Abstract
Objective
This study aimed to assess the public’s knowledge of stroke before and after viewing an educational video about stroke risk factors, preventive measures, and alarming signs.
Methods
A single-arm interventional study was conducted in Lebanon using a 3-minute video-based education about stroke. A pre- and post-structured questionnaire compared the level of knowledge about stroke.
Results
The study included 685 participants. Knowledge of stroke, risk factors, warning signs, treatment, and preventive measures significantly increased post-educational video sessions. A higher baseline knowledge score was associated with a family history of stroke (Beta = 1.76) and being a healthcare professional (Beta = 3.35). Participants between 25 and 34 years (Beta=-1.39) and those with a high risk of stroke (Beta=-1.03) were significantly associated with a lower knowledge score.
Conclusion
This study demonstrated the effectiveness of a video-based educational tool to raise awareness about stroke. Short, targeted audio-visual resources using lay language can convey health education messages and influence behavioral changes. The community can benefit from a large-scale educational campaign that targets different socio-economic statuses to enhance knowledge of stroke and save lives.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-20552-3.
Keywords: Stroke, Educational video, Health promotion, Awareness, Population health
Introduction
A stroke is a medical emergency that requires urgent and specialized care [1]. Early recognition of stroke warning signs and prompt access to care is critical for improving patient outcomes and reducing the risk of disability and death [2]. Studies have shown that public knowledge of stroke is limited [3] and highlighted the importance of educational programs for disease and complications avoidance [4], that can significantly improve stroke knowledge and awareness in patients and their families [5].
In fact, educational campaigns must target at-risk individuals, family members, and communities at large, to reduce stroke morbidity and mortality [6]. Educational material should focus on enhancing public awareness and knowledge of stroke signs and symptoms, encouraging individuals to take quick action, avoiding risk factors, and taking preventive strategies [7–9]. Educational strategies can be health campaigns, community outreach programs, and educational resources, including brochures, videos, and seminars [10].
Relevant international societies made efforts to address this gap. For example, the American Heart Association/American Stroke Association (AHA/ASA) implemented a community-based stroke education program using interactive sessions covering the disease risk factors, warning signs, and the importance of seeking timely medical attention [11]. Data shows that in low- and middle-income countries (LMICs), the burden of stroke is still increasing [12]. In Lebanon, stroke is the second leading cause of death, with rates ranging between 14.1 and 22% [13]. Despite the detrimental impact of stroke, knowledge and awareness about this disease remain limited [14, 15]. Therefore, this study aimed to assess the effect of an educational video intervention and identify predictors that may contribute to variations in knowledge and awareness outcomes by conducting a comparative analysis of knowledge and awareness levels among participants before and after the implementation of the intervention.
Methods
Study design
A single-arm cross-sectional study with an interventional approach was conducted between July 01, 2022, and September 30, 2022, to comprehensively evaluate the effect of and the factors influencing an educational video intervention.
Participants
Eligible participants were adults aged 25 years and older residing in Lebanon. The threshold of 25 years was chosen because individuals between the ages of 18 and 25 are considered emerging adults [16] who are unlikely to be interested in chronic diseases.
Procedure
Data were collected through an anonymous online questionnaire created on Google Forms, a cloud-based survey powered by Google™. The online survey included a 3-minute educational video titled “Think Fast, Act Fast to Save a Life” embedded after the pre-test knowledge survey and before the post-knowledge section. Both the questionnaire and the educational video were compatible with the American Stroke Association online awareness materials and were translated into Arabic, the native language of Lebanon and other countries in the region, according to the World Health Organization’s translation guidelines [17]. A forward translation was first performed from English into Arabic, and then the translated version was back-translated into English. The two English versions were compared, with minor discrepancies corrected by consensus between the translators and the authors. Thus, the questionnaire was available in both languages and was electronically distributed via social media platforms, e.g., WhatsApp, Instagram, Twitter, and Facebook. The link to the questionnaire is available in supplementary material.
Before administration, the questionnaire was pilot-tested with a sample of 20 individuals to identify any potential ambiguities. Further validation involved content review by experts, including one of the authors, to ensure comprehensive coverage of relevant content. Subsequent feedback prompted necessary revisions for clarity and cultural relevance. Additionally, the validation process assessed construct validity and reliability, utilizing Cronbach’s alpha for internal consistency, to ensure the questionnaire effectively measures the intended construct. Results of the Factor analysis (Promax rotated component matrix) are found in supplementary material. In brief, the questionnaire explains 48.67% of the variance and its internal consistency was confirmed through Cronbach’s alpha, yielding a high value of 0.911. Furthermore, the questionnaire encompassed the following six sections: (1) demographics, (2) lifestyle, (3) health status, (4) pre-test of knowledge and awareness about the disease, attributable risk factors, alarming signs, and preventive measures, (5) a three-minute educational video available in both English and Arabic (links available in supplementary material), followed by (6) a post-test that consisted of the same sets of questions included in the pre-test.
Ethical considerations
This study, approved by the Institutional Review Board at Abu Dhabi University under code CoHS–22-05-00018 on 05/16/2022, adhered to the Declaration of Helsinki. Before filling out the online survey, participants were briefed about the study objectives and their right to withdraw at any time. Informed consent was obtained from all participants, by including a consent statement at the beginning of the survey. Participants were required to read the statement and click a checkbox indicating their agreement to participate in the study before proceeding to the questionnaire. Participants did not receive any financial reward for their participation. The online survey was anonymous and voluntary. Collected data were encrypted, stored in password-protected computers, and presented as de-identified electronic files in Microsoft Excel and SPSS.
Sample size calculation
The minimum sample size was calculated using the G-Power software version 3.0.10.
The calculated effect size was 0.0526, expecting squared multiple correlations of 0.05 (R2 deviation from 0) related to the Omnibus test of multiple regression. The minimum necessary sample was n = 371, considering an alpha error of 5%, a power of 80%, and allowing 15 predictors to be included in the model. A minimum sample of 400 participants was targeted to account for potential missing values.
Data analysis
Data were analyzed on SPSS software version 25. A descriptive analysis was performed using absolute frequencies and percentages for categorical variables and means and standard deviations (SD) for quantitative measures.
As the skewness and kurtosis values of the dependent variable (knowledge total score) were within the acceptable range (− 2 and + 2), the data were considered to be normally distributed. In addition, the normal probability plots of the dependent variables were analyzed and the results showed a normal distribution.
The paired sample t-test was used to compare the stroke knowledge score before and after the education session. Also, a repeated measures ANOVA was performed to evaluate the mean change of the stroke total knowledge pre- and post-educational session after adjusting for the following covariates: age, gender, marital status, smoking, alcohol consumption, education level, healthy lifestyle index, having a stroke, a family history of stroke, and having any medical illness. The healthy lifestyle index, based on prior research [18–21], considers three types of variables: eating well, healthy weight and physical activity and provides a consolidated measure reflecting adherence to health-promoting habits and behaviors. It is calculated by summing individual scores for maintaining body weight in the normal range, being a non-smoker or former smoker, abstaining from alcohol, engaging in various levels of exercise (mild, moderate, and vigorous), and consuming fruits, vegetables, and fluids daily.
Three linear regressions were conducted, with the knowledge total score before and after the educational session and the difference between the two sessions as separate dependent variables. The model included sociodemographic variables along with those related to stroke risk factors. A p-value < 0.05 was considered significant.
Results
Sample description
A total of 685 participants were included in the study. Participants were predominantly females 63.8%, highly educated, and aged 25 to 44. Only 2% had a history of previous stroke was seen in 2%, while 35.6% had a family history of stroke, 27% had a family history of myocardial infarction, 19% had high cholesterol, and 16% had high blood pressure. Around half had a healthy lifestyle, including no smoking, mild to moderate exercising, and a normal BMI (Table 1).
Table 1.
Sociodemographic characteristics of the participants
| Variable | N (%) |
|---|---|
| Total participants | 685 (100) |
| Gender | |
| Male | 248 (36.2%) |
| Female | 437 (63.8%) |
| Age | |
| 25–34 | 285 (41.6%) |
| 35–44 | 127 (18.5%) |
| 45–54 | 155 (22.6%) |
| 55 and above | 118 (17.2%) |
| Marital status | |
| Single/widowed/divorced | 325 (47.4%) |
| Married | 360 (52.6%) |
| Education level | |
| Primary | 30 (4.4%) |
| Secondary | 50 (7.3%) |
| University | 605 (88.3%) |
| Being a healthcare professional | |
| Yes | 135 (19.7%) |
| No | 550 (80.3%) |
| Stroke risk factors | |
| Family history of stroke | |
| Yes | 244 (35.6%) |
| No | 441 (64.4%) |
| Previous stroke | |
| Yes | 14 (2.0%) |
| No | 671 (98.0%) |
| Smoking | |
| Never smoke | 401 (58.5%) |
| Current smoker | 234 (34.2%) |
| Former smoker | 50 (7.3%) |
| Physical activity | |
| Inactive (Sedentary) | 24 (3.5%) |
| Mild | 359 (52.4%) |
| Moderate | 229 (33.4%) |
| Vigorous | 73 (10.7%) |
| BMI categories | |
| Underweight | 24 (3.5%) |
| Healthy weight | 334 (48.8%) |
| Overweight | 225 (32.8%) |
| Obese | 102 (14.9%) |
| Having any of the following health conditions | |
| High blood pressure | 110 (16.1%) |
| History of myocardial infarction | 35 (5.1%) |
| Family history of myocardial infarction | 184 (26.9%) |
| History of coronary artery disease | 65 (9.5%) |
| High cholesterol level | 130 (19.0%) |
| Diabetes | 68 (9.9%) |
| History of deep vein thrombosis | 30 (4.4%) |
| History of pulmonary embolism | 19 (2.8%) |
| Severe headache (migraine) | 132 (19.3%) |
| Mean ± SD | |
| Household crowding index | 0.95 ± 0.52 |
Comparison of stroke knowledge before and after the educational session
Table 2 presents the percentages of correct answers about stroke, stroke types, risk factors, warning signs, preventive measures, treatment, and the emergency status of disease occurrence. The frequency of correct responses improved after the educational intervention as compared to before.
Table 2.
Public knowledge of stroke among participants
| Question | Pre-education | Post-education | p-value |
|---|---|---|---|
| n (%) | n (%) | ||
| Definition of stroke (1 correct answer: brain) | |||
| Correct | 619 (90.4%) | 648 (94.6%) | < 0.001 |
| Wrong | 30 (4.4%) | 17 (2.5%) | |
| Unknown | 36 (5.3%) | 20 (2.9%) | |
| Types of stroke (2 types) | |||
| 1 type correct (ischemic or hemorrhagic) | 584 (85.3%) | 651 (95.0%) | < 0.001 |
| 2 types correct (ischemic and hemorrhagic) | 297 (43.4%) | 520 (75.9%) | < 0.001 |
| Unknown | 236 (34.5%) | 67 (9.8%) | < 0.001 |
| Risk factors for stroke - Diseases (Overall 5 factors) | |||
| At least 1 factor correct | 123 (18.0%) | 52 (7.6%) | < 0.001 |
| 2 factors correct | 72 (10.5%) | 40 (5.8%) | |
| 3 factors correct | 93 (13.6%) | 62 (9.1%) | |
| More than 3 factors correct | 397 (58.0%) | 531 (77.5%) | |
| Unknown | 617 (90.1%) | 592 (86.4%) | 0.004 |
| Risk factors for stroke - Lifestyle and others (Overall 6 factors) | |||
| At least 1 factor correct | 82 (12.0%) | 30 (4.4%) | < 0.001 |
| 2 factors correct | 57 (8.3%) | 10 (1.5%) | |
| 3 factors correct | 104 (15.2%) | 33 (4.8%) | |
| More than 3 factors correct | 442 (64.5%) | 612 (89.3%) | |
| Unknown | 160 (23.4%) | 47 (6.9%) | < 0.001 |
| Stroke warning signs (overall 5 symptoms) | |||
| At least 1 symptom correct | 68 (9.9%) | 27 (3.9%) | < 0.001 |
| 2 symptoms correct | 45 (6.6%) | 8 (1.2%) | |
| 3 symptoms correct | 76 (11.1%) | 21 (3.1%) | |
| More than 3 symptoms correct | 496 (72.4%) | 629 (91.8%) | |
| Unknown | 307 (44.8%) | 99 (14.5%) | < 0.001 |
| Stroke Treatment (overall 2 treatment options) | |||
| 1 treatment option correct | 566 (82.6%) | 647 (94.5%) | < 0.001 |
| 2 treatment options correct | 388 (56.6%) | 587 (85.7%) | < 0.001 |
| In case of stroke, when to call ambulance | |||
| Correct | 624 (91.1%) | 650 (94.9%) | < 0.001 |
| Wrong | 61 (8.9%) | 35 (5.1%) | |
| Prevention of stroke (overall 6 lifestyle measures) | |||
| At least 1 measure correct | 2 (0.3%) | 18 (2.6%) | < 0.001 |
| 2 measures correct | 2 (0.3%) | - | |
| 3 measures correct | 5 (0.7%) | 6 (0.9%) | |
| More than 3 measures correct | 676 (98.7%) | 661 (96.5%) |
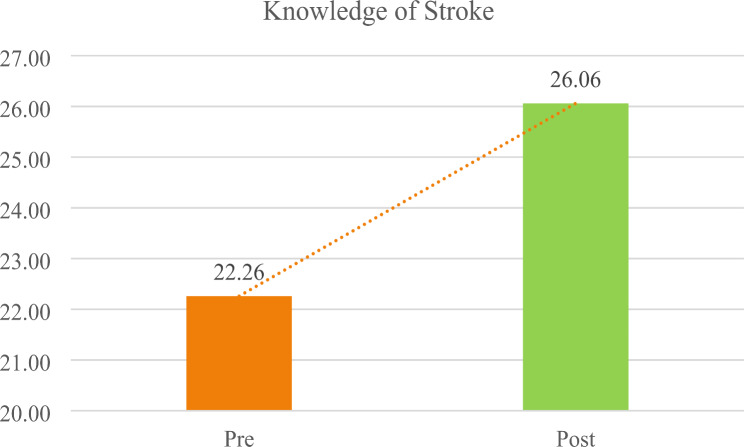
Figure 1 shows the means of the knowledge total score before and after the educational session, after adjustment over age, gender, marital status, smoking, alcohol consumption, education level, healthy lifestyle, having a stroke, a family history of stroke, and having any medical illness. A significantly higher increase was found in the total knowledge score after the educational video (22.26 vs. 26.06, Mean difference = 3.80, confidence level 3.44–4.15, p < 0.001).
Fig. 1.
Adjusted mean of the knowledge total score before and after educational video
Bivariate analysis
The pre-test results showed a significantly higher mean score knowledge among healthcare professionals and participants with a family history of stroke. The post-test results indicated a significantly higher mean knowledge in participants 55 years and above. The difference in knowledge score pre- and post-intervention in each variable is significant where a higher mean knowledge score was found in the post intervention group as compared to the pre intervention group (p < 0.001 for all) (Table 3).
Table 3.
Factors affecting the knowledge score (pre/post-test)
| Variable | Knowledge score | ||||
|---|---|---|---|---|---|
| Pre-test | P value | Post-test | P value | p-value of the difference in knowledge score pre- and post-intervention | |
| Gender | |||||
| Male | 22.46 ± 6.03 | 0.528 | 26.26 ± 4.74 | 0.442 | |
| Female | 22.15 ± 6.33 | 25.95 ± 5.07 | |||
| Mean ± SE | 22.31 ± 0.24 | 26.11 ± 0.19 | < 0.001 | ||
| Age (years) | |||||
| 25–34 | |||||
| No | 22.01 ± 6.05 | 0.202 | 26.26 ± 4.23 | 0.256 | |
| Yes | 22.62 ± 6.44 | 25.80 ± 5.81 | |||
| Mean ± SE | 22.32 ± 0.24 | 26.03 ± 0.19 | < 0.001 | ||
| 35–44 | |||||
| No | 22.36 ± 6.19 | 0.411 | 26.15 ± 4.94 | 0.315 | |
| Yes | 21.85 ± 6.33 | 25.66 ± 4.98 | |||
| Mean ± SE | 22.11 ± 0.30 | 25.91 ± 0.24 | < 0.001 | ||
| 45–54 | |||||
| No | 22.34 ± 6.20 | 0.571 | 25.97 ± 5.14 | 0.344 | |
| Yes | 22.01 ± 6.30 | 26.40 ± 4.23 | |||
| Mean ± SE | 22.18 ± 0.28 | 26.18 ± 0.22 | < 0.001 | ||
| 55 and above | |||||
| No | 22.28 ± 6.38 | 0.849 | 25.93 ± 5.23 | 0.036 | |
| Yes | 22.16 ± 5.41 | 26.71 ± 3.20 | |||
| Mean ± SE | 22.22 ± 0.31 | 26.32 ± 0.25 | < 0.001 | ||
| Marital status | |||||
| Single/widowed/divorced | 22.86 ± 6.01 | 0.017 | 25.98 ± 5.38 | 0.674 | |
| Married | 21.72 ± 6.35 | 26.14 ± 4.53 | |||
| Mean ± SE | 22.29 ± 0.24 | 26.06 ± 0.19 | < 0.001 | ||
| University degree | |||||
| No | 22.47 ± 4.99 | 0.752 | 26.50 ± 4.67 | 0.408 | |
| Yes | 22.24 ± 6.36 | 26.01 ± 4.99 | |||
| Mean ± SE | 22.35 ± 0.37 | 26.25 ± 0.29 | < 0.001 | ||
| Being a healthcare professional | |||||
| No | 21.62 ± 6.22 | < 0.001 | 25.93 ± 5.04 | 0.159 | |
| Yes | 24.91 ± 5.49 | 26.60 ± 4.55 | |||
| Mean ± SE | 23.26 ± 0.29 | 26.27 ± 0.24 | < 0.001 | ||
| Previous stroke | |||||
| No | 22.22 ± 6.25 | 0.221 | 26.05 ± 4.98 | 0.623 | |
| Yes | 24.28 ± 3.72 | 26.71 ± 2.94 | |||
| Mean ± SE | 23.25 ± 0.84 | 26.38 ± 0.67 | < 0.001 | ||
| Family history of stroke | |||||
| No | 21.67 ± 6.58 | < 0.001 | 26.00 ± 5.00 | 0.649 | |
| Yes | 23.34 ± 5.34 | 26.18 ± 4.87 | |||
| Mean ± SE | 22.51 ± 0.24 | 26.09 ± 0.19 | < 0.001 | ||
| Any high risk disease | |||||
| No | 22.45 ± 6.20 | 0.386 | 26.39 ± 4.39 | 0.067 | |
| Yes | 22.04 ± 6.24 | 25.68 ± 5.53 | |||
| Mean ± SE | 22.25 ± 0.24 | 26.04 ± 0.19 | < 0.001 | ||
| Current smoker | |||||
| No | 22.24 ± 6.31 | 0.875 | 26.27 ± 4.77 | 0.135 | |
| Yes | 22.32 ± 6.04 | 25.67 ± 5.27 | |||
| Mean ± SE | 22.28 ± 0.25 | 25.97 ± 0.19 | < 0.001 | ||
| Consumes alcohol | |||||
| No | 22.25 ± 6.37 | 0.936 | 26.00 ± 5.21 | 0.710 | |
| Yes | 22.28 ± 6.06 | 26.14 ± 4.67 | |||
| Mean ± SE | 22.26 ± 0.24 | 26.07 ± 0.19 | < 0.001 | ||
| Healthy lifestyle index | |||||
| No | 22.15 ± 6.21 | 0.250 | 26.05 ± 5.02 | 0.890 | |
| Yes | 22.93 ± 6.26 | 26.13 ± 4.51 | |||
| Mean ± SE | 22.54 ± 0.34 | 26.09 ± 0.27 | < 0.001 | ||
SE: Standard Error
Multivariable analysis
A first linear regression model was performed, taking the stroke knowledge pre-educational video as the dependent variable. The results showed that having a family history of stroke (Beta = 1.76) and being a healthcare professional (Beta = 3.35) were significantly associated with a higher knowledge score (Table 4, Model 1).
Table 4.
Factors associated with knowledge, before and after the educational video as well as the difference between them
| Model 1: taking the knowledge of stroke pre-test as the dependent variable | |||||
|---|---|---|---|---|---|
| Unstandardized Beta | Standardized Beta | p-value | Confidence interval | ||
| Lower Bound | Upper Bound | ||||
| Age in years (25–34) | -0.722 | -0.057 | 0.371 | -2.304 | 0.861 |
| Age in years (35–344) | -0.360 | -0.022 | 0.652 | -1.925 | 1.206 |
| Age in years (45–54) | -0.220 | -0.015 | 0.773 | -1.717 | 1.277 |
| Gender (female vs. male*) | -0.370 | -0.029 | 0.465 | -1.365 | 0.624 |
| History of stroke (yes vs. no*) | 2.252 | 0.051 | 0.177 | -1.019 | 5.522 |
| Family history of stroke (yes vs. no*) | 1.769 | 0.136 | < 0.001 | 0.801 | 2.737 |
| Healthcare professional (yes vs. no*) | 3.354 | 0.215 | < 0.001 | 2.158 | 4.550 |
| Alcohol (yes vs. no*) | 0.220 | 0.018 | 0.655 | -0.748 | 1.188 |
| Healthy lifestyle (yes vs. no*) | 0.592 | 0.033 | 0.377 | -0.725 | 1.909 |
| Current smoker (yes vs. no*) | 0.115 | 0.012 | 0.768 | -0.647 | 0.876 |
| Any high-risk disease (yes vs. no*) | -0.652 | -0.052 | 0.189 | -1.626 | 0.322 |
| Marital status (Married vs. single*) | -0.899 | -0.072 | 0.129 | -2.062 | 0.263 |
| University degree (yes vs. no*) | -0.596 | -0.031 | 0.444 | -2.125 | 0.933 |
| Model 2: taking the knowledge of stroke post-test as the dependent variable | |||||
| Unstandardized Beta | Standardized Beta | p -value | Confidence interval | ||
| Lower Bound | Upper Bound | ||||
| Age in years (25–34) | -1.399 | -0.139 | 0.034 | -2.694 | -0.104 |
| Age in years (35–344) | -1.193 | -0.094 | 0.068 | -2.475 | 0.088 |
| Age in years (45–54) | -0.485 | -0.041 | 0.437 | -1.710 | 0.741 |
| Gender (female vs. male*) | -0.219 | -0.021 | 0.597 | -1.034 | 0.595 |
| History of stroke (yes vs. no*) | 0.778 | 0.022 | 0.569 | -1.900 | 3.456 |
| Family history of stroke (yes vs. no*) | 0.326 | 0.032 | 0.419 | -0.466 | 1.119 |
| Healthcare professional (yes vs. no*) | 0.879 | 0.071 | 0.078 | -0.100 | 1.859 |
| Alcohol (yes vs. no*) | 0.266 | 0.027 | 0.510 | -0.526 | 1.058 |
| Healthy lifestyle (yes vs. no*) | 0.052 | 0.004 | 0.924 | -1.026 | 1.130 |
| Current smoker (yes vs. no*) | -0.083 | -0.011 | 0.794 | -0.707 | 0.541 |
| Any high risk disease (yes vs. no*) | -1.031 | -0.104 | 0.011 | -1.828 | -0.234 |
| Marital status (Married vs. single*) | -0.119 | -0.012 | 0.807 | -1.070 | 0.833 |
| University degree (yes vs. no*) | -0.356 | -0.023 | 0.577 | -1.608 | 0.896 |
| Model 3: taking the difference between the knowledge of stroke pre and post session as the dependent variable. | |||||
| Unstandardized Beta | Standardized Beta | p -value | Confidence interval | ||
| Lower Bound | Upper Bound | ||||
| Age in years (25–34) | -0.651 | -0.065 | 0.304 | -1.893 | 0.591 |
| Age in years (35–344) | -0.794 | -0.063 | 0.206 | -2.025 | 0.437 |
| Age in years (45–54) | -0.274 | -0.023 | 0.646 | -1.445 | 0.897 |
| Gender (female vs. male*) | 0.126 | 0.012 | 0.750 | -0.650 | 0.901 |
| History of stroke (yes vs. no*) | -1.525 | -0.044 | 0.242 | -4.082 | 1.032 |
| Family history of stroke (yes vs. no*) | -1.424 | -0.139 | < 0.001 | -2.185 | -0.663 |
| Healthcare professional (yes vs. no*) | -2.475 | -0.200 | < 0.001 | -3.414 | -1.536 |
| Alcohol (yes vs. no*) | 0.050 | 0.005 | 0.897 | -0.709 | 0.810 |
| Healthy lifestyle (yes vs. no*) | -0.558 | -0.040 | 0.290 | -1.593 | 0.477 |
| Current smoker (yes vs. no*) | -0.569 | -0.055 | 0.151 | -1.345 | 0.207 |
| Any high risk disease (yes vs. no*) | -0.360 | -0.036 | 0.355 | -1.124 | 0.404 |
| Marital status (Married vs. single*) | 0.749 | 0.076 | 0.108 | -0.165 | 1.663 |
| University degree (yes vs. no*) | 0.154 | 0.010 | 0.803 | -1.055 | 1.363 |
Variables entered in the three models: gender, age, ever stroke, History of stroke, healthcare professional, smoking, alcohol, healthy lifestyle, medical illness, marital status and level of education
*Reference group
When taking the knowledge of stroke post-education, the results showed that being between 25 and 34 years (Beta=-1.39) and having any high-risk disease (Beta=-1.03) were significantly associated with a lower knowledge score (Table 4, Model 2).
A third linear regression analysis taking the difference between the knowledge of stroke pre- and post-education as the dependent variable showed that having a family history of stroke (Beta=-1.42) and being a healthcare professional (Beta=-2.47) were significantly associated with a lower difference in the knowledge score (Table 4, Model 3).
Discussion
Our study showed that a brief educational video could enhance the public’s knowledge about stroke risk factors, symptoms, and preventive measures within the Lebanese community.
A prior study in Lebanon indicated insufficient awareness of stroke risk factors and the importance of dialing 112 (the emergency number in Lebanon) when stroke symptoms occur, underscoring the need for health education programs to reduce stroke-related morbidity and mortality [15]. Educational videos have been recognized as efficient tools for a broad audience, with visual images offering advantages over verbal communication, including conveying additional information within a limited timeframe, simplifying complex ideas, illustrating dynamic concepts, and engaging and retaining the audience’s attention more efficiently [22]. For example, studies utilizing animated video formats for educational interventions have shown consistent improvements in short-term patient health outcomes [23]. Similarly, a systematic review in 2012 confirmed the value of video-based education in altering health behaviors, showing efficacy in promoting various health-related actions, including prostate cancer screening, sunscreen adherence, human immunodeficiency virus (HIV) testing, and treatment adherence [24]. The literature focusing on stroke knowledge and awareness has also demonstrated positive outcomes [25, 26].
In our study, the three-minute video employed persuasive techniques, images, and modeling to communicate essential information and influence participants’ health behavior. Participants exhibited a notable improvement in identifying stroke resulting from bleeding or an obstruction in blood flow to the brain. This improved awareness aligns with findings from previous studies conducted globally [27–29]. Furthermore, the ability to distinguish between a stroke and a heart attack is crucial, and our results contribute to reducing confusion between these two conditions, evident in the increased understanding of stroke’s definition after watching the educational video, especially recognizing that it occurs in the brain, not the heart.
Notably, participants demonstrated an enhanced understanding of diseases and lifestyle factors associated with an elevated risk of stroke. The pre-test revealed a lack of knowledge about risk factors, consistent with earlier research [29, 30]. However, post-education scores significantly increased, emphasizing the pivotal role of health education in expanding public awareness.
Improvements were also evident in participants’ recognition of stroke warning signs, particularly those emphasized by FAST (Facial, Arms, Speech, Time). Previous studies highlighted challenges in the community in detecting these signs [30, 31]. However, our results indicated increased awareness, with respondents expressing a willingness to promptly seek medical assistance and call an ambulance in the event of a stroke, both before and after the intervention, mirroring findings from other studies [27–29]. This consistency highlights the prevailing perception among the public that stroke is a life-threatening and urgent medical condition.
Family history of stroke emerged as a predictor of stroke knowledge, consistent with research in Nigeria, Morocco, and France, emphasizing the role of interpersonal relationships in disseminating medical information [32–34]. Traumatic experiences with close relatives may contribute to heightened awareness and understanding of stroke [35]. Moreover, older participants (aged 55+) had higher improvement in stroke knowledge, potentially influenced by a greater likelihood of comorbidities, motivating them to learn more about the condition.
Before watching the video, most respondents had a robust understanding of stroke prevention strategies, a comprehension that remained consistently high after the educational intervention. In contrast to earlier research findings, our sample displayed a superior level of optimal knowledge [36, 37]. This difference may be attributed to variations in the socioeconomic and sociodemographic characteristics of the participants, particularly the higher rate of formal education in our sample.
While a few studies have suggested a gender-based difference in stroke awareness and interest in health-related topics, with females exhibiting a higher level of understanding [38–40], our findings did not align with this specific trend.
Some studies have demonstrated that individuals who embrace healthy behaviors such as regular exercise [41] and maintaining a nutritious diet [42] tend to possess greater awareness of the warning signs, risk factors, and preventive measures associated with stroke. However, our findings did not provide evidence supporting this relationship.
Furthermore, our study revealed a deficiency in participants’ understanding of the optimal stroke treatment, validating similar findings in existing research [43, 44]. Previous studies on stroke awareness have predominantly focused on symptoms and risk factors, rather than adequate attention to treatment alternatives. Without knowledge about available treatments or the urgency of the situation, the recognition of symptoms alone is unlikely to prompt individuals to take swift action [45], hence the importance of time in public awareness campaigns when advocating for the best possible treatment approaches. Following the educational video, participants demonstrated an increased awareness of stroke treatment, reinforcing the idea that the visual and auditory elements inherent in video content provide a more immersive learning experience, enhancing the comprehension and retention of critical concepts related to stroke awareness and management. Combining visual representations of symptoms, emergency response procedures, and preventive measures created a comprehensive learning environment that caters to various learning styles. Moreover, the accessibility of videos such as the one used in this study across digital platforms ensures a broader reach, enabling wide dissemination of vital information to communities, thereby contributing significantly to the overall effort to enhance public awareness and preparedness for stroke and how to manage it.
Limitations and strengths
The study has several limitations that need to be acknowledged. The online survey could introduce selection bias as individuals with no internet access and those unfamiliar with technology would be excluded. Consequently, an overestimation of the knowledge results is likely as less privileged populations may have had a lower chance of inclusion. In addition, a large proportion of participants were healthcare professionals (19.7%), who may possess higher baseline knowledge compared to the general public, thus limiting the possibility of representing the broader Lebanese population.
The questionnaire employed in the study consisted of closed-ended questions, which could lead to an overestimation of stroke knowledge among respondents. Participants self-reported their characteristics and responses, which could contribute to non-differential information bias. We also relied on participants’ honesty in following the instructions to view the educational video in its entirety and to complete the survey in the correct order. Moreover, the platform used did not have mechanisms to enforce these steps, which may introduce bias in the data collection process. Furthermore, the study did not measure the long-term effects of the educational intervention. Larger-scale prospective studies would be required to evaluate this outcome. Nonetheless, our study used of a meticulously validated questionnaire to ensure the reliability and validity of our data collection and represents the first attempt to assess the effectiveness of an educational video in improving stroke knowledge in Lebanon potentially saving lives.
Conclusion
This study demonstrated the effectiveness of a video-based educational tool to raise awareness about stroke. Short, targeted audio-visual resources using lay language can convey health education messages and influence behavioral changes. The community can benefit from a large-scale educational campaign that targets different socio-economic statuses to enhance knowledge of stroke and save lives.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Abbreviations
- AHA/ASA
American Heart Association/American Stroke Association
- LMICs
Low- and Middle-Income Countries
- SPSS
Statistical Package for the Social Sciences
- ANOVA
Analysis of Variance
- HIV
Human Immunodeficiency Virus
Author contributions
M.C obtained funding. M.C, K.I and P.S developed the research question and contributed to the study design and analysis plan. M.C, K.I, P.S developed the educational video and piloted the questionnaire. S.Y, T.A, Y.S collected the data. J.S, F.S, H.S, H.H contributed to literature review. C.H performed the statistical analyses. C.H and K.I validated the questionnaire. J.S, K.I, H.S, H.H, F.S, S.Y, T.A, Y.S drafted the manuscript. All authors critically revised the manuscript, gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Funding
This research received an internal grant from the Office of Research and Sponsored Programs at Abu Dhabi University.
Data availability
All data generated or analysed during this study are included in this published article and its supplementary information files. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The Institutional Review Board at Abu Dhabi University gave approval to conduct this study (CoHS-22-05-00018.16/May/2022), and informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sakr F, Dabbous M, Akel M, Salameh P, Hosseini H. Adherence to Post-stroke Pharmacotherapy: Scale Validation and correlates among a sample of stroke survivors. Medicina. 2022;58:1109. 10.3390/medicina58081109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wj P, Aa R, Om TA, Nc A et al. B, K B, 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018;49. 10.1161/STR.0000000000000158
- 3.Machaalani M, Fakhry B, Zwaideh M, Mendelek K, Mahmoud N, Hammoud T, et al. Knowledge, attitude, and practice toward Cardiovascular diseases in the Lebanese Population. Global Heart. 2022;17. 10.5334/gh.1138 [DOI] [PMC free article] [PubMed]
- 4.Schwamm LH, Pancioli A, Acker JE, Goldstein LB, Zorowitz RD, Shephard TJ, et al. Recommendations for the establishment of Stroke systems of Care. Stroke. 2005;36:690–703. 10.1161/01.STR.0000158165.42884.4F [DOI] [PubMed] [Google Scholar]
- 5.Lo SHS, Chang AM, Chau JPC. Study protocol: a randomised controlled trial of a nurse-led community-based self-management programme for improving recovery among community-residing stroke survivors. BMC Health Serv Res. 2016;16:387. 10.1186/s12913-016-1642-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feigin VL, Roth GA, Naghavi M, Parmar P, Krishnamurthi R, Chugh S, et al. Global burden of stroke and risk factors in 188 countries, during 1990–2013: a systematic analysis for the global burden of Disease Study 2013. Lancet Neurol. 2016;15:913–24. 10.1016/S1474-4422(16)30073-4 [DOI] [PubMed] [Google Scholar]
- 7.Kim YS, Park S-S, Bae H-J, Heo JH, Kwon SU, Lee B-C, et al. Public awareness of stroke in Korea. Stroke. 2012;43:1146–9. 10.1161/STROKEAHA.111.638460 [DOI] [PubMed] [Google Scholar]
- 8.Rosamond WD, Folsom AR, Chambless LE, Wang C-H, McGovern PG, Howard G, et al. Stroke incidence and survival among Middle-aged adults. Stroke. 1999;30:736–43. 10.1161/01.STR.30.4.736 [DOI] [PubMed] [Google Scholar]
- 9.O’Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376:112–23. 10.1016/S0140-6736(10)60834-3 [DOI] [PubMed] [Google Scholar]
- 10.Kleindorfer D, Khoury J, Broderick JP, Rademacher E, Woo D, Flaherty ML, et al. Temporal Trends Public Aware Stroke Stroke. 2009;40:2502–6. 10.1161/STROKEAHA.109.551861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sposito J, Zipf A, Alhowaymel F, Tala Almutairi M, Breda K. Community-based stroke Recognition Education and Response: an evidence-based intervention project. Creat Nurs. 2018;24:251–7. 10.1891/1078-4535.24.4.251 [DOI] [PubMed] [Google Scholar]
- 12.Sakr F, Dabbous M, Akel M, Salameh P, Hosseini H. Construction and validation of the 17-Item stroke-specific quality of Life Scale (SS-QOL-17): a Comprehensive Short Scale to assess the functional, psychosocial, and therapeutic factors of QOL among Stroke survivors. Int J Environ Res Public Health. 2022;19:15668. 10.3390/ijerph192315668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abdo R, Abboud H, Salameh P, El Hajj T, Hosseini H. Mortality and predictors of death poststroke: data from a Multicenter prospective cohort of Lebanese stroke patients. J Stroke Cerebrovasc Dis. 2019;28:859–68. 10.1016/j.jstrokecerebrovasdis.2018.11.033 [DOI] [PubMed] [Google Scholar]
- 14.Khalil HM, Lahoud N. Knowledge of stroke warning signs, risk factors, and response to stroke among Lebanese older adults in Beirut. J Stroke Cerebrovasc Dis 2020;29. 10.1016/j.jstrokecerebrovasdis.2020.104716 [DOI] [PubMed]
- 15.Saade S, Hallit S, Salameh P, Hosseini H. Knowledge and response to stroke among Lebanese adults: a Population-based survey. Front Public Health. 2022;10. 10.3389/fpubh.2022.891073 [DOI] [PMC free article] [PubMed]
- 16.Lally M, Valentine-French S. Emerging and early adulthood. Parenting and family diversity issues. Iowa State University Digital; 2020. 10.31274/isudp.8
- 17.World Health Organization. WHODAS 2.0 Translation Guidelines 2011. https://terrance.who.int/mediacentre/data/WHODAS/Guidelines/WHODAS 2.0 Translation guidelines.pdf
- 18.Fukunaga A, Inoue Y, Chandraratne N, Yamaguchi M, Kuwahara K, Indrawansa S, et al. Healthy lifestyle index and its association with hypertension among community adults in Sri Lanka: a cross-sectional study. PLoS ONE. 2020;15:e0226773. 10.1371/journal.pone.0226773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hu P, Zheng M, Huang J, Fan H-Y, Fan C-J, Ruan H-H, et al. Effect of healthy lifestyle index and lifestyle patterns on the risk of mortality: a community-based cohort study. Front Med. 2022;9:920760. 10.3389/fmed.2022.920760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peila R, Xue X, Qi Q, Dannenberg AJ, Allison MA, Johnson KC, et al. Healthy Lifestyle Index and Risk of Cardiovascular Disease among Postmenopausal Women with Normal Body Mass Index. J Am Heart Association. 2023;12:e029111. 10.1161/JAHA.122.029111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meer R, van de Pol J, van den Brandt PA, Schouten LJ. The association of healthy lifestyle index score and the risk of renal cell cancer in the Netherlands cohort study. BMC Cancer. 2023;23:156. 10.1186/s12885-023-10627-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hurtubise L, Martin B, Gilliland A, Mahan J. To play or not to play: leveraging video in Medical Education. J Graduate Med Educ. 2013;5:13. 10.4300/JGME-05-01-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dahodwala M, Geransar R, Babion J, de Grood J, Sargious P. The impact of the use of video-based educational interventions on patient outcomes in hospital settings: a scoping review. Patient Educ Couns. 2018;101:2116–24. 10.1016/j.pec.2018.06.018 [DOI] [PubMed] [Google Scholar]
- 24.Tuong W, Larsen ER, Armstrong AW. Videos to influence: a systematic review of effectiveness of video-based education in modifying health behaviors. J Behav Med. 2014;37:218–33. 10.1007/s10865-012-9480-7 [DOI] [PubMed] [Google Scholar]
- 25.Chan Y-F, Lavery R, Fox N, Kwon R, Zinzuwadia S, Massone R, et al. Effect of an Educational Video on Emergency Department patient stroke knowledge. J Emerg Med. 2008;34:215–20. 10.1016/j.jemermed.2007.04.003 [DOI] [PubMed] [Google Scholar]
- 26.Albalawi MF, Shaqran T, Alhawiti SH, Alwadiee AS, Albalawi YM, Albalawi WH. Effect of an educational intervention on knowledge and perception of individuals at risk for stroke in Tabuk, Saudi Arabia. Neurosciences J. 2020;25:18–24. 10.17712/nsj.2020.1.20190018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hickey A, Holly D, McGee H, Conroy R, Shelley E. Knowledge of stroke risk factors and warning signs in Ireland: development and application of the stroke awareness questionnaire (SAQ). Int J Stroke. 2012;7:298–306. 10.1111/j.1747-4949.2011.00698.x [DOI] [PubMed] [Google Scholar]
- 28.Ayanniyi O, Akande O, Mustapha A. Knowledge and perception of stroke among adults in Osogbo, Nigeria. Afr J Med Med Sci 2006;35. [PubMed]
- 29.Pandian JD, Jaison A, Deepak SS, Kalra G, Shamsher S, Lincoln DJ, et al. Public Awareness of Warning Symptoms, risk factors, and treatment of stroke in Northwest India. Stroke. 2005;36:644–8. 10.1161/01.STR.0000154876.08468.a0 [DOI] [PubMed] [Google Scholar]
- 30.Kamran S, Bener AB, Deleu D, Khoja W, Jumma M, Al Shubali A, et al. The level of awareness of stroke risk factors and symptoms in the Gulf Cooperation Council countries: Gulf Cooperation Council stroke awareness study. Neuroepidemiology. 2008;29:235–42. 10.1159/000112856 [DOI] [PubMed] [Google Scholar]
- 31.Sungbun S, Tangkawanich T, Thanakumma O, Pitchayakoon N, Srichote W. A community-based participatory approach to increase public knowledge of stroke among ethnic minorities in the northern mountains of Thailand: 10.55131/jphd/2022/200201. J Public Health Dev. 2022;20:1–11. 10.55131/jphd/2022/200201 [Google Scholar]
- 32.Wahab KW, Kayode OO, Musa OI. Knowledge of stroke risk factors among nigerians at High Risk. J Stroke Cerebrovasc Dis. 2015;24:125–9. 10.1016/j.jstrokecerebrovasdis.2014.07.053 [DOI] [PubMed] [Google Scholar]
- 33.Kharbach A, Obtel M, Achbani A, Bouchriti Y, Hassouni K, Lahlou L, et al. Level of knowledge on Stroke and Associated factors: a cross-sectional study at primary. Health Care Centers Morocco. 2020;86:83. 10.5334/aogh.2885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Derex L, Adeleine P, Nighoghossian N, Honnorat J, Trouillas P. Évaluation Du Niveau D’information concernant l’accident vasculaire cérébral des patients admis dans une unité neurovasculaire française. Rev Neurol. 2004;160:331–7. 10.1016/S0035-3787(04)70908-X [DOI] [PubMed] [Google Scholar]
- 35.Sadeghi-Hokmabadi E, Vahdati SS, Rikhtegar R, Ghasempour K, Rezabakhsh A. Public knowledge of people visiting Imam Reza hospital regarding stroke symptoms and risk factors. BMC Emerg Med. 2019;19:36. 10.1186/s12873-019-0250-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tibebu NS, Emiru TD, Tiruneh CM, Nigat AB, Abate MW, Demelash AT. Knowledge on Prevention of Stroke and its Associated factors among hypertensive patients at Debre Tabor General Hospital: an Institution-based cross-sectional study. Risk Manage Healthc Policy. 2021;14:1681–8. 10.2147/RMHP.S303876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Arisegi SA, Awosan KJ, Oche MO, Sabir AA, Ibrahim MT. Knowledge and practices related to stroke prevention among hypertensive and diabetic patients attending specialist hospital, Sokoto, Nigeria. The Pan African Medical Journal 2018;29. 10.11604/pamj.2018.29.63.13252 [DOI] [PMC free article] [PubMed]
- 38.Sug Yoon S, Heller RF, Levi C, Wiggers J, Fitzgerald PE. Knowledge of stroke risk factors, warning symptoms, and treatment among an Australian Urban Population. Stroke. 2001;32:1926–30. 10.1161/01.STR.32.8.1926 [DOI] [PubMed] [Google Scholar]
- 39.Ramírez-Moreno JM, Alonso-González R, Peral-Pacheco D, Millán-Núñez MV, Aguirre-Sánchez JJ. Knowledge of stroke a study from a sex perspective. BMC Res Notes. 2015;8:604. 10.1186/s13104-015-1582-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stroebele N, Müller-Riemenschneider F, Nolte CH, Müller-Nordhorn J, Bockelbrink A, Willich SN. Knowledge of risk factors, and warning signs of stroke: a systematic review from a gender perspective. Int J Stroke. 2011;6:60–6. 10.1111/j.1747-4949.2010.00540.x [DOI] [PubMed] [Google Scholar]
- 41.Woldetsadik FK, Kassa T, Bilchut WH, Kibret AK, Guadie YG, Eriku GA. Stroke related knowledge, Prevention practices and Associated factors among hypertensive patients at University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia, 2021. Frontiers in Neurology 2022;13. 10.3389/fneur.2022.839879 [DOI] [PMC free article] [PubMed]
- 42.Wong WP, Yeung M, Loh S, Lee M, Ghazali F, Chan C, et al. Stroke-related knowledge, lifestyle behaviours and health beliefs in Singaporean Chinese: implications for health education. Health Educ J. 2013;72:386–97. 10.1177/0017896912446554 [Google Scholar]
- 43.Baldereschi M, Di Carlo A, Vaccaro C, Polizzi B, Inzitari D, The Promotion Implementation of Stroke Care in Italy Project Working Group. Stroke Knowl Italy Neurol Sci. 2015;36:415–21. 10.1007/s10072-014-1964-5 [DOI] [PubMed] [Google Scholar]
- 44.Faiz KW, Sundseth A, Thommessen B, Rønning OM. Patient knowledge on stroke risk factors, symptoms and treatment options. VHRM. 2018;14:37–40. 10.2147/VHRM.S152173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Herpich F, Rincon F. Management of Acute ischemic stroke. Crit Care Med. 2020;48:1654. 10.1097/CCM.0000000000004597 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article and its supplementary information files. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.