Abstract
Introduction
The use of pneumoperitoneum is an essential step for performing laparoscopic and robotic surgery. Pneumoperitoneum insufflation can cause complications such as pneumothorax, subcutaneous emphysema, and pneumomediastinum. The purpose of this meta-analysis is to compare the safety of using the conventional insufflation system versus a Valveless insufflation system as devices for manufacturing pneumoperitoneum in robotic-assisted nephrectomy.
Methods
A comprehensive literature search was conducted on PUBMED, EMBASE, SCOPUS, and Cochrane, from inception until January 2024. Randomized and nonrandomized prospective studies were included in the meta-analysis, performed by the R+ Rstudio.
Results
Three publications encompassing 478 patients were included. We observed no difference in SCE (OR 0.60, CI 95% 0.27;1.34, p = 0.134, I2 = 0), PNM (OR 0.82, CI 95% 0.24;2.78, p = 0.558, I2 = 0), When comparing groups conventional insufflation system (CIS) versus AirSealTM insufflation system (AIS) with pneumoperitoneum pressure of 15 mmHg or 12 mmHg.
Conclusion
The presented data showed no difference between the AIS when compared with CIS in Pneumoperitoneum insufflation-related complications.
Keywords: Valveless, Standard insufflation, Robot-assisted, Partial nephrectomy, Neumoperitoneum insufflation-related complications
Introduction
Minimally invasive surgery, including either traditional laparoscopic and robot-assisted laparoscopic approaches to renal surgery have been widely used. When compared to open surgery, results show less postoperative pain, shorter hospital stay, and less blood loss [1, 2]. However, despite its safety, pneumoperitoneum insufflation, in which carbon dioxide is usually used, can cause metabolic and hemodynamic changes, as well as complications.
Pneumoperitoneum insufflation-related complications (PIC) occur because CO2 dissects the subcutaneous tissue and fascia, and can cause subcutaneous emphysema (SCE), pneumothorax (PTX) and, more rarely, pneumomediastinum (PMS) [3]. These complications can lead to such clinical changes as metabolic acidosis and hypercarbia [4–6]. Although SCE has a rate of 12.5% to 45% in laparoscopic kidney and adrenal surgeries after radiographic studies, fortunately, it is a self-limiting complication in the vast majority of cases [4, 7]. The occurrence of PTX and PMS can be explained by the presence of congenital diaphragmatic channels and the passage of gas through the foramen of the inferior vena cava [8–10].
Factors related to the presence of PIC are the interaction of gas volume used, insufflation exposure time, gas flow rate, increased intra-abdominal insufflation pressure, and factors related to the patient and the trocar insertion [4, 11].
The insufflation of pneumoperitoneum is a fundamental step of the robotic-assisted PN, and can be done by 2 systems: conventional insufflation system (CIS) and valveless insufflation; The second one, the AirSealTM insufflation system (AIS) (CONMED, Utica, NY) is a valveless trocar system, that enables a stable pneumoperitoneum with continuous smoke evacuation and CO2 recirculation during surgery, reducing CO2 absorption and consumption [11]. Previous studies, in urological surgery, found superiority in the stability of pneumoperitoneum when AIS is used compared to CIS [12–14].
This meta-analysis aims to compare the incidence of PIC in robotic partial nephrectomy when using AIS vs. CIS, composed exclusively of prospective studies on the topic.
Material and methods
Eligibility criteria
This study was registered at Prospero CRD42024508682. A search was conducted at PubMed/MEDLINE, Embase, Cochrane, and Scopus data-bases from its inception to January 2024 to identify Prospective Studies, reporting the Comparison of valveless and standard insufflation on pneumoperitoneum‑related complications in robotic partial nephrectomy for various causes. Our outcomes of interest were the rate of SCE and PMS.
Search strategy and data extraction
We systematically searched PubMed, Embase, Cochrane, and Scopus Central Register of Prospective Studies from inception to January 2024 with the following search terms: (‘valve less’ OR ‘valveless’ OR ‘Standard Insufflation’) AND (‘Robotic Partial Nephrectomy’ OR ‘robot-assisted partial nephrectomy’). Zotero was utilized to remove any duplicate studies. Two independent researchers conducted a screening of titles and abstracts to eliminate irrelevant studies. Following this process, the full text was reviewed to select the included studies. Any disagreements were solved by a third reviewer.
Quality assessment
Data was independently extracted from the included studies by two authors. Any discrepancies among the extracted data were resolved by discussion with a third reviewer. The Rob2 tool [15] was used to assess the quality of the RCTs and ROBIN-1 was used to assess the quality of non-RCTs.
Statistical analysis
The meta-analysis was performed by the R + Rstudio (RStudio Team (2023). Rstudio: Integrated Development for R. Rstudio, PBC, Boston, MA) [15]. Dichotomous data are presented as Odds Ratio with 95% CI. Pooled estimates were calculated with the random-effect model, considering that the patients came from different populations. For all statistical analyses, a two-sided value of p < 0,05 was considered statistically significant. The I2 statistic and the p-value tests were used to assess heterogeneity.
Results
Study selection and characteristics
The search retrieved 23 articles. After screening, 4 Prospective studies were included in this meta-analysis (Fig. 1). In total, 478 patients were included, and data as baseline characteristics, device type, age and gender. Two different pneumoperitoneum pressure values were used among the studies (15 mmHg and 12 mmHg) (Table 1).
Fig. 1.
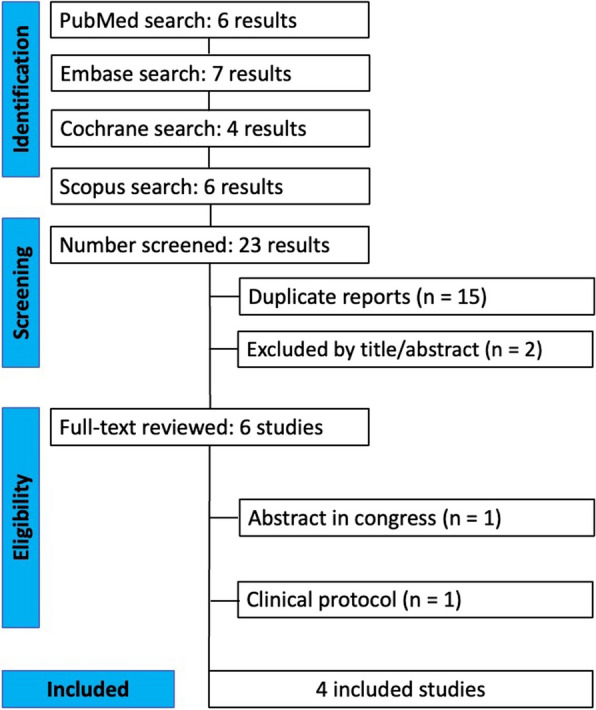
Prisma flow diagram
Table 1.
Baseline characteristics of included studies
| Study | Design | Pneumoperitoneum | Pressure | Airseal/standard | Mean Age (y) ± SD / airseal / standard | Gender (%), male / female / airseal / standard | Pneumothorax airseal / standard |
|---|---|---|---|---|---|---|---|
| Annino et al., 2017 [12] | Cohort | Airseal versus standard | 15 mmHg | 67/55 | 66.2 (6.8) / 67 (7.9) |
M: 70% / 74,5% F: 30% / 25,5% |
0 / 0 |
| Desroches et al., 2021 [16] | RCT | Airseal versus standard | 15 mmHg | 69/66 | 60.1(11.8) / 60 (12.5) |
M: 62% / 65% / F: 38% / 35% |
3 (5%) / 3(5%) |
| Feng et al., 2021 [17] | RCT | Airseal versus standard | 15 mmHg | 31/31 | 60.4 (12) / 61 (11.6) |
M: 58% / 61% / F: 42% / 39% |
1 (3,2%) / 3 (9,6%) |
| Wei et al., 2024 [18] | RCT | Airseal versus standard | 12 mmHg | 31/31 | 56.1 (4.6) / 53.7 (3.9) |
M: 64.5% / 54.8% F: 45.2% / 35.5% |
- |
Subcutaneous emphysema (SCE)
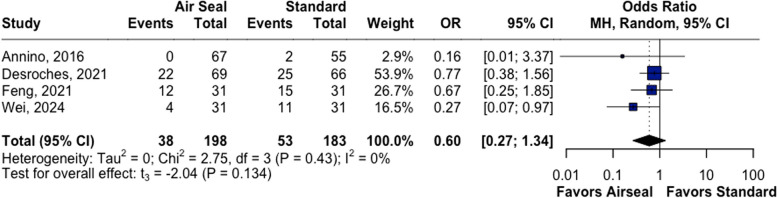
AIS was no different when compared to CIS method in our primary outcome (SCE) (OR 0.60, CI 95% 0.27;1.34, p = 0.134, I2 = 0) (Fig. 2).
Fig. 2.
AirSeal versus Standard group pneumoperitoneum insufflation, no difference in SCE complication. A Forest plot of subcutaneous emphysema SCE (enfisema subcutâneo), CI, confidence
Pneumothorax (PTX)
It was not possible to evaluate pneumothorax rates through meta-analysis because one of the studies did not present the complication in any of the groups [12].
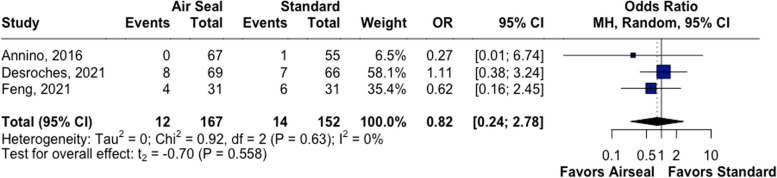
Pneumomediastinum (PMS)
AIS was no different when compared to CIS method in our primary outcome (PMS) (OR 0.82, CI 95% 0.24;2.78, p = 0.558, I2 = 0 (Fig. 3).
Fig. 3.
AirSeal versus Standard group pneumoperitoneum insufflation, no difference in PMS complication. A Forest plot of pneumomediastinum PMS (pneumomediastino), CI, confidence interval
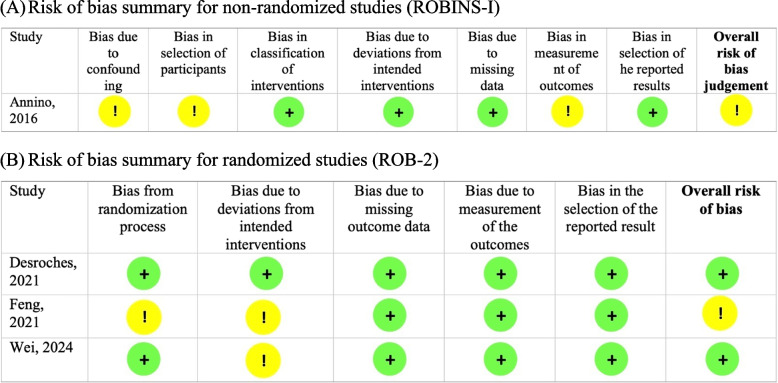
Risk of bias
The only trial non-RCT [12] was assessed by Robins-I score, ant it presented a moderate risk of bias (Fig. 4A). On the other hand, the RCTs trials were assessed through Rob-2 tool, which presented a low overall score of bias in Desroches 2021 trial, and a moderate risk in the Feng’s 2021 study (Fig. 4B).
Fig. 4.
Risk of bias of the included studies (ROBINS-1) and (ROB-2). Risk os bias (robins1). A Risk of bias summary for non-randomized studies (ROBINS-I). B Risk of bias summary for randomized studies (ROB-2). C Risk of bias summary for randomized studies (ROB-2)
Discussion
In our meta-analysis, we included 478 patients from 4 different Prospective Studies comparing AIS vs CIS, who underwent robotic PN, using Pneumoperitoneum pressure of 15 mmHg or 12 mmHg. We observed that AIS was not superior to CIS regarding PIC, such as SCE e PMS.
American Urological Association and European Association of Urology have no position regarding the optimal technique for pneumoperitoneum. Increased intra-abdominal insufflation pressure is a cause of complications such as subcutaneous emphysema and periodic episodes of blood pressure peaks during its use. Thus, the AIS emerges as a device with a theoretical benefit over these complications. Although the use of AIS versus the CIS method boasts, in the AIS group, a lower rate of complications in the AIS group, as PTX, SCE, and PMS, this difference has not been statistically proven [17].
Of the 4 studies evaluated in this work, only Desroches et al. statistically demonstrated the superiority of AIS versus CIS in SCE when comparing pneumoperitoneum pressure of 12 mmHg versus 15 mmHg. There was no superiority in other complications between the pressure of 12 mmHg versus 15 mmHg and 15 mmHg versus 15 mmHg in AIS versus CIS [12, 16, 17, 19]. Wei et al. demonstrated that there is an association between airseal and lower rates of subcutaneous emphysema when using pressures of 12 mmHg [18]. Recently a meta-analysis [20], was published and showed that the use of airseal would be associated with lower rates of subcutaneous emphysema and pain after surgery. We did not find this association.
PTX is one of the most feared complications of laparoscopic surgeries, which can lead the patient to a relevant clinical complication and consequently to an unscheduled outcome. The main causes for such complication are: simple gas diffusion, iatrogenesis, anatomical defects [21]. The main risk factors involved in the genesis of PTX during laparoscopic surgery are surgical time > 200 min, positive end tidal CO2 > 50 mmHg, and operator inexperience [22–24].
The rate of PTX was not evaluated since one of the selected studies did not present cases of PTX. Further studies should be carried out to evaluate the rate of PTX during robotic PN, when using AIS vs. CIS.
Conclusion
The synthesis of the available evidence showed no difference between the AIS when compared with CIS in Pneumoperitoneum insufflation-related complications. However, the results suggest that with a higher N, the comparison in vogue would be statistically significant. More RCTs are necessary to ratify our findings.
Acknowledgements
Nothing to declare.
Abbreviations
- PIC
Pneumoperitoneum Insufflation-related Complications
- CO2
Carbon Dioxide
- SCE
Subcutaneous Emphysema
- PTX
Pneumothorax
- PMS
Pneumomediastinum
- CIS
Conventional Insufflation System
- AIS
AirSeal Insufflation System
- PN
Partial Nephrectomy
- Rob2
Cochrane Risk of Bias Tool Version 2
- RStudio
Integrated Development Environment for R
- PBC
Public Benefit Corporation
- I2
Heterogeneity Statistic
Authors’ contributions
Richard Dobrucki de Lima conceived, screened the papers, and wrote. Lucas Schenk de Almeida screened the papers and wrote. Breno Cordeiro Porto and Carlo Passerotti screened the papers. José Pinhata Otoch supervised. José Arnaldo Shiomi da Cruz and Rodrigo Afonso da Silva Sardenberg supervised and guided.
Funding
Not applicable.
Data availability
Data is provided within the manuscript in Table 1 (at the end of the document).
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors have reviewed and approved the manuscript for publication.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wein AJ, Kavoussi LR, Partin AW, Peters CA. Campbell-Walsh Urology. 10th ed. Philadelphia: Elsevier Saunders; 2012. p. 204. [Google Scholar]
- 2.Wu Z, Li M, Liu B, Cai C, Ye H, Lv C, Yang Q, Sheng J, Song S, Qu L, Xiao L, Sun Y, Wang L. Robotic versus open partial nephrectomy: a systematic review and meta-analysis. PLoS One. 2014;9(4):e94878. 10.1371/journal.pone.0094878. PMID:24740259;PMCID:PMC3989253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuntz C, Wunsch A, Bödeker C, Bay F, Rosch R, Windeler J, Herfarth C. Effect of pressure and gas type on intraabdominal, subcutaneous, and blood pH in laparoscopy. Surg Endosc. 2000;14(4):367–71. 10.1007/s004640000156. PMID: 10790557. [DOI] [PubMed] [Google Scholar]
- 4.Ott DE. Subcutaneous emphysema–beyond the pneumoperitoneum. JSLS. 2014;18(1):1–7. 10.4293/108680813X13693422520882. Erratum in: JSLS. 2016 Apr-Jun;20(2). pii: e2016.00050. 10.4293/JSLS.2016.00050. PMID: 24680136; PMCID: PMC3939322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wahba RW, Tessler MJ, Kleiman SJ. Acute ventilatory complications during laparoscopic upper abdominal surgery. Can J Anaesth. 1996;43(1):77–83. 10.1007/BF03015963. PMID: 8665641. [DOI] [PubMed] [Google Scholar]
- 6.Abe H, Bandai Y, Ohtomo Y, Shimomura K, Nayeem SA, Idezuki Y. Extensive subcutaneous emphysema and hypercapnia during laparoscopic cholecystectomy: two case reports. Surg Laparosc Endosc. 1995;5(3):183–7. PMID: 7633643. [PubMed] [Google Scholar]
- 7.Ng CS, Gill IS, Sung GT, Whalley DG, Graham R, Schweizer D. Retroperitoneoscopic surgery is not associated with increased carbon dioxide absorption. J Urol. 1999;162(4):1268–72. PMID: 10492177. [PubMed] [Google Scholar]
- 8.Sharma KC, Kabinoff G, Ducheine Y, Tierney J, Brandstetter RD. Laparoscopic surgery and its potential for medical complications. Heart Lung. 1997;26(1):52–64; quiz 65-7. 10.1016/s0147-9563(97)90009-1. PMID: 9013221. [DOI] [PubMed] [Google Scholar]
- 9.Batra MS, Driscoll JJ, Coburn WA, Marks WM. Evanescent nitrous oxide pneumothorax after laparoscopy. Anesth Analg. 1983;62(12):1121–3. PMID: 6228171. [PubMed] [Google Scholar]
- 10.Fitzgerald SD, Andrus CH, Baudendistel LJ, Dahms TE, Kaminski DL. Hypercarbia during carbon dioxide pneumoperitoneum. Am J Surg. 1992;163(1):186–90. 10.1016/0002-9610(92)90274-u. PMID: 1733368. [DOI] [PubMed] [Google Scholar]
- 11.Lee DW, Kim MJ, Lee YK, Lee HN. Does intraabdominal pressure affect development of subcutaneous emphysema at gynecologic laparoscopy? J Minim Invasive Gynecol. 2011;18(6):761–5. 10.1016/j.jmig.2011.08.006. Epub 2011 Sep 21 PMID: 21940220. [DOI] [PubMed] [Google Scholar]
- 12.Annino F, Topazio L, Autieri D, Verdacchi T, De Angelis M, Asimakopoulos AD. Robotic partial nephrectomy performed with Airseal versus a standard CO2 pressure pneumoperitoneum insufflator: a prospective comparative study. Surg Endosc. 2017;31(4):1583–90. 10.1007/s00464-016-5144-y. Epub 2016 Aug 5. [DOI] [PubMed]
- 13.Bucur P, Hofmann M, Menhadji A, Abedi G, Okhunov Z, Rinehart J, Landman J. Comparison of pneumoperitoneum stability between a valveless trocar system and conventional insufflation: a prospective randomized trial. Urology. 2016;94:274–80. 10.1016/j.urology.2016.04.022. Epub 2016 Apr 27 PMID: 27130263. [DOI] [PubMed] [Google Scholar]
- 14.Herati AS, Andonian S, Rais-Bahrami S, Atalla MA, Srinivasan AK, Richstone L, Kavoussi LR. Use of the valveless trocar system reduces carbon dioxide absorption during laparoscopy when compared with standard trocars. Urology. 2011;77(5):1126–32. 10.1016/j.urology.2010.06.052. Epub 2010 Oct 2 PMID: 20888033. [DOI] [PubMed] [Google Scholar]
- 15.R Core Team. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2023. [Google Scholar]
- 16.Desroches B, Porter J, Bhayani S, Figenshau R, Liu PY, Stifelman M. Comparison of the safety and efficacy of valveless and standard insufflation during robotic partial nephrectomy: a prospective, randomized, Multi-institutional Trial. Urology. 2021;153:185–91. 10.1016/j.urology.2021.01.047. Epub 2021 Feb 10 PMID: 33577899. [DOI] [PubMed] [Google Scholar]
- 17.Feng TS, Heulitt G, Islam A, Porter JR. Comparison of valve-less and standard insufflation on pneumoperitoneum-related complications in robotic partial nephrectomy: a prospective randomized trial. J Robot Surg. 2021;15(3):381–8. 10.1007/s11701-020-01117-z. Epub 2020 Jul 6 PMID: 32632561. [DOI] [PubMed] [Google Scholar]
- 18.Wei M, Yang W, Zhou J, Ye Z, Ji Z, Dong J, Xu W. Comparison of AirSeal versus conventional insufflation system for retroperitoneal robot-assisted laparoscopic partial nephrectomy: a randomized controlled trial. World J Urol. 2024;42(1):90. 10.1007/s00345-024-04819-3. PMCID:PMC10881696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nepple KG, Kallogjeri D, Bhayani SB. Benchtop evaluation of pressure barrier insufflator and standard insufflator systems. Surg Endosc. 2013;27(1):333–8. 10.1007/s00464-012-2434-x. Epub 2012 Jul 26 PMID: 22833262. [DOI] [PubMed] [Google Scholar]
- 20.Fan G, Chen Y, Wang J, Wu Y, Wang Y, Hu K, Tang T. Comparison of AirSeal versus conventional insufflation system for robot-assisted partial nephrectomy: a meta-analysis and systematic review. J Robot Surg. 2024;18(1):269. 10.1007/s11701-024-02023-4. PMID: 38922386. [DOI] [PubMed] [Google Scholar]
- 21.Machairiotis N, Kougioumtzi I, Dryllis G, Katsikogiannis N, Katsikogianni F, Courcoutsakis N, Kioumis I, Pitsiou G, Zarogoulidis K, Zarogoulidis P. Laparoscopy induced pneumothorax. J Thorac Dis. 2014;6(S4):S404–6. 10.3978/j.issn.2072-1439.2014.08.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hawasli A. Spontaneous resolution of massive laparoscopyassociated pneumothorax: the case of the bulging diaphragm and review of the literature. J Laparoendosc Adv Surg Tech A. 2002;12:77–82. [DOI] [PubMed] [Google Scholar]
- 23.Gueret G, Guischard F, Dumoulin JL, et al. Lifethreatening bilateral pneumothorax caused by misconnection of the laser lens cooling system during gynecologic laparoscopy. Anesthesiology. 1999;91:1179–80. [DOI] [PubMed] [Google Scholar]
- 24.Labow DM, Conlon KC. Pneumothorax after diagnostic laparoscopy. Surg Endosc. 1999;13:935–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is provided within the manuscript in Table 1 (at the end of the document).