Abstract
Study Design
Systematic Review.
Objectives
While substantial research has explored the impact of osteoporosis on patients undergoing adult spinal deformity (ASD) correction, the literature remains inconclusive. As such, the purpose of this study is to synthesize and analyze existing studies pertaining to osteoporosis as a predictor of postoperative outcomes in ASD surgery.
Methods
We performed a systematic review and meta-analysis to determine the effect that a diagnosis of osteoporosis, based on ICD-10 coding, dual-energy X-ray absorptiometry (DEXA) or computed tomography, has on the incidence of adverse outcomes following surgical correction of ASD. Statistical analysis was performed using Comprehensive Meta-Analysis (Version 2) using a random effects model to account for heterogeneity between studies.
Results
After application of inclusion and exclusion criteria, 36 and 28 articles were included in the systematic review and meta-analysis, respectively. The meta-analysis identified greater rates of screw loosening amongst osteoporotic patients (70.5% vs 31.9%, P = .009), and decreased bone mineral density in patients who developed proximal junctional kyphosis (PJK) (.69 vs .79 g/cm2, P = .001). The systematic review demonstrated significantly increased risk of any complication, reoperation, and proximal junctional failure (PJF) associated with reduced bone density. No statistical difference was observed between groups regarding fusion rates, readmission rates, and patient-reported and/or functional outcome scores.
Conclusion
This study demonstrates a higher incidence of screw loosening, PJK, and revision surgery amongst osteoporotic ASD patients. Future investigations should explore outcomes at various follow-up intervals in order to better characterize how risk changes with time and to tailor preoperative planning based on patient-specific characteristics.
Keywords: osteoporosis, deformity, spine, thoracolumbar
Introduction
Adult spinal deformity (ASD) represents a complex constellation of spinal pathologies characterized by abnormal sagittal and/or coronal curvature of the spine. 1 These deviations can lead to significant functional impairment and decreased quality of life, often necessitating surgical correction. Amongst patients undergoing deformity correction, osteoporosis is a common comorbidity that predisposes patients to greater risks of postoperative complications as a consequence of compromised bone quality. 2
The intersection of osteoporosis and ASD surgery presents a significant clinical burden globally. The negative impact of osteoporosis on postoperative outcomes following surgical correction of ASD has been well-documented, spanning from increased risk of hardware failure and pseudarthrosis to postoperative vertebral fractures and reoperation.3,4 Dual-energy X-ray absorptiometry (DEXA) scans are therefore routinely incorporated into patients’ preoperative assessments such that they can be medically optimized with anabolic therapy prior to ASD surgery. 5
While a substantial body of research has explored the impact of osteoporosis on patients undergoing ASD surgery, reports within the literature taken in aggregate remain indeterminate.
The current understanding of osteoporosis as a risk factor in ASD surgery therefore remains inconclusive, further contributing to non-uniform clinical practices in detection and appropriate management. 4 As such, the purpose of this study is to synthesize and analyze the existing array of high-quality investigations pertaining to osteoporosis as a predictor of postoperative outcomes in ASD surgery. Doing so would better clarify contemporary knowledge surrounding the effect of osteoporosis, potentially underscoring the need for standardized preoperative optimization.
Methods
Following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, we performed a systematic review to determine the effect of osteoporosis on the incidence of adverse outcomes following surgical correction of adult spinal deformities. Informed consent and IRB approval were not necessary given the nature of this study.
The first step involved querying the Medline (PubMed) database from 1990 through August 2022 using the following terms: “osteoporosis” AND “deformity” AND (“outcomes” OR “revision” OR “reoperation” OR “complication”). All English studies, both prospective and retrospective, were included initially that assessed patients with a diagnosis of osteoporosis and reported on the incidence of radiographic, surgical, clinical, and postoperative outcomes. Patients were defined as having a diagnosis of osteoporosis based on ICD-10 coding or a confirmed diagnosis of decreased bone density on DEXA or computed tomography (CT).
We began our initial exclusion filter by eliminating the following studies: systematic reviews, literature reviews, case reports, studies without osteoporotic patients, studies without relevant postoperative outcomes, technique/treatment comparisons, and those where vertebral surgery was due to specific indications such as trauma, neoplasia, or compression fractures. Furthermore, studies with limited sample sizes, which we defined as less than 20 patients, and those without a surgical intervention performed were also removed. After this preliminary exclusion, full-text articles were removed if they were unrelated to adult lumbar spine deformity, cement augmentation was utilized as part of the surgical intervention, or if the study was performed prior to 1990.
The electronic database search and screening were carried out by 2 independent reviewers. Papers were screened based on title, abstract, and full text, and duplicates were removed. Subsequently, the references of full texts were examined to identify any relevant studies missed within our initial query. These were also subjected to the aforementioned screening criteria, ensuring that only articles reporting on outcomes after surgery for ASD were included. After the study selection was finalized, data collection, systematic review, and meta-analysis were performed.
A data collection sheet was created using the Cochrane Consumers and Communication Review Group’s Data Extraction Template for Included Studies. 6 Eligible articles were reviewed by 3 authors who collected the following information: author name, publication year, study type, patient populations, indications for surgery, and the outcomes assessed. Moreover, study outcomes were further classified into the following groups: radiographic outcomes, surgical outcomes, patient-reported outcomes, and other complications. Finally, the risk of bias was assessed using the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) method, and articles were assigned a GRADE of either very low, low, moderate, or high. 7
Statistical Analysis
Statistical analysis was performed using Comprehensive Meta-Analysis (Version 2). Differences in populations between studies were statistically taken into account by utilizing the random effects model. Factoring in standard deviations and sample sizes, the differences between means were calculated and compared between conditions. Categorical and continuous values with reportable standard deviations were included and P-values <.05 were considered significant.
Results
Study Characteristics
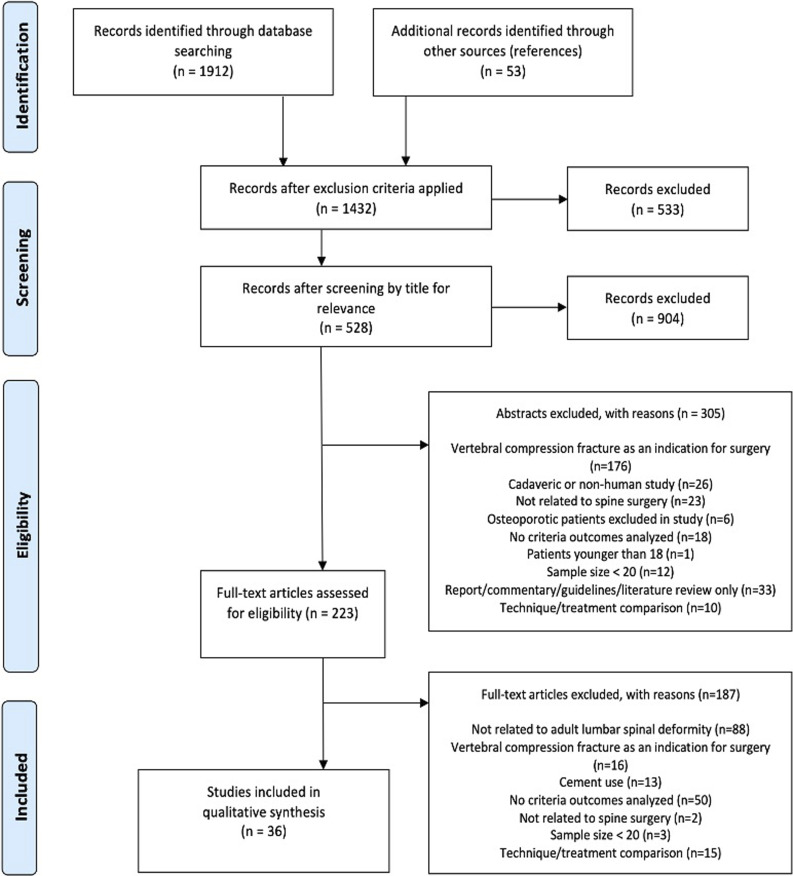
The PRISMA diagram outlines the process of study inclusion and exclusion, as well as the reasons for exclusion (Figure 1). Our initial query of the database yielded 1912 records, as well as 53 additional studies that were later identified through searching references of included papers. After the application of exclusion criteria, 1432 records remained, after which 528 were eligible for inclusion after title screening. Of these, 223 articles underwent full-text review, and 36 were ultimately included in this systematic review. 35 were retrospective studies, and one was a prospective study. 28 articles were included in the meta-analysis (Table 1).
Figure 1.
Study selection process.
Table 1.
Characteristics of Studies Focusing on Outcomes After Surgery for Correction of Adult Spinal Deformity.
| Study | Type of Study | Patient population/Indications | Radiographic Outcomes | Surgical Outcomes | Clinical Outcomes | Complications | Level of Evidence | Quality of Evidence (Grade) |
|---|---|---|---|---|---|---|---|---|
| Yagi et al 2012* | Retrospective case series (n = 76) | Patients undergoing long instrumented (>5 levels) spine fusion for adult idiopathic scoliosis | PJK | IV | Very low | |||
| Park et al 2017 | Retrospective case review (n = 160) | Patients undergoing long spinal fusion to the sacrum for ASD | PJK PJF |
IV | Very low | |||
| Yagi et al al 2011* | Retrospective case series (n = 157) | Patients undergoing long instrumented (>5 levels) spine fusion for adult idiopathic scoliosis | PJK | IV | Low | |||
| Wang et al 2016* | Prospective cohort study (n = 98) | Patients undergoing instrumented segmental posterior spinal fusion (>4 levels) for degenerative lumbar scoliosis | PJK | II | Very low | |||
| Lee et al 2014* | Retrospective comparative study (n = 47) | Patients undergoing lumbar fusion for sagittal imbalance due to lumbar degenerative kyphosis | PJK | III | Very low | |||
| Kyrölä et al 2019* | Retrospective cohort study (n = 79) | Patients undergoing corrective surgery of coronal or sagittal deformity of the spine | PJF Rod breakage |
SRS-30 ODI |
Neural injury | III | Low | |
| Yagi et al 2018 | Retrospective propensity-matched cohort study (n = 113) | Patients undergoing long instrumented (>5 levels) spine fusion for adult idiopathic scoliosis | PJF SVA, PI-LL, PT |
III | Very low | |||
| Hyun et al 2016* | Retrospective database review (n = 44) | Patients undergoing multilevel (>5 levels) spinal instrumented fusion stopping at the thoracolumbar junction (from T9 to L2) for ASD | PJK | III | Low | |||
| Rodriguez-Fontan et al 2020* | Retrospective matched cohort study (n = 80) | Patients undergoing posterior instrumented fusion for correction of ASD | PJK PJF |
III | Low | |||
| Park et al 2020* | Retrospective case series (n = 63) | Patients undergoing all-pedicle-screw instrumentation and fusion for ASD with the upper instrumented level at the thoracolumbar junction | PJF | IV | Low | |||
| Kim et al 2016* | Retrospective case series (n = 49) | Patients undergoing multilevel (>4 levels) posterior fusion with instrumentation for ASD | PJK | IV | Very low | |||
| Kim et al 2020* | Retrospective case series (n = 68) | Patients undergoing long fusion surgery with pelvic fixation using bilateral iliac screws for ASD | PJK Screw loosening |
IV | Low | |||
| Bridwell et al 2013* | Retrospective case series (n = 90) | Patients undergoing primary instrumented multilevel posterior spinal fusion (≥5 levels) for adult idiopathic/degenerative scoliosis | PJK | IV | Very low | |||
| Maruo et al 2013* | Retrospective case series (n = 90) | Patients undergoing long instrumented spinal fusion (≥6 levels) to the sacrum for ASD | PJK | IV | Very low | |||
| Harris et al 2022 | Retrospective cohort study (n = 91) | Patients undergoing posterior spinal fusion (≥5 levels) for ASD | Intraoperative blood loss | III | Low | |||
| Scheer et al 2016* | Retrospective multicenter database study (n = 557) | Patients undergoing posterior spinal fusion for ASD | Overall major intra-or perioperative complications | III | Low | |||
| Raad et al 2017* | Retrospective review (n = 237) | Patients undergoing multilevel (≥5 levels) spinal fusion for ASD | Intraoperative blood loss | III | Low | |||
| Klineberg et al 2016* | Retrospective multicenter database study (n = 380) | Patients undergoing corrective surgery of coronal or sagittal deformity of the spine | Hospital length of stay | III | Low | |||
| Amin et al 2018* | Retrospective review (n = 303) | Patients undergoing multilevel (≥5 levels) spinal fusion for ASD | Nonroutine discharge | III | Low | |||
| Noh et al 2019 | Retrospective comparative study (n = 203) | Patients undergoing multilevel (≥4 levels) posterior spinal fusion for ASD | Overall mechanical complications | III | Low | |||
| Gupta et al 2000* | Retrospective comparative study (n = 399) | Patients undergoing long (≥7 levels) posterior spinal fusion for scoliosis | Revision surgery | III | Low | |||
| Puvanesarajah et al 2016* | Retrospective database review (n = 2293) | Patients undergoing long (≥8 levels) posterolateral spinal fusion for ASD | Revision surgery | III | Low | |||
| Varshneya et al 2022* | Retrospective cohort study (n = 2564) | Patients undergoing long (≥7 levels) posterior spinal fusion for adult spinal scoliosis | Index hospitalization cost Outpatient cost |
Revision surgery Readmission Neural injury Overall complications |
III | Low | ||
| Taliaferro et al 2021* | Retrospective state database review (n = 12 641) | Patients undergoing posterolateral lumbar fusion (≥3 levels) for degenerative spinal deformity | Revision surgery Readmission |
III | Very low | |||
| Yagi et al 2011* | Retrospective database review (n = 176) | Women treated surgically for scoliosis with preoperative BMD assessment of the lumbar spine and femoral neck determined by DXA | Fusion rate | Overall complications | III | Low | ||
| Ploumis et al 2015 | Retrospective case series (n = 54) | Patients undergoing multilevel (≥4 levels) fusions ending at L5 or S1 for ASD | C7PL distance from the midsacrum in the coronal plane | IV | Very low | |||
| Yuan et al 2021* | Retrospective study (n = 130) | Patients undergoing long spinal fusion (≥5 levels) for degenerative lumbar scoliosis | Screw loosening | III | Low | |||
| Banno et al 2019* | Retrospective study (n = 106) | Patients undergoing fusion surgery with bilateral iliac screws for ASD with 2 groups: Conventional two-rod or multi-rod constructs | Screw loosening | III | Low | |||
| Nakazawa et al 2018* | Retrospective case series (n = 23) | Patients undergoing surgery for ASD using S2 alar screws as anchors in the lower vertebrae | SVA, PI-LL Screw loosening |
IV | Low | |||
| O'Leary et al | Retrospective matched cohort analysis (n = 44) | Patients undergoing spinal fusion (≥4 segments) with long segmental pedicle screw constructs for ASD | Pedicle screw fracture | III | Low | |||
| Lertudomphonwanit et al 2018* | Retrospective cohort study (n = 526) | Patients undergoing long posterior fusion (≥5 levels) to the sacrum for ASD | Rod fracture | III | Low | |||
| Kim et al 2015* | Retrospective study (n = 40) | Patients undergoing surgery involving posterior column release with segmental pedicle screw insertion for lumbar degenerative kyphosis | Pseudarthrosis Cage subsidence Proximal adjacent fractures SVA, LL, TK, PT, SL, sagittal decompensation |
III | Low | |||
| Xu et al 2022* | Retrospective study (n = 78) | Patients undergoing lumbosacral instrumentation for degenerative lumbar scoliosis | Screw loosening | III | Low | |||
| Zhang et al 2021* | Retrospective study (n = 79) | Patients undergoing long fusion arthrodesis (≥4 segments) for scoliosis | Low back pain | III | Low | |||
| Yuan et al 2020 | Retrospective cohort study (n = 123) | Patients undergoing spinal fusion for adult degenerative lumbar scoliosis | Minimum clinically important difference in outcome | III | Low | |||
| Passias et al 2020 | Retrospective case series (n = 166) | Patients undergoing surgical correction of ASD with 3 year ODI follow-up | Sustained vs deteriorated functionality | IV | Very low |
* = included in meta-analysis.
PJK/PJF, proximal junctional kyphosis/failure; SVA, sagittal vertical axis; PI-LL, pelvic incidence-lumbar lordosis; LL, lumbar lordosis; TK, thoracic kyphosis; PT, pelvic tilt; C7PL, C7 plumbline; SL, sacral slope; SRS-30, scoliosis research society deformity sequence questionnaire; ODI, Oswestry Disability Index.
Risk of Bias and Quality of Evidence
The level of evidence was determined for each study using the Journal of Bone and Joint Surgery schema. 8 One article was characterized by level II evidence, 24 by level III evidence, and 11 by level IV evidence. The GRADE guidelines were used to assess the quality of evidence, 7 wherein 25 studies were deemed to have very low-quality evidence, and 11 with low quality.
Radiographic Outcomes
Proximal Junctional Kyphosis and Failure
Of the included studies, 14 focused on proximal junctional kyphosis (PJK) and/or failure as radiographic outcomes after surgical correction of ASD (Table 2).9-22 Specifically, 10 papers reported on the significance of osteoporosis as a risk factor for the development of PJK, with four—Wang et al, Hyun et al, Kim et al, and Yagi et al—yielding a significant relationship (P < .001, P = .003, P = .027, and P = .044, respectively).9,10,18,20 Six studies did not find a significant association between lower BMD and the development of PJK,11,13-15,19,21 and Rodriguez-Fontan et al also assessed osteoporosis as a risk factor for the development of either PJK or proximal junctional failure (PJF) but was unable to establish significance. 17
Table 2.
Summarized Results of Studies Focusing on Radiographic Outcomes.
| Study | Type of Study | Patient population/Indications | Outcome of Interest | Results |
|---|---|---|---|---|
| Yagi et al 2012* | Retrospective case series (n = 76) | Patients undergoing long instrumented (>5 levels) spine fusion for adult idiopathic scoliosis | PJK┼ | T-score of PJK group: −1.32 ± .34 T-score of non-PJK group: −1.08 ± .32 |
| Park et al 2017 | Retrospective case review (n = 160) | Patients undergoing long spinal fusion to the sacrum for ASD | PJK PJF┼ |
(+) or (−) osteoporosis: PJK P-value = .55 (+) or (−) osteoporosis: PJF P-value <.001 |
| Yagi et al al 2011* | Retrospective case series (n = 157) | Patients undergoing long instrumented (>5 levels) spine fusion for adult idiopathic scoliosis | PJK | BMD of PJK group: .69 ± .19 g/cm2 BMD of non-PJK group: .79 ± .18 g/cm2 |
| Wang et al 2016* | Prospective cohort study (n = 98) | Patients undergoing instrumented segmental posterior spinal fusion (>4 levels) for degenerative lumbar scoliosis | PJK┼ | BMD of PJK group: −1.4 ± .8 g/cm2 BMD of non-PJK group: −.7 ± .3 g/cm2 Multivariate OR: 3.27 (95% CI: 9.85-91.13, P < .001) |
| Lee et al 2014* | Retrospective comparative study (n = 47) | Patients undergoing lumbar fusion for sagittal imbalance due to lumbar degenerative kyphosis | PJK | BMD of PJK group: −2.19 ± 1.27 g/cm2 BMD of non-PJK group: −1.98 ± 1.58 g/cm2 |
| Kyrölä et al 2019* | Retrospective cohort study (n = 79) | Patients undergoing corrective surgery of coronal or sagittal deformity of the spine | PJF┼ Rod breakage |
PJF group: 50.0% with osteoporosis Non-PJF group: 15.5% with osteoporosis Rod breakage group: 40.0% with osteoporosis Non-rod breakage group: 15.9% with osteoporosis |
| Yagi et al 2018 | Retrospective propensity-matched cohort study (n = 113) | Patients undergoing long instrumented (>5 levels) spine fusion for adult idiopathic scoliosis | PJF┼ PI-LL SVA PT |
T-score < −1.5: 33% with PJF T-score ≥ −1.5: 8% with PJF Univariate OR: 6.4 (95% CI: 1.2-32.3, P < .01) PI-LL of T-score < −1.5: 36.8 ± 23.5° PI-LL of T-score ≥ −1.5: 34.6 ± 23.3° SVA of T-score < −1.5: 81.8 ± 59.1 mm SVA of T-score ≥ −1.5: 80.6 ± 59.2 mm PT of T-score < −1.5: 30.8 ± 11.6° PT of T-score ≥1.5: 30.7 ± 11.7° |
| Hyun et al 2016* | Retrospective database review (n = 44) | Patients undergoing multilevel (>5 levels) spinal instrumented fusion stopping at the thoracolumbar junction (from T9 to L2) for ASD | PJK┼ | T-score of PJK group: −2.5 ± 1.2 T-score of non-PJK group: −1.3 ± 1.3 |
| Rodriguez-Fontan et al 2020* | Retrospective matched cohort study (n = 80) | Patients undergoing posterior instrumented fusion for correction of ASD | PJK + PJF | Multivariate OR: 2.6 (95% CI: .9-6.8, P = .08) |
| Park et al 2020* | Retrospective case series (n = 63) | Patients undergoing all-pedicle-screw instrumentation and fusion for ASD with the upper instrumented level at the thoracolumbar junction | PJF┼ | Multivariate OR: 4.46 (95% CI: 1.13-17.62, P = .03) |
| Kim et al 2017* | Retrospective case series (n = 49) | Patients undergoing multilevel (>4 levels) posterior fusion with instrumentation for ASD | PJK┼ | T-score of PJK group: −2.30 ± .85 T-score of non-PJK group: −1.01 ± .67 |
| Kim et al 2020* | Retrospective case series (n = 68) | Patients undergoing long fusion surgery with pelvic fixation using bilateral iliac screws for ASD | PJK Screw loosening |
T-score of PJK group: −2.9 ± 1.1 T-score of non-PJK group: −2.6 ± 1.3 T-score of screw loosening group: −2.9 ± 1.2 T-score of non-screw loosening group: −2.5 ± 1.3 |
| Bridwell et al 2013* | Retrospective case series (n = 90) | Patients undergoing primary instrumented multilevel posterior spinal fusion (≥5 levels) for adult idiopathic/degenerative scoliosis | PJK | PJK group: 33.3% with osteoporosis Non-PJK group: 32.8% with osteoporosis |
| Maruo et al 2013* | Retrospective case series (n = 90) | Patients undergoing long instrumented spinal fusion (≥6 levels) to the sacrum for ASD | PJK | PJK group: 55% with osteoporosis Non-PJK group: 37% with osteoporosis |
| Yagi et al 2011* | Retrospective database review (n = 176) | Women treated surgically for scoliosis with preoperative BMD assessment of the lumbar spine and femoral neck determined by DXA | Fusion rate | Fusion rate by spine T-score: 88.9% with osteoporosis; 94.1% with osteopenia; 93.5% normal fusion rate by hip T-score: 89.5% with osteoporosis; 93.1% with osteopenia; 94.3% normal |
| Ploumis et al 2015 | Retrospective case series (n = 54) | Patients undergoing multilevel (≥4 levels) fusions ending at L5 or S1 for ASD | C7PL distance from the midsacrum in the coronal plane┼ | F = 4.99 on repeated measures regression analysis (P = .032) |
| Yuan et al 2021* | Retrospective study (n = 130) | Patients undergoing long spinal fusion (≥5 levels) for degenerative lumbar scoliosis | Screw loosening┼ | T-score of screw loosening group: −2.1 ± 1.0 T-score of non-screw loosening group: −1.4 ± 1.5 Multivariate OR: 2.40 (95% CI: 2.40-27.97, P = .001) |
| Banno et al 2019* | Retrospective study (n = 106) | Patients undergoing fusion surgery with bilateral iliac screws for ASD with 2 groups: Conventional two-rod or multi-rod constructs | Screw loosening┼ | T-score of screw loosening group: −1.9 ± 0.9 T-score of non-screw loosening group: −1.0 ± 0.8 Multivariate OR: 2.63 (95% CI: 1.17-5.90, P = .019) |
| Nakazawa et al 2018* | Retrospective case series (n = 23) | Patients undergoing surgery for ASD using S2 alar screws as anchors in the lower vertebrae | Screw loosening PI-LL PI-LL┼ SVA |
T-score of screw loosening group: −2.0 ± 1.16 T-score of non-screw loosening group: −.96 ± .68 T-score of PI-LL <10°: −1.5 ± 1.3 T-score of PI-LL ≥10°: −1.6 ± 1.0 BMD of PI-LL <10°: 1.04 ± .31 BMD of PI-LL ≥10°: .74 ± .17 T-score of SVA <40 mm: −1.6 ± 1.1 T-score of SVA ≥40 mm: −1.5 ± 1.2 |
| O'Leary et al | Retrospective matched cohort analysis (n = 44) | Patients undergoing spinal fusion (≥4 segments) with long segmental pedicle screw constructs for ASD | Pedicle screw fracture | T-score of fracture group: −1.73 ± .76 T-score of non-fracture group: −.58 ± 1.12 |
| Lertudomphonwanit et al 2018* | Retrospective cohort study (n = 526) | Patients undergoing long posterior fusion (≥5 levels) to the sacrum for ASD | Rod fracture┼ | Rod fracture group: 23.5% with osteoporosis Non-rod fracture group: 22.1% with osteoporosis |
| Kim et al 2015* | Retrospective study (n = 40) | Patients undergoing surgery involving posterior column release with segmental pedicle screw insertion for lumbar degenerative kyphosis | Pseudarthrosis SVA LL PT TK SL Sagittal decompensation (SD) Cage subsidence Proximal adjacent fractures |
Rate of pseudarthrosis: 6.3% with osteoporosis, 13.3% with osteopenia, 33.3% with severe osteoporosis SVA of osteopenia: 74.4 ± 58.1 SVA of osteoporosis: 92.8 ± 72.9 SVA of severe osteoporosis: 110.1 ± 92.8 LL of osteopenia: 33.0 ± 2.4 LL of osteoporosis: 33.0 ± 9.3 LL of severe osteoporosis: −33.0 ± 22.1 PT of osteopenia: −37.5 ± 14.7 PT of osteoporosis: −33.1 ± 13.1 PT of severe osteoporosis: 34.6 ± 11.3 TK of osteopenia: 30.6 ± 9.1 TK of osteoporosis: 32.1 ± 16.5 TK of severe osteoporosis: 34.6 ± 11.3 SL of osteopenia: 26.2 ± 8.5 SL of osteoporosis: 24.6 ± 7.5 SL of severe osteoporosis: 26.7 ± 9.9 Osteopenic group: 33.3% with SD Osteoporotic group: 43.8% with SD Severely osteoporotic group: 22.2% with SD Osteopenic group: 6.7% with CS Osteoporotic group: 31.2% with CS Severely osteoporotic group: 22.2% with CS Osteopenic group: 20.0% with fractures Osteoporotic group: 6.3% with fractures Severely osteoporotic group: 33.3% with fractures |
| Xu et al 2022* | Retrospective study (n = 78) | Patients undergoing lumbosacral instrumentation for degenerative lumbar scoliosis | Screw loosening┼ | Screw loosening group: 75.0% with osteoporosis Non-screw loosening group: 20.6% with osteoporosis |
* = included in meta-analysis.
┼ = statistically significant relationship between outcome and osteoporosis (P < .05).
PJK/PJF, proximal junctional kyphosis/failure; SVA, sagittal vertical axis; PI-LL, pelvic incidence-lumbar lordosis; LL, lumbar lordosis; TK, thoracic kyphosis; PT, pelvic tilt; C7PL, C7 plumbline; SL, sacral slope.
In their retrospective case series of 160 patients who underwent long spinal fusion to the sacrum for ASD, Park et al demonstrated that while osteoporosis was not a significant risk factor for the development of PJK, it was a significant predictor of PJF (P < .001). 15 In fact, all 4 articles that investigated PJF found that patients with poor bone stock were at higher risk for developing this complication.12,15,16,22 Kyrölä et al, Park et al, and Yagi et al all established a higher risk of PJF amongst patients with osteoporosis (P = .018, P = .03, and P < .01).12,16,22
Screw Loosening
Five studies assessed the relationship between osteoporosis and screw loosening after surgical correction of ASD, with 3 identifying low BMD as a risk factor.23-25 Yuan et al and Banno et al’s retrospective studies found that patients who experienced screw loosening had lower average T-scores (P = .002 and P = .005, respectively).23,25 Xu et al reported that 20.6% of patients had a diagnosis of osteoporosis in the non-screw loosening group compared with 75.0% in the screw loosening group in their cohort of patients who underwent instrumentation for degenerative lumbar scoliosis (P < .001). 24 In contrast, Kim et al and Nakazawa et al did not report differences in T-scores between patients with and without screw loosening in their respective retrospective studies.11,26
Fusion Rate and Pseudarthrosis
One study reported on the relationship between bone mineral density and fusion rates while the other reported rates of pseudarthrosis, with neither study successfully establishing significance.19,27
Implant Fracture
Two studies investigated the relationship between bone mineral density and the risk of rod fracture,12,28 while 1 study looked at pedicle screw fracture rates. 29 Neither Kyrölä et al nor Lertudomponwanit et al were able to establish an association between osteoporosis and rod breakage.12,28 O’Leary et al, however, found that osteoporotic patients were at significantly increased risk of pedicle screw fracture in their matched cohort analysis patients with long segmental pedicle screw constructs (T-scores: −1.73 ± .76 vs −.58 ± 1.12, P = .02). 29
Cage Subsidence and Adjacent Fractures
Kim et al conducted a study overviewing cage subsidence and adjacent fractures following surgical correction of lumbar degenerative kyphosis but found that neither outcome was more prevalent amongst osteoporotic patients. 27
Spinopelvic Parameters
Other radiographic outcomes assessed in 4 studies included coronal distance of C7 plumbline to the central sacral line (C7PL), pelvic incidence-lumbar lordosis (PI-LL), sagittal vertebral axis (SVA), pelvic tilt, thoracic kyphosis, sacral slope, and sagittal decompensation.22,26,27,30
The one study examining changes in C7PL was a single-center, retrospective review by Ploumis et al In this study, 54 patients who underwent long spinal fusion with ASD demonstrated that osteoporosis was a statistically significant factor for the changes of coronal C7PL (F = 4.99, P = .032). 30
Two studies studied the relationship between osteoporosis and PI-LL in patients with ASD. Nakazawa et al assessed sufficient correction, defined as postoperative PI-LL mismatch <10°, and found that patients with sufficient compared to insufficient correction had significantly different pre-operative BMDs (1.04 ± .31 vs .74 ± .17, P = .03), but not T-scores (−1.5 ± 1.3 vs −1.6 ± 1.0, P = .86). 26 The other study by Yagi et al did not find a difference in PI-LL between the mildly low BMD group and the severely low BMD group. 22
Three papers assessing SVA all determined that osteoporosis was not a significant risk factor for this postoperative radiographic parameter.22,26,27 In addition to SVA, Kim et al investigated other spinopelvic parameters such as lumbar lordosis, pelvic tilt, thoracic kyphosis, sacral slope, and sagittal decompensation in 40 patients with lumbar degenerative kyphosis, none of which were significantly associated with osteoporosis. 27 The other paper by Yagi et al that examined the relationship between pelvic tilt and osteoporosis was also unable to find a significant difference. 22
Complications
Overall Complications
Four studies assessed overall complications of osteoporotic individuals vs non-osteoporotic individuals undergoing surgery for ASD (Table 3).3,19,31,32 Yagi et al and Varshneya et al did not find an association between osteoporosis and a higher rate of complications.3,19 However, Noh et al reported an increased hazard ratio with osteoporosis for the development of mechanical complications after multilevel posterior spinal fusion (HR: .28, 95% CI: .14-.53, P = .0001). 32 Scheer et al also found that osteoporosis was significantly more prevalent in patients who developed complications compared to those who did not (18.9% vs 10.3%, respectively, P = .0065). 31
Table 3.
Summarized Results of Studies Focusing on Rates of Various Complications.
| Study | Type of Study | Patient population/Indications | Outcome of Interest | Results |
|---|---|---|---|---|
| Kyrölä et al 2019* | Retrospective cohort study (n = 79) | Patients undergoing corrective surgery of coronal or sagittal deformity of the spine | Neural injury | Neural injury group: 0% with osteoporosis Non-neural injury group: 23.4% with osteoporosis |
| Scheer et al 2016* | Retrospective multicenter database study (n = 557) | Patients undergoing posterior spinal fusion for ASD | Overall major intra-or perioperative complications┼ | Complication group: 18.9% with osteoporosis No complication group: 10.3% with osteoporosis |
| Noh et al 2019 | Retrospective comparative study (n = 203) | Patients undergoing multilevel (≥4 levels) posterior spinal fusion for ASD | Overall mechanical complications┼ | Multivariate HR: .28 (95% CI: .14-.53, P = .0001) |
| Gupta et al 2000* | Retrospective comparative study (n = 399) | Patients undergoing long (≥7 levels) posterior spinal fusion for scoliosis | Revision surgery┼ | Bivariate OR: 1.75 (95% CI: 1.13-2.71, P = .0130) |
| Puvanesarajah et al 2016* | Retrospective database review (n = 2293) | Patients undergoing long (≥8 levels) posterolateral spinal fusion for ASD | Revision surgery┼ | 1y revision group: 12.7% with osteoporosis 2y revision group: 19.7% with osteoporosis 3y revision group: 22.0% with osteoporosis 4y revision group: 23.5% with osteoporosis 5y revision group: 23.9% with osteoporosis Multivariate OR at 5y: 1.98 (95% CI: 1.60-2.46, P < .0001) |
| Varshneya et al 2022* | Retrospective cohort study (n = 2564) | Patients undergoing long (≥7 levels) posterior spinal fusion for adult spinal scoliosis | Overall complications Revision surgery┼ Readmission Neural injury |
Complication rate: 54.6% in osteoporosis Complication rate: 49.2% in non-osteoporosis 90d revision OR: 1.1 (95% CI: .9-1.4, P = .2561) 6m revision OR: 1.3 (95% CI: 1.0-1.6, P = .0276) 1y revision OR: 1.4 (95% CI: 1.1-1.7, P = .0036) ┼ 2y revision OR: 1.6 (95% CI: 1.3-1.9, P < .001) ┼ 30d readmission OR: 1.4 (95% CI: 1.1-1.9, P = .0098) 60d readmission OR: 1.3 (95% CI: 1.1-1.7, P = .0221) 90d readmission OR: 1.3 (95% CI: 1.1-1.6, P = .0371) Rate of neural injury: 1.0% in osteoporosis Rate of neural injury: .8% in non-osteoporosis |
| Taliaferro et al 2021* | Retrospective state database review (n = 12 641) | Patients undergoing posterolateral lumbar fusion (≥3 levels) for degenerative spinal deformity | Revision surgery┼ Readmission┼ |
Univariate OR: 1.40 (95% CI: 1.13-1.74, P < .001) 30d readmission OR: 1.28 (95% CI: 1.12-1.45, P < .01) 90d readmission OR: 1.37 (95% CI: 1.23-1.53, P < .001) |
| Yagi et al 2011* | Retrospective database review (n = 176) | Women treated surgically for scoliosis with preoperative BMD assessment of the lumbar spine and femoral neck determined by DXA | Overall complications | Complication rate by spine T-score: 27.8% with osteoporosis; 5.9% with osteopenia; 14.9% normal Complication rate based on hip T-score: 10.5% with osteoporosis; 12.6% with osteopenia; 15.7% normal |
* = included in meta-analysis.
┼ = statistically significant relationship between outcome and osteoporosis (P < .05).
Revision Surgery
In total, 4 studies assessed the impact of osteoporosis on rates of revision surgery.2,3,33,34 Gupta et al and Taliaferro both found that osteoporosis significantly increases the likelihood of revision surgery in patients with ASD (P = .013 and P < .001, respectively).2,34 In Puvanesarajah et al’s PearlDiver database review of 2293 patients who underwent ≥8 level primary thoracolumbar posterolateral fusion, osteoporosis was significantly more prevalent in patients who had revisions at 1, 2, 3, 4, and 5 years postoperatively compared to patients who did not undergo reoperation (P < .005 for all). 33 Varshneya et al’s regression analysis of a cohort of Medicare patients undergoing ASD correction identified osteoporosis as an independent risk factor for revision surgery within 1 and 2 years (P = .0036 and P < .001), but not at 90 days or 6 months after surgery. 3
Readmission Rates
Two studies examined the interplay between osteoporosis and readmission following surgery for ASD.3,34 Taliaferro et al’s univariate analysis identified osteoporosis as a significant risk factor for readmission within both 30 days and 90 days after index surgery (P < .01 for both), 34 while Varshneya et al was unable to establish a significant relationship between those who had osteoporosis compared to those who did not at 30, 60, and 90 days after discharge. 3
Neurologic Injury
Two studies assessed the relationship between osteoporosis and neurologic injuries following surgery for ASD.3,12 Neither Kyrölä et al nor Varshneya et al established a significant relationship between these 2 variables.3,12
Surgical and Patient-Reported Outcomes
Surgical Outcomes
Three studies focused on the relationship between osteoporosis and postoperative surgical outcomes including length of stay, total index hospitalization cost, outpatient cost, and discharge disposition.3,35,36 Klineberg et al reported a higher prevalence of osteoporosis in patients with a hospital length of stay ≥9 days. 35 Varshneya et al looked at both total index hospitalization cost and outpatient cost in 2564 Medicare patients undergoing ASD correction surgery. Although the difference in index hospitalization cost was not different, the outpatient cost was significantly greater for patients with osteoporosis compared to those without (P < .05). 3 Finally, Amin et al determined that osteoporosis is a risk factor for non-routine discharge of patients to a rehabilitation facility instead of home (OR: 3.20, 95% CI: 1.70-5.80, P < .001) (Table 4). 36
Table 4.
Summarized Results of Studies Focusing on Surgical, Hospital, and Patient-Related Outcomes.
| Study | Type of Study | Patient population/Indications | Outcome of Interest | Result |
|---|---|---|---|---|
| Kyrölä et al 2019* | Retrospective cohort study (n = 79) | Patients undergoing corrective surgery of coronal or sagittal deformity of the spine | Worst 20th percentile of SRS-30 and/or ODI scores | Multivariate OR: 1.85 (95% CI: .35-9.77, P = .47) |
| Harris et al 2022 | Retrospective cohort study (n = 91) | Patients undergoing posterior spinal fusion (≥5 levels) for ASD | Intraoperative MBL┼ | Osteoporosis group: Mean EBL 2383 ± 1019 mL Non-osteoporosis group: Mean EBL 1482 ± 622 mL Multivariate OR: 2.47 (95% CI: 1.03-5.89, P = .042) |
| Raad et al 2017* | Retrospective review (n = 237) | Patients undergoing multilevel (≥5 levels) spinal fusion for ASD | Intraoperative MBL┼ | MBL group: 33% with osteoporosis Non-MBL group: 15% with osteoporosis Multivariate OR: 2.40 (95% CI: 1.10-5.40, P = .026) |
| Klineberg et al 2016* | Retrospective multicenter database study (n = 380) | Patients undergoing corrective surgery of coronal or sagittal deformity of the spine | Hospital length of stay┼ | LOS ≥9 days: 22.9% with osteoporosis LOS <9 days: 11.3% with osteoporosis |
| Amin et al 2018* | Retrospective review (n = 303) | Patients undergoing multilevel (≥5 levels) spinal fusion for ASD | Nonroutine discharge┼ | Nonroutine discharge: 34% with osteoporosis Discharge to home: 17% with osteoporosis Multivariate OR: 2.4 (95% CI: 1.3-4.5, P = .008) |
| Varshneya et al 2022* | Retrospective cohort study (n = 2564) | Patients undergoing long (≥7 levels) posterior spinal fusion for adult spinal scoliosis | Index hospitalization cost Outpatient cost within 30 days┼ Outpatient cost within 60 days┼ Outpatient cost within 90 days┼ |
Osteoporosis group: $111,088 Non-osteoporosis group: $101,771 Osteoporosis group: $5960 Non-osteoporosis group: $4721 Osteoporosis group: $8421 Non-osteoporosis group: $6620 Osteoporosis group: $10,123 Non-osteoporosis group: $8130 |
| Zhang et al 2021* | Retrospective study (n = 79) | Patients undergoing long fusion arthrodesis (≥4 segments) for scoliosis | Low back pain┼ | No or mild LBP: 45.7% with osteoporosis Moderate/severe LBP: 72.7% with osteoporosis Multivariate OR: 4.57 (95% CI: 1.33-15.77, P = .016) |
| Yuan et al 2020 | Retrospective cohort study (n = 123) | Patients undergoing spinal fusion for adult degenerative lumbar scoliosis | MCID in outcome | T-score of missed MCID: −1.87 ± 1.15 T-score of reached MCID: −1.78 ± 1.20 BMD of missed MCID: .65 ± .14 g/cm2 BMD of reached MCID: .67 ± .13 g/cm2 |
| Passias et al 2020 | Retrospective case series (n = 166) | Patients undergoing surgical correction of ASD with 3 year ODI follow-up | Sustained vs deteriorated functionality┼ | Deteriorated functionality: 22.9% with osteoporosis Sustained functionality: 9.3% with osteoporosis |
* = included in meta-analysis.
┼ = statistically significant relationship between outcome and osteoporosis (P < .05).
SRS-30, scoliosis research society deformity sequence questionnaire; ODI, Oswestry Disability Index; MBL, major blood loss; MCID, minimum clinically important difference; LBP, low back pain.
Intraoperative Blood Loss
Harris et al and Raad et al reported on the relationship between osteoporosis and major blood loss (MBL) during multilevel fusion for ASD, and both established that lower bone mineral density was predictive of increased risk of MBL intraoperatively (P = .042 and P = .026, respectively).37,38
Functional Outcomes
Four studies assessed clinical outcomes in patients with ASD including functionality, level of back pain postoperatively, clinical improvement, and patient satisfaction.12,39-41 Higher rates of osteoporosis were identified in patients with a decline in functionality postoperatively 39 and those with persistent moderate/severe low back pain. 40 However, Yuan et al did not find a difference in T-score or BMD between patients who missed and reached a minimum clinically important difference. 41 Lastly, being in the worst 20th percentile of scoliosis research society deformity sequence questionnaire (SRS-30) and/or Oswestry Disability Index scores were not associated with osteoporosis. 12
Meta-Analysis Results
Overall, 28 studies were eligible for inclusion in the meta-analysis, as marked in Table 1. Forest plots for all analyses in Tables 5 to 7 are available as supplementary files. Table 5 reports on the different rates of 9 outcomes between osteoporotic and non-osteoporotic patients. Only rates of screw loosening were found to significantly differ between osteoporotic and non-osteoporotic patients when pooled from 2 papers (70.5% vs 31.9%, P = .009).23,24 Four articles focused on PJK and found that 37.9% of osteoporotic patients vs 26.3% of patients with normal BMD developed this complication (P = .130).14,17,21,42 Three articles assessed the rate of any complication postoperatively but found no significant differences between osteoporotic and non-osteoporotic patients (35.9% vs 29.4%, P = .683).3,19,43 The overall rate of revision surgery was also not different across the 3 pooled studies, with 30.6% of osteoporotic patients and 21.3% of non-osteoporotic patients undergoing reoperation at any time point after index surgery (P = .081).2,3,33 Two papers reported on PJF,12,16 2 on fusion rates,19,27 2 on rates of neural injury,3,12 2 on rates of rod breakage,12,28 and 2 on readmission rates within 30 days,3,34 but none of these differences were statistically significant.
Table 5.
Results of the Meta-Analysis Comparing Outcomes After Surgery for Deformity of the Adult Thoracolumbar Spine Between Osteoporotic and Non-osteoporotic Patients.
| Outcome | Osteoporosis(%) | Non-osteoporosis (%) | P value |
|---|---|---|---|
| Overall complication rate | 35.9 ± 11.5 | 29.4 ± 11.2 | .683 |
| Fusion rate | 92.0 ± 4.7 | 93.3 ± 1.9 | .795 |
| Rate of neural injury | 1.0 ± 15.5 | 11.5 ± 11.3 | .585 |
| Rate of PJK | 37.9 ± 6.2 | 26.3 ± 4.5 | .130 |
| Rate of PJF | 41.1 ± 13.7 | 16.8 ± 11.4 | .175 |
| Revision surgery rate | 30.6 ± 3.8 | 21.3 ± 3.7 | .081 |
| Rate of rod breakage | 21.0 ± 5.5 | 14.5 ± 3.8 | .330 |
| 30 day readmission rate | 14.8 ± 2.4 | 11.7 ± 2.4 | .366 |
| Rate of screw loosening | 70.5 ± 10.7 | 31.9 ± 10.2 | .009 |
Table 7.
Results of the Meta-Analysis Comparing Bone Quality Between Cases and Controls Where all Patients Underwent Fixation of T10 and Beyond.
| Outcome | Parameter | Cases | Controls | P value |
|---|---|---|---|---|
| Proximal junctional kyphosis | T-score | −2.067 ± .045 | −1.132 ± .048 | <.001 |
| Screw loosening | T-score | - | - | - |
Table 6 reports on the differences in bone quality between cases and controls for PJK and screw loosening using average T-scores. Included papers investigated patients who underwent fixation down to the pelvis to maintain consistency in comparisons. Two studies compared T-scores between PJK and non-PJK cohorts and found that patients who developed PJK had significantly lower T-scores (−2.597 ± .476 vs −1.796 ± .461, P < .001).10,11 Similarly, 2 studies were pooled to assess screw loosening and found that patients who developed this complication had significantly lower T-scores than their counterparts (−2.269 ± .169 vs −1.479 ± .165, P < .001).11,25,26
Table 6.
Results of the Meta-Analysis Comparing Bone Quality Between Cases and Controls Where all Patients Underwent Pelvic Fixation.
| Outcome | Parameter | Cases | Controls | P value |
|---|---|---|---|---|
| Proximal junctional kyphosis | BMD | - | - | - |
| Proximal junctional kyphosis | T-score | −2.597 ± .476 | −1.796 ± .461 | <.001 |
| Screw loosening | T-score | −2.269 ± .169 | −1.479 ± .165 | <.001 |
Table 7 demonstrates differences in T-scores between patients who developed PJK and those who did not after fixation of the T10 segment and beyond. There were an insufficient number of studies available to assess rates of screw loosening in this cohort. Across 4 studies, T-scores were significantly lower amongst patients who developed PJK than those who did not (−2.067 ± .045 vs −1.132 ± .048, P < .001).9,10,13,18
Discussion
Herein, we conduct a systematic review and meta-analysis to assess the impact of osteoporosis on outcomes following ASD surgery. In contrast with degenerative conditions, the management of spinal deformities often involves much lengthier and technically complex surgeries, often with significant complication rates both intraoperatively and postoperatively.3,31,44 Our meta-analysis identified a 30.6% revision rate in osteoporotic patients compared with 21.3% in non-osteoporotic patients across a pooled cohort of 5256 patients, but this difference was not statistically significant (P = .081). Notably, however, all 4 papers in the systematic review that reported on this outcome reported that osteoporosis was a risk factor for the reoperation of ASD.2,3,33,34 With the prevalence of osteoporosis ranging from 16%-61% across these 4 studies, and a reoperation rate between 4.2%-32.1% within a range of 90 days to 5 years, it is possible that these differences may have skewed the results of the meta-analysis. Moreover, Puvanesarajah et al investigated a cohort of 2293 patients who underwent multilevel (≥8 segments) thoracolumbar posterolateral fusion for ASD and found that a significantly greater proportion of patients who underwent reoperation at 1, 2, 3, 4, and 5 years after the index surgery were osteoporotic. Osteoporosis was furthermore a strong independent predictor of 5-year revision rates on their multivariate analysis (OR: 1.98, 95% CI: 1.60-2.46, P < .0001). 33 These results indicate that future investigations into not just reoperation rates, but any outcome after surgery, should be stratified by follow-up period.
Puvanesarajah et al also identified instrumentation failure as the most common reason for reoperation at 5 years, which was present in over 50% of patients who required reoperation. 33 This suggests that the impaired biomechanical strength of osteoporotic bone may present a significant surgical and financial burden. Osteoporosis is a metabolic bone disease that affects the microarchitecture and structural integrity of bone throughout the body, which often means that obtaining sufficient fixation is increasingly challenging in this population.45,46 A large review performed by Akinturk et al in 2022 of 79 articles with a total of 26 207 patients reported an overall complication rate of 34.5%, the most common being hardware failure, PJK, and distal junctional kyphosis. 47 In our study, 2 of 4 papers found that patients with osteoporosis were at significantly increased risk of developing any perioperative or postoperative complication,31,32 and the meta-analysis corroborated that 35.9% of osteoporotic patients experienced complications compared to 29.4% of non-osteoporotic patients (Table 5). In Varshneya et al’s large retrospective database study of 2564 patients, osteoporosis was identified in 61.0% of patients using ICD-9 coding. Although multivariate regression analysis ultimately did not identify osteoporosis as a significant risk factor for the development of postoperative complications, osteoporotic patients had significantly higher rates of select comorbidities, including cancer, history of cerebrovascular accident, and peripheral vascular disease, as well as an overall greater Charlson comorbidity index (P < .0001). 3 Though not directly related to outcomes after spine surgery, these findings highlight the unique challenges that both surgeons and patients face when faced with the interplay between reduced bone mineral density and surgical correction of ASD.
Though it remains unclear to what degree overall complication rates are affected by poor bone stock, we established that rates of pedicle screw loosening do significantly differ. Given the heterogeneity across results, screw loosening was analyzed 2 different ways: the first was based on rates between osteoporotic and non-osteoporotic patients (Table 5), and the second was based on differences in T-scores between patients with and without screw loosening (Table 6). We were able to identify differing rates of screw loosening between osteoporotic and non-osteoporotic patients (70.5% vs 31.9%, P = .009), which is consistent with the current literature.45,48-51 Nonetheless, the clinical significance of screw loosening has not been fully elucidated. In Yuan et al’s retrospective cohort study of 130 patients who underwent a minimum of 5-level fusion for lumbar scoliosis, osteoporosis was identified as a significant risk factor for pedicle screw loosening within the 12-month follow-up period (OR: 2.40, P = .001). However, patients experienced improvements in visual analog scale (VAS) back, VAS leg, SRS-22, and ODI scores after surgery irrespective of the presence or absence of pedicle screw loosening. 23 Several other investigations have shown that functional outcome scores were not affected by pedicle screw loosening.49,52 Other investigations have reported that functional outcomes may be affected by screw loosening, but these were in degenerative lumbar conditions which are distinct from ASD.48,50,53 However, Banno et al compared risk factors and outcomes of iliac screw loosening after ASD correction in 72 patients and reported that patients who developed loosening did not experience improvements in their ODI scores at the 2-year follow-up compared with patients whose screws remained appropriately fitted. 54 These findings indicate that more granular investigations into which patients are at higher risk of subpar clinical improvement are necessary, regardless of the presence or absence of certain radiographic signs.
In addition to screw loosening, our meta-analysis found that patients who developed PJK postoperatively had lower bone mineral densities (BMD) than their non-osteoporotic counterparts (.69 ± .03 g/cm2 vs .79 ± .01 g/cm2, P = .001). Proximal junctional kyphosis is a subtype of adjacent segment disease and is generally defined radiographically by the presence of kyphosis greater than 10° between the lower endplate of the upper instrumented vertebra (UIV) and the upper endplate of the vertebra 2 levels above the UIV.9,10 Proximal junctional kyphosis can result in persistent or recurrent postoperative pain, instability, and neurological deficit, and it is thought to be related to overly rigid instrumentation that results in increased load concentration at the UIV and subsequently accelerated degeneration and kyphosis.17,18,20 The diminished ability of osteoporotic bone to accommodate these increased forces, coupled with the fact that patients with osteoporosis are frequently comorbid with sarcopenia, often exacerbates preexisting propensity for developing adjacent segment disease, or specifically PJK.10,55 A 2022 systematic review and meta-analysis by Han et al overviewing 2388 patients who underwent surgical correction of ASD identified osteoporosis as a significant independent risk factor for the development of PJK (OR: 2.86, 95% CI: 1.64-4.99, P = .0002). 56 The authors also identified overcorrection of lumbar lordosis as a risk factor (OR: 2.20, 95% CI: 1.41-3.42, P = .0005). Specifically, a mismatch between pelvic incidence and lumbar lordosis is a known contributing factor to adjacent segment degeneration, as well as to reduced health-related quality of life scores, both of which are also more prevalent amongst patients with osteoporosis.57-59 These findings highlight the need for careful surgical planning informed by preoperative spinopelvic parameters to minimize the risk of adjacent segment degeneration while still attaining sufficient spinal alignment.
These spinopelvic parameters are frequently assessed pre- and postoperatively and include the coronal distance of C7 plumbline to the central sacral line (C7PL), pelvic incidence-lumbar lordosis (PI-LL), sagittal vertebral axis (SVA), pelvic tilt, thoracic kyphosis, sacral slope, and sagittal decompensation. Of these, 1 paper investigating C7PL established osteoporosis as a risk factor for coronal plane changes, 30 and another found that sufficient correction of PI-LL to <10° was associated with a higher preoperative BMD (P = .03), but not T-score (P = .86). 26 Although our 3 papers investigating SVA correction were unable to establish osteoporosis as a risk factor, sagittal alignment is known to be important for maintaining painless posture, and the compensatory biomechanical processes triggered by sagittal imbalance have been linked with reduced quality of life measures.12,60,61 Nakazawa et al reported that ODI scores at the final follow-up were significantly higher amongst patients who achieved a postoperative SVA increase of <40 mm compared to those with an increase of ≥40 mm. 26 Some investigations suggest that longer fusions may be more suitable for attaining favorable spinopelvic measurements, highlighting the complex interplay between bone quality, objective measurements of the spine, and functional outcomes.26,62,63 As such, it is difficult to draw conclusions regarding the impact of osteoporosis on postoperative spinopelvic parameters from this limited sample of patients, and future investigations utilizing a large cohort are warranted.
While our systematic review and meta-analysis pertaining to the impact of osteoporosis on outcomes after surgical correction of ASD highlights that reduced bone quality indeed may influence select outcomes, our study is not without limitations. Firstly, the retrospective nature of the majority of included studies limits conclusions that may be drawn given the reduced quality and grade of evidence. When performing the meta-analysis, different studies often tracked outcomes using different follow-up periods, which skewed the prevalence of these outcomes. For example, it is unsurprising that reoperation rates would significantly differ between a 90-day vs five-year postoperative period — therefore, more granular data from each study about the number of patients who underwent reoperation within each time interval would provide a more robust analysis of the role osteoporosis might play as a risk factor. To mitigate this concern, we sought to include papers with a minimum of 1-year follow-up or a mean follow-up interval of at least 1 year when this information was available. There were several papers that did not include this information, making uniform application of this criterion more difficult. For this reason, some of the results of the meta-analysis should be interpreted with caution, and this assessment highlights the need for a more uniform method of collecting outcomes based on follow-up length. Lastly, as there is no method in which T-scores and BMD can be retrospectively converted, individual analyses were performed based on measurement technique, which may have diminished the statistical power underlying some of the meta-analysis results given the inability to pool these patients. It may be helpful for future investigations to report both sets of measurements.
Conclusion
This systematic review and meta-analysis sought to determine the impact of osteoporosis as a risk factor for adverse outcomes following surgical correction of ASD. Reduced bone quality was significantly associated with an increased risk of screw loosening, and may also impact rates of reoperation, the development of PJF, and perioperative complications such as increased intraoperative blood loss. In contrast, osteoporosis did not seem to increase the risk of pseudarthrosis, PJK, or hospital readmission. Spinopelvic parameters such as pelvic incidence-lumbar lordosis and the sagittal vertical axis are frequently assessed pre- and postoperatively to determine whether surgical correction was sufficient, but we were unable to identify differences in these measurements between osteoporotic and non-osteoporotic patients. Our findings highlight the need for continued investigation into the magnitude of osteoporosis’s impact on surgical outcomes, especially at various follow-up intervals, with the goal of optimizing medical management and surgical techniques to reduce the frequency of complication events in this vulnerable population.
Supplemental Material
Supplemental Material for The Effect of Osteoporosis on Complications and Reoperation Rates After Surgical Management of Adult Thoracolumbar Spinal Deformity: A Systematic Review and Meta Analysis by Elizabeth A. Lechtholz-Zey, Brandon S. Gettleman, Mina Ayad, Emily S. Mills, Hannah Shelby, Andy Ton, Ishan Shah, Michael M. Safaee, Jeffrey C. Wang, Ram K. Alluri, and Raymond J. Hah in Global Spine Journal
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Elizabeth A. Lechtholz-Zey, Brandon S. Gettleman, Mina Ayad, Emily S. Mills, Hannah Shelby, Andy Ton, and Ishan Shah have nothing to disclose. Michael M. Safaee has received grant funding from ATEC, NuVasive, DePuy Synthesis for lectures and presentations, and financial support from USC for attending meetings. Jeffrey C. Wang has received intellectual property royalties from Zimmer Biomet, NovApproach, SeaSpine, and DePuy Synthes. Raymond J. Hah has received grant funding from SI bone, consulting fees from NuVasive, and support from the North American Spine Society to attend meetings. Ram K. Alluri has received grant funding from NIH, consulting fees from HIA Technologies, and payment from Eccentrial Robotics for lectures and presentations.
IRB Statement: Institutional review board (IRB) approval was not required as no patient information was collected for this study.
Supplemental Material: Supplemental material for this article is available online
ORCID iDs
Andy Ton https://orcid.org/0000-0002-8891-0353
Ishan Shah https://orcid.org/0009-0008-0910-5956
Ram K. Alluri https://orcid.org/0000-0001-5919-707X
Raymond J. Hah https://orcid.org/0000-0001-7513-3519
References
- 1.Kim HJ, Yang JH, Chang DG, et al. Adult spinal deformity: current concepts and decision-making strategies for management. Asian Spine J. 2020;14(6):886-897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta A, Cha T, Schwab J, et al. Osteoporosis increases the likelihood of revision surgery following a long spinal fusion for adult spinal deformity. Spine J. 2021;21(1):134-140. [DOI] [PubMed] [Google Scholar]
- 3.Varshneya K, Bhattacharjya A, Jokhai RT, et al. The impact of osteoporosis on adult deformity surgery outcomes in Medicare patients. Eur Spine J. 2022;31(1):88-94. [DOI] [PubMed] [Google Scholar]
- 4.Gupta A, Cha T, Schwab J, et al. Osteoporosis is under recognized and undertreated in adult spinal deformity patients. J Spine Surg. 2021;7(1):1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carlson BC, Robinson WA, Wanderman NR, et al. A review and clinical perspective of the impact of osteoporosis on the spine. Geriatr Orthop Surg Rehabil. 2019;10:2151459319861591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ryan R, Synnot A, Prictor M, Hill S. Cochrane consumers and communication review group. Data extraction template for included studies. Group CCaCR. https://cccrgcochraneorg [Google Scholar]
- 7.Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383-394. [DOI] [PubMed] [Google Scholar]
- 8.Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85(1):1-3. [PubMed] [Google Scholar]
- 9.Hyun SJ, Kim YJ, Rhim SC. Patients with proximal junctional kyphosis after stopping at thoracolumbar junction have lower muscularity, fatty degeneration at the thoracolumbar area. Spine J. 2016;16(9):1095-1101. [DOI] [PubMed] [Google Scholar]
- 10.Kim DK, Kim JY, Kim DY, Rhim SC, Yoon SH. Risk factors of proximal junctional kyphosis after multilevel fusion surgery: more than 2 years follow-up data. J Korean Neurosurg Soc. 2017;60(2):174-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim YH, Ha KY, Chang DG, et al. Relationship between iliac screw loosening and proximal junctional kyphosis after long thoracolumbar instrumented fusion for adult spinal deformity. Eur Spine J. 2020;29(6):1371-1378. [DOI] [PubMed] [Google Scholar]
- 12.Kyrölä K, Kautiainen H, Pekkanen L, Mäkelä P, Kiviranta I, Häkkinen A. Long-term clinical and radiographic outcomes and patient satisfaction after adult spinal deformity correction. Scand J Surg. 2019;108(4):343-351. [DOI] [PubMed] [Google Scholar]
- 13.Lee JH, Kim JU, Jang JS, Lee SH. Analysis of the incidence and risk factors for the progression of proximal junctional kyphosis following surgical treatment for lumbar degenerative kyphosis: minimum 2-year follow-up. Br J Neurosurg. 2014;28(2):252-258. [DOI] [PubMed] [Google Scholar]
- 14.Maruo K, Ha Y, Inoue S, et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine. 2013;38(23):E1469-E1476. [DOI] [PubMed] [Google Scholar]
- 15.Park SJ, Lee CS, Chung SS, Lee JY, Kang SS, Park SH. Different risk factors of proximal junctional kyphosis and proximal junctional failure following long instrumented fusion to the sacrum for adult spinal deformity: survivorship analysis of 160 patients. Neurosurgery. 2017;80(2):279-286. [DOI] [PubMed] [Google Scholar]
- 16.Park SJ, Lee CS, Park JS, Lee KJ. Should thoracolumbar junction be always avoided as upper instrumented vertebra in long instrumented fusion for adult spinal deformity?: Risk factor analysis for proximal junctional failure. Spine. 2020;45(10):686-693. [DOI] [PubMed] [Google Scholar]
- 17.Rodriguez-Fontan F, Reeves BJ, Noshchenko A, et al. Strap stabilization for proximal junctional kyphosis prevention in instrumented posterior spinal fusion. Eur Spine J. 2020;29(6):1287-1296. [DOI] [PubMed] [Google Scholar]
- 18.Wang H, Ma L, Yang D, et al. Incidence and risk factors for the progression of proximal junctional kyphosis in degenerative lumbar scoliosis following long instrumented posterior spinal fusion. Medicine. 2016;95(32):e4443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yagi M, King AB, Boachie-Adjei O. Characterization of osteopenia/osteoporosis in adult scoliosis: does bone density affect surgical outcome? Spine. 2011;36(20):1652-1657. [DOI] [PubMed] [Google Scholar]
- 20.Yagi M, King AB, Boachie-Adjei O. Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine. 2012;37(17):1479-1489. [DOI] [PubMed] [Google Scholar]
- 21.Bridwell KH, Lenke LG, Cho SK, et al. Proximal junctional kyphosis in primary adult deformity surgery: evaluation of 20 degrees as a critical angle. Neurosurgery. 2013;72(6):899-906. [DOI] [PubMed] [Google Scholar]
- 22.Yagi M, Fujita N, Tsuji O, et al. Low bone-mineral density is a significant risk for proximal junctional failure after surgical correction of adult spinal deformity: a propensity score-matched analysis. Spine. 2018;43(7):485-491. [DOI] [PubMed] [Google Scholar]
- 23.Yuan L, Zhang X, Zeng Y, Chen Z, Li W. Incidence, risk, and outcome of pedicle screw loosening in degenerative lumbar scoliosis patients undergoing long-segment fusion. Global Spine J. 2023;13:1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu F, Zhou S, Zou D, Li W, Sun Z, Jiang S. The relationship between S1 screw loosening and postoperative outcome in patients with degenerative lumbar scoliosis. BMC Musculoskelet Disord. 2022;23(1):186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Banno T, Hasegawa T, Yamato Y, et al. Multi-rod constructs can increase the incidence of iliac screw loosening after surgery for adult spinal deformity. Asian Spine J. 2019;13(3):500-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nakazawa T, Inoue G, Imura T, et al. Radiographic and clinical outcomes from the use of S2 alar screws in surgery for adult spinal deformity. Global Spine J. 2018;8(7):668-675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim KT, Chan CYW, Lee SH, Huh DS, Son ES. Surgical correction in patients with lumbar degenerative kyphosis who had low bone mineral density: an analysis of 40 patients with a minimum follow-up of two years. Asian Spine J. 2015;9(1):65-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lertudomphonwanit T, Kelly MP, Bridwell KH, et al. Rod fracture in adult spinal deformity surgery fused to the sacrum: prevalence, risk factors, and impact on health-related quality of life in 526 patients. Spine J. 2018;18(9):1612-1624. [DOI] [PubMed] [Google Scholar]
- 29.O’Leary PT, Bridwell KH, Lenke LG, et al. Risk factors and outcomes for catastrophic failures at the top of long pedicle screw constructs: a matched cohort analysis performed at a single center. Spine. 2009;34(20):2134-2139. [DOI] [PubMed] [Google Scholar]
- 30.Ploumis A, Simpson AK, Cha TD, Herzog JP, Wood KB. Coronal spinal balance in adult spine deformity patients with long spinal fusions. J Spinal Disord Tech. 2015;28(9):341-347. [DOI] [PubMed] [Google Scholar]
- 31.Scheer JK, Smith JS, Schwab F, et al. Development of a preoperative predictive model for major complications following adult spinal deformity surgery. J Neurosurg Spine. 2017;26(6):736-743. [DOI] [PubMed] [Google Scholar]
- 32.Noh SH, Ha Y, Obeid I, et al. Modified global alignment and proportion scoring with body mass index and bone mineral density (GAPB) for improving predictions of mechanical complications after adult spinal deformity surgery. Spine J. 2020;20(5):776-784. [DOI] [PubMed] [Google Scholar]
- 33.Puvanesarajah V, Shen FH, Cancienne JM, et al. Risk factors for revision surgery following primary adult spinal deformity surgery in patients 65 years and older. J Neurosurg Spine. 2016;25(4):486-493. [DOI] [PubMed] [Google Scholar]
- 34.Taliaferro K, Rao A, Theologis AA, Cummins D, Callahan M, Berven SH. Rates and risk factors associated with 30- and 90-day readmissions and reoperations after spinal fusions for adult lumbar degenerative pathology and spinal deformity. Spine Deform. 2022;10(3):625-637. [DOI] [PubMed] [Google Scholar]
- 35.Klineberg EO, Passias PG, Jalai CM, et al. Predicting extended length of hospital stay in an adult spinal deformity surgical population. Spine. 2016;41(13):E798-E805. [DOI] [PubMed] [Google Scholar]
- 36.Amin RM, Raad M, Jain A, et al. Risk factors for nonroutine discharge in adult spinal deformity surgery. Spine J. 2019;19(2):357-363. [DOI] [PubMed] [Google Scholar]
- 37.Raad M, Amin R, Jain A, Frank SM, Kebaish KM. Multilevel arthrodesis for adult spinal deformity: when should we anticipate major blood loss? Spine Deform. 2019;7(1):141-145. [DOI] [PubMed] [Google Scholar]
- 38.Harris AB, Wang KY, Mo K, et al. Bone mineral density T-score is an independent predictor of major blood loss in adult spinal deformity surgery. Global Spine J. 2024;14:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Passias PG, Bortz CA, Lafage V, et al. Durability of satisfactory functional outcomes following surgical adult spinal deformity correction: a 3-year survivorship analysis. Oper Neurosurg (Hagerstown). 2020;18(2):118-125. [DOI] [PubMed] [Google Scholar]
- 40.Zhang D, Gao X, Ding W, Cui H. Predictors and correlative factors for low back pain after long fusion arthrodesis in patients with adult scoliosis. Adv Ther. 2021;38(7):3803-3815. [DOI] [PubMed] [Google Scholar]
- 41.Yuan L, Zeng Y, Chen Z, Li W, Zhang X, Ni J. Risk factors associated with failure to reach minimal clinically important difference after correction surgery in patients with degenerative lumbar scoliosis. Spine. 2020;45(24):E1669-E1676. [DOI] [PubMed] [Google Scholar]
- 42.Yagi M, Akilah KB, Boachie-Adjei O. Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine. 2011;36(1):E60-E68. [DOI] [PubMed] [Google Scholar]
- 43.Scheer JK, Mundis GM, Klineberg E, et al. Recovery following adult spinal deformity surgery: the effect of complications and reoperation in 149 patients with 2-year follow-up. Eur Spine J. 2016;25(8):2612-2621. [DOI] [PubMed] [Google Scholar]
- 44.Soroceanu A, Burton DC, Oren JH, et al. Medical complications after adult spinal deformity surgery: incidence, risk factors, and clinical impact. Spine. 2016;41(22):1718-1723. [DOI] [PubMed] [Google Scholar]
- 45.Weiser L, Huber G, Sellenschloh K, et al. Insufficient stability of pedicle screws in osteoporotic vertebrae: biomechanical correlation of bone mineral density and pedicle screw fixation strength. Eur Spine J. 2017;26(11):2891-2897. [DOI] [PubMed] [Google Scholar]
- 46.Wittenberg RH, Shea M, Swartz DE, Lee KS, White AA, 3rd, Hayes WC. Importance of bone mineral density in instrumented spine fusions. Spine. 1991;16(6):647-652. [DOI] [PubMed] [Google Scholar]
- 47.Akıntürk N, Zileli M, Yaman O. Complications of adult spinal deformity surgery: a literature review. J Craniovertebr Junction Spine. 2022;13(1):17-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bokov A, Bulkin A, Aleynik A, Kutlaeva M, Mlyavykh S. Pedicle screws loosening in patients with degenerative diseases of the lumbar spine: potential risk factors and relative contribution. Global Spine J. 2019;9(1):55-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ohtori S, Inoue G, Orita S, et al. Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine. 2013;38(8):E487-E492. [DOI] [PubMed] [Google Scholar]
- 50.Zou D, Muheremu A, Sun Z, Zhong W, Jiang S, Li W. Computed tomography Hounsfield unit–based prediction of pedicle screw loosening after surgery for degenerative lumbar spine disease. J Neurosurg Spine. 2020;32(5):716-721. [DOI] [PubMed] [Google Scholar]
- 51.Coe JD, Warden KE, Herzig MA, McAfee PC. Influence of bone mineral density on the fixation of thoracolumbar implants. A comparative study of transpedicular screws, laminar hooks, and spinous process wires. Spine. 1990;15(9):902-907. [DOI] [PubMed] [Google Scholar]
- 52.Kim JW, Park SW, Kim YB, Ko MJ. The effect of postoperative use of teriparatide reducing screw loosening in osteoporotic patients. J Korean Neurosurg Soc. 2018;61(4):494-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lee CK, Kim D, An SB, et al. An optimal cortical bone trajectory technique to prevent early surgical complications. Br J Neurosurg. 2024;38:208-214. [DOI] [PubMed] [Google Scholar]
- 54.Banno T, Hasegawa T, Yamato Y, et al. Prevalence and risk factors of iliac screw loosening after adult spinal deformity surgery. Spine. 2017;42(17):E1024-E1030. [DOI] [PubMed] [Google Scholar]
- 55.Terracciano C, Celi M, Lecce D, et al. Differential features of muscle fiber atrophy in osteoporosis and osteoarthritis. Osteoporos Int. 2013;24(3):1095-1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Han X, Ren J. Risk factors for proximal junctional kyphosis in adult spinal deformity after correction surgery: a systematic review and meta-analysis. Acta Orthop Traumatol Turc. 2022;56(3):158-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ham DW, Kim HJ, Park SM, Park SJ, Park J, Yeom JS. The importance of thoracolumbar junctional orientation, change in thoracolumbar angle, and overcorrection of lumbar lordosis in development of proximal junctional kyphosis in adult spinal deformity surgery. J Neurosurg Spine. 2022;1(aop):1-9. [DOI] [PubMed] [Google Scholar]
- 58.Sun XY, Zhang XN, Hai Y. Optimum pelvic incidence minus lumbar lordosis value after operation for patients with adult degenerative scoliosis. Spine J. 2017;17(7):983-989. [DOI] [PubMed] [Google Scholar]
- 59.Wu HH, Chou D, Hindoyan K, et al. Upper instrumented vertebra–femoral angle and correlation with proximal junctional kyphosis in adult spinal deformity. Spine Deformity. 2022;10(2):449-455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bess S, Line B, Fu KM, et al. The health impact of symptomatic adult spinal deformity: comparison of deformity types to United States population norms and chronic diseases. Spine. 2016;41(3):224-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Protopsaltis TS, Lafage R, Smith JS, et al. The lumbar pelvic angle, the lumbar component of the T1 pelvic angle, correlates with HRQOL, PI-LL mismatch, and it predicts global alignment. Spine. 2018;43(10):681-687. [DOI] [PubMed] [Google Scholar]
- 62.Kondo R, Yamato Y, Nagafusa T, et al. Effect of corrective long spinal fusion to the ilium on physical function in patients with adult spinal deformity. Eur Spine J. 2017;26(8):2138-2145. [DOI] [PubMed] [Google Scholar]
- 63.Yasuda T, Hasegawa T, Yamato Y, et al. Lumbosacral junctional failures after long spinal fusion for adult spinal deformity—which vertebra is the preferred distal instrumented vertebra? Spine Deformity. 2016;4(5):378-384. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for The Effect of Osteoporosis on Complications and Reoperation Rates After Surgical Management of Adult Thoracolumbar Spinal Deformity: A Systematic Review and Meta Analysis by Elizabeth A. Lechtholz-Zey, Brandon S. Gettleman, Mina Ayad, Emily S. Mills, Hannah Shelby, Andy Ton, Ishan Shah, Michael M. Safaee, Jeffrey C. Wang, Ram K. Alluri, and Raymond J. Hah in Global Spine Journal