Abstract
Background
Hemophagocytic lymphohistiocytosis (HLH) is characterized by immune dysregulation that results in an uncontrolled hyperinflammatory state. HLH is classified into two main categories: primary (familial) HLH and secondary (acquired) HLH. Secondary HLH can result from various underlying, including infection-associated hemophagocytic syndrome (IAHS) and macrophage activation syndrome (MAS) associated with rheumatologic disorders, among others. Epstein–Barr virus (EBV) often causes IAHS, but central nervous system (CNS) involvement is rare among systemic lupus erythematosus (SLE) patients. We report a case of EBV encephalitis associated with HLH in a patient with childhood-onset SLE.
Case presentation
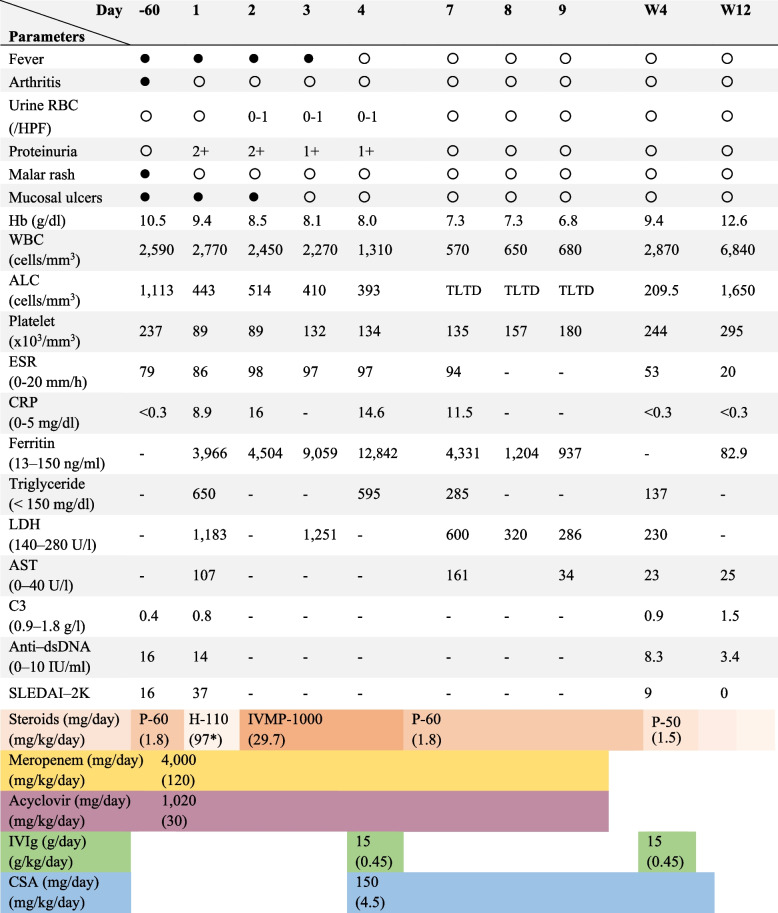
A 12-year-old girl had received a diagnosis of SLE 2 months before presentation. After a period of inactive disease on treatment, fever and seizures, with altered mental status and hallucinations, developed over several weeks. A complete blood cell count (CBC) revealed pancytopenia, accompanied by elevated levels of inflammatory markers: 86 mm/hr erythrocyte sedimentation rate, 8.9 mg/dl c-reactive protein, and 3,966 ng/mL of ferritin. The differential diagnosis included active neuropsychiatric SLE, CNS infection and neurological manifestations in secondary HLH, which could have represented either IAHS or MAS. Meropenem and acyclovir were initially administered for clinical acute encephalitis, followed by pulse methylprednisolone; however, the fever persisted, and another CBC revealed progressive cytopenia. A bone marrow study showed hypocellularity and active hemophagocytic activity, and intravenous immunoglobulin was additionally given due to the diagnosis of HLH. Cerebrospinal fluid (CSF) analysis showed 60/mm3 white blood cells (N 55%, L 45%), 141 mg/dL glucose (0.7 blood-CSF glucose ratio), < 4 mg/dL protein; results of Gram stain and bacterial culture were negative. The viral encephalitis panel from the CSF confirmed EBV infection. Bone marrow immunohistochemistry examination revealed increasing levels of CD8 + T-cell and equivocal positive results for EBV-encoded RNA in situ hybridization; therefore, HLH potentially associated with EBV was diagnosed. After treatment with IVIg, cyclosporin A, and prednisolone, the patient’s symptoms gradually improved and she was eventually able to return to school.
Conclusions
Our case highlights the importance of a thorough differential diagnosis, including EBV encephalitis associated with HLH, in patients with childhood SLE, particularly in cases of clinical deterioration occurs after initial treatment.
Keywords: EBV, Encephalitis, Hemophagocytic lymphohistiocytosis, Pediatric, Systemic lupus erythematosus
Background
Hemophagocytic lymphohistiocytosis (HLH) is characterized by immune dysregulation that results in an uncontrolled hyperinflammatory state [1, 2]. It has two main categories: primary HLH, which includes cases associated with genetic mutations and primary immune deficiencies, and secondary (acquired) HLH [1–3]. Secondary HLH can be triggered by a range of underlying conditions, including infection-associated hemophagocytic syndrome (IAHS), malignancy-associated HLH, HLH associated with rheumatologic diseases–most commonly systemic juvenile idiopathic arthritis and systemic lupus erythematosus (SLE), referred to as macrophage activation syndrome (MAS)–as well as HLH linked to immunodeficiency, and HLH of unknown origin [1, 2, 4–7].
Extensive studies of IAHS in various cohorts have revealed that the Epstein–Barr virus (EBV) is the pathogen most commonly associated with IAHS [8, 9]. In immunocompetent children, EBV infection classically is asymptomatic or manifests with characteristics of infectious mononucleosis such as fever, fatigue, cervical lymphadenopathy and upper respiratory tract symptoms [10]. A minority of EBV-infected children may exhibit neurological manifestations of encephalitis, meningitis, Guillain-Barré syndrome, and acute demyelinating encephalomyelitis, which commonly occur in immunocompromised children [10, 11]. Despite being the most common virus-associated IAHS and causing significant mortality [12], the pathogenesis of EBV-associated disease of the central nervous system (CNS) remains incompletely understood [13]. Three main mechanisms have been proposed: direct invasion of the CNS by EBV, immune-mediated mechanisms, and reactivation of EBV infection, which typically occurs in immunosuppressed hosts [11, 14]. Therefore, in patients with EBV infection in the CNS caused by different mechanisms, non-CNS symptoms may not appear, which poses challenges for diagnosis.
SLE itself may involve immune dysregulation; this is compounded by treatment with immunosuppressive agents, which thereby increases the risk of infection in patients with SLE. However, EBV encephalitis is infrequently reported even in adult-onset SLE [15]. To raise awareness of an unusual condition, we report a case in which a patient with SLE exhibited clinical signs of neuropsychiatric involvement. This scenario highlights the importance of including potential origins of neurological involvement in the differential diagnosis.
Case presentation
A 12-year-old girl had been diagnosed with childhood-onset SLE, presenting with fever, malar rash, arthritis in both wrists, painless oral ulcer, leukopenia, and hypocomplementemia (Fig. 1). Of note, there were no renal or neurological abnormalities at the time of diagnosis. Initial immunological investigation revealed positive antinuclear antibodies (1:1280 speckled pattern) and anti-double-stranded DNA antibodies (anti–dsDNA) (16 IU/ml), while the other autoantibodies were unknown. She was treated by a general pediatrician at another hospital with prednisolone (60 mg; 1.8 mg/kg/day) and hydroxychloroquine (5 mg/kg/day), and the disease was clinically inactive, as indicated by a modified Systemic Lupus Erythematosus Disease Activity Index 2000 [16, 17] (SLEDAI-2 K) score of zero. Over the next several weeks, she developed progressive altered mental status, visual, and auditory hallucinations, low-grade fever, and was referred to our hospital with generalized tonic seizure. Physical examination revealed a temperature of 39ºC, blood pressure of 97/62 mmHg, and a pulse rate of 130/minute. Her level of consciousness fluctuated during the day; she exhibited confusion about time, place and person. She had a painless oral ulcer and a modestly palpable liver (span of 10 cm) and spleen. Neurological examination revealed normal deep tendon reflexes, no cranial nerve involvement, and no neck stiffness. Other findings were unremarkable (e.g., neither cervical lymphadenopathy nor exudative tonsils).
Fig. 1.
Clinical course and laboratory parameter of the patient
Laboratory investigation revealed an erythrocyte sedimentation rate of 86 mm/hour (normal: 0–20 mm/hour), c-reactive protein (CRP) level of 8.9 mg/dL (normal: 0–5 mg/dL), creatinine level of 0.42 mg/dL, blood urea nitrogen level of 10 mg/dL, aspartate aminotransferase level of 107 U/L (normal: 0–40 U/L), globulin level of 3.7 g/dL, and albumin level of 3.3 g/dL. A complete blood cell count revealed pancytopenia with hemoglobin levels of 9 g/dL, a white blood cell count of 2,770 cells/mm3 (absolute neutrophil count, 800/mm3; absolute lymphocyte count, 443/mm3), and a platelet count of 89,000 cells/mm3. Urinalysis revealed albuminuria (2 + albumin) with negative red blood cell and white blood cell, and significant proteinuria (urine protein–creatinine ratio of 3.8). Levels of complements and immunological markers appeared abnormal: 0.8 g/L of C3 (normal: 0.9–1.8 g/L), 34 mg/dL of C4 (normal: 10–40 mg/dL), and 14 IU/mL anti–dsDNA antibody (normal: 0–10 IU/mL). Autoantibody profile revealed positive for anti-nRNP (3 +), anti-Sm (3 +), anti-SS-A (3 +), anti-Ro-52 (3 +), and anti-SS-B (3 +), while tests for anti-Scl-70, anti-Jo-1, anti-CENP, anti-nucleosome, and anti-histone were negative. Her SLEDAI-2 K score significantly rose to 37. The differential diagnosis included acute encephalitis, neuropsychiatric SLE, thrombotic microangiopathy, antiphospholipid syndrome and neurological involvement in secondary HLH such as IAHS or MAS. Meropenem and acyclovir were initiated for the treatment of acute encephalitis and systemic corticosteroids was switch to hydrocortisone (100 mg/m2/day) due to concerns regarding the ongoing infectious process.
Cranial magnetic resonance imaging (MRI) and magnetic resonance angiography revealed ill-defined patchy hyperintense lesions in the parasagittal region of the right parietal lobe and the right high parietal lobe, without contrast enhancement, suggestive of focal encephalitis. There was no evidence of thromboembolism, infarction, or bleeding in the brain. Lumbar puncture was later performed, and the cerebrospinal fluid analysis (CSF) revealed a white blood cell count of 60/mm3 (55% neutrophils, 45% lymphocytes), a glucose level of 141 mg/dL (blood–CSF glucose ratio of 0.7), and a protein level of < 4 mg/dL. CSF cytologic analysis revealed no any hemophagocytic histiocytes or macrophages and latex agglutination tests for bacteria, including Streptococcus pneumoniae, Neisseria meningitidis, Streptococcus agalactiae and Hemophilus influenzae type b, yielded negative results, as did a Gram stain and bacterial culture of CSF. Oligoclonal band testing, which could indicate intrathecal immunoglobulin synthesis (e.g. multiple sclerosis or demyelinating diseases) [18] and has been reported in CNS-HLH [19, 20], was not performed due to unavailability.
Additional laboratory tests were obtained out of concern for HLH because of the unremitting fever, hepatosplenomegaly and cytopenia. The findings were of significant elevations in ferritin (3,966 ng/mL; normal: 13–150 ng/mL), lactate dehydrogenase (1,183 U/L; normal: 140–280 U/L), and fasting triglyceride levels (850 mg/dL; normal: < 150 mg/dL). Tests for natural killer cell activity, soluble CD25 levels, and molecular diagnosis tests for familial HLH were unavailable in our center. After no bacterial pathogens were identified in blood, urine, and CSF within the first 24 h and further investigation suggested the diagnosis of HLH (IAHS or MAS), the systemic corticosteroids regimen subsequently intensified into pulse intravenous methylprednisolone 1,000 mg (29.7 mg/kg/day).
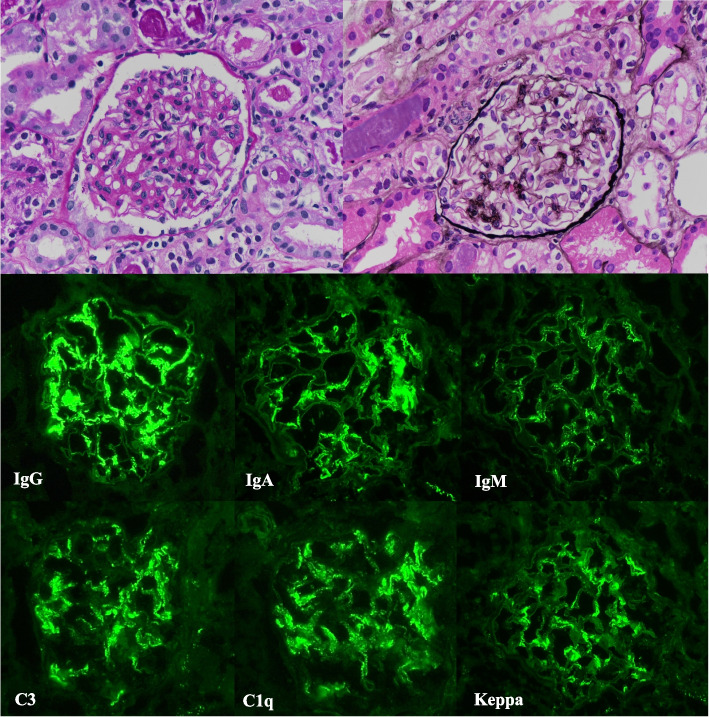
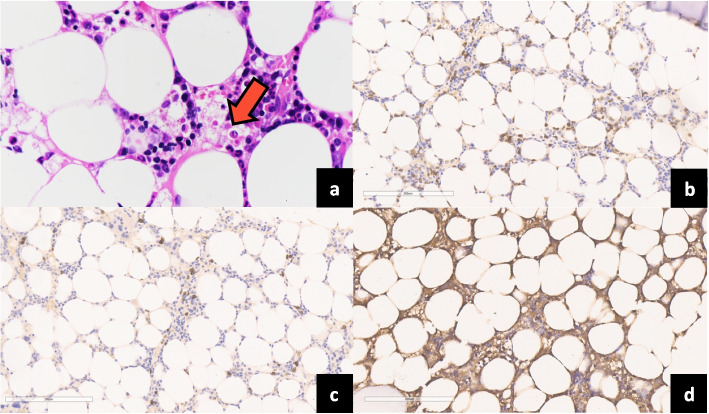
Despite this initial aggressive treatment (meropenem, acyclovir, pulse intravenous methylprednisolone), the fever and altered mental status persisted; laboratory tests revealed ongoing cytopenia and hyperferritinemia, other possible causes, such as thrombotic microangiopathy, and secondary HLH, such as IAHS, were suspected. Renal biopsy revealed mesangial hypercellularity that was compatible with lupus nephritis class II without evidence of thrombosis (Fig. 2), together with a normal serum level of ADAMTS-13 (154.6 U/dL; normal: 73–164 U/dL). Bone marrow aspiration revealed actively hemophagocytic histiocytes (Fig. 3) but no evidence of bacteria, which led to the diagnosis of HLH (6/8) by HLH-2004 criteria [21], or of MAS [22], which was possibly secondary to active SLE [22]. Additionally, our patient ‘s HScore of 276 further indicated a > 99% probability of HLH [23]. In accordance with the intensified protocol of HLH-2004, cyclosporin A was administered alongside supportive therapy, including intravenous immunoglobulin (0.5 g/kg every 4 weeks) and cotrimoxazole prophylaxis. [21, 24]. Etoposide was omitted because of severe cytopenia during treatment.
Fig. 2.
Renal pathological study. Immunofluorescence revealed mild mesangial hypercellularity and granular pattern staining in the mesangial area, which were compatible with a diagnosis of lupus nephritis class II. (Periodic acid–Schiff stain; original magnification, 400 .) No subepithelial deposition was evident. (Silver stain; original magnification, 400 )
Fig. 3.
The examination of bone marrow revealed evident histiocytes with hemophagocytic activity (Hematoxylin and eosin stain; original magnification, 40 ) (a), as were increased numbers of CD8+ T cells with modest cytological atypia (b). CD20.+ B cells (c) and positive Epstein–Barr virus–encoded RNA in situ hybridization were rare (d). (Hematoxylin and eosin stain, immunohistochemistry stain; original magnification, 20 )
The results of tests for anti-ribosomal P, anti–N–methyl–d–aspartate receptor (Anti–NMDAR), antimyelin–oligodendrocyte glycoprotein antibody (Anti–MOG) and antiphospholipid antibodies (APLs), which included anti–β2 glycoprotein 1 immunoglobulin (Ig) G, anticardiolipin IgG, and lupus anticoagulant, were negative. The viral encephalitis panel from CSF—which included human herpesviruses types 1, 2, 6, and 7; varicella-zoster virus; EBV; cytomegalovirus; human enterovirus; human adenovirus; parvovirus B19, and human parechovirus—was subjected to polymerase chain reaction (PCR), which yielded a result positive for EBV DNA. The qualitative EBV viral load in both serum and CSF were within the limits of detection (210–10,000,000 IU/mL). Tests for IgM and IgG to serum viral capsid antigen and Epstein–Barr nuclear antigen were unfortunately not available.
The diagnosis of HLH, whether caused by hyperinflammatory states in active SLE or EBV infection, was challenging. To assess the bone marrow histopathologically, immunohistochemistry studies and EBV-encoded RNA in situ hybridization (EBER-ISH) were performed. The EBER-ISH results were equivocal positive, thereby decreasing the likelihood of SLE as the primary cause of secondary HLH and indicating that EBV infection is the more probable trigger. Immunohistochemistry further demonstrated an increased presence of CD8+ T cells, wherein CD4+ T cells, indicating EBV reactivation, and CD20+ B cells were exceptionally rare. These results suggested the presence of EBV in the patient’s bone marrow, supporting a potential link between acute EBV infection and the development of secondary HLH in our case [25]. During treatment with meropenem, acyclovir, IVIg, systemic corticosteroids, and cyclosporin A, her state of consciousness improved, as did laboratory parameters (Fig. 1). Four weeks after beginning treatment, she had no fever, seizures, or hallucinations. The prednisolone dosage was tapered down, and her SLEDAI-2 K score gradually decreased.
Discussion
The association between EBV encephalitis in SLE is infrequently reported; the diagnosis is a multifaceted clinical challenge that necessitates comprehensive investigation into infectious and immune dysregulation mechanisms. In the case of our 12-year-old patient with childhood-onset SLE who presented with fever, seizures, and altered consciousness, thorough investigation led to the diagnosis of HLH potentially related to EBV encephalitis. The patient responded well to treatment, with improvement in neurological symptoms.
Neurological symptoms such as headaches, seizures, weakness, psychosis and cognitive impairment could be manifestations of neuropsychiatric SLE, which occurs in 13.5%–34.6% of cases of childhood-onset SLE [26–28]. Many of these symptoms overlap with those of CNS infections or with neurological manifestations in SLE complications such as MAS, APS and thrombotic microangiopathy [29–32]; this poses diagnostic challenges and necessitates tailored management strategies. Recent comprehensive studies of clinical manifestations and laboratory findings have revealed distinctions between CNS infections and neuropsychiatric SLE [29, 30]; for example, high-grade fever (> 39ºC) is more common, disease duration is longer and high-dose corticosteroids are used more often in patients with CNS infection [29, 30]. In our patient, the disease lasted more than 2 months, and high-dose prednisolone (60 mg/day) was part of treatment. Therefore, an infectious case should be given more consideration.
The prevalence of abnormal CRP levels, hypoalbuminemia and, in CSF, decreased glucose level and increased protein levels [29, 30] was also more prevalent among patients with CNS infection disease. Although CSF protein levels were higher in this population [29, 30], the pathogens identified included bacteria, mycobacteria, and parasites; only 3.4% of cases were attributed to viruses, including EBV and herpesvirus, which might explain the viral pattern observed in the CSF of those patients [29]. Moreover, according to the results from a pediatric encephalitis registry in Canada, the CSF protein level was normal in patients with virus-associated encephalitis, which is consistent with our case [33]. To date, CSF neopterin and interferon alpha levels have been identified as potential biomarkers for neuropsychiatric SLE [34], although the availability of testing is limited in our setting.
EBV encephalitis has been reported in immunocompromised patients [10, 11], but the pathogenesis of EBV-associated CNS disease remains incompletely understood [13]. Proposed mechanisms include direct viral invasion, immune-mediated infection and reactivation of latent infection, wherein viral reactivation via infected B cells leads to neurological infection, particularly in immunocompromised patients [10, 35]. Antibodies to EBV that are produced in the nerve sheath contribute to viral reactivation in the CNS, mainly in immunosuppressed states, for which serological assays may be unhelpful as a result of dysfunction in antibody production [13, 36]. Diagnosis is therefore determined by the detection of EBV nucleic acid by PCR in CSF [37, 38]. Furthermore, patients with EBV infection produce antineuronal antibodies against myelin–oligodendrocyte glycoprotein (anti–MOG antibodies), whose protein structure is similar to that of EBV [39, 40]. Therefore, the immune system potentially contributes to CNS symptoms, and in some patients, detection of the EBV genome in CSF may not be feasible [41]. Conversely, EBV was detected by PCR in brain autopsies in a large EBV encephalitis cohort, which further implicates direct infection of the CNS by EBV [33]. As a result, EBV infection in the CNS may be present even in the absence of typical symptoms of infectious mononucleosis, such as lymphadenopathy, hepatosplenomegaly and upper respiratory tract symptoms. The proposed mechanism of EBV infection in our patient could have been direct EBV invasion of the CNS, which would account for her acutely altered mental state, lack of typical symptoms of infectious mononucleosis, abnormal brain MRI findings, and EBV detection by PCR in CSF without hemophagocytic histiocytes or macrophages in CSF cytology. Immunohistopathological evidence was supported EBV-associated HLH, indicated by increased CD8+ T cells infiltration with equivocal positive EBER-ISH results in bone marrow and negative anti-MOG results [25]. EBV infection of the CNS might be present in patients without clinical signs of infectious mononucleosis, as observed in our patient and in accordance with the report by Doja et al., who found that 95.2% of the patients with EBV encephalitis lacked symptoms of infectious mononucleosis [33].
Rare cases of SLE with EBV encephalitis are listed in Table 1. Hongbo et al. described a 21-year-old man with headache, seizures and depression in whom adult-onset SLE and EBV encephalitis were eventually diagnosed and responded well to immunosuppressive agents and antiviral treatment with ganciclovir [15]. With regard to the greater severity and frequency of neurological involvement in childhood-onset SLE [42, 43], Brogna et al. described a 7-year-old boy with EBV encephalitis without HLH features before neuropsychiatric SLE developed, which suggests that EBV reactivation is a potential trigger of neuropsychiatric SLE [44]. In the case reported by Hongbo et al., prolonged disease duration and high-dose prednisolone administration may have induced an immunosuppressive state, which was conducive to EBV infection as in our patient. Because the clinical neurological manifestations of neuropsychiatric SLE and CNS infection are similar, differentiating between the two could be challenging. Autoantibodies such as antiribosomal P, antiNMDAR and APLs have been implicated in neuropsychiatric SLE, although study findings have been variable [27, 45], and in our patients, results of all autoantibody tests were negative. Moreover, the detection of EBV by PCR in CSF and the increasing numbers of CD8+ T cells with equivocal positive EBER-ISH results in bone marrow corroborated the diagnosis of EBV encephalitis associated HLH in our patient.
Table 1.
Summary of published cases of EBV encephalitis in SLE patients
| Case 1 | Case 2 | Our case | |
|---|---|---|---|
| Country, Y | China, 2012 | Italy, 2016 | Thailand, 2024 |
| Age | 21 years | 7 years | 12 years |
| Sex | Male | Male | Female |
| Onset from diagnosis | 34 days | Prior SLE diagnosed | 60 days |
| Symptoms | Seizure | Dystonia | Seizure |
| Headache | Psychiatric | Psychosis | |
| Hypertension | symptom | Fever | |
| Fever | Seizure | ||
| Investigation | |||
| Blood | |||
| WBC (cells/mm3) | n/a | - | 2,770 |
| ALC (cells/mm3) | n/a | - | 443 |
| Platelet (cells/mm3) | n/a | - | 89,000 |
| CRP (mg/L) | n/a | - | 8.9 |
| ESR (mm/h) | 36 | - | 86 |
| Albumin (g/dl) | 2.6 | n/a | 3.3 |
| EBV DNA | + | EBNA + | - |
| EBV IgM | + | VCA IgM- | n/a |
| EBV IgG | n/a | VCA IgG + | n/a |
| Anti-dsDNA (IU/mL) | + | - | 14 |
| Anti-ribosomal P | n/a | n/a | - |
| APLs | ACL- | - | - |
| Anti-NMDAR | n/a | n/a | - |
| C3 | Low | - | Low |
| C4 | Low | - | Normal |
| CSF | |||
| WBC | n/a | 10 (L100%) | 60 (N 55%, L45%) |
| RBC | n/a | - | - |
| CSF/serum glucose ratio | n/a | - | 0.7 |
| Protein | n/a | - | < 4 |
| EBV DNA | n/a | + | + |
| EBV IgM | + | n/a | n/a |
| EBV IgG | + | n/a | n/a |
| Treatment | MP | IVIg | IVIg |
| Ganciclovir | MP | MP | |
| AED | Acyclovir | Acyclovir | |
| AED | Meropenem | ||
| Risperidone | CSA | ||
| AED | |||
| Outcome | Complete recovery | Complete recovery | Complete recovery |
Abbreviations: ACL Anticardiolipin antibody, AED Anti–epileptic drug, ALC Absolute lymphocyte count, Anti–dsDNA Anti–double-stranded deoxyribonucleic acid, Anti–NMDAR anti–N–methyl–d–aspartate receptor, APLs Antiphospholipid antibodies, CRP C-reactive protein, CSA Cyclosporin A, CSF Cerebrospinal fluid, DNA Deoxyribonucleic acid, EBNA Epstein–Barr virus nuclear antigen, EBV Epstein–Barr virus, ESR Erythrocyte sedimentation rate, Ig Immunoglobulin, IVIg Intravenous immunoglobulin, L Lymphocyte, MP Methylprednisolone, N Neutrophile, n/a Not available, RBC Red blood cell, SLE Systemic Lupus Erythematosus, VCA Viral capsid antigen, W Week, WBC White blood cell, Y Year
The treatment of HLH typically involves a multi-faceted approach that includes systemic corticosteroids, immunosuppressive agents (cyclosporin A, etoposide), and, in certain cases, rituximab [21, 46]. Rituximab, a monoclonal antibody targeting CD20 on B cells, may be beneficial in cases of HLH associated with EBV [46]. A study involving 42 patients with EBV-associated HLH who received a rituximab containing regimen showed promising results: 43% of patients experienced clinical improvement in symptoms such as fever and hepatosplenomegaly, with a statistically significant 3.7-fold decrease in viral load and serum ferritin [47]. However, another study by Meng GQ found that among patients with EBV-infected T and NK cells associated HLH, rituximab did not lead to a significant decline in EBV DNA [48]. Given that our patient’s bone marrow study revealed a predominance of CD8 + T cells with a low number of CD20 + B cells, suggesting limited potential benefit from rituximab. Furthermore, the patient’s clinical and laboratory parameters improved with the current treatment regimen, making the initiation of rituximab unnecessary. Therefore, based on the clinical response and the bone marrow findings, we did not proceed with rituximab therapy.
As far as we are aware, our patient represents the first reported case of EBV encephalitis associated HLH in childhood-onset SLE. Because her symptoms were multisystemic, indicative of potentially active neuropsychiatric SLE (SLEDAI-2 K score of 37) or infection, she was given antibiotics, antiviral medications and pulse intravenous methylprednisolone; however, she responded only partially to this treatment. The increase in serum CRP level (which is not commonly observed in patients with active SLE [49]) and the presence of hyperferritinemia indicated the possibility of either infection or HLH [30].
Conclusion
In both EBV encephalitis associated HLH [12] and MAS in active SLE, neurological symptoms are reported, and potentially life-threatening manifestations may develop. The majority of cases of MAS and active SLE respond to immunosuppressive agents [50]; in our patient, however, despite comprehensive investigation and monitoring, was refractory to treatment, including pulse intravenous methylprednisolone. This suggests other possibilities of neurological symptoms can occur in childhood-onset SLE. Recognizing secondary HLH, not limited to EBV encephalitis associated HLH, is crucial for optimal management and improving patient outcome.
Acknowledgements
We sincerely acknowledge Professor Kulkanya Chokephaibulkit for her invaluable expertise and insightful suggestions, which greatly enhanced the quality of our manuscript.
Abbreviations
- Anti–dsDNA
Anti–double–stranded deoxyribonucleic acid
- Anti-MOG
Anti–myelin-oligodendrocyte glycoprotein
- Anti–NMDAR
Anti–N–methyl–d–aspartate receptor
- APLs
Antiphospholipid antibodies
- CNS
Central nervous system
- CRP
C-reactive protein
- CSF
Cerebrospinal fluid
- EBER-ISH
Epstein–Barr virus–encoded RNA in situ hybridization
- EBV
Epstein–Barr virus
- HLH
Hemophagocytic lymphohistiocytosis
- IAHS
Infection-associated hemophagocytic syndrome
- Ig
Immunoglobulin
- MAS
Macrophage activation syndrome
- MRI
Magnetic resonance imaging
- PCR
Polymerase chain reaction
- SLE
Systemic lupus erythematosus
- SLEDAI-2K
Systemic Lupus Erythematosus Disease Activity Index 2000
Authors’ contributions
KC, TK, and ST contributed to conception, data acquisition, and manuscript preparation. KC and TK contributed equally to this paper and are designated as co-first authors. ST drafted the manuscript, prepared the figures and tables, reviewed and critically revised the manuscript. All histopathology reported were prepared and approved by NP and CC. All authors provided patient care, reviewed and approved the final version of this manuscript.
Funding
The Navamindradhiraj University Research Fund provided funding for language editing in this study.
Data availability
The data is included within the article.
Declarations
Ethics approval and consent to participate
This study was reviewed and approved by the Institutional Review Board, Faculty of Medicine Vajira Hospital. (COE no. 007/2022X).
Consent for publication
Written informed consent to participate in this study was obtained from the patient’s legal guardian/next of kin for publication.
Competing interests
All authors declare no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Krit Cheawcharnpraparn and Thiraporn Kanjanaphan are co-first authors and equally contributed to the manuscript.
Contributor Information
Thiraporn Kanjanaphan, Email: Thiraporn@nmu.ac.th.
Sirikarn Tangcheewinsirikul, Email: sirikarn.t@nmu.ac.th.
References
- 1.George MR. Hemophagocytic lymphohistiocytosis: review of etiologies and management. J Blood Med. 2014;5:69–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Janka GE. Familial and acquired hemophagocytic lymphohistiocytosis. Annu Rev Med. 2012;63:233–46. [DOI] [PubMed] [Google Scholar]
- 3.Faitelson Y, Grunebaum E. Hemophagocytic lymphohistiocytosis and primary immune deficiency disorders. Clin Immunol. 2014;155(1):118–25. [DOI] [PubMed] [Google Scholar]
- 4.Lin CI, Yu HH, Lee JH, Wang LC, Lin YT, Yang YH, et al. Clinical analysis of macrophage activation syndrome in pediatric patients with autoimmune diseases. Clin Rheumatol. 2012;31(8):1223–30. [DOI] [PubMed] [Google Scholar]
- 5.Minoia F, Davi S, Horne A, Demirkaya E, Bovis F, Li C, et al. Clinical features, treatment, and outcome of macrophage activation syndrome complicating systemic juvenile idiopathic arthritis: a multinational, multicenter study of 362 patients. Arthritis Rheumatol. 2014;66(11):3160–9. [DOI] [PubMed] [Google Scholar]
- 6.Aytac S, Batu ED, Unal S, Bilginer Y, Cetin M, Tuncer M, et al. Macrophage activation syndrome in children with systemic juvenile idiopathic arthritis and systemic lupus erythematosus. Rheumatol Int. 2016;36(10):1421–9. [DOI] [PubMed] [Google Scholar]
- 7.Canna SW, Marsh RA. Pediatric hemophagocytic lymphohistiocytosis. Blood. 2020;135(16):1332–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu XJ, Wang HS, Ju XL, Xiao PF, Xiao Y, Xue HM, Shi HY, Gao YJ, Jia GC, Li XR, Zhao WH, Wang NL, Tang YM; Histiocytosis Study Group of the Chinese Pediatric Society. Clinical presentation and outcome of pediatric patients with hemophagocytic lymphohistiocytosis in China: A retrospective multicenter study. Pediatr Blood Cancer. 2017;64(4). 10.1002/pbc.26264. [DOI] [PubMed]
- 9.Harnchoowong S, Soponkanaporn S, Vilaiyuk S, Lerkvaleekul B, Pakakasama S. Central nervous system involvement and thrombocytopenia as predictors of mortality in children with hemophagocytic lymphohistiocytosis. Front Pediatr. 2022;10: 941318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheng H, Chen D, Peng X, Wu P, Jiang L, Hu Y. Clinical characteristics of Epstein-Barr virus infection in the pediatric nervous system. BMC Infect Dis. 2020;20(1):886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martelius T, Lappalainen M, Palomaki M, Anttila VJ. Clinical characteristics of patients with Epstein Barr virus in cerebrospinal fluid. BMC Infect Dis. 2011;11: 281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oguz MM, Sahin G, Altinel Acoglu E, Polat E, Yucel H, Oztek Celebi FZ, et al. Secondary hemophagocytic lymphohistiocytosis in pediatric patients: a single center experience and factors that influenced patient prognosis. Pediatr Hematol Oncol. 2019;36(1):1–16. [DOI] [PubMed] [Google Scholar]
- 13.Volpi A. Epstein-Barr virus and human herpesvirus type 8 infections of the central nervous system. Herpes. 2004;11(Suppl 2):120A-A127. [PubMed] [Google Scholar]
- 14.Weinberg A, Li S, Palmer M, Tyler KL. Quantitative CSF PCR in Epstein-Barr virus infections of the central nervous system. Ann Neurol. 2002;52(5):543–8. [DOI] [PubMed] [Google Scholar]
- 15.Hongbo C, Hongzhen M, Lingzhi H, Maosheng X, Mei C. Secondary neuropsychiatric manifestations caused by Epstein-Barr virus encephalitis in a new onset systemic lupus erythematosus patient. Rheumatol Int. 2012;32(8):2321–3. [DOI] [PubMed] [Google Scholar]
- 16.Gladman DD, Ibanez D, Urowitz MB. Systemic lupus erythematosus disease activity index 2000. J Rheumatol. 2002;29(2):288–91. [PubMed] [Google Scholar]
- 17.Uribe AG, Vila LM, McGwin G Jr, Sanchez ML, Reveille JD, Alarcon GS. The systemic lupus activity measure-revised, the Mexican Systemic Lupus Erythematosus Disease Activity Index (SLEDAI), and a modified SLEDAI-2K are adequate instruments to measure disease activity in systemic lupus erythematosus. J Rheumatol. 2004;31(10):1934–40. [PubMed] [Google Scholar]
- 18.Nikolopoulos D, Kitsos D, Papathanasiou M, Kapsala N, Garantziotis P, Pieta A, et al. Demyelinating syndromes in systemic lupus erythematosus: data from the “Attikon” Lupus Cohort. Front Neurol. 2022;13: 889613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pastula DM, Burish M, Reis GF, Bollen A, Cha S, Ralph J, et al. Adult-onset central nervous system hemophagocytic lymphohistiocytosis: a case report. BMC Neurol. 2015;15:203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Benson LA, Li H, Henderson LA, Solomon IH, Soldatos A, Murphy J, et al. Pediatric CNS-isolated hemophagocytic lymphohistiocytosis. Neurol Neuroimmunol Neuroinflamm. 2019;6(3): e560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Henter JI, Horne A, Arico M, Egeler RM, Filipovich AH, Imashuku S, et al. HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48(2):124–31. [DOI] [PubMed] [Google Scholar]
- 22.Parodi A, Davi S, Pringe AB, Pistorio A, Ruperto N, Magni-Manzoni S, et al. Macrophage activation syndrome in juvenile systemic lupus erythematosus: a multinational multicenter study of thirty-eight patients. Arthritis Rheum. 2009;60(11):3388–99. [DOI] [PubMed] [Google Scholar]
- 23.Fardet L, Galicier L, Lambotte O, Marzac C, Aumont C, Chahwan D, et al. Development and validation of the HScore, a score for the diagnosis of reactive hemophagocytic syndrome. Arthritis Rheumatol. 2014;66(9):2613–20. [DOI] [PubMed] [Google Scholar]
- 24.Imashuku S, Morimoto A, Ishii E. Virus-triggered secondary hemophagocytic lymphohistiocytosis. Acta Paediatr. 2021;110(10):2729–36. [DOI] [PubMed] [Google Scholar]
- 25.El-Mallawany NK, Curry CV, Allen CE. Haemophagocytic lymphohistiocytosis and Epstein-Barr virus: a complex relationship with diverse origins, expression and outcomes. Br J Haematol. 2022;196(1):31–44. [DOI] [PubMed] [Google Scholar]
- 26.Yu HH, Lee JH, Wang LC, Yang YH, Chiang BL. Neuropsychiatric manifestations in pediatric systemic lupus erythematosus: a 20-year study. Lupus. 2006;15(10):651–7. [DOI] [PubMed] [Google Scholar]
- 27.Schwartz N, Stock AD, Putterman C. Neuropsychiatric lupus: new mechanistic insights and future treatment directions. Nat Rev Rheumatol. 2019;15(3):137–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kisaarslan AP, Cicek SO, Batu ED, Sahin S, Gurgoze MK, Cetinkaya SB, et al. Neuropsychiatric involvement in juvenile-onset systemic lupus erythematosus: a multicenter study. Joint Bone Spine. 2023;90(4): 105559. [DOI] [PubMed] [Google Scholar]
- 29.Jiang M, Shi X, Gao X, Niu J, Hu X, Zhao L, et al. Clinical features of central nervous system infections and experience in differential diagnosis from neuropsychiatric lupus erythematosus in a cohort of 8491 patients with systemic lupus erythematosus. Arthritis Res Ther. 2019;21(1):189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fang H, Lan L, Qu Y, Zhang Q, Lv J. Differences between central nervous system infection and neuropsychiatric systemic lupus erythematosus in patients with systemic lupus erythematosus. J Int Med Res. 2018;46(1):485–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Borgia RE, Gerstein M, Levy DM, Silverman ED, Hiraki LT. Features, treatment, and outcomes of macrophage activation syndrome in childhood-onset systemic lupus erythematosus. Arthritis Rheumatol. 2018;70(4):616–24. [DOI] [PubMed] [Google Scholar]
- 32.Giani T, Smith EM, Al-Abadi E, Armon K, Bailey K, Ciurtin C, et al. Neuropsychiatric involvement in juvenile-onset systemic lupus erythematosus: Data from the UK Juvenile-onset systemic lupus erythematosus cohort study. Lupus. 2021;30(12):1955–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Doja A, Bitnun A, Ford Jones EL, Richardson S, Tellier R, Petric M, et al. Pediatric Epstein-Barr virus-associated encephalitis: 10-year review. J Child Neurol. 2006;21(5):384–91. [DOI] [PubMed] [Google Scholar]
- 34.Labouret M, Costi S, Bondet V, Trebossen V, Le Roux E, Ntorkou A, et al. Juvenile Neuropsychiatric Systemic Lupus Erythematosus: Identification of Novel Central Neuroinflammation Biomarkers. J Clin Immunol. 2023;43(3):615–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee GH, Kim J, Kim HW, Cho JW. Clinical significance of Epstein-Barr virus in the cerebrospinal fluid of immunocompetent patients. Clin Neurol Neurosurg. 2021;202: 106507. [DOI] [PubMed] [Google Scholar]
- 36.Obel N, Hoier-Madsen M, Kangro H. Serological and clinical findings in patients with serological evidence of reactivated Epstein-Barr virus infection. APMIS. 1996;104(6):424–8. [DOI] [PubMed] [Google Scholar]
- 37.Tselis A, Duman R, Storch GA, Lisak RP. Epstein-Barr virus encephalomyelitis diagnosed by polymerase chain reaction: detection of the genome in the CSF. Neurology. 1997;48(5):1351–5. [DOI] [PubMed] [Google Scholar]
- 38.Steiner I, Budka H, Chaudhuri A, Koskiniemi M, Sainio K, Salonen O, et al. Viral meningoencephalitis: a review of diagnostic methods and guidelines for management. Eur J Neurol. 2010;17(8):999-e957. [DOI] [PubMed] [Google Scholar]
- 39.Lang HL, Jacobsen H, Ikemizu S, Andersson C, Harlos K, Madsen L, et al. A functional and structural basis for TCR cross-reactivity in multiple sclerosis. Nat Immunol. 2002;3(10):940–3. [DOI] [PubMed] [Google Scholar]
- 40.Wang H, Munger KL, Reindl M, O’Reilly EJ, Levin LI, Berger T, et al. Myelin oligodendrocyte glycoprotein antibodies and multiple sclerosis in healthy young adults. Neurology. 2008;71(15):1142–6. [DOI] [PubMed] [Google Scholar]
- 41.Nakamura Y, Nakajima H, Tani H, Hosokawa T, Ishida S, Kimura F, et al. Anti-MOG antibody-positive ADEM following infectious mononucleosis due to a primary EBV infection: a case report. BMC Neurol. 2017;17(1):76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sousa S, Goncalves MJ, Ines LS, Eugenio G, Jesus D, Fernandes S, et al. Clinical features and long-term outcomes of systemic lupus erythematosus: comparative data of childhood, adult and late-onset disease in a national register. Rheumatol Int. 2016;36(7):955–60. [DOI] [PubMed] [Google Scholar]
- 43.Torrente-Segarra V, Salman Monte TC, Rua-Figueroa I, Sanchez-Alonso F, Lopez-Longo FJ, Galindo-Izquierdo M, et al. Juvenile- and adult-onset systemic lupus erythematosus: a comparative study in a large cohort from the Spanish Society of Rheumatology Lupus Registry (RELESSER). Clin Exp Rheumatol. 2017;35(6):1047–55. [PubMed] [Google Scholar]
- 44.Brogna C, Manna R, Contaldo I, Romeo DM, Stefanini MC, Chiaretti A, et al. Intravenous immunoglobulin for Pediatric Neuropsychiatric Lupus Triggered by Epstein-Barr Virus Cerebral Infection. Isr Med Assoc J. 2016;18(12):763–6. [PubMed] [Google Scholar]
- 45.Ho RC, Thiaghu C, Ong H, Lu Y, Ho CS, Tam WW, et al. A meta-analysis of serum and cerebrospinal fluid autoantibodies in neuropsychiatric systemic lupus erythematosus. Autoimmun Rev. 2016;15(2):124–38. [DOI] [PubMed] [Google Scholar]
- 46.Qureshi Z, Altaf F, Jamil A, Siddique R. Rituximab as a therapeutic strategy in hemophagocytic lymphohistiocytosis: efficacy, outcomes, and survival-insights from a systematic review. Am J Clin Oncol. 2024;47:498–508. [DOI] [PubMed] [Google Scholar]
- 47.Chellapandian D, Das R, Zelley K, Wiener SJ, Zhao H, Teachey DT, et al. Treatment of Epstein Barr virus-induced haemophagocytic lymphohistiocytosis with rituximab-containing chemo-immunotherapeutic regimens. Br J Haematol. 2013;162(3):376–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Meng GQ, Wang JS, Wang YN, Wei N, Wang Z. Rituximab-containing immuno-chemotherapy regimens are effective for the elimination of EBV for EBV-HLH with only and mainly B lymphocytes of EBV infection. Int Immunopharmacol. 2021;96: 107606. [DOI] [PubMed] [Google Scholar]
- 49.Aringer M. Inflammatory markers in systemic lupus erythematosus. J Autoimmun. 2020;110: 102374. [DOI] [PubMed] [Google Scholar]
- 50.Liu AC, Yang Y, Li MT, Jia Y, Chen S, Ye S, et al. Macrophage activation syndrome in systemic lupus erythematosus: a multicenter, case-control study in China. Clin Rheumatol. 2018;37(1):93–100. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data is included within the article.