Abstract
Objectives
The aim of this study was to assess the efficacy of pelvic osteotomy and ventral fixation of the ischium using cortical screws and polymethylmethacrylate (PMMA) for feline pelvic canal stenosis (PCS) associated with malunion after conservative management of pelvic fractures.
Methods
Surgical pelvic enlargement was performed for PCS in six cats. The medical records, including information on the patients, surgical procedures, defecation and complications, were reviewed. The sacral index (SI) and colonic:lumbar:vertebral ratio (CLVR) were evaluated based on pre- and postoperative radiographs.
Results
This study included five castrated male cats and one spayed female cat. Postoperative improvements in constipation and defecatory difficulty were noted in all cases. The postoperative SI was significantly higher (mean 0.93, range 0.72–1.13) than the preoperative SI (mean 0.59, range 0.45–0.74) (P <0.001). However, no statistically significant change was found in the CLVR preoperatively and up to 3 months postoperatively. A successful union of the ilium was observed, without implant failures. One case developed necrosis of the pubic surgical wound.
Conclusions and relevance
This study indicated the potential benefits of pelvic osteotomy and ventral fixation of the pelvic floor using screws and PMMA for achieving pelvic cavity enlargement in treating feline PCS associated with defecatory problems.
Keywords: Pelvic canal stenosis, pelvic osteotomy, polymethylmethacrylate, ventral fixation
Introduction
Orthopaedic pelvic injuries in cats reportedly include iliac body, pelvic floor, acetabular and ischial fractures, as well as sacroiliac fractures/luxation.1,2 Typical pelvic injury combinations in cats include the following: iliac body fracture with contralateral sacroiliac joint dislocation and pelvic floor fracture; iliac body and pelvic floor fractures with unilateral sacroiliac joint dislocation; or bilateral sacroiliac joint dislocation and pelvic floor fracture. Such multiple orthopaedic pelvic injuries considerably destabilise the pelvic structure.1,2 If left untreated, these fracture combinations can lead to the collapse of the ventral (ischium and pubis) and caudal (beyond the iliac body) components of the pelvis, causing malunion and pelvic canal stenosis (PCS).3,4
PCS resulting from malunion after pelvic fracture contributes to 25% of secondary megacolon cases.4–6 Research suggests that surgical intervention to enlarge the pelvic cavity is recommended if constipation due to PCS is present for less than 6 months.7,8 If constipation persists for more than 6 months, subtotal colectomy is recommended.4,7–9 Although various surgical approaches for PCS have been reported, few reports are available on the short- to long-term follow-up evaluation.3,10–13
The aim of this study was to introduce a novel surgical technique for pelvic enlargement, combining corrective osteotomy of the ilium and pubis with ventral fixation of the pelvic floor using screws and polymethylmethacrylate (PMMA), in cats with PCS and to evaluate its clinical efficacy based on short- to long-term postoperative outcomes. We hypothesised that this method would avoid postoperative restenosis of the pelvis and improve defecatory function.
Materials and methods
Cases
Cases of defecatory difficulty and PCS after pelvic fractures managed at the Veterinary Medical Teaching Hospital of Nippon Veterinary and Life Science University between 2010 and 2019 were included in this study.
Details collected from the medical records included age, weight, sex, defecation status, duration of constipation, surgical method and postoperative complications. Pelvic radiography was performed pre- and postoperatively (see radiographs of cases 1, 2 and 4–6 in the supplementary material), and in some cases, CT was performed preoperatively. Defecatory function, based on owner interviews, was categorised into the following three grades: grade 1 (natural defecation without assistance); grade 2 (no manual removal of faeces but requiring lactulose as oral stool softener); and grade 3 (intermittent or continuous manual removal of faeces necessary). Complications were classified as major if they necessitated additional surgical intervention and minor if not.
Surgery
Anaesthesia was induced using propofol (7 mg/kg IV) and maintained with inhalational isoflurane and oxygen after endotracheal intubation. Fully controlled respiratory management employed a pressure-controlled ventilator (maximum airway pressure 8–15 cm H2O, inspiratory: expiratory ratio 1:2–1:4). Perioperative measures included lactated Ringer’s solution infusion (3–5 ml/kg/h) for blood volume maintenance, epidural administration of 0.5% bupivacaine hydrochloride (0.2 ml/kg) and morphine hydrochloride (0.1 µg/kg), and continuous fentanyl infusion (1–3 µg/kg/h) for analgesia. Antibiotics included cefmetazole (25 mg/kg IV), administered approximately 1 h before skin incision and every 90 mins intraoperatively. 14 All surgeries were performed by one surgeon (YH). After induction of general anaesthesia, the caudal lumbar area and both dorsal and ventral aspects of the pelvis were shaved and aseptically prepared. The cat was positioned in dorsal recumbency and a ventral approach to the pelvis was made. A sagittal saw (Colibri II; DePuy Synthes) was used to create an osteotomy of the pelvic floor. Subsequently, the patient was placed in lateral recumbency to enable surgical exposure of the lateral aspect of the ilium, which was severely displaced into the pelvic cavity. 15 After identifying the caudal edge of the sacroiliac joint, an osteotomy was made perpendicular to the long axis of the ilium.
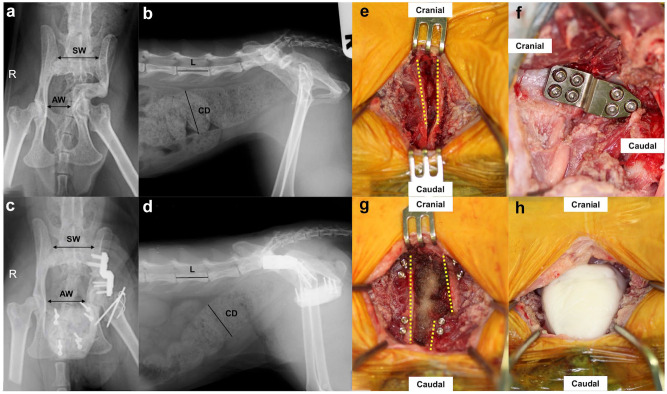
The caudal fragment of the ilium was retracted craniolaterally; a reconstruction (MIZUHO) or custom-made crank plate (Platon Japan Co) was used to stabilise the osteotomy site (Figure 1). Crank plates were available with four, seven or eight screw holes and allowed the use of 2.4 mm cortical screws. The crank plate available with seven screw holes had two and one holes on the cranial and caudal sides, respectively, with locking features. All crank plates were designed to achieve 7.5 mm lateral displacement of the caudal fragment (Figure 2). After wound closure, the patient was placed in dorsal recumbency again and the separation of the ventral pelvic osteotomy was confirmed. Anchor screws were inserted into the ventral aspect of the pubis and ischium. To protect the pelvic cavity organs, such as the ureters and rectum, absorbent haemostatic material (AVITENE; Davol) and a pedunculated fat graft, harvested subcutaneously, were placed into the osteotomy site. Liquid PMMA bone cement (Surgical Simplex; Stryker Japan KK) was applied to incorporate the anchor screws and form a ventral fixation support. During bone cement polymerisation, lavage with 4°C physiological saline was performed to avoid thermal polymerisation damage. The wound was closed once the bone cement had fully solidified.
Figure 1.
(a–d) Radiographic and (e–h) intraoperative findings of case 3. Preoperative (a) ventrodorsal and (b) lateral aspects of the pelvis are shown. Postoperative (c) ventrodorsal and (d) lateral aspects of the pelvis are shown. In the ventrodorsal view, the left ilial body is displaced medially from the caudal edge of the sacroiliac joint; narrowing of the pelvic cavity is clearly observed. The width of the sacrum at the cranial border (SW) and across the width of the pelvic canal at the narrowest point, between the medial cortices of the acetabulae (AW), are indicated by arrows. These measurements are used to calculate the sacral index (SI), which is the ratio of these two measurements. Lateral radiographs show enlargement of the descending colon with marked faecal impaction and deformed fusion of the ilial body. Postoperative radiography reveals pelvic cavity enlargement. The maximum diameter of the colon (CD) and the length of L5 (L) are delineated by solid black bars. (e) Yellow dotted lines indicate the separation line of the pelvic floor osteotomy; (f) the ilium is osteotomised and fixed with a crank plate (seven holes); (g) eight anchor screws are inserted into the ventral aspect of the pelvic floor; (h) placement of polymethylmethacrylate
Figure 2.
A design drawing of a typical crank plate. This shows an eight-hole crank plate. All crank plates are designed to facilitate a 7.5 mm lateral displacement of the caudal bone fragment after ilial osteotomy. Measurements on the drawing are in mm
A fentanyl patch (12.5 μg/h, Duprop MT patch; Janssen Pharmaceutical) was applied to provide analgesia immediately postoperatively. Fentanyl was continuously infused until the patch was effective and was tapered as necessary. The patch was removed 3 days postoperatively. Postoperative management included a 2-week cage rest period and administration of cefmetazole 25 mg/kg IV q12h.
Radiographic evaluation
Bone union after osteotomy of the ilium was assessed using postoperative radiography. Bone union at the osteotomy site of the pelvic floor could not be evaluated because of the presence of PMMA. The integrity of the plates and screws was evaluated at the ilial osteotomy site. It seems unlikely that PMMA was destroyed at the pelvic floor; therefore, the integrity of the screws used was evaluated. Radiographs were taken immediately postoperatively, and at 1.5, 3, 6, 12 and 24 months postoperatively and every year thereafter for cases in which long-term follow-up was possible.
Sacral index
The pelvic shape was assessed using ventrodorsal radiography (Figure 1). The sacral index (SI) was calculated as the ratio of the narrowest width of the pelvic canal (AW) to the width of the cranial sacrum (SW), measured between the medial cortices of the acetabulae (SI = AW/SW). 3
Degree of pelvic canal narrowing
Pelvic canal narrowing was quantified following the methodology described by Hamilton et al. 3 The SI was calculated as the width of the pelvic canal divided by that of the cranial sacrum. The SI of normal cats has been reported to be 0.97. 3 Therefore, the estimated width of the pelvic canal before injury can be calculated by multiplying the normal SI by the cranial sacral width of each case. 3 The degree of pelvic canal narrowing is expressed as the ratio of the original width of the pelvic canal before injury to the width of the pelvic canal after injury. However, since the original width of the pelvic canal before injury cannot be measured, the calculated estimated width of the pelvic canal before injury was used. Subsequently, the degree of pelvic canal narrowing was expressed as a percentage, using the estimated width of the pelvic canal before injury and the narrowed width of the pelvic canal after injury for each case.
Colonic:lumbar:vertebral ratio
The colonic:lumbar:vertebral ratio (CLVR), an index used for assessing defecatory abnormalities, 6 was assessed based on an abdominal lateral radiograph encompassing the lumbar vertebrae and pelvis (Figure 1). The CLVR was calculated as the ratio of the maximum colon diameter to the length of the L5 vertebral body. The colon’s maximum diameter was measured from the ilial tuberosity to the pelvic entrance at its most distended point. 6
Statistical analysis
The SI and CLVR were measured by one examiner (RS). They were also measured by radiographic images using OsiriX-Lite software version 14.0.1 (Pixmeo). Pre- and postoperative SIs and CLVRs were analysed using repeated measures analysis of variance with mixed methods in SAS software version 9.3 (SAS 2011; SAS Institute). The Tukey–Kramer test adjusted for multiple comparisons was used, with significance set at P <0.05. Analyses were conducted preoperatively, immediately postoperatively and 2 weeks, 1.5 months and 3 months postoperatively, acknowledging that regular long-term follow-ups were not available for some cases.
Results
Case information and outcomes
Six cats (five castrated males and one spayed female), weighing 3.6–5.5 kg (mean 4.3 kg), were included in this study. Detailed information of each case is presented in Table 1. Five cats were confirmed to have pelvic malunion upon rescue and subsequently developed PCS. One cat, initially treated conservatively for a pelvic fracture upon rescue, subsequently developed PCS and defecatory problems. All cases had confirmed pelvic malunion and PCS. However, their fracture timelines and post-injury clinical histories were unclear. Of the six cats, five underwent pelvic CT. Details of the orthopaedic injuries are summarised in Table 2. The plates used were a reconstruction plate in one case, a four-hole crank plate in one case, a seven-hole crank plate in one case and an eight-hole crank plate in three cases (Table 2). Preoperatively, all cases were classified as having grade 3 defecatory function. Three months postoperatively, defecatory function improved to grades 1 and 2 in five and one cases, respectively. Two cases of persistent defecatory problems for 2–3 years showed postoperative improvements. The only major complication involved necrosis of the subcutaneous tissue of the pubic surgical wound (case 4).
Table 1.
Characterisation and evaluation of six cats with pelvic canal stenosis
| Case | Breed | Sex | Age (years) | Body weight (kg) | Grade of defecatory abnormality | Duration of clinical signs | SI | Pelvic canal narrowing (%) | Colonic lumbar vertebral ratio | Maximum follow-up period | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative 3 months | Preoperative | Postoperative 3 months | Preoperative | Postoperative 3 months | ||||||||
| 1 | Mixed | SF | 4 | 3.7 | 3 | 3 years | 0.45 | 0.72 | 53.3 | 26.1 | 1.51 | 1.12 | 3 months |
| 2 | Mixed | CM | 2 | 3.6 | 3 | 5 months | 0.43 | 1.13 | 55.2 | −16.8 | 1.07 | 1.03 | 3 years |
| 3 | Mixed | CM | Estimated 4 | 3.6 | 3 | 2–3 years | 0.61 | 1.04 | 37.5 | −6.9 | 1.43 | 1.18 | 3 months |
| 4 | Mixed | CM | Age unknown | 5.4 | 3 | Unknown | 0.76 | 0.90 | 21.6 | 6.9 | 0.96 | 1.06 | 1.5 years |
| 5 | Mixed | CM | Estimated 5 | 3.8 | 3 | Unknown | 0.66 | 1.05 | 32.4 | −8.3 | 1.16 | 0.91 | 4.5 months |
| 6 | Mixed | CM | Estimated 2 | 5.5 | 3 | Unknown | 0.50 | 0.71 | 48.7 | 27.2 | 1.27 | 0.90 | 4 years |
The normal value of the sacral index (SI) is 0.97. SI = width of pelvic canal/width of cranial border of sacrum
CM = castrated male; SF = spayed female
Table 2.
Details of the orthopaedic injuries and implants used in the six cases
| Case | Fracture site | Details of implants | |
|---|---|---|---|
| Body of the ilium | Pelvic floor | ||
| 1 | Left sacroiliac luxation, right femoral neck fracture, left acetabular fracture, fracture of the pubis and ischium | 2.0 mm reconstruction plate (MI) ∅2.0 mm cortical screw ×6 (J&J) |
∅1.5 mm cortical screw ×2 (J&J) ∅2.0 mm cortical screw ×6 (J&J) PMMA |
| 2 | Left ilial body fracture, fracture of the pubis and ischium | Titanium crank plate (4 × 4 hole) (PJ) ∅2.4 mm titanium cortical screw ×4 (PJ) |
∅1.5 mm cortical screw ×10 (J&J) PMMA |
| 3 | Left ilial body fracture, fracture of the pubis and ischium | Titanium crank plate (4 × 3 hole) (PJ) ∅2.4 mm titanium cortical screw ×7 (PJ) ∅2.4 mm titanium locking screw ×7 (PJ) |
∅1.5 mm cortical screw ×8 (J&J) PMMA |
| 4 | Right sacroiliac luxation, fracture of the pubis and ischium | Titanium crank plate (2 × 2 hole) (PJ) ∅2.4 mm titanium cortical screw ×4 (PJ) |
∅1.5 mm cortical screw ×6 (J&J) PMMA |
| 5 | Left ilial body fracture, fracture of the pubis and ischium | Titanium crank plate (4 × 4 hole) (PJ) ∅2.4 mm titanium cortical screw ×4 (PJ) |
∅1.5 mm cortical screw ×8 (J&J) PMMA |
| 6 | Right sacroiliac luxation, fracture of the pubis and ischium | Titanium crank plate (4 × 4 hole) (PJ) ∅2.4 mm titanium cortical screw ×4 (PJ) |
∅1.5 mm cortical screw ×8 (J&J) PMMA |
J&J = Johnson & Johnson; MI = MIZUHO; PJ = Platon Japan Co; PMMA = polymethylmethacrylate
∅ = screw diameter
Radiographic assessment
Five of the six cases (cases 1–3, 5 and 6) exhibited healing of the iliac osteotomy site within 2–6 months postoperatively. In case 4, bone union was confirmed 9 months postoperatively. Throughout the observation period, no failure of metal implants or PMMA was noted.
SI
The evaluation of pre- and postoperative radiographs revealed no pelvic restenosis (Table 1). The mean preoperative SI was 0.57 (range 0.43–0.76), whereas the mean postoperative SI was 0.93 (range 0.72–1.13), indicating a significant postoperative increase (P <0.001) (Table 3). In three cases (cases 2, 4 and 6) with long-term follow-up (1.5–4 years postoperatively), no pelvic restenosis was observed.
Table 3.
Comparison of preoperative and postoperative SI and CLVR in the six cases
| Preoperatively | Immediately postoperatively | 2 weeks postoperatively | 1.5 months postoperatively | 3 months postoperatively | |
|---|---|---|---|---|---|
| SI | 0.57 ± 0.08a | 0.90 ± 0.08b | 0.92 ± 0.08b | 0.94 ± 0.08b | 0.93 ± 0.08b |
| CLVR | 1.23 ± 0.06a | 1.02 ± 0.06a | 1.18 ± 0.06a | 1.01 ± 0.07a | 1.03 ± 0.06a |
Same lowercase letters indicate no significant difference between columns (significance level: P <0.05)
Data are mean ± SE.
CLVR = colonic:lumbar:vertebral ratio; SI = sacral index
Degree of pelvic canal narrowing
Before the corrective surgery, the mean pelvic canal narrowing was 41.5% (range 21.6–55.2). Case 4 exhibited moderate narrowing (10–30%) and five cases (cases 1–3, 5 and 6) showed severe narrowing (>30%) (Table 1). Three cases (cases 1, 2 and 6) had a narrowing of ⩾45%, categorised as high risk for constipation-related issues. 13 Postoperatively, the mean degree of narrowing was reduced to 4.7% (range −6.9 to 27.2), and pelvic cavity enlargement was confirmed in all cases.
CLVR
The mean preoperative CLVR was 1.23 (range 0.96–1.51). The CLVRs of four cases (cases 2 and 4–6) were below 1.28: one (case 3) was in the range of 1.28–1.48 and another (case 1) exceeded 1.48 (Table 1). The mean postoperative CLVR decreased to 1.03 (range 0.90–1.18). None of the cases showed a CLVR >1.48 (indicating a megacolon) after surgery. 6 No significant difference was found in the maximum colon diameter to L5 length ratio from preoperatively to 3 months postoperatively (Table 3).
Discussion
This study evaluated a surgical procedure for achieving pelvic enlargement in cats with PCS, combining pelvic osteotomies and internal fixation of both the ilial and midline osteotomy sites. No case of restenosis of the pelvic cavity was observed postoperatively, and clinical signs improved even in cases with long-term defecatory problems.
Corrective surgical methods for malunion associated with PCS have been reported, including the use of plates, 8 external skeletal fixators, 16 lag screws 13 and spacers.17,18 However, most case reports have lacked long-term follow-up assessments. Schrader 8 evaluated long-term clinical signs after pelvic enlargement but did not include an anatomical evaluation of the pelvic cavity. To our knowledge, no previous reports of combined corrective osteotomy of the ilium and midline pelvic floor with ventral fixation of the pelvic floor using screws and PMMA are available. The present study provides a short- and long-term assessment of both the clinical and anatomical features of pelvic enlargement surgery in cats. PMMA, which is characterised by high compressive strength compared with tensile strength, 19 counteracts forces that may cause medial displacement of the caudal ilial osteotomy fragment. It was hypothesised that by combining ventral fixation of the pubis and ischium, the force that pulls the caudal ilial fragment into the pelvic cavity at the ilial osteotomy site could be neutralised. This study demonstrated a significant postoperative improvement in the SI compared with preoperative values in all cases, without significant pelvic restenosis observed up to 3 months postoperatively. In addition, in three cases of long-term follow-up (approximately 1.5–4 years postoperatively), SI measurements over time indicated no signs of pelvic cavity restenosis compared with immediate postoperative values. Furthermore, no instance of plate fracture or screw loosening was observed throughout the observation period in any case. In 2009, Hamilton et al 3 showed that in approximately half of the cases treated with ilial plating alone, screw loosening occurred within 4–6 weeks, followed by postoperative pelvic stenosis.
A crank or reconstruction plate was used to enlarge the narrowed pelvic cavity in the lateral direction while displacing the osteotomised caudal fragment outward. To prevent restenosis of the pelvic cavity, anchor screws were placed on the ventral aspect of the pelvic floor (ischium and pubis) and these were fixed with PMMA. Notably, two cases (cases 1 and 3), which had constipation and defecatory problems for 2–3 years, showed improvement of clinical signs postoperatively. Despite needing lactulose as an oral stool softener postoperatively, case 1 exhibited improved clinical signs. No significant difference was observed between pre- and postoperative CLVRs. A CLVR >1.48 is indicative of megacolon. 6 In case 1, this ratio was 1.51 preoperatively but did not exceed 1.48 postoperatively, suggesting that pelvic cavity enlargement could alleviate long-term constipation and defecation difficulties. Moreover, surgical treatment could facilitate the management of the constipated patient by periodic manual evacuation. In small animal clinical practice, surgical pelvic cavity enlargement is recommended for PCS-induced constipation lasting for less than 6 months,7,8 whereas subtotal colectomy is advised for durations exceeding 6 months.4,7–9 Our results highlight the potential benefits of pelvic cavity enlargement and reconstruction in resolving PCS, even in cases where constipation secondary to PCS has persisted beyond 6 months.
In this study, a crank plate was used in five cases and a reconstruction plate in one case at the ilial osteotomy site. The crank plate allows a 7.5 mm lateral shift of the caudal fragment relative to the cranial fragment, facilitating reliable pelvic enlargement. However, as the size of the ilium, location of the initial fracture and severity of malunion will vary in individual cases, preparing specific crank plates for each case might be necessary. Currently, crank plates are custom-made to order and may not be immediately available to the surgeon. Therefore, it may require some time to obtain them. Care should be taken when using an alternative plate in place of the crank plate, as excessive bending may reduce rigidity.
A major postoperative complication, subcutaneous tissue necrosis of the ventral surgical wound, was observed in case 4. However, this was effectively managed with surgical debridement. Roh et al 18 reported urinary dysfunction as a potential complication after symphyseal distraction osteotomy using PMMA for PCS. This was attributed to tension in the ischiocavernosus muscle (originating from the caudal surface of the ischial tuberosity and inserting into the bulbospongiosus muscle) 20 and excessive pelvic enlargement. In our study, no case of postoperative urinary dysfunction or peripheral neuropathy was noted. This may be because our technique involves unilateral osteotomy of the ilium with lateral translation of the caudal fragment while simultaneously separating the pubic symphysis. As a limitation of the study, the number of cases was small and the follow-up period was short. Further studies with a larger number of cases and longer follow-up assessments are warranted.
Conclusions
This study describes a pelvic enlargement technique in cats for PCS. This approach combined osteotomies of the ilium and midline pelvic floor and used crank (or reconstruction) plates to stabilise the ilial osteotomy and screws and PMMA to stabilise the pelvic floor osteotomy.
Supplemental Material
Pre- and postoperative radiographs of cases 1, 2 and 4–6.
Acknowledgments
The authors thank everyone involved in this study. They also thank Editage for English language editing.
Footnotes
Accepted: 10 July 2024
HF is employed by Platon Japan, Tokyo, Japan, the manufacturer of crank plates and screws used in this study. The authors declared that there were no other conflicts of interest.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: The work described in this manuscript involved the use of non-experimental (owned or unowned) animals. Established internationally recognised high standards (‘best practice’) of veterinary clinical care for the individual patient were always followed and/or this work involved the use of cadavers. Ethical approval from a committee was therefore not specifically required for publication in JFMS. Although not required, where ethical approval was still obtained, it is stated in the manuscript.
Informed consent: Informed consent (verbal or written) was obtained from the owner or legal custodian of all animal(s) described in this work (experimental or non-experimental animals, including cadavers, tissues and samples) for all procedure(s) undertaken (prospective or retrospective studies). For any animals or people individually identifiable within this publication, informed consent (verbal or written) for their use in the publication was obtained from the people involved.
ORCID iD: Ryoichi Suzuki  https://orcid.org/0009-0000-3990-1111
https://orcid.org/0009-0000-3990-1111
Supplementary material: The following file is available as supplementary material:
Pre- and postoperative radiographs of cases 1, 2 and 4–6.
References
- 1. Grierson J. Dealing with pelvic fractures in cats. In Practice 2019; 41: 106–114. [Google Scholar]
- 2. Bookbinder PF, Flanders JA. Characteristics of pelvic fracture in the cat. Vet Comp Orthop Traumatol 1992; 5: 122–127. [Google Scholar]
- 3. Hamilton MH, Evans DA, Langley-Hobbs SJ. Feline iliac fractures: assessment of screw loosening and pelvic canal narrowing after lateral plating. Vet Surg 2009; 38: 326–333. [DOI] [PubMed] [Google Scholar]
- 4. Colopy-Poulsen SA, Danova NA, Hardie RJ, et al. Managing feline obstipation secondary to pelvic fracture. Comp Contin Educ Pract Vet 2005; 27: 662–669. [Google Scholar]
- 5. White RN. Surgical management of constipation. J Feline Med Surg 2002; 4: 129–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Trevail T, Gunn-Moore D, Carrera I, et al. Radiographic diameter of the colon in normal and constipated cats and cats with megacolon. Vet Radiol Ultrasound 2011; 52: 516–520. [DOI] [PubMed] [Google Scholar]
- 7. Matthiesen DT, Scavelli TD, Whitney WO. Subtotal colectomy for the treatment of obstipation secondary to pelvic fracture malunion in cats. Vet Surg 1991; 20: 113–117. [DOI] [PubMed] [Google Scholar]
- 8. Schrader SC. Pelvic osteotomy as a treatment for obstipation in cats with acquired stenosis of the pelvic canal: six cases (1978–1989). J Am Vet Med Assoc 1992; 200: 208–213. [PubMed] [Google Scholar]
- 9. DeGroot W, Gibson TW, Reynolds D, et al. Internal hemipelvectomy for treatment of obstipation secondary to pelvic malunion in 3 cats. Can Vet J 2016; 57: 955–960. [PMC free article] [PubMed] [Google Scholar]
- 10. Ferguson JF. Triple pelvic osteotomy for the treatment of pelvic canal stenosis in a cat. J Small Anim Pract 1996; 37: 495–498. [DOI] [PubMed] [Google Scholar]
- 11. Prassinos NN, Adamama-Moraitou KK, Gouletsou PG, et al. Symphyseal distraction-osteotomy using a novel spacer of spirally fashioned orthopaedic wire for the management of obstipation. J Feline Med Surg 2007; 9: 23–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Averill SM, Johnson AL, Schaeffer DJ. Risk factors associated with development of pelvic canal stenosis secondary to sacroiliac separation: 84 cases (1985–1995). J Am Vet Med Assoc 1997; 211: 75–78. [PubMed] [Google Scholar]
- 13. Cinti F, Cavaliere L, Degna MT, et al. Triple pelvic osteotomy fixed with lag screw for the treatment of pelvic canal stenosis in five cats. Vet Comp Orthop Traumatol 2020; 33: 363–369. [DOI] [PubMed] [Google Scholar]
- 14. Whittem TL, Johnson AL, Smith CW, et al. Effect of perioperative prophylactic antimicrobial treatment in dogs undergoing elective orthopedic surgery. J Am Vet Med Assoc 1999; 215: 212–216. [PubMed] [Google Scholar]
- 15. Johnson KA. The pelvis and hip joint. In: Piermattei’s atlas of surgical approaches to the bones and joints of the dog and cat. 5th ed. St Louis, MO: Elsevier Saunders, 2014, pp 317–320. [Google Scholar]
- 16. Pinna S, Tassani C, Rossini M, et al. External fixator for the treatment of narrowed pelvic canal in a cat. Vet Med-Czech 2021; 66: 356–362. [Google Scholar]
- 17. Atallah FA, Silva RS, Oliveira ALDA, et al. Subcolectomy and symphyseal distraction-osteotomy using a spacer of spirally fashioned orthopedic wire: a treatment option for cats with pelvic canal stenosis, megacolon and obstipation. Ciência Rural 2016; 46: 1472–1478. [Google Scholar]
- 18. Roh YH, Kim JN, Byun PM, et al. Ischiocavernosus muscle release for urethral obstruction treatment after pelvic symphyseal distraction osteotomy in a cat with pelvic stenosis. Vet Sci 2021; 8. DOI: 10.3390/vetsci8100225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lewis G. Properties of acrylic bone cement: state of the art review. J Biomed Mater Res 1997; 38: 155–182. [DOI] [PubMed] [Google Scholar]
- 20. Martin WD, Fletcher TF, Bradley WE. Perineal musculature in the cat. Anat Rec 1974; 180: 3–14. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Pre- and postoperative radiographs of cases 1, 2 and 4–6.