13), or a combination of these. Figure 1.
Figure 1.
PRISMA 2020 review flow diagram.
Study design
Individual study details are available in Table 3. The 16 studies included 3 randomised controlled trials (RCTs),22–24 3 qualitative studies,26–28 8 cohort series,29–36 1 prospective observational study, 37 and 1 mixed methods study. 38
Table 3.
Summary data - Details of Studies Included in Review (NA = not available).
| Study author | Study design | Country of study | Duration (months) | Participants (n) | Diagnostic criteria | Mean age | % male | % Female | Type of splint | Duration of continuous splint wear (weeks) |
|---|---|---|---|---|---|---|---|---|---|---|
| Ayhan et al 2021 | Prospective cohort study | Turkey | 6 | 46 | Mallet finger | 39.8 | 50 | 50 | Stack splint | 6 |
| Grubhofer et al 2019 | Prospective observational study | Switzerland | NA | 50 | Rotator cuff injury | 56 | 66 | 34 | Postoperative immobilisation in an abduction shoulder brace | 6 |
| Kaskutas and Powell 2013 | Qualitative | USA | NA | 19 | Flexor tendon injury | 35 | 47.4 | 52.6 | Synergistic orthosis with hinged wrist (reports this as most common but doesn't give a breakdown on this) | 7.2 |
| Kolmus et al 2012 | RCT | Australia | 24 | 52 | Axilla burn | NA | 65.4 | 34.6 | Otto bock Omo Immobiliser shoulder splint | 6 |
| Loewenstein et al 2022 | RCT | USA | 12 | 24 | Fractures of the hand or wrist operative treatment | 37.5 | 70.8 | 29.2 | Standard care (postoperative care based on the treating surgeon’s clinical judgement) | NA |
| Mercurio et al 2023 | Prospective cohort study | Italy | 36 | 100 | Rotator cuff injury | 60.9 | 55 | 45 | Shoulder abduction brace | 4 |
| Mottay 2020 | Mixed methods | South Africa | 47 | 75 | Extensor tendon repairs zone repairs 5 to 7 | |||||
| 1 or 2 digits | NA | 83 | 17 | Relative motion extension splint | NA | |||||
| O'Brien and Presnell 2010 | Qualitative | Australia | 3 | 12 | Intraarticular fracture of finger | 31.83 | 50 | 50 | Distraction splint | 6 |
| O'Brien and bailey 2011 | RCT | Australia | 46 | 64 | Mallet finger | 37.6 | 65.6 | 34.4 | Stack splint (control), dorsal aluminium, or custom thermoplastic | 8 |
| Roh et al 2016 | Prospective cohort study | South Korea | 21 | 72 | Mallet finger | 39.4 | 68 | 32 | Volar-padded aluminium orthosis | 7 |
| Savaş and Aydoğan, 2022 | Prospective cohort study | Turkey | 15 | 133 | Flexor or extensor tendon injury | 38.2 | 75.2 | 33 | Static and dynamic flexor and extensor tendon splints | 3 |
| Silverio and Cheung 2014 | Prospective cohort study | USA | 26 | 50 | Rotator cuff injury | 64 | 44.4 | 55.6 | Abduction brace | 6 |
| Mortazavi et al 2023 | Prospective cohort study | Sweden | 36 | 86 | Proximal phalanx fractures | 49 | 33 | 67 | Hand based POSI | 6 |
| Weir et al 2023 | Prospective cohort study | USA | 26 | 65 | Post-surgical shoulder procedures | 59 | 49.2 | 50.8 | Shoulder sling | 4 |
| Cole et al 2023 | Qualitative | Australia | 3 | 3 | Finger injuries | 35 | 33.3 | 66.6 | Relative motion orthosis | 4-8 weeks |
| Azad et al 2023 | Prospective cohort study | USA | Not stated | 45 | Soft tissue mallet injuries | 51 | 65 | 35 | Dorsal extension splint | 6 weeks |
Study duration data were available for 13 studies and ranged from 3 months to 47 months with an average of 23 months. The mean sample size was 56 participants, ranging from 12 to 133.
Demographic details
The mean age of participants was 44.5 years (available in 10 studies) with most participants being men (mean across all studies 58% male). All study participants had a history of a traumatic injury of their upper limb, which required immobilisation or partial immobilisation using a removable splint. Five studies involved splinting of the shoulder or axilla region24,30,33,35,37 and 11 to the wrist or hand22,23,26–29,31,32,34,36,38
Methods of measuring adherence
Out of the 16 studies included in this review, 14 studies measured adherence. The remaining studies did not include a direct measure of adherence but were included in the review as they reported on potential barriers to adherence. There was significant variation in the methods used to measure adherence (Table 4). Eight studies22,24,26,29,32,34,36,38 relied on patient or therapist reported data either in the form of novel questionnaires, interview, or other non-structured means to measure adherence. Four studies utilised an already established classification system tool, either the medical adherence measurement score (MAM score),30,33 or a modified version of a classification system23,31 developed by Groth et al. 39 Two studies utilised temperature sensors fitted within the splint to monitor adherence.35,37
Table 4.
Adherence measures.
| Study author | Method used to measure adherence | Method used to classify adherence |
|---|---|---|
| Ayhan et al 2021 | Patient reported - none structured | Not discussed |
| Grubhofer et al 2019 | Temperature (Orthotimer) sensor | Classification system: High compliance - 80% or more, low compliance less than 80% |
| Kaskutas and Powell 2013 | Patient reported - telephone interview | Not discussed |
| Kolmus et al 2012 | Patient reported - questionnaire | Classification system: Adherent - wore splint for 4 or more days in a week for 6 h or more, and 4 or more nights a week for 4 or more hours |
| Loewenstein et al 2022 | Patient/therapist reported - none structured | Not discussed |
| Mercurio et al 2023 | Medical adherence measurement questionnaire (MAM score) | MAM score |
| Mottay 2020 | Therapist and patient reported - none structured | Not discussed |
| O'Brien and bailey 2011 | Modified groth classification | Classification system: Based on the 3-point scale described by groth. Compliant, secondarily compliant, noncompliant |
| Roh et al 2016 | Modified groth classification | Classification system: Based on the 3-point scale described by groth. Compliant, secondarily compliant, noncompliant |
| Savaş and Aydoğan, 2022 | Patient reported - questionnaire | Classification system: Fully adherent - participants wore splint 100% as recommended. Partial non-adherence - patients who did not wear orthosis for 100% of the recommended time but never used the injured hand. Non-adherent - patients who did not wear orthosis for 100% of the recommended time and used the injured hand |
| Silverio and Cheung 2014 | Medical adherence measurement questionnaire (MAM score) | MAM score |
| Mortazavi et al | Patient reported diary | Participant classified as adherent if wore the splint more than 5 nights in a week |
| Weir et al | Temperature (HOBO MX2201) sensor | Classification system: High compliance - 80% or more, low compliance - less than 80% |
| Azad et al | Patient reported | Any removal of splint was considered non-adherence |
Methods used to quantify adherence
Ten studies reported the method they used to quantify adherence (Table 4). The studies using the MAM reported the MAM score expressed as a percentage.30,33 The two studies utilising the modified Groth classification23,31 reported adherence using a modified version of the 3-point scale as described by Groth. 39 Grubhofer et al 35 and Weir et al 37 presented the adherence data captured by temperature sensors as a percentage and then used this to classify participants as having either high compliance (equal to or more than 80% wear time prescribed), or low compliance (less than 80%.). The remaining four studies developed their own classification systems. Azad et al 36 classified anyone who removed their splint as non-adherent. Kolmus et al 24 classified participants as adherent if they wore their splint for four or more days in a week for 6 hours or more, and four or more nights a week for four or more hours. Mortazavi et al 34 took a similar approach and classified those who wore their splint more than 5 nights a week as adherent. In contrast to this, Savas et al 32 classified full adherence as participants who wore their splint 100% of the prescribed time and never used their hand, partial adherence for those who did not wear their splint 100% of the time, but never used the injured hand and non-adherence as participants who did not wear their splint 100% of the time and used the injured hand.
Barriers to splint adherence
Barriers to adherence were presented in 13 out of the 16 studies included in this review. Interestingly, most of the barriers were reported by the clinical investigator teams themselves, rather than being directly reported by participants. These investigator-reported barriers were either assumed based on the teams’ clinical opinion22,23,31,34,38 or inferred based on correlations made from the study data being analysed.30–33,35 Five studies presented barriers that had been reported by patients themselves.24,26,27,32 A summary of these barriers is presented in Table 5.
Table 5.
Barriers to adherence.
| Investigator reported barriers | Patient reported barriers | |||
|---|---|---|---|---|
| Study author | Data collection method | Assumed barriers | Barriers reported based on study data | |
| Kaskutas, Powell 2013 | Standardised telephone interviews | Not discussed | Not discussed | Difficulties carrying out functional daily activities such as taking care of baby, cooking and job involving keyboard work |
| Kolmus et al 2012 | Participant reported | Not discussed | Not discussed | Patients perceived splint no longer required, therefore removed by 6 weeks |
| Loewenstein et al 2022 | Not clear | Correlation between adherence and financial burden of attending routine appointments. Authors also suggested a link between clinician empathy and adherence | Not discussed | Not discussed |
| Mercurio et al 2023 | Analysis of study data | Not discussed | Correlations between female sex and adherence to the brace, and between adherence to the splint and the number of weeks it was worn, while no correlation emerged between adherence to the brace and functional and psychological results | Not discussed |
| Mottay 2020 | Clinician focus groups | Link between patients’ perception of injury being resolved and early splint removal. Correlation between decreased perception of injury severity and rehabilitation complexity and non-adherence. Language and comprehension of instructions also thought to be a barrier. Suggested link between the financial burden of attending appointments and non-adherence | Not discussed | Not discussed |
| O'Brien 2010 | Patient reported - qualitative interviews | Not discussed | Not discussed | Patients who did not perceive their injury to be significant were less likely to be adherent |
| Also reported that patients believed the outcome will be improved by being adherent to treatment | ||||
| O'Brien and bailey 2011 | Adherence based on a predetermined criterion, using a 3-point scale designed by groth et al | Some assumed barriers inferred related to adherence and attendance to clinical appointments, but not clearly discussed | Not discussed | Not discussed |
| Roh et al 2016 | Barriers identified from correlations between the quantitative data | Correlation between decreased occupational level, physical activity and psychological factors and non-adherence | Correlations between data and adherence, poor health literacy | Not discussed |
| Savaş and Aydoğan, 2022 | Participants completed a questionnaire at 3 weeks | Not discussed | Correlation between non-adherence and Beck's depression inventory score | Difficulties with daily activities e.g using the bathroom, dressing, personal hygiene, grooming, eating, worship, housework, dressing kids, driving, using mobile phone, using remote control, working |
| Also reported not wanting to wear splint and ashamed of splint | ||||
| Some patients reported that they did not care or believe in the splint benefit | ||||
| Silverio, Cheung 2014 | Analysis of study data | Not discussed | Correlation between being a smoker and non-adherence | Not discussed |
| Mortazavi et al 2023 | Patient diaries | Splint discomfort and stiffness | Not discussed | Not discussed |
| Weir et al 2023 | Study data correlated with adherence | Not discussed | Correlation between male sex and higher BMI | Not discussed |
| Cole et al 2023 | Semi-structured interviews and photovoice software | Not discussed | Not discussed | Difficulties carrying out work duties, washing hands, holding mugs, dressing and writing |
| Some patients thought the splint became grubby and did not like the appearance | ||||
| Skin problems also reported due to moisture under splint | ||||
Therapist reported barriers included the financial burden of attending appointments,22,38 a decreased perception of injury and rehabilitation complexity,27,38 language barriers and decreased comprehension of instructions 38 and splint discomfort and stiffness. 35 Roh et al 31 also suggested that there was a correlation between adherence and decreased occupational level, physical activity, and psychological factors. A link between adherence and clinical empathy was also made. 22
Several studies used demographic data and adherence data to make inferences regarding adherence. Roh et al 31 reported a strong correlation between health literacy and adherence and suggested that poor health literacy was linked to poor adherence. Two further studies discussed the link between psychological well-being and adherence but reported conflicting findings with one study suggesting a link between Beck’s depression score and adherence 32 and another study reporting no link between adherence and the psychological related data. 30 Correlations were also noted between being a smoker and non-adherence. 33 Male sex was also linked to increased non-adherence. 30
Patient reported barriers to adherence were cited as being predominantly due to limitations in functional activities and the hygiene and appearance of the splint.24,27,28,32 Participants reported significant difficulty in carrying out daily functional activities such as caring for themselves,28,32 caring for their baby or children,24,32 cooking,24,32 driving 32 and carrying out their job.24,27,28,32 Savaş an Aydoğan 32 listed many factors that contributed to participants removing their splint (23 in total). In addition to those noted above, necessary religious activities were also linked to adherence. This led these authors to conclude that to perform daily tasks, participants had to be non-adherent. 24
Kolmus et al 24 also reported that participants removed their splint early if they felt their clinical outcome (range of movement) had improved. The belief that outcome could be affected by adherence was also reported by O'Brien et al. 27 They suggested that if participants in their study could positively influence their outcome, they were more likely to be adherent to their splint.
Methodological quality
Of the three RCTs included in this trial,22–24 two were assessed as ‘low risk of bias23,24 and one study was considered as having as ‘some concerns’. 22 However, although The CASP checklist 25 applied to all the studies in this review is not designed to provide a reporting outcome, a summary can be found in the Supplementary material Table 1 as a measure of quality.
Discussion
Despite being a critical aspect of healthcare provision, adherence to treatment is often poorly reported and under investigated in clinical research. Upper limb splinting therapy is no exception to this. In this present systematic review, we have identified a wide variety in the methods used in the measurement of adherence, with no obvious clear standard practice. We also have identified several different factors that have been associated with poor adherence to splinting in a clinical context.
Measuring adherence
The ability to measure splint adherence accurately and objectively, and assess a participant as being adherent to wearing their splint, is not only important in clinical practice, but also in research settings. In healthcare, poor adherence often leads to poor outcomes and an increase in usage, which is costly both for patients and for the National Health Service (NHS).13,40,41 Being able to measure adherence has therefore been identified as a major global challenge. 41 In research, for those trials aiming to compare one treatment modality to another, it is essential to understand the participants’ adherence to the treatment. Researchers need to be able to confidently classify someone as being adherent to a splint or not to mitigate the risk of a type 2 error in their trial. If participants are not adherent, the study cannot show the effectiveness of interventions with any certainty.
In this present review, a variety of methods of assessing adherence were employed, and it is notable that there was not one predominant technique employed. Patient or clinician reported measures of adherence (interview, diaries self-reported patterns) are commonly used both in clinical practice 42 and in clinical trials, particularly in relation to pharmacological studies. 43 They are a quick, cheap, and easy method of establishing adherence rates. However, it is well documented that patients reported overestimate their adherence significantly. 44 To improve the reliability of adherence data several studies reported in this review developed their own novel questionnaires,24,32 however the specific details of these questionnaires were lacking 24 and therefore the methodological robustness of these questionnaires remains unclear.
This review also highlighted the use of two established adherence measurement tools namely the MAM 45 and the Groth classification system. 39 The MAM is a screening tool that aims to identify self-reported barriers to adherence and assess adherence. 45 This tool was originally developed for the paediatric population. The Groth classification system measures adherence by combining information on the patients’ splint wear, exercise programme and attendance to their therapy appointments. 39 Although these measures attempt to provide a more reliable, quantifiable measure of adherence, they are non-validated measures, relying predominantly on patient or therapist reported data, and therefore are subject to the same limitations as other self-reported measures of adherence.
Due to these limitations in patient reported adherence data, there remains a lack of a gold standard method of measuring adherence. 15 In recent years there has been a move towards using electronic sensors to monitor adherence, particularly for measuring adherence to medication. These sensors can be embedded in medical devices to measure temperature, pressure, or movement changes and this provides quantitative data, which can be used to classify adherence. The ‘Orthotimer’ sensor and ‘HOBO MX2201’ are two such devices. These temperature sensors are embedded within a prescribed orthosis and monitors temperature at pre-defined time intervals to measure on/off wear. The data are then downloaded and analysed to give an objective measure of adherence. In this the review, the studies by Grubhofer et al 37 and Weir et al 35 embedded these sensors in shoulder abduction brace/sling, and adherence measured by comparing the wear time data captured from the sensors, with the prescribed wear time.
The use of electronic sensors may appear to provide the accurate, reliable data required to measure adherence. However, a recent systematic review of electronic devices or sensors demonstrates that many of the sensors used are not practical for studies outside the laboratory and there are still accuracy concerns, with many of them either under or over estimating adherence. 42 For example, temperature sensors are reported to be sensitive to ambient temperature and therefore may give a false reading of don/doff time. 42
The other challenge facing clinicians and researchers is the quantification of adherence. They must use the adherence data to then define someone as being adherent or non-adherent to the prescribed intervention. This review has demonstrated that there is also no consensus on the methods used to quantify adherence. Some authors suggest that adherence should be 100% to be classified as adherent.32,36 However, in relation to splint wearing this is likely to be unachievable. We would suggest that a more pragmatic approach to providing a meaningful adherence classification may be to calculate the measure of crude adherence and reduce this by an acceptable proportion of non-adherence, to give a threshold that must be met to be classified as being adherent. In relation to splint wearing, this may be, for example activities such as wound care, hand washing, hand therapy treatment sessions or removing the splint for religious practices. This approach would allow investigators to set a percentage threshold, that could be used to classify adherence. If the adherence data shows a percentage wear time above the threshold they could be classified as adherent and below that threshold. This was also the broad approach Grubhofer et al 37 and Weir et al 35 took using a threshold of 80%. Anything above this was classed as adherent, anything below this non-adherent.
It should be noted that the distribution of the wear time could also be an important consideration in adherence clinically. For example, someone may be prescribed to always wear a splint for 5 weeks, and using this classification they could remove their splint for a whole week and still be deemed highly compliant. Investigators may therefore also wish to set additional rules such as the splint must be worn each day and removed for no longer than 30 min at a time. Although this may provide a more accurate measure of adherence, it also adds to the complexity of data analysis.
When attempting to measure adherence we must also consider the functional activities that are carried out whilst the splint has been removed. In clinical practice, the types of activities that a participant carries out with their hand whilst not wearing the splint may be just as important on outcome as the total wear time and adherence. For example, if someone has had a finger flexor tendon repair and wears their splint 95% of the time but removes it to change a car tyre - they may still be classified as highly adherent, but that one activity may lead to tendon re-rupture and failure of treatment. Some of the papers included in this review included questions around the functional use of the hand whilst not wearing the splint 32 or asked about the reasons why participants removed their splint and barriers to adherence, 24 a question that is also included in the MAM used by Silverio and Cheung 33 and Mercurio et al. 30
Barriers to adherence
Barriers to adherence are well documented in the literature, 46 particularly in relation to adherence to medication regimes. This is reported in the MAM published in 2003 1 which, as previously discussed, provides a framework for understanding adherence.
Many of these barriers are also commonly seen in relation to splint wearing. Kaskutas and Powell 26 reported that patients in their study had significant difficulty in carrying out daily functional activities such as caring for their baby, cooking, and working. Similarly, Savas and Aydogan 32 reported 23 different reasons that participants gave for removing their splint in their questionnaire 3 weeks post-surgery.
Given the poor adherence rates to medical intervention described by the WHO 1 (50% non-adherence) it is vital that clinicians try and understand potential barriers to treatment. If clinicians understand these barriers, they then can have meaningful conversations, and make patient-centred decisions about which treatment the patient is most likely to adhere to.
Limitations of this review
There are a number of limitations to this present study. Firstly, our focus was solely on studies pertaining to the treatment of the upper limb. However, further studies relating to the lower limb and spine may also have yielded important information regarding the measurement of splint adherence. Similarly, case series, and grey literature were also excluded from this search, which may also have provided further data. However, these exclusion criteria were necessary to provide a direct answer to the specific question under consideration, and also to preserve the quality of data assessment.
Furthermore, it was not possible to perform a meta-analysis of the results. In an ideal scenario, our data synthesis would have included a direct comparison of study outcomes. However, due to data heterogeneity this was not possible and therefore a narrative synthesis was performed instead.
Finally, it is also true that the definition of the term ‘splint’ is not used uniformly in the literature. Throughout this report, we have used the term ‘splint’ to reflect the commonly preferred terminology of United Kingdom (UK) based hand therapists, but it is possible that understanding of this has differs between the studies we included. However, this was however mitigated against to some degree by the use of the terms ‘orthosis’ and ‘brace’ alongside ‘splint’ in our search strategy.
Conclusion
This review demonstrates that the methods used to measure adherence and quantify adherence in upper limb splinting following traumatic injury, are inconsistent. Several methods have been presented, but all have limitations. Many studies in this review rely on self-reported adherence data and although data collection is quick, convenient, and cheap and regularly used in studies, it is however, well known to be unreliable due to recall bias. 42 The use of sensors to measure adherence could provide more quantitative and reliable data and is often seen as the optimal method of measuring adherence as they provide objective continuous tracking of behaviour, 15 however this technology is in its infancy, and more work is required to increase the reliability of these. Once reliable tools measuring adherence have been developed, researchers then need to establish an agreed classification system to categorise someone as being adherence or non-adherent to an upper limb splint following trauma.
For clinical trials studying a splint or medical device, it is essential that researchers are confident that participants are using the prescribed splint as advised. Being able to measure adherence and accurately classify adherence raises this confidence and ensures data rigor.
This review has also covered the barriers to splint adherence. If researchers and clinicians can understand the barriers to splint adherence, and aim to mitigate these barriers, patients and participants are more likely adhere to the splint provided. As improved adherence is linked to better health outcomes and decreased health utilisation, 1 this is of utmost importance.
Ultimately, being able to measure and understand barriers to splint adherence will enable researchers to conduct high-quality trials and allow clinicians to make patient-centred decisions around splint prescribing. Therefore, further research is needed to establish robust methods to measure and classify adherence and identify the barriers to splint adherence.
Supplemental Material
Supplemental Material for What are the barriers to upper limb splint adherence, and how is adherence measured? A systematic review by Emma Bamford, Jamie A Mawhinney, Nick Johnson, Ian Shelton, Anna Selby, Avril Drummond in Hand Therapy
Author contributions: EB conceived and led the project; EB, AD and NAJ designed the project; EB, JAM, IS and AS reviewed the abstracts, manuscripts and performed data extraction; EB performed the analysis, EB and JAM wrote the paper; all authors reviewed the manuscript; AD and NJ supervised the project.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: EB is Chief Investigator, AD Co-Chief Investigator and AS and NJ are co-applicants of Flexor Injury Rehabilitation Splint Trial (FIRST) - an NIHR HTA funded Multi-centre RCT NIHR133582. No data directly collected from FIRST is included in this review. IS and JAM have no declarations of interest to declare.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was partly funded by an NIHR/HEE Pre-Doctoral Fellowship completed by EB at the University of Nottingham and supervised by AD.
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs
Emma Bamford https://orcid.org/0000-0002-1588-5708
Anna Selby https://orcid.org/0000-0003-1098-5782
References
- 1.World Health Organisation . Adherence to Long-Term Therapies: Evidence for Action. WHO (World Health Organisation), 2003. https://www.paho.org/en/documents/who-adherence-long-term-therapies-evidence-action-2003 (accessed 19 March 2024). [Google Scholar]
- 2.Urquhart J. Patient non-compliance with drug regimens: measurement, clinical correlates, economic impact. European Heart Journal 1996. DOI: 10.1093/eurheartj/17.suppl_a.8. [DOI] [PubMed] [Google Scholar]
- 3.Vermeire E, Hearnshaw H, Van Royen P, et al. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther 2001; 26: 331–342. DOI: 10.1046/j.1365-2710.2001.00363.x. [DOI] [PubMed] [Google Scholar]
- 4.Aldan G, Helvaci A, Ozdemir L, et al. Multidimensional factors affecting medication adherence among patients with chronic obstructive pulmonary disease. J Clin Nurs 2022; 31: 1202–1215. [DOI] [PubMed] [Google Scholar]
- 5.Kloppenburg M, Van Beest S, Kroon FPB. Thumb base osteoarthritis: a hand osteoarthritis subset requiring a distinct approach. Best Pract Res Clin Rheumatol 2017; 31: 649–660. DOI: 10.1016/j.berh.2018.08.007. [DOI] [PubMed] [Google Scholar]
- 6.Tang JB. Flexor tendon injuries. Clin Plast Surg 2019; 46: 295–306. [DOI] [PubMed] [Google Scholar]
- 7.Jawed A, Ansari MT, Gupta V. TFCC injuries: how we treat? J Clin Orthop Trauma 2020; 11: 570–579. DOI: 10.1016/j.jcot.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lewis KJ, Coppieters MW, Ross L, et al. Group education, night splinting and home exercises reduce conversion to surgery for carpal tunnel syndrome: a multicentre randomised trial. J Physiother 2020; 66: 97–104. DOI: 10.1016/j.jphys.2020.03.007. [DOI] [PubMed] [Google Scholar]
- 9.Thakker A, Gupta VK, Gupta KK. The anatomy, presentation and management options of cubital tunnel syndrome. J Hand Surg Asian Pac Vol 2020; 25: 393–401. DOI: 10.1142/S2424835520400032. [DOI] [PubMed] [Google Scholar]
- 10.Kerr L, Jewell VD, Jensen L. Stretching and splinting interventions for poststroke spasticity, hand function, and functional tasks: a systematic review. Am J Occup Ther 2020; 74: 7405205050p1–7405205050p15. DOI: 10.5014/ajot.2020.029454. [DOI] [PubMed] [Google Scholar]
- 11.Roll SC, Hardison ME. Effectiveness of occupational therapy interventions for adults with musculoskeletal conditions of the forearm, wrist, and hand: a systematic review. Am J Occup Ther 2017; 71: 7101180010p1–7101180010p12. DOI: 10.5014/ajot.2017.023234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sandford F, Barlow N, Lewis J. A study to examine patient adherence to wearing 24-hour forearm thermoplastic splints after tendon repairs. J Hand Ther 2008; 21: 44–52. [DOI] [PubMed] [Google Scholar]
- 13.O’Brien L. Adherence to therapeutic splint wear in adults with acute upper limb injuries: a systematic review. Hand Ther 2010; 15: 3–12. [Google Scholar]
- 14.Kvarnstrom K, Airaksinen M, Liira H. Barriers and facilitators to medication adherence: a qualitative study with general practitioners. BMJ Open 2018; 8: e015332. DOI: 10.1136/bmjopen-2016-015332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mason M, Cho Y, Rayo J, et al. Technologies for medication adherence monitoring and technology assessment criteria: narrative review. JMIR Mhealth Uhealth 2022; 10: e35157. DOI: 10.2196/35157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hickey S, Rodgers J, Wollstein R. Barriers to adherence with post-operative hand therapy following surgery for fracture of the distal radius. J Hand Microsurg 2015; 7: 55–60. DOI: 10.1007/s12593-014-0168-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. The BMJ 2021; 372: n71. DOI: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bamford E, Shelton I, Mawhinney J, et al. A review of splint adherence in people who have sustained traumatic injuries of the upper limb, and how adherence is measured. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023403415 (accessed 12 March 2024).
- 19.American Society of Hand Therapists . Coding. [Internet] https://asht.org/practice/practice-management/orthotics-related/coding#:∼:text=Splint—Thetermsplintrefers,therapistsforapplyingacast (2024, accessed 27 November 2023).
- 20.Davies G, Yeomans D, Tolkien Z, et al. Methods for assessment of patient adherence to removable orthoses used after surgery or trauma to the appendicular skeleton: a systematic review. Trials 2020; 21: 507. DOI: 10.1186/s13063-020-04456-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Online) 2011; 343: d5928. DOI: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Loewenstein SN, Pittelkow E, Kukushliev VV, et al. The effects of postoperative physician phone calls for hand and wrist fractures: a prospective, randomized controlled trial. Cureus 2022; 14: e22202. DOI: 10.7759/cureus.22202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.O’Brien LJ, Bailey MJ. Single blind, prospective, randomized controlled trial comparing Dorsal aluminum and custom thermoplastic splints to stack splint for acute mallet finger. Arch Phys Med Rehabil 2011; 92: 191–198. [DOI] [PubMed] [Google Scholar]
- 24.Kolmus AM, Holland AE, Byrne MJ, et al. The effects of splinting on shoulder function in adult burns. Burns 2012; 38: 638–644. [DOI] [PubMed] [Google Scholar]
- 25.CASP Checklist . Critical appraisal skills programme (CASP). https://casp-uk.net/casp-tools-checklists/ (accessed 27 November 2023).
- 26.Kaskutas V, Powell R. The impact of flexor tendon rehabilitation restrictions on individuals’ independence with daily activities: implications for hand therapists. J Hand Ther 2013; 26: 22–28. [DOI] [PubMed] [Google Scholar]
- 27.O’Brien L, Presnell S. Patient experience of distraction splinting for complex finger fracture dislocations. J Hand Ther 2010; 23: 249–260. [DOI] [PubMed] [Google Scholar]
- 28.Cole T, Jamwal R, Hirth MJ. Photovoice to explore the patient experience of a relative motion orthosis following a hand injury. J Hand Ther 2023; 36: 433–447. [DOI] [PubMed] [Google Scholar]
- 29.Ayhan E, Kuzucu Y, Aslaner EE, et al. Evaluating stack splint use for mallet finger. J Hand Surg Asian Pac 2021; 26: 47–51. [DOI] [PubMed] [Google Scholar]
- 30.Mercurio M, Castioni D, de Filippis R, et al. Postoperative psychological factors and quality of life but not shoulder brace adherence affect clinical outcomes after arthroscopic rotator cuff repair. J Shoulder Elbow Surg 2023; 32: 1953–1959. DOI: 10.1016/j.jse.2023.02.138. [DOI] [PubMed] [Google Scholar]
- 31.Roh YH, Lee BK, Park MH, et al. Effects of health literacy on treatment outcome and satisfaction in patients with mallet finger injury. J Hand Ther 2016; 29: 459–464. [DOI] [PubMed] [Google Scholar]
- 32.Savaş S, Aydoğan Ç. Factors affecting orthosis adherence after acute traumatic hand tendon repairs: a prospective cohort study. J Hand Ther 2022; 35: 32–40. [DOI] [PubMed] [Google Scholar]
- 33.Silverio LM, Cheung EV. Patient adherence with postoperative restrictions after rotator cuff repair. J Shoulder Elbow Surg 2014; 23: 508–513. [DOI] [PubMed] [Google Scholar]
- 34.Mortazavi K, Carlsson IK, Dahlin LB, et al. Hand function 6 weeks following non-surgically treated proximal phalangeal fractures and factors associated to upper extremity disability. Eur J Physiother 2023; 25: 213–222. [Google Scholar]
- 35.Weir TB, Enobun B, Livesey MG, et al. Increased actual sling wear is associated with better early patient-reported and image-based outcomes after shoulder surgery. J Shoulder Elbow Surg 2023; 32: 1392–1400. [DOI] [PubMed] [Google Scholar]
- 36.Azad A, Kegel G, Phelps J, et al. A prospective analysis of patient characteristics affecting the outcome of dorsal splinting for soft tissue mallet injuries. Hand 2023; 18: 1330–1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grubhofer F, Ernstbrunner L, Gerber C, et al. Effect of abduction brace wearing compliance on the results of arthroscopic rotator cuff repair. JBJS Open Access 2022; 7: e21.00148. DOI: 10.2106/JBJS.OA.21.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mottay N, Govender P, Mpanza D. The use of the ICAM Splint Programme in Zone IV to VII Extensor Tendon Repairs: patient outcomes and clinician experiences in a specialised hand unit in SA. S Afr j occup ther 2020; 50: 23–34. [Google Scholar]
- 39.Groth GN, Wilder DM, Young VL. The impact of compliance on the rehabilitation of patients with mallet finger injuries. J Hand Ther 1994; 7: 21–24. DOI: 10.1016/S0894-1130(12)80037-8. [DOI] [PubMed] [Google Scholar]
- 40.Reach G. How is patient adherence possible? A novel mechanistic model of adherence based on humanities. Patient Prefer Adherence 2023; 17: 1705–1720. DOI: 10.2147/PPA.S419277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Park LG, Howie-Esquivel J, Dracup K. Electronic measurement of medication adherence. West J Nurs Res 2015; 37: 28–49. DOI: 10.1177/0193945914524492. [DOI] [PubMed] [Google Scholar]
- 42.Devanand DB, Kedgley AE. Objective methods of monitoring usage of orthotic devices for the extremities: a systematic review. Sensors 2023; 23: 7420. DOI: 10.3390/s23177420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kubica A, Kosobucka A, Michalski P, et al. Self-reported questionnaires for assessment adherence to treatment in patients with cardiovascular diseases. Medical Research Journal 2018; 2: 115–122. DOI: 10.5603/mrj.2017.0015. [DOI] [Google Scholar]
- 44.Garfield S, Clifford S, Eliasson L, et al. Suitability of measures of self-reported medication adherence for routine clinical use: a systematic review. BMC Med Res Methodol 2011; 11: 149. DOI: 10.1186/1471-2288-11-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zelikovsky N, Schast AP. Eliciting accurate reports of adherence in a clinical interview: development of the medical adherence measure. Pediatr Nurs, vol 34. [PubMed] [Google Scholar]
- 46.Kinnear FJ, Wainwright E, Perry R, et al. Enablers and barriers to treatment adherence in heterozygous familial hypercholesterolaemia: a qualitative evidence synthesis. BMJ Open 2019; 9: e030290. DOI: 10.1136/bmjopen-2019-030290. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for What are the barriers to upper limb splint adherence, and how is adherence measured? A systematic review by Emma Bamford, Jamie A Mawhinney, Nick Johnson, Ian Shelton, Anna Selby, Avril Drummond in Hand Therapy