Abstract
Study Design
Retrospective, matched case-control study.
Objective
To investigate the risk factors of reoperation after percutaneous endoscopic lumbar discectomy (PELD) due to recurrent lumbar disc herniation (rLDH) and to establish a set of individualized prediction models.
Methods
Patients who underwent PELD successfully from January 2016 to February 2022 in a single institution were enrolled in this study. Six methods of machine learning (ML) were used to establish an individualized prediction model for reoperation in rLDH patients after PELD, and these models were compared with logistics regression model to select optimal model.
Results
A total of 2603 patients were enrolled in this study. 57 patients had repeated operation due to rLDH and 114 patients were selected from the remaining 2546 nonrecurrent patients as matched controls. Multivariate logistic regression analysis showed that disc herniation type (P < .001), Modic changes (type II) (P = .003), sagittal range of motion (sROM) (P = .022), facet orientation (FO) (P = .028) and fat infiltration (FI) (P = .001) were independent risk factors for reoperation in rLDH patients after PELD. The XGBoost AUC was of 90.71%, accuracy was approximately 88.87%, sensitivity was 70.81%, specificity was 97.19%. The traditional logistic regression AUC was 77.4%, accuracy was about 77.73%, sensitivity was 47.15%, specificity was 92.12%.
Conclusion
This study showed that disc herniation type (extrusion, sequestration), Modic changes (type II), a large sROM, a large FO and high FI were independent risk factors for reoperation in LDH patients after PELD. The prediction efficiency of XGBoost model was higher than traditional Logistic regression analysis model.
Keywords: recurrent lumbar disc herniation, percutaneous endoscopic lumbar discectomy, risk factors, machine learning, prediction model
Introduction
One of the most common lumbar diseases is lumbar disc herniation (LDH). The prevalence of LDH has risen steadily in recent years. 1 Percutaneous endoscopic lumbar discectomy (PELD) is a popular minimally invasive technology that has several advantages, such as less intraoperative bleeding, less muscle damage, quick recovery, short hospital stay, and others. 2 However, the risk of recurrent lumbar disc herniation (rLDH) after surgery is reported in 5% to 21% of patients.3,4 The second operation has many hazards, so it is necessary to analyze the risk factors of rLDH to prevent rLDH.
Several risk factors associated with rLDH after PELD have been reported in previous studies,1,5-7 such as age, gender, body mass index (BMI), alcohol, smoking, diabetes, hypertension, degree of disc degeneration, Modic changes, location of disc herniation, type of disc herniation, disc height index (DHI), sagittal range of motion (sROM), facet orientation (FO)and section tendency (FT). However, The findings of various studies are inconclusive, making it impossible to draw reliable conclusions about these risk factors. Previous research have found that disc degeneration diseases is closely related to waist muscle function, 8 but few studies have been proceeded whether paravertebral cross-sectional area (CSA) and muscle FI are risk factors for rLDH.
In recent years, artificial intelligence (AI) has gradually applied to various fields of medicine, and machine learning (ML), as a branch of AI, can automatically predict the output based on the characteristics of input data through algorithms. Compared with traditional statistical methods, ML can process big data more accurately, so as to significantly improve the diagnostic accuracy and prognosis prediction. It has been applied in the medical field like medical management, clinically assisted decision-making, patient monitoring and medical intervention.9,10 Currently, single-factor or multi-factor logistics regression is generally used to establish risk prediction models for rLDH studies.1-3 Classical models in ML are rarely used to build predictive models.
In this study, we established a retrospective, matched case-control study to investigate the risk factors of reoperation after PELD because of rLDH and establish a Multi-factor logistics regression prediction model. Then, six methods including decision tree and XGBoost et al in ML were used to establish an individualized prediction model and compared with the multi-factor logistics regression model to select the optimal model. In order to provide clinical doctors with surgical decision-making when they treat LDH patients.
Materials and Methods
Patients Population
The study was performed in compliance with ethical standards and was approved by the institutional review board of our hospital. In our study, Patients who underwent PELD successfully because of a single-level L4-L5 or L5-S1 disc herniation in Zhongda Hospital Southeast University from January 2016 to February 2022 were enrolled in this retrospective study, and because of the low incidence of rLDH, a matched case-control design was used. This study was approved by the Institutional Ethics Committee of Zhongda Hospital Southeast University (reference number:2022ZDSYLL406-P01). As we wanted to include multiple variables in our risk factor analysis, so we just performed 1:2 matching according to surgical level (L4-L5 or L5-S1) and primary diagnosis. 11 Case group (n = 57) was defined as patients undergoing operation again after PELD, while control group (n = 114) was randomly selected from patients with no recurrence according to corresponding clinical characteristics. We excluded those patients with LDH at other levels and those who underwent primary surgery at L4-L5 or L5-S1 level in other hospitals. The reoperation of rLDH is defined as the symptoms of LDH patients were significantly improved after operation. The patients had LDH symptoms again at any time after operation and underwent surgery for the same segment again. We excluded patients with missing follow-up, failed operations and incomplete information. For any patient with new symptoms of sciatica, magnetic resonance imaging (MRI) was performed and assessed for the presence of rLDH by a doctor with a title above the attending doctor.
Data Collection and Assessment
The clinical data of the patients were collected from the HIS system and imaging system of the hospital, and the relevant clinical data and imaging examination results of the two groups after admission were recorded. Data of age, gender, BMI, drinking, smoking, diabetes, hypertension, degree of disc degeneration, Modic change, location of disc herniation, type of disc herniation, DHI, sROM, FO, FT, CSA and the degree of muscle fat infiltration (FI) were compared.
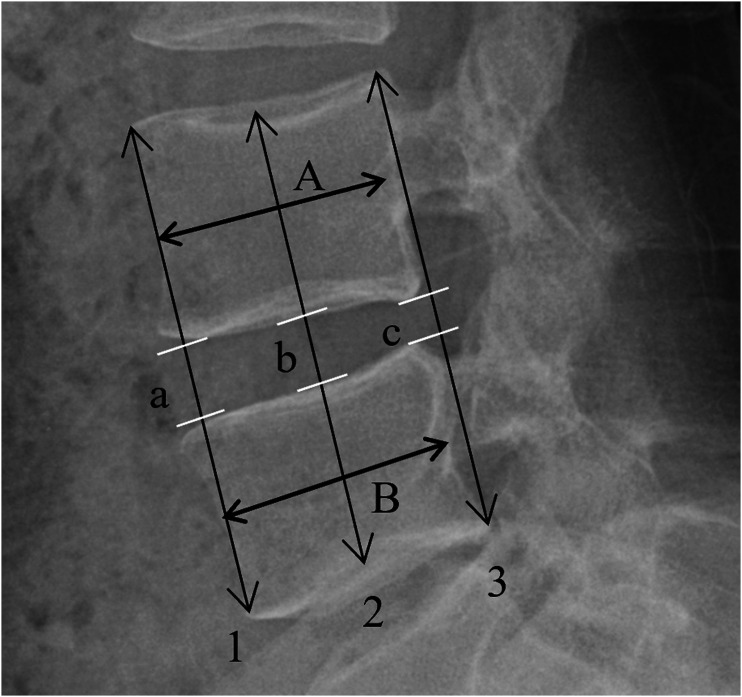
All imaging data were measured at the surgical level. The herniation types were classified as protrusion, extrusion, and sequestration. 6 According to Pfirrmann 12 standard, the disc degeneration grade was assessed on T2-weighted sagittal sequences. We took L4-L5 disc as the adjacent disc of L5-S1 level and the one with more severe degeneration grade among L3-L4 and L5-S1 discs as the adjacent disc of L4-L5 level in this study. Modic changes are divided into 3 types:Type I (low T1 and high T2), Type II (high T1 and high T2), Type III (low T1 and T2). 6 DHI was measured according to the method used by Youn 13 (Figure 1). sROM, FO and FT were measured according to the method used by Shi. 6 Measurement of sROM of L4-L5 or L5-S1. The sROM of L4-L5 or L5-S1 can be calculated by the difference between flexion a and extension b angles, which was measured in relation to the lines of the superior and inferior endplate of L4-L5 or L5-S1. Measurement of FO and FT. One line was drawn in the midsagittal plane of the vertebra, and the other two lines were drawn tangential to the superior articular process of each facet joint. The facet joint angles relative to the sagittal plane were a and β. FO = (a+β)/2; FT = |a-β|.
Figure 1.
Youn, M.S methods of measuring DHI: A, B: sagittal diameter from the midvertebral level of the consecutive vertebra; 1: the line between the anterior/superior corner of the upper vertebra and anterior/inferior corner of the lower vertebra; 2: the line between the middle/superior point of the upper vertebra and middle/inferior point of the lower vertebra; 3: the line between the posterior/superior corner of the upper vertebra and posterior/inferior corner of the lower vertebra; a, b, c measured disc height on lines 1, 2, and 3. DHI = [(a + b + c)/3]/[(A + B)/2].
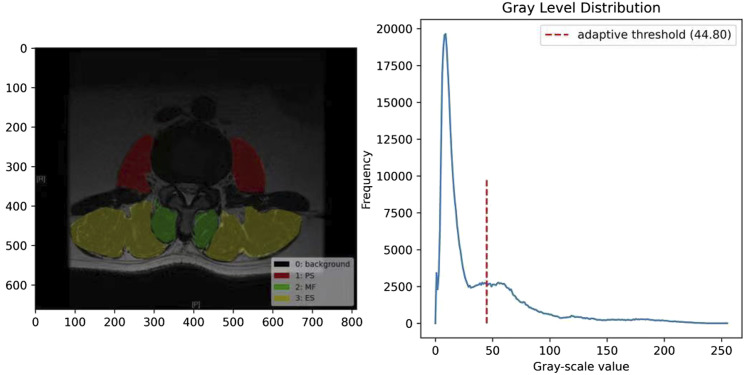
In this study, we selected L4-L5 disc level from MRI images to measure the paravertebral muscles because previous studies have demonstrated that the muscle of this level is 6-9 times more likely to be affected than any other levels. 14 The CSA of the paravertebral muscles of L4-L5 was measured using the grey-scale discrimination method proposed by Ding et al, 15 and the CSA was obtained by dividing the region of interest (ROI) according to the boundary of each paravertebral muscle in the cross-section. We used Labelme (MIT,5.1.1) Threshold method to measure the number of fat pixels in each paravertebral muscle ROI as a percentage of the total number of pixels. OTSU algorithm 16 is used to realize the adaptive threshold for global image division 15 (Figure 2).
Figure 2.
Measurement method of the CSA and FI. The Labelme (MIT,5.1.1) Threshold method on the middle layer of magnetic resonance image in L4-L5 level. The OTSU algorithm was used to achieve an adaptive threshold for global image segmentation to distinguish between muscle tissue and fat tissue.
Statistical Analysis
All data were analysed using SPSS Statistics software (ver-sion 22.0, SPSS Inc, Chicago, IL, USA). Univariate analysis was performed using Students t test and Chi-squared test for clinical and radiological parameters. Multiple logistic regression analysis was performed to confirm independent risk factors for rLDH. Any variable with a P value not more than .2 6 on univariate analysis was included in the multiple logistic regression models. A P < .05 was considered as statistically significant.
Machine Learning Method
In addition to statistical analysis with logistic regression model, tree-based models and some other commonly used machine learning classifiers such as Stochastic Gradient Descent, Supported Vector Classifier (with linear kernel), Decision Tree, Random Forest, Gradient Boosting and XGBoost are constructed to predict whether rLDH in PELD patients will undergo operation again. In this study, the recursive feature elimination method is applied to select the features when training the models. For every possible combination of the selected features, the performance of each model on the test dataset are recorded, and the features are selected to maximize the AUC value. After feature selection, grid search method is applied to tune the model parameters, and we reconstruct the feature selection processing with the updated parameters for each model. We iterate over and over until the result of feature selection does not change, at which time the parameters and feature combination are considered as the optimal configuration for the current model.
Cross Validation
In order to avoid the effect of the randomness of data partitioning on model evaluation, this study used the k-fold cross-validation (K = 5) method to randomly divide the data of 171 samples into five groups. When evaluating each model, 4 groups of data are used as training group, and the remaining data is test group. The average of the five test results was used as the final evaluation result.
Model Evaluation Indicators
In this study, the reoperation prediction task is a binary classification task, so the area under the ROC curve (AUC) is used as the first evaluation index. In addition, this study also used the prediction accuracy, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) to evaluate the performance of the model. Probabilistic calibration curves were also used to evaluate the model performance.
Result
Baseline Patient Data
A total of 2603 patients who underwent PELD at L4-L5 or L5-S1 level were enrolled in this study, including 1468 patients with L4-L5 disc herniation and 1135 patients with L5-S1 disc herniation. After follow-up, 57 patients who underwent operation again were diagnosed with rLDH by the recurrent symptom of sciatica and corresponding imaging examination, including 34 patients with L4-L5 disc herniation and 23 patients with L5-S1 disc herniation. 114 patients were selected from the remaining 2546 nonrecurrent patients as matched controls (1:2) according to corresponding clinical characteristics of reoperation cases. The reoperation incidence of rLDH was 2.2% (57/2603). There was no significant difference in surgical level between cases and controls. All characteristics are shown in Table 1.
Table 1.
Comparison of all Characteristics Between Control and Case Groups.
| Variable | Controls (N = 114) | Cases (N = 57) | Total (N = 171) | P |
|---|---|---|---|---|
| Gender, n | 0.606 | |||
| Male | 74 (64.91%) | 40 (70.18%) | 114 (66.67%) | |
| Female | 40 (35.09%) | 17 (29.82%) | 57 (33.33%) | |
| Age (years) | 44.09 ± 13.63 | 48.70 ± 16.32 | 45.63 ± 14.70 | 0.053 |
| BMI (kg/m2) | 23.98 [22.50;27.00] | 25.00 [23.00;26.00] | 24.20 [22.50;27.00] | 0.377 |
| Hypertension, n | 0.762 | |||
| No | 84 (73.68%) | 40 (70.18%) | 124 (72.51%) | |
| Yes | 30 (26.32%) | 17 (29.82%) | 47 (27.49%) | |
| Smoking, n | 0.34 | |||
| No | 105 (92.11%) | 55 (96.49%) | 160 (93.57%) | |
| Yes | 9 (7.89%) | 2 (3.51%) | 11 (6.43%) | |
| Diabetes, n | 0.32 | |||
| No | 100 (87.72%) | 46 (80.70%) | 146 (85.38%) | |
| Yes | 14 (12.28%) | 11 (19.30%) | 25 (14.62%) | |
| Herniated disc type, n (%) | 0 | |||
| Protrusion | 42 (36.84%) | 1 (1.75%) | 43 (25.15%) | |
| Extrusion | 62 (54.39%) | 33 (57.89%) | 95 (55.56%) | |
| Sequestration | 10 (8.77%) | 23 (40.35%) | 33 (19.30%) | |
| Surgical level disc degeneration, n (%) | 0.163 | |||
| II | 8 (7.02%) | 4 (7.02%) | 12 (7.02%) | |
| III | 21 (18.42%) | 15 (26.32%) | 36 (21.05%) | |
| IV | 71 (62.28%) | 26 (45.61%) | 97 (56.73%) | |
| V | 14 (12.28%) | 12 (21.05%) | 26 (15.20%) | |
| Adjacent level disc degeneration, n (%) | 0.026 | |||
| I | 1 (0.88%) | 1 (1.75%) | 2 (1.17%) | |
| II | 25 (21.93%) | 5 (8.77%) | 30 (17.54%) | |
| III | 39 (34.21%) | 22 (38.60%) | 61 (35.67%) | |
| IV | 46 (40.35%) | 22 (38.60%) | 68 (39.77%) | |
| V | 3 (2.63%) | 7 (12.28%) | 10 (5.85%) | |
| Modic changes, n (%) | 0 | |||
| No | 105 (92.11%) | 42 (75.00%) | 147 (86.47%) | |
| Type I | 5 (4.39%) | 1 (1.79%) | 6 (3.53%) | |
| Type II | 3 (2.63%) | 12 (21.43%) | 15 (8.82%) | |
| Type III | 1 (0.88%) | 1 (1.79%) | 2 (1.18%) | |
| DHI | 0.32 [0.28;0.36] | 0.31 [0.27;0.34] | 0.32 [0.28;0.36] | 0.249 |
| sROM, (deg) | 8.18 ± 2.97 | 9.46 ± 3.60 | 8.61 ± 3.24 | 0.015 |
| FO, (deg) | 44.75 [38.50;48.50] | 49.00 [45.50;53.00] | 47.00 [39.50;50.00] | 0 |
| FT, (deg) | 4.00 [2.00;6.50] | 4.00 [2.00;6.00] | 4.00 [2.00;6.50] | 0.73 |
| CSA (pixel) | 70025.00 [56606.00;85885.00] | 70434.00 [56220.00;81577.00] | 70221.00 [56399.50;85619.00] | 0.939 |
| FI | 0.08 [0.04;0.11] | 0.09 [0.06;0.15] | 0.08 [0.05;0.13] | 0.016 |
BMI, body-mass index; DHI, disc height index; sROM, sagittal range of motion; FO, facet orientation; FT, facet tropism; CSA, cross-sectional area; FI, fat infiltration.
Univariate analysis showed that disc herniation type (P < .001), Modic changes Type II (P < .001), sROM(P = .017), FO (P = .001) and FI (P = .01) were significantly associated with rLDH reoperation (Table 2). Factors with P < .2 were included in the multivariate logistic regression analysis. Multivariate logistic regression analysis showed that the disc herniation type (extrusion, sequestration) (P < .001), Modic changes (type II) (P = .003), sROM(P = .022), FO (P = .028) and FI (P = .001) were independent risk factors for rLDH reoperation after PELD (Table 3). Among the 57 patients with rLDH reoperation, 31 patients underwent PELD again and 26 patients underwent lumbar fusion again.
Table 2.
Univariate Analysis of Risk Factors for Reoperation in rLDH Patients after PELD.
| Variable | B | SE | z | p | OR [95%CI] |
|---|---|---|---|---|---|
| Gender | -.24 | .350 | -.688 | .492 | .79 [.4.1.56] |
| Age | .022 | .011 | 1.922 | .055 | 1.02 [1.1.04] |
| BMI | .031 | .051 | .609 | .542 | 1.03 [.93.1.14] |
| Hypertension | .174 | .359 | .484 | .628 | 1.19 [.59.2.41] |
| Smoking | -.857 | .799 | -1.073 | .283 | .42 [.09.2.03] |
| Diabetes | .535 | .441 | 1.215 | .224 | 1.71 [.72.4.05] |
| Herniated disc type | |||||
| Protrusion | |||||
| Extrusion | 3.107 | 1.035 | 3.003 | .003 | 22.35 [2.94,169.8] |
| Sequestration | 4.571 | 1.080 | 4.230 | <.001 | 96.6 [11.62,802.81] |
| Surgical level disc degeneration | |||||
| II | |||||
| III | .357 | .699 | .510 | .610 | 1.43 [.36.5.63] |
| IV | -.311 | .654 | -.476 | .634 | .73 [.2.2.64] |
| V | .539 | .728 | .741 | .459 | 1.71 [.41.7.14] |
| Adjacent level disc degeneration | |||||
| I | |||||
| II | -1.609 | 1.497 | -1.075 | .282 | .2 [.01.3.76] |
| III | -.573 | 1.439 | -.398 | .691 | .56 [.03.9.47] |
| IV | -.738 | 1.438 | -.513 | .608 | .48 [.03.8.01] |
| V | .847 | 1.574 | .538 | .590 | 2.33 [.11.50.98] |
| Modic changes | |||||
| No | |||||
| Type I | -.693 | 1.111 | -.624 | .533 | .5 [.06.4.41] |
| Type II | 2.303 | .671 | 3.432 | <.001 | 10 [2.69.37.24] |
| Type III | .916 | 1.426 | .643 | .520 | 2.5 [.15.40.9] |
| DHI | -2.896 | 2.233 | -1.297 | .195 | .06 [0.4.39] |
| sROM | .125 | .052 | 2.378 | .017 | 1.13 [1.02.1.26] |
| FO | .081 | .025 | 3.297 | .001 | 1.08 [1.03.1.14] |
| FT | .022 | .044 | .490 | .624 | 1.02 [.94.1.11] |
| CSA | 0 | .000 | .269 | .788 | 11,1 |
| FI | 5.698 | 2.205 | 2.584 | .010 | 298.2 [3.96,22477.49] |
rLDH, recurrent lumbar disc herniation; PELD, percutaneous endoscopic lumbar discectomy; BMI, body-mass index; DHI, disc height index; sROM, sagittal range of motion; FO, facet orientation; FT, facet tropism; CSA, cross-sectional area; FI, fat infiltration.
Table 3.
Multivariate Logistic Regression Analysis of Risk Factors for Reoperation in rLDH Patients after PELD.
| Variable | B | SE | z | p | OR [95%CI] |
|---|---|---|---|---|---|
| -9.317 | 2.209 | -4.217 | <.001 | ||
| Gender | .003 | .015 | .216 | .829 | 1 [.97.1.03] |
| Herniated disc type | |||||
| Protrusion | |||||
| Extrusion | 3.538 | 1.121 | 3.155 | .002 | 34.4 [3.82,309.83] |
| Sequestration | 5.196 | 1.217 | 4.270 | <.001 | 180.56 [16.63,1960.32] |
| Modic changes | |||||
| No | |||||
| Type I | -.767 | 1.576 | -.487 | .626 | .46 [.02.10.18] |
| Type II | 3.02 | 1.005 | 3.006 | .003 | 20.5 [2.86,146.86] |
| Type III | 1.636 | 1.728 | .947 | .344 | 5.14 [.17,151.97] |
| DHI | -3.88 | 3.293 | -1.178 | .239 | .02 [0.13.11] |
| sROM | .184 | .081 | 2.282 | .022 | 1.2 [1.03.1.41] |
| FO | .068 | .031 | 2.192 | .028 | 1.07 [1.01.1.14] |
| FI | 10.986 | 3.340 | 3.289 | .001 | 59035.03 [84.74,41127545.1] |
rLDH, recurrent lumbar disc herniation; PELD, percutaneous endoscopic lumbar discectomy; sROM, sagittal range of motion; FO, facet orientation; FI, fat infiltration.
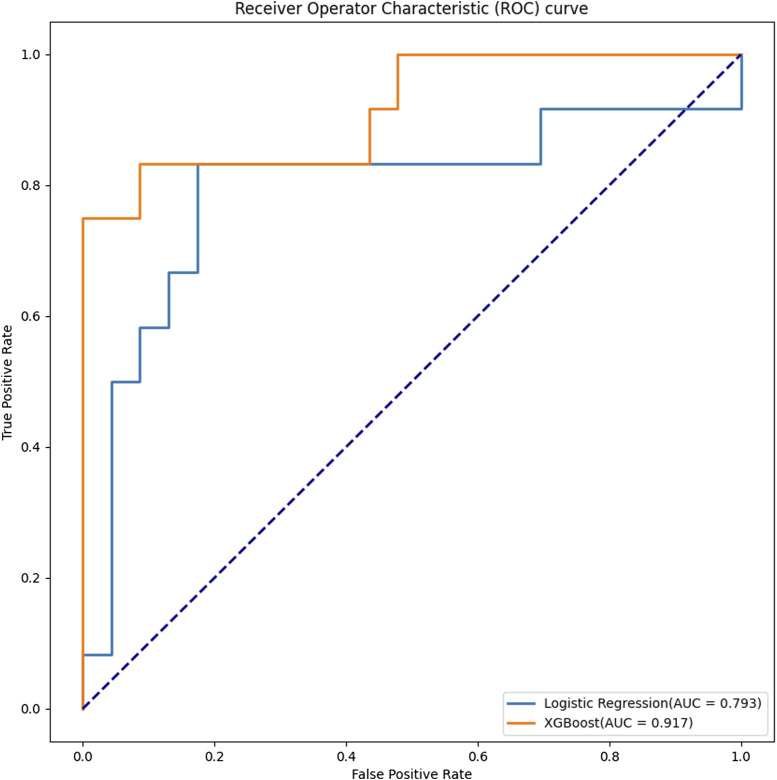
Model Evaluation
The mean AUC scores through 5-fold cross-validation was used as the final evaluation index. We used stochastic gradient descent, linear support vector machines, decision trees, random forests, gradient boosting, XGBoost and traditional logistic regression classifiers to predict whether to reoperate for rLDH in patients after PELD. The XGBoost model achieved better results in this task compared to other models in terms of index such as AUC. The performance of these models, including AUC, accuracy and the 4 main confusion matrix metrics (sensitivity, specificity, PPV, NPV) is shown in Table 4.
Table 4.
5-Fold Cross Validation Yielded the Average Scores of the Individual Models.
| Classifier | n_Features | AUC | Accuracy | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|---|---|
| Logistic Regression | 9 | 0.77 ( 0.10) | 0.78 ( 0.08) | 0.47 ( 0.20) | 0.92 ( 0.05) | 0.76 ( 0.16) | 0.79 ( 0.08) |
| SGD | 16 | 0.76 ( 0.05) | 0.78 ( 0.04) | 0.59 ( 0.18) | 0.81 ( 0.06) | 0.57 ( 0.15) | 0.81 ( 0.07) |
| Linear Supported Vector | 5 | 0.80 ( 0.09) | 0.77 ( 0.07) | 0.41 ( 0.12) | 0.95 ( 0.04) | 0.82 ( 0.15) | 0.77 ( 0.07) |
| Decision Tree | 4 | 0.74 ( 0.07) | 0.74 ( 0.09) | 0.65 ( 0.10) | 0.79 ( 0.09) | 0.61 ( 0.15) | 0.82 ( 0.06) |
| Random Forest | 16 | 0.86 ( 0.09) | 0.82 ( 0.07) | 0.55 ( 0.10) | 0.97 ( 0.03) | 0.88 ( 0.10) | 0.82 ( 0.05) |
| Gradient Boosting | 9 | 0.86 ( 0.05) | 0.85 ( 0.04) | 0.64 ( 0.13) | 0.95 ( 0.02) | 0.85 ( 0.06) | 0.85 ( 0.03) |
| XGBoost | 12 | 0.91 ( 0.06) | 0.89 ( 0.05) | 0.71 ( 0.07) | 0.97 ( 0.04) | 0.94 ( 0.08) | 0.87 ( 0.04) |
rLDH, recurrent lumbar disc herniation; PELD, percutaneous endoscopic lumbar discectomy; sROM, sagittal range of motion; FO, facet orientation; FI, fat infiltration.
Table 4 showed that the best model for predicting the need for repeat operation in patients with rLDH after PELD is XGBoost, with an AUC of 90.71%, accuracy of approximately 88.87%, sensitivity of 70.81%, specificity of 97.19%, PPV of 94% and NPV of 87.42%. The traditional logistic regression AUC was 77.4%, accuracy was about 77.73%, sensitivity was 47.15%, specificity was 92.12%, PPV was 75.67% and NPV was 73.12%. Overall, the indexes of XGBoost demonstrate its good discriminatory performance, especially when compared to other evaluation ML algorithms as well as traditional logistic regression.
Figure 3 showed the ROCs for the respective results of the logistic regression and XGboost models applied to the test set, with the numbers next to the ordered pairs indicating the probability threshold for achieving the best discriminative performance. These results showed that the optimal model selected from Table 4 exhibits good discriminatory performance when applied to the resistance test set.
Figure 3.
ROC curves from traditional logistic regression and XGBoost on the test group, with whether patients had repeat operation as an outcome measure. The coordinates indicated the best specificity and sensitivity, while the number next to the coordinate indicated the probability threshold for achieving the best performance (as judged by the Jorden index).
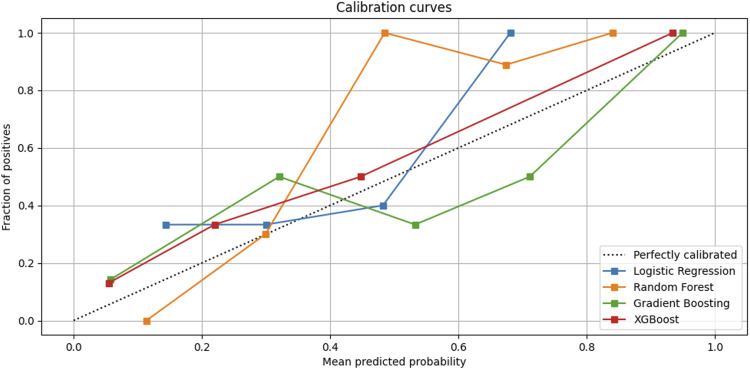
Probabilistic calibration curves are used to judge model performance and A better model would be around the standard line (Figure 4). The random forest model in Figure 4 exhibits a Sigmoid-like shape and is a lack of confidence. However, the calibration curve of overconfident model should be an inverse Sigmoid shape, such as the Gradient Boosting model in the figure. We found that the logistic regression classifier gives even worse results, while the best performer is the XGBoost model, which has a calibration curve very close to a straight line with a slope of 1 past the origin. Overall, this figure showed that our algorithm achieves a good calibration with respect to the underlying data.
Figure 4.
The horizontal coordinate is the predicted probability and below the black standard line indicates that the predicted value is greater than the actual (or observed) value, ie the risk is overestimated. Therefore, a better model would be around the standard line.
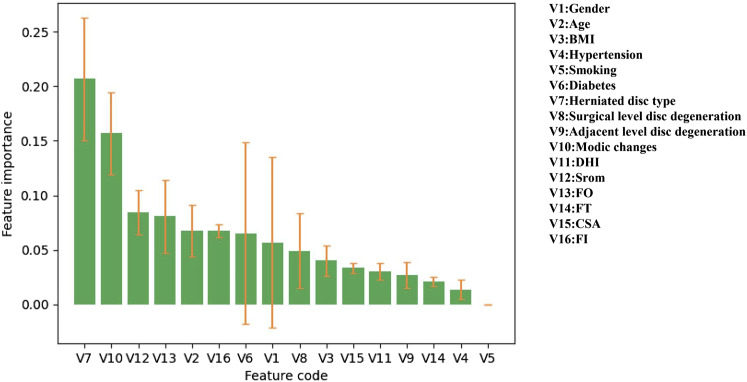
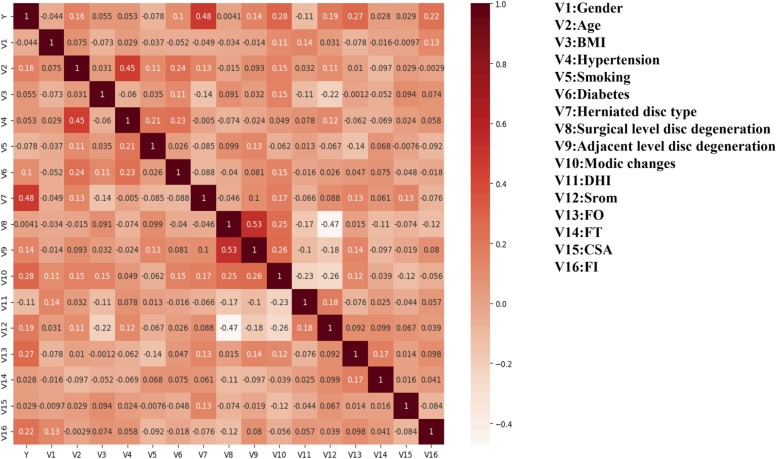
Feature Importance
We used the XGBoost model and the Mean Decrease Impurity method to record the mean importance assessment of all features in each of the 5-fold cross-validation experiments and calculated the standard deviation to determine the most important predictors for the final ML models (Figure 5). The correlation matrix and heat map was shown in Figure 6. The XGBoost model discarded variable Hypertension, Smoking, Diabetes and FT, which echoed the feature importance results, and we found that variable Diabetes fluctuated greatly in experiments, so it is not a good feature. While variable Hypertension, Smoking and FT did not contribute more to the model predictions. Finally, we found that the top 6 risk factors on relative importance were: disc herniation type, Modic change, sROM, FO, age and FI (the top 6 influences were chosen because relative importance of age and FI were essentially close)
Figure 5.
Relative importance of the risk factors of predicting the need for repeat operation in patients with rLDH after PELD in the XGBoost model.
Figure 6.
Correlations between risk factors of reoperation in rLDH patients after PELD were shown in the correlation matrix and heat map.
Discussion
The rLDH after PELD is one of serious postoperative complications, and rLDH occurs in 5% to 21% of patients,3,4 A large-sample study in Korean showed that 12.4% of patients treated with endoscopic discectomy underwent operation again. 17 Nevertheless, there has been no unified standard for the definition of rLDH after PELD. rLDH can be considered to occur if the patient has similar symptoms as before or imaging shows the protrusion of the same level again after a certain period of time after operation in most researchers’ opinion. 18 However, in previous studies, many researchers think that only recurrence in the same location or the same level can be considered as rLDH.19,20 There is no exact definition of rLDH in terms of how long between surgical time and the recurrence time. For example, Kyoung-Tae et al 21 suggested that a patient who has re-herniation symptoms can be defined as rLDH only after a painless period of at least 6 months after discectomy, while Yao et al 2 thought that only a one-month pain-free period was needed. It is one-side for some doctors to diagnose some patients who have herniation symptoms again after PELD as rLDH just according to clinical feature. Therefore, the definition of rLDH remains to be discussed However, patients who underwent surgery again after PELD in the same level can be determined to have recurrence. 22 Therefore, this study only targeted patients who underwent surgery again after PELD in the same level and their symptoms were relieved.
In this study, we were surprised to find that the XGBoost model showed good discriminatory performance in all indicators compared to the traditional logistic regression model, with a prediction accuracy of 88.87% and an AUC of 90.71%, while the logistic regression accuracy was only 77.73% and an AUC of 77.4%. The multifactorial logistic regression model found that disc herniation type, Modic change (Type II), sROM, FO, FI were independent risk factors for rLDH reoperation after PELD. The XGBoost model with better predictive accuracy also included these five factors in the top 6 of relative importance.
We classified the herniation types into protrusion, extrusion, and sequestration and found that the proportion of extrusion and sequestration was significantly higher in the reoperation group than in the non-reoperation group. The type of extrusion and sequestration are severe types of disc herniation and will have more extensive subjects with larger anular defects. Extrusion and sequestration disc herniation are more likely to have incomplete disc removal during surgery that may lead to reoperation. There is also a possibility that the operation accelerates the severe loss of disc height and leads to intervertebral instability in these two types of disc herniation, thereby increasing the risk of open surgery.21,23
Modic changes as a potential factor of rLDH has rarely been reported. A 2 year retrospective study by Kim et al 20 had found an association between Modic changes and recurrence after PELD, consistent with the results of our study. Modic changes has been proved to have a strong relationship with low back pain and disc degeneration and specific types of endplate defects associated with low back pain.24,25 Therefore, Modic changes lead to an altered disc stress which leads to an increased probability of recurrence. This study also found that rLDH was closely associated with Modic type II, which is histologically manifested by marrow fat degeneration or marrow ischaemic necrosis. Whether the degeneration of endplate fat degeneration or ischaemic necrosis also predicts the possibility of disc degeneration needs further investigation.
Only a few researchers have listed sROM and FO as rLDH imaging factors. Kim et al 21 found that large sROM is a risk factor for rLDH in 2009, which was corroborated by Shi et al 6 and is consistent with the results of this study. Li et al 4 had reported that FO and FT as risk factors for rLDH after open discectomy. Wang et al26,27 reported that a close relationship between FO\FT and lumbar disc herniation in adolescents, and Schleich et al 28 also reported that deformities of the lumbar facet joints and lumbar disc herniation were closely related. The asymmetry of the facet joints accelerated the degeneration of the facet joints and discs, making them more likely to cause lumbar disc herniation. In our study, a significant correlation was found between FO and the occurrence of rLDH.
Previous studies have found that both low back pain and degenerative diseases of the lumbar spine are closely related to waist muscle function, 8 but few studies have included muscle factors as risk factors in rLDH. CSA and FI are commonly used to measure lumbar muscle function. 29 In this study, FI was found to be an independent risk factor for reoperation in rLDH. Stevens et al 29 found that patients with unilateral LDH had ipsilateral multifidus muscle changes after a systematic review and meta-analysis of the literature related to lumbar disc herniation and unilateral multifidus muscle changes. This study innovatively listed CSA and muscle FI as possible risk factors for rLDH reoperation after PELD in LDH patients. It was found that there was no statistically significant difference in CSA between cases and controls, but in terms of FI, the mean muscle fat infiltration rate in the case group was 9%, which was statistically significantly different from that of the control group. Because increased muscle FI leads to decreased muscle function, paravertebral muscle hypofunction would change the original biomechanical relationship, resulting in increased or uneven disc stress, which in turn will lead to back pain and lumbar disc degeneration. At the same time, disc degeneration can also lead to lumbar instability and paravertebral muscles will degenerate because of compensation.
Machine learning plays an important role in the diagnosis and prediction of spinal diseases.30,31 The establishment of many models allows clinicians to better know the possibility of infection and the prognosis of patients.32,33 Fan et al used deep learning to identify the image features of lumbosacral reconstruction, so as to predict the difficulty of percutaneous endoscopic transforaminal discectomy, thus providing suggestions for the selection of surgical methods for surgeon. 34 In this study, this model is expected to help surgeons decide whether patients with lumbar disc herniation should undergo open or minimally invasive surgery before they operate on them.
This study also has several limitations. Firstly, this was a single-center retrospective study so the number of cases in case group was relatively small. ML models are often difficult to train with small samples, and more data can make the model have better generalization ability. Secondly, we included only patients who underwent operation again at our hospital or who were followed for reoperation at another hospital. Some patients were lost to follow-up. Thirdly, the grid search method is not efficient for fine-tuning the XGBoost classifier because of its large number of parameters. XGBoost is not suitable for scenarios with high feature dimensions, and its performance in this work greatly depends on the results of feature selection. Fourthly, not all known risk factors for rLDH were included in the present analysis. Therefore, prospective studies with a larger sample of recurrent cases and a more comprehensive follow-up period are necessary to better refine the model.
Conclusion
This study showed that the disc herniation type, Modic changes (type II), sROM, FO, and FI were significantly associated with rLDH reoperation. Disc herniation (extrusion, sequestration), Modic changes (type II), a large sROM, a large FO and high FI were independent risk factors for reoperation in LDH patients after PELD. ML methods have better potential for such multi-factor prediction tasks than traditional logistic regression models, and the XGBoost model ultimately used in this study demonstrated good sensitivity and specificity, with a prediction accuracy of 88.87% and an AUC of 90.71%. This study demonstrated that ML-based disease prediction models can help clinical surgeons to make surgical decisions and reliable diagnostic analysis can be provided efficiently and objectively when there are sufficient data.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The work was supported by the National Natural Science Foundation of China (81572109 and 81871810); National Natural Science Foundation of China Youth Science Foundation Project (82202768). No relevant financial activities outside the submitted work.
Disclaimer: The manuscript submitted does not contain information about medical device(s)/drug(s).
ORCID iDs
Zheng-Ming Shan https://orcid.org/0000-0001-8366-5259
References
- 1.Brooks M, Dower A, Abdul Jalil MF, Kohan S. Radiological predictors of recurrent lumbar disc herniation: a systematic review and meta-analysis. J Neurosurg Spine. 2020;34:1-11. [DOI] [PubMed] [Google Scholar]
- 2.Yao Y, Liu H, Zhang H, et al. Risk Factors for Recurrent Herniation After Percutaneous Endoscopic Lumbar Discectomy. World Neurosurg. 2017;100:1-6. [DOI] [PubMed] [Google Scholar]
- 3.Shin EH, Cho KJ, Kim Y T, Park MH. Risk factors for recurrent lumbar disc herniation after discectomy. Int Orthop. 2019;43(4):963-967. [DOI] [PubMed] [Google Scholar]
- 4.Li Z, Yang H, Liu M, et al. Clinical Characteristics and Risk Factors of Recurrent Lumbar Disk Herniation: A Retrospective Analysis of Three Hundred Twenty-One Cases. Spine (Phila Pa 1976). 2018;43(21):1463-1469. [DOI] [PubMed] [Google Scholar]
- 5.Siccoli A, Staartjes VE, Klukowska AM, Muizelaar JP, Schröder ML. Overweight and smoking promote recurrent lumbar disk herniation after discectomy. Eur Spine J. 2022;31:604-613. [DOI] [PubMed] [Google Scholar]
- 6.Shi H, Zhu L, Jiang ZL, Wu XT. Radiological risk factors for recurrent lumbar disc herniation after percutaneous transforaminal endoscopic discectomy: a retrospective matched case-control study. Eur Spine J. 2021;30(4):886-892. [DOI] [PubMed] [Google Scholar]
- 7.Kong M, Xu D, Gao C, et al. Risk factors for recurrent l4-5 disc herniation after percutaneous endoscopic transforaminal discectomy: a retrospective analysis of 654 cases. Risk Manag Healthc Pol. 2020;13:3051-3065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seyedhoseinpoor T, Taghipour M, Dadgoo M, et al. Alteration of lumbar muscle morphology and composition in relation to low back pain: a systematic review and meta-analysis. Spine J. 2022;22(4):660-676. [DOI] [PubMed] [Google Scholar]
- 9.Ren GK Yu, Xie Z, et al. Current Applications of Machine Learning in Spine: From Clinical View. Global Spine J. 2021;12. doi: 10.1177/21925682211035363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khan O, Badhiwala J H, Witiw C D, Wilson JR, Fehlings MG. Machine learning algorithms for prediction of health-related quality-of-life after surgery for mild degenerative cervical myelopathy. Spine J. 2021;21(10):1659-1669. [DOI] [PubMed] [Google Scholar]
- 11.Yurac R, Zamorano J J, Lira F, Valiente D, Ballesteros V, Urzúa A. Risk factors for the need of surgical treatment of a first recurrent lumbar disc herniation. Eur Spine J. 2016;25(5):1403-1408. [DOI] [PubMed] [Google Scholar]
- 12.Pfirrmann C W, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001;26(17):1873-1878. [DOI] [PubMed] [Google Scholar]
- 13.Youn M S, Shin J K, Goh T S, Lee JS. Clinical and radiological outcomes of endoscopic partial facetectomy for degenerative lumbar foraminal stenosis. Acta Neurochir (Wien). 2017;159(6):1129-1135. [DOI] [PubMed] [Google Scholar]
- 14.Skorupska E. Muscle atrophy measurement as assessment method for low back pain patients. Adv Exp Med Biol. 2018;1088:437-461. [DOI] [PubMed] [Google Scholar]
- 15.Ding J Z, Kong C, Li X Y, Sun Xy, Lu Sb, Zhao Gg. Different degeneration patterns of paraspinal muscles in degenerative lumbar diseases: a MRI analysis of 154 patients. Eur Spine J. 2022;31(3):764-773. [DOI] [PubMed] [Google Scholar]
- 16.Barros W K P, Dias L A, Fernandes M A C. Fully Parallel Implementation of Otsu Automatic Image Thresholding Algorithm on FPGA. Sensors (Basel). 2021;21(12):4151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim C H, Chung C K, Park C S, Choi B, Kim MJ, Park BJ. Reoperation rate after surgery for lumbar herniated intervertebral disc disease: nationwide cohort study. Spine (Phila Pa 1976). 2013;38(7):581-590. [DOI] [PubMed] [Google Scholar]
- 18.Huang W, Han Z, Liu J, Yu L, Yu X. Risk factors for recurrent lumbar disc herniation: a systematic review and meta-analysis. Medicine (Baltim). 2016;95(2):e2378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kara B, Tulum Z, Acar U. Functional results and the risk factors of reoperations after lumbar disc surgery. Eur Spine J. 2005;14(1):43-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim J M, Lee S H, Ahn Y, Yoon DH, Lee CD, Lim ST. Recurrence after successful percutaneous endoscopic lumbar discectomy. Minim Invasive Neurosurg. 2007;50(2):82-85. [DOI] [PubMed] [Google Scholar]
- 21.Kim KT, Park SW, Kim YB. Disc height and segmental motion as risk factors for recurrent lumbar disc herniation. Spine (Phila Pa 1976). 2009;34(24):2674-2678. [DOI] [PubMed] [Google Scholar]
- 22.Kim KT, Lee DH, Cho DC, Sung JK, Kim YB. Preoperative risk factors for recurrent lumbar disk herniation in L5-S1. J Spinal Disord Tech. 2015;28(10):E571-E577. [DOI] [PubMed] [Google Scholar]
- 23.McGirt MJ, Eustacchio S, Varga P, et al. A prospective cohort study of close interval computed tomography and magnetic resonance imaging after primary lumbar discectomy: factors associated with recurrent disc herniation and disc height loss. Spine (Phila Pa 1976). 2009;34(19):2044-2051. [DOI] [PubMed] [Google Scholar]
- 24.Chen L, Battié M C, Yuan Y, Yang G, Chen Z, Wang Y. Lumbar vertebral endplate defects on magnetic resonance images: prevalence, distribution patterns, and associations with back pain. Spine J. 2020;20(3):352-360. [DOI] [PubMed] [Google Scholar]
- 25.Feng Z, Liu Y, Yang G, Battié MC, Wang Y. Lumbar vertebral endplate defects on magnetic resonance images: classification, distribution patterns, and associations with modic changes and disc degeneration. Spine (Phila Pa 1976). 2018;43(13):919-927. [DOI] [PubMed] [Google Scholar]
- 26.Wang H, Zhou Y. Facet tropism: possible role in the pathology of lumbar disc herniation in adolescents. J Neurosurg Pediatr. 2016;18(1):111-115. [DOI] [PubMed] [Google Scholar]
- 27.Wang H, Zhang Z, Zhou Y. Irregular alteration of facet orientation in lumbar segments: possible role in pathology of lumbar disc herniation in adolescents. World Neurosurg. 2016;86:321-327. [DOI] [PubMed] [Google Scholar]
- 28.Schleich C, Müller-Lutz A, Blum K, et al. Facet tropism and facet joint orientation: risk factors for the development of early biochemical alterations of lumbar intervertebral discs. Osteoarthritis Cartilage. 2016;24(10):1761-1768. [DOI] [PubMed] [Google Scholar]
- 29.Stevens S, Agten A, Timmermans A, Vandenabeele F. Unilateral changes of the multifidus in persons with lumbar disc herniation: a systematic review and meta-analysis. Spine J. 2020;20(10):1573-1585. [DOI] [PubMed] [Google Scholar]
- 30.Harada GK, Siyaji ZK, Mallow GM, et al. Artificial intelligence predicts disk re-herniation following lumbar microdiscectomy: development of the “RAD” risk profile. Eur Spine J. 2021;30(8):2167-2175. [DOI] [PubMed] [Google Scholar]
- 31.Wirries A, Geiger F, Hammad A, et al. Ai prediction of neuropathic pain after lumbar disc herniation-machine learning reveals influencing factors. Biomedicines. 2022;10(6):1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang MZ, Ou-Yang HQ, Liu JF, et al. Predicting postoperative recovery in cervical spondylotic myelopathy: construction and interpretation of T2*-weighted radiomic-based extra trees models. Eur Radiol. 2022;32(5):3565-3575. [DOI] [PubMed] [Google Scholar]
- 33.Hopkins BS, Mazmudar A, Driscoll C, et al. Using artificial intelligence (AI) to predict postoperative surgical site infection: a retrospective cohort of 4046 posterior spinal fusions. Clin Neurol Neurosurg. 2020;192:105718. [DOI] [PubMed] [Google Scholar]
- 34.Fan G, Liu H, Wang D, et al. Deep learning-based lumbosacral reconstruction for difficulty prediction of percutaneous endoscopic transforaminal discectomy at L5/S1 level: a retrospective cohort study. Int J Surg. 2020;82:162-169. [DOI] [PubMed] [Google Scholar]