Abstract
Background:
Previous systematic reviews have reported the incidence of anterior knee pain (AKP) and extension deficit (ED) after anterior cruciate ligament reconstruction (ACLR); however, both outcomes are estimated separately and thus are assumed to be uncorrelated.
Purpose:
To estimate whether there is a clinically relevant association between the population effects of ED and AKP after ACLR.
Study Design:
Systematic review; Level of evidence, 2.
Methods:
Under PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, a systematic review was conducted by searching PubMed, EMBASE, and the Cochrane Library electronic databases for published articles reporting incidence of both AKP and ED after ACLR with either bone–patellar tendon–bone (BPTB) or hamstring (HS) graft that returned 298 studies after the initial search. A Bayesian hierarchical measurement error model estimated the population effect of ED and AKP.
Results:
Twelve publications involving 976 patients (mean follow-up, 77.9 months; range, 24-180 months) were included in the systematic review. There was a clear, moderate correlation between population ED and population AKP for the BPTB (r = 0.40; 95% CI, 0.39-0.42) and the HS grafts (r = 0.35; 95% CI, 0.33-0.36). Model expected estimates for the population effects of AKP and ED were 24.1% (95% CI, 17.4%-31.9%) and 17.5% (95% CI, 10.6%-25.0%), respectively, for the BPTB graft and 16.1% (95% CI, 9.2%-23.9%) and 13.1% ED (95% CI, 6.0%-20.8%) for the HS graft, respectively. The posterior mean difference in AKP between BPTB and HS grafts was clear and substantial (8.3% [95% CI, 0.3% to 16.1%]); there was no substantial difference in the posterior mean difference of ED between BPTB and HS grafts (4.3% [95% CI, –3.8% to 13.0%).
Conclusion:
Our systematic review demonstrated a moderate but clear correlation between ED and AKP irrespective of graft type. From a clinical perspective, this association emphasizes the need for intraoperative achievement of full extension and avoidance of situations that may cause ED. The higher incidence of AKP in patients with BPTB graft may also be attributed to factors related to the graft harvest site. Future metaregression analyses could investigate whether additional factors such as follow-up duration or rehabilitation protocols can moderate the association between AKP and ED after ACLR with either BPTB or HS graft.
Keywords: ACL, knee, patellar tendon, autograft, patellar tendon, Bayesian modeling
Graft selection in patients undergoing anterior cruciate ligament (ACL) reconstruction (ACLR) is a very important decision and is part of a long-lasting debate in the scientific community because it is a factor that influences a successful outcome of the ACLR in terms of donor-site morbidity,6,12 rerupture,24,27,37,52 infection rate,35,39 functional deficits,2,7,8 and patient-reported outcome measures.19,38,47 The most common grafts are the patellar tendon either as the central third or as the medial third, the hamstring (HS) tendon graft as a 4-strand graft or as a quadrupled semitendinosus graft, and in recent years the quadriceps tendon graft. 3 Each one of these grafts has its advantages and disadvantages in incorporation and function as a graft, but these grafts also are associated with anatomic and functional defects that influence the final outcome and the patient's quality of life and activities. 35
The most successful scenario would be that the defect heals with similar tissue and that the recovery is completed without any functional alterations caused by the harvested graft. The healing of the patellar tendon or HS tendon defect has been investigated with magnetic resonance imaging and ultrasonography studies,13,36,46 and the potential functional deficits have been investigated using electrophysiology or dynamometry or other biomechanical methods together with clinical examination tests such as anterior knee pain (AKP), kneeling pain, knee walking, or numbness in the incision site.4,14,22,30,31,43
AKP after ACLR is often cited as a major reason for avoiding the use of a bone–patellar tendon–bone (BPTB) graft, despite its many well-documented advantages.14,19,51 However, previous research indicated that AKP is primarily caused by extension deficit (ED) after ACLR.44,45 Therefore, Shelbourne and Trumper45 proposed regaining full extension intraoperatively as well as postoperatively, introducing an accelerated rehabilitation protocol to regain and retain full movement of the knee joint, especially full extension or hyperextension compared with the contralateral healthy side. 45 The multifactorial nature of AKP, rather than that related specifically to BPTB graft selection, is further demonstrated by its prevalence, albeit at a lesser degree, in ACLR using HS tendon graft.19,51
Previous systematic reviews have compared BPTB versus HS grafts in terms of AKP and ED as well as other objective clinical and patient-reported outcomes.7,8,19,35,47,49,51 However, in all these studies, both outcomes are reported independently and no previous study has estimated whether there is a clinically relevant association between the population effects of ED and AKP. 18 Thus, the aim of the present study was to estimate the association between ED and AKP after ACLR with either BPTB or HS graft.
Methods
Literature Search
The present systematic review was conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines using a checklist. We conducted an extensive search of studies published between 1990 and August 2022 in PubMed, EMBASE, and the Cochrane Library electronic databases. We utilized the search strategy proposed by Cochrane, and our search key terms included “ACL,”“anterior cruciate ligament,”“reconstructive surgical procedures,”“patellar tendon,”“hamstring,”“gracilis,”“semitendinosus,”“autologous, ”and “long term” in various combinations. The full text was reviewed if the abstract indicated that the article might be a prospective cohort study (PCS) of ACLR with BPTB versus HS tendon autografts. A manual search was also conducted by reviewing the references of the articles derived by the electronic search to identify potential additional studies.
Study Selection
Inclusion criteria for study selection were as follows: (1) a randomized controlled trial (RCT) or a PCS (level of evidence 1 or 2); (2) patients having undergone primary ACLR for a unilateral ACL rupture; (3) BPTB autografts compared with HS tendon autografts for ACLR; (4) follow-up of ≥2 years; and (5) reporting assessment of both AKP and ED. Exclusion criteria were as follows: case-control study, retrospective cohort study, or case series; follow-up of <2 years; graft other than BPTB and HS; follow-up studies with the same patients from the same center performing the same technique; non-English language articles; and in vitro, animal, or cadaveric studies.
Data Extraction
Data were extracted independently from each eligible study by 2 review authors (J.D.G. and K.P.) using a standard Excel spreadsheet (Microsoft). Any discrepancies between the extracted data were resolved by consensus. Where required, the corresponding authors were contacted for additional data. The primary outcomes extracted were percentages of AKP and ED along with their standard errors per graft type and study. In addition, the following data were extracted from all eligible studies: first author and year of publication, study design, number of patients, duration of follow-up, loss at follow-up, type of graft fixation.
Methodological Quality
The methodological quality of each eligible study was independently assessed by 2 review authors (J.D.G. and K.P.) using the Jadad scale for RCTs and the Newcastle-Ottawa Scale (NOS) for PCSs. 49 A quality score of ≥3 from the Jadad scale was considered to indicate a high-quality RCT and a score of ≥7 on the 9-point NOS indicated high-quality PCS. 49
Statistical Analysis
We employed a Bayesian hierarchical measurement error model. 5 Within the Bayesian framework, the true outcomes of the different studies follow their own distribution. 21 This distribution of true effects has a mean (the “population” true effect that is being estimated) and a variance, representing the between-study variability. 18 Bayesian methods allow direct modeling of the uncertainty in the estimate of the between-study variability, can be superior in estimating pooled effects (especially when the number of included studies is small), and produce full posterior distributions of any model effect. 21 Our analyses were carried out in the R programming language using the wrapper package brms interfaced with Stan to perform sampling. 5 Our model included outcome, graft type, their interaction to estimate the population effects of AKP and ED for BPTB and HS grafts, and a random intercept for study identification to estimate the between-study variability. Weakly informative priors were used in order to exert minimal effect on the data.5,21 The model also permitted an estimation of the correlation coefficient between the population effects of AKP and ED. 5 The magnitude of the correlation was evaluated as trivial (>0.1), small (>0.2), moderate (0.3-0.5), large (>0.5), very large (>0.7). 9 We sampled the posterior distribution using Hamiltonian Monte Carlo with 4 chains and 2500 post–warm up samples per chain. The model passed all diagnostic statistics (all Rhat values <1.01, all effective sample sizes >400, 0 divergent iterations). 21 We evaluated the robustness of our model by conducting a sensitivity analysis via excluding 1 study in each round and evaluating the influence of any single study on the estimates of model effects. 18 We also considered 2 additional models: 1 with the addition of study design (RCT vs PCS) as a categorical predictor and 1 with the addition of follow-up (≤5 years vs ≥6 years) as a categorical predictor. Each of these models was compared with the initial model via leave-one-out cross-validation. 5 Neither of these additional models outperformed the initial simpler model; thus, the initial model was retained.
Results
Study Inclusion
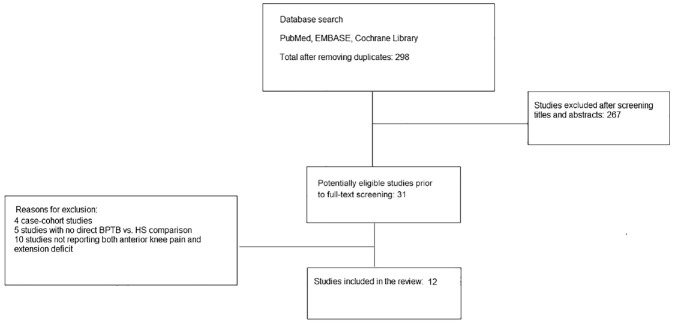
An initial literature search of PubMed, EMBASE, and the Cochrane Library yielded a total of 789 articles. All duplicate publications were excluded for a total of 298 unique articles. According to our exclusion criteria, 267 articles were removed, and the remaining 31 abstracts were further screened by reviewing the full-text article. Nineteen articles were further excluded: 4 case-cohort studies (level of evidence, 3), 5 having no direct comparison of BPTB versus HS ACLR outcomes, and 10 not reporting data on both AKP and ED. Thus, there were 12 publications that fulfilled all criteria and were subsequently included in this systematic review (Figure 1). ‖
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart. BPTB, bone–patellar tendon–bone; HS, hamstring.
Methodological Quality
Sample size ranged from 50 to 126 patients (mean, 81 patients). Clinical follow-up was reported in all 12 studies, with follow-up rates ranging from 72% to 100%. All 4 PCSs1,20,26,40 were of high quality as judged by the NOS scale, whereas 1 out of 8 RCTs 15 was deemed of high quality according to the Jadad scale (Table 1). All studies had a minimum of 2 years of follow-up data. Follow-up ranged from 24 to 180 months (mean, 77.9 months).
Table 1.
Characteristics of the Included Trials a
| Author/Year | Design | Number of Patients | Lost to Follow-up, n | BPTB Graft Fixation | HS Graft Fixation | Quality Rating | ||
|---|---|---|---|---|---|---|---|---|
| Femoral | Tibial | Femoral | Tibial | |||||
| Ibrahim et al, 2005 20 | PCS | 110 | 25 | EB | ISc | EB | Sc+W/Pl+Sc+St | 9 b |
| Laxdal et al, 2005 25 | RCT | 79 | 9 | ISc | ISc | ISc | ISc | 2 |
| Liden et al, 2007 28 | RCT | 71 | 3 | ISc | ISc | ISc | ISc | 2 |
| Matsumoto et al, 2006 33 | RCT | 80 | 8 | ISc | ISc | ISc | ISc | 1 |
| Zaffagnini et al, 2006 50 | RCT | 50 | 0 | ISc | ISc | EB | Sc | 2 |
| Webster et al, 2016 48 | RCT | 65 | 18 | EB | ISc | EB | P+W | 2 |
| Sajovic et al, 2011 41 | RCT | 64 | 2 | ISc | Sc | ISc | Sc | 1 |
| Aglietti et al, 1994 1 | PCS | 63 | 3 | Sc+W | ISc+Sc+W | Sc+W | Sc+W | 8 b |
| Laxdal et al, 2007 26 | PCS | 126 | 3 | ISc | ISc | ISc | ISc | 9 b |
| Sadoghi et al, 2011 40 | PCS | 92 | 0 | CP | ISc | EB | ISc | 8 b |
| Gifstad et al, 2013 15 | RCT | 114 | 12 | ISc | ISc | Sc+WL | Sc+WL | 3 c |
| Konrads al, 2016 23 | RCT | 62 | 15 | ISc | ISc | EB | Su | 2 |
BPTB, bone–patellar tendon–bone; CP, cross-pin; EB, Endobutton; HS, hamstring; ISc, interference screw; P, post; PCS, prospective cohort study; Pl, plate; RCT, randomized controlled trial; Sc, screw; St, staple; Su, suture; W, washer; WL, washerlock.
High-quality PCS based on the Newcastle-Ottawa Scale rating.
High-quality RCT based on the Jadad Scale rating.
Characteristics of Included Studies and Review Findings
Table 1 presents the fixation techniques used for each graft for the tibial and femoral tunnels. For BPTB grafts, nearly all studies used interference screw fixation for the tibial bone plugs while the femoral bone plugs were a little more variable (8 studies used interference screw fixation, 2 used Endobutton (Smith+Nephew), 1 used screw plus washer, and 1 used cross-pins). Femoral tunnels on HS fixation relied on interference screws or Endobutton in a total of 10 studies. On the contrary, tibial HS fixation was quite variable and included interference screws in 5 studies, and screw, washer/plate, screws plus staple, screws plus washerlock and sutures in the rest of the studies. AKP and ED ranged from 5% to 51% and 0% to 38%, respectively, for BPTB grafts; and 3% to 30% and 0% to 28%, respectively, for HS grafts (Table 2).
Table 2.
Reported Incident of Anterior Knee Pain and Extension Deficit per Graft Type a
| Author/Year | Follow-up, mo (range) | BPTB | HS | ||
|---|---|---|---|---|---|
| AKP | ED | AKP | ED | ||
| Ibrahim et al, 2005 20 | 81 (60-96) | 25 | 35 | 6.7 | 17.8 |
| Laxdal et al, 2005 25 | 26 (20-36) | 29 | 5 | 34 | 16 |
| Liden et al, 2007 28 | 86 (68-114) | 39 | 26 | 23 | 21 |
| Matsumoto et al, 2006 33 | 80 (56-111) | 5.4 | 2.9 | 10.8 | 5.7 |
| Zaffagnini et al, 2006 50 | 60 (not reported) | 36 | 20 | 12 | 25 |
| Webster et al, 2016 48 | 184 (168-204) | 38 | 0 | 27 | 0 |
| Sajovic et al, 2011 41 | 132 (not reported) | 48 | 0 | 29.6 | 0 |
| Aglietti al, 1994 1 | 28 (22-39) | 13.3 | 0 | 10 | 0 |
| Laxdal al, 2007 26 | 25 (24-35) | 22.2 | 37.8 | 24.4 | 28.2 |
| Sadoghi al, 2011 40 | 26 (24-32) | 51.2 | 9.8 | 25.5 | 9.8 |
| Gifstad al, 2013 15 | 84 (63-94) | 9.8 | 14.6 | 2.8 | 25 |
| Konrads al, 2016 23 | 120 (not reported) | 20.8 | 4.2 | 4.3 | 0 |
Values are presented as percentages unless otherwise noted. AKP, anterior knee pain; BPTB, bone–patellar tendon–bone; ED, extension deficit; HS, hamstring.
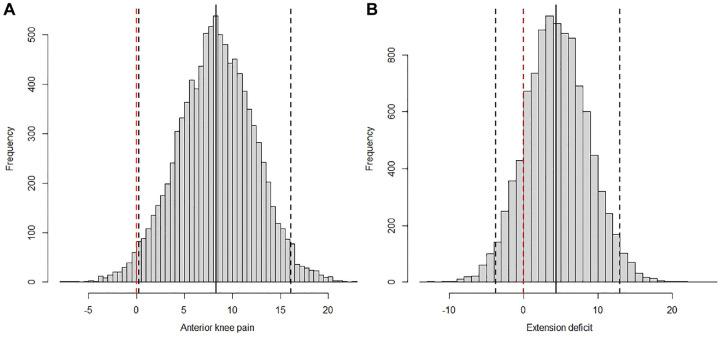
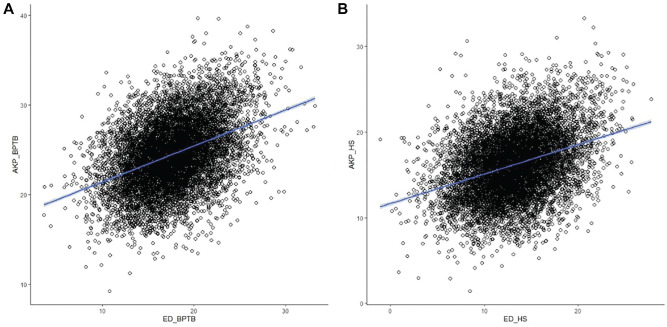
According to our model, the population effect of AKP was 24.1% on average (with a 95% CI of 17.4%-31.9%) and the population effect of ED was 17.5% on average (with a 95% CI of 10.6%-25.0%) for BPTB grafts; the population effect of AKP was 16.1% on average (with a 95% CI of 9.2%-23.9%) and the population effect of ED was 13.1% on average (with a 95% CI of 6.0%-20.8%) for the HS grafts (Figure 2).There was a clear and substantial difference in the population effect of AKP between BPTB and HS grafts. The posterior mean difference was 8.3% (95% CI, 0.3% to 16.1%) and there was 98% probability that this difference was >0 (Figure 3A). There was no substantial difference in the population effect of ED between BPTB and HS grafts. The posterior mean difference was 4.3% (95% CI, –3.8% to 13.0%), and there was only an 86% probability that this difference was >0 (Figure 3A). There was a clear, moderate correlation between the population effects of AKP and ED for either the BPTB (r = 0.40; 95% CI, 0.39-0.42) (Figure 4A) or the HS (r = 0.35; 95% CI, 0.33-0.36) graft (Figure 4B). The results of our series of sensitivity analyses showed that there was not any particularly influential study among all selected studies.
Figure 2.
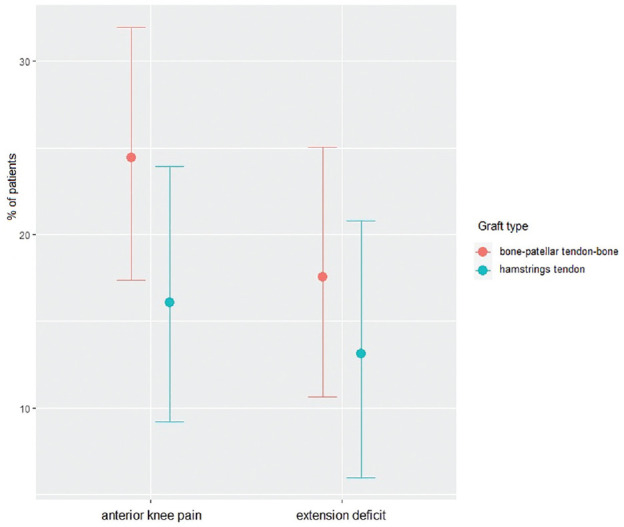
Model expected population effects of anterior knee pain and extension deficit by graft type.
Figure 3.
Differences in the posterior distributions of model expected population effects of (A) anterior knee pain and (B) extension deficit between graft types. The vertical solid black lines denote 95% CI of the distribution of differences and the dashed red line denotes zero.
Figure 4.
Posterior distribution of the population effects of anterior knee pain (AKP) and extension deficit (ED) for (A) bone–patellar tendon–bone (BPTB) and (B) hamstring (HS).
Discussion
The primary findings of the present study were that there was a moderate but clear association between the population effects of ED and AKP for both grafts (BPTB: r = 0.40 [95% CI, 0.39-0.42]; HS: r = 0.35 [95% CI, 0.33-0.36]) and, as expected, the population effect of AKP was higher in BPTB compared with HS (24.1% [95% CI, 17.4%-31.9%] vs 16.1% [95% CI, 9.2%-23.9%], respectively); on the contrary, evidence for a higher ED population effect in BPTB compared with HS grafts were less strong (17.5% [95% CI, 10.6%-25.0%] and 13.1% [95% CI, 6.0%-20.8%], respectively).
The higher AKP in BPTB compared with HS is in accordance with recent meta-analyses (Figure 3A).19,49,51 It should be noted, however, that even though there are significant between-graft differences as per the incidence of AKP,19,48,49,51 it evolves favorably and dissolves within 2 years of follow-up in 83% of patients who follow optimal rehabilitation. 39 Evidence for higher ED in BPTB compared with HS was not as strong (Figure 3B), and this is also in line with the mixed findings from previous analyses.19,49,51 For example, differences in favor of the HS graft have been reported 51 but others have found nonsignificant trends 49 or even no short- or long-term differences between the 2 graft types for deficits of ≥5°. 19
In addition, the present review demonstrated a moderate correlation between the population effects of ED and AKP; in the above previous analyses, ED and AKP population effects are estimated separately and are thus assumed to be uncorrelated. 18 In fact, it has been argued that ED may contribute to AKP due to improper placement of either tunnel or an inadequate notchplasty, which will result in impingement and prevention of full extension and AKP during the healing phase of the graft. 44 Over the past several years, a large body of knowledge has accumulated to improve the anatomic placement of the graft intra-articularly, which does not cause impingement and ED, thus subsequently reducing AKP.10,13,16,29
AKP has been reported as a complication related to donor-site morbidity after ACLR using BPTB graft and as the main factor to avoid this graft,19,51 despite its other advantages such as stability, lower rates of rerupture, and lesser rates of infection.10,24,35,37-39,52 The origin of AKP after ACLR has been under investigation.42,44 It is mainly attributed to the harvesting of the BPTB graft, although it is not rare in patients who have had an HS graft ACLR. 42 In fact, it has been recommended to avoid full hyperextension in the postoperative period after HS graft ACLR, presumably because the stress may stretch the graft. 44 However, regaining full hyperextension later in the postoperative period may not be feasible and the resulting ED of the flexion contracture may cause AKP. 44
Furthermore, it has previously been demonstrated that ED was an important predisposing factor for AKP in the early postoperative period (at 3 months). 34 More importantly, the vast majority of patients with AKP at 2 years of follow-up also had AKP at the 3-month follow-up, potentially highlighting the need for early recovery of extension range of motion. 34 To this notion, Shelbourn and Trumper 45 already underlined this phenomenon and found it very important to achieve full extension intraoperatively, or hyperextension if there is any in the contralateral knee, which has to be maintained with an accelerated postoperative mobilization and physiotherapy. 45 The appearance of AKP in patients treated with HS graft, despite not having a scar on the anterior surface of the knee, further supports this view.32,42,44 The lower incidence of AKP using HS graft can be attributed to a faster postoperative restoration of quadriceps muscle function compared to BPTB graft. 31
In a recent study, the existence of ED was 5.3 times more likely associated with AKP while a BPTB graft was associated with a 3.4 incidence ratio. 32 This complication has been connected to BPTB graft because patients operated on using BPTB graft showed 2.3 times more probability of developing an ED compared with patients with HS graft. The authors advocated an optimal position of the graft between the lateral femoral condyle and the posterior cruciate ligament, which allows full extension immediately postoperative. 32 This correct placement of the graft anatomically seems to be very important and very much influences the generation of ED and also potentially explains the difference of AKP and ED from the literature.11,32 de Abreu-e-Silva et al 11 showed with a 3-dimensional computed tomography comparative study where an ED was observed more often using the transtibial technique. 11 In our review, 10 out of 12 studies used the transtibial technique; thus, we cannot infer whether more modern surgical procedures can moderate the association between ED and incidence of AKP.
Previous researchers advocated an accelerated mobilization and physical therapy after using a BPTB graft to gain full range of motion.44,45 In a study of 602 patients and 122 control patients, a protocol focused on full extension early postoperatively was successful in preventing AKP, provided the graft was positioned in a place that allowed immediate full extension. 45 However, even if the incidence of AKP was more often seen in patients treated using BPTB compared with HS graft, the complaints disappeared over time, and 15 years later there was no difference between the 2 groups. 48 This is further supported by the findings of Rousseau et al 39 who reported diminishing AKP within 2 years after ACLR. 39 A previous study reported that a contemporary surgical technique with more medial incision, bone grafting, and closing of the peritendon was associated with lower AKP compared with that in the majority of the studies included in the present review. 17 If more advanced techniques can lower AKP related to the BPTB graft site, the clinical value of the association between ED and AKP will be strengthened. Moreover, Sanchis-Alfonso et al 42 reviewed the association between quadriceps strength deficit and AKP and advocated an improved rehabilitation protocol to avoid AKP.
When interpreting a systematic review, the sample size of the included studies, as well as their level of evidence, must be taken into account. A total of 976 patients were available to assess the association of AKP and ED in BPTB and HS grafts, which is lower compared with previous studies.19,49,51 Modeling ED and AKP via measurement error model allows taking into account the uncertainty in the reported estimates, which is influenced by the sample size of each individual study, and also estimating an index of their association. 18 All included studies were either RCTs (level 1) or PCSs (level 2). All included PCSs were rated as high quality, but on the other hand, nearly all RCTs were rated as medium quality. The effect of study design was initially tested but the model did not perform better; therefore, our analysis viewed study design as a trivial predictor of either ED or AKP. Similarly, using follow-up (≤5 years vs ≥6 years) as a predictor did not improve model fit. Thus, these subgroup analyses and the sensitivity analyses to detect heterogeneity provided support for the robustness of our results.
Limitations
The final clinical results may have been affected by the inconsistency in the fixation methods selected, differences in the rates of follow-up loss, and the rehabilitative protocols selected during the postoperative period. Our analysis cannot distinguish whether the association between the population effects of AKP and ED is due to specifically harvesting autograft tissue. In this regard, future meta-analyses should also estimate rates of AKP and ED in allografts versus BPTB and HS grafts. There was also some discrepancy between studies as per the reporting of AKP. In addition, most studies consider AKP postoperatively without any consideration of the degree and incidence of preoperative AKP. All articles included were published in English, thus potentially introducing some degree of publication bias. Finally, the effects of patient characteristics (ie, age, sex, activity level) cannot be considered because of data unavailability.
Conclusion
There is a moderate but clear correlation between ED and AKP irrespective of graft type. From a clinical perspective, this association emphasizes the need for intraoperative achievement of full extension and avoidance of situations that may cause ED. The higher incidence of AKP in patients with BPTB graft may also be attributed to factors related to the graft harvest site. Future metaregression analyses could investigate whether additional factors such as follow-up duration or rehabilitation protocols can moderate the association between AKP and ED after ACLR with either BPTB or HS graft.
Footnotes
Final revision submitted January 21, 2024; accepted February 26, 2024.
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Aglietti P, Buzzi R, Zaccherotti G, De Biase P. Patellar tendon versus doubled semitendinosus and gracilis tendons for anterior cruciate ligament reconstruction. Am J Sports Med. 1994;22(2):211-217. [DOI] [PubMed] [Google Scholar]
- 2. Belk JW, Kraeutler MJ, Carver TJ, McCarty EC. Knee osteoarthritis after anterior cruciate ligament reconstruction with bone–patellar tendon–bone versus hamstring tendon autograft: a systematic review of randomized controlled trials. Arthroscopy. 2018;34(4):1358-1365. [DOI] [PubMed] [Google Scholar]
- 3. Bowman EN, Limpisvasti O, Cole BJ, El Attrache N. Anterior cruciate ligament reconstruction graft preference most dependent on patient age: a survey of United States surgeons. Arthroscopy. 2021;37(5):1559-1566. [DOI] [PubMed] [Google Scholar]
- 4. Brinlee AW, Dickenson SB, Hunter-Giordano A, Snyder-Mackler L. ACL reconstruction rehabilitation: clinical data, biologic healing, and criterion-based milestones to inform a return-to-sport guideline. Sports Health. 2022;14(5):770-779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Burkner PC. Brms: an R package for Bayesian multilevel models using Stan. J Stat Soft. 2017;80:1-28. [Google Scholar]
- 6. Cervellin M, de Girolamo L, Bait C, Denti M, Volpi P. Autologous platelet-rich plasma gel to reduce donor-site morbidity after patellar tendon graft harvesting for anterior cruciate ligament reconstruction: a randomized, controlled clinical study. Knee Surg Sports Traumatol Arthrosc. 2012;20(1):114-120. [DOI] [PubMed] [Google Scholar]
- 7. Chee MY, Chen Y, Pearce CJ, et al. Outcome of patellar tendon versus 4-strand hamstring tendon autografts for anterior cruciate ligament reconstruction: a systematic review and meta-analysis of prospective randomized trials. Arthroscopy. 2017;33(2):450-463. [DOI] [PubMed] [Google Scholar]
- 8. Chen H, Liu H, Chen L. Patellar tendon versus 4-strand semitendinosus and gracilis autografts for anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials with mid- to long-term follow-up. Arthroscopy. 2020;36(8):2279-2291. [DOI] [PubMed] [Google Scholar]
- 9. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 10. Cristiani R, Sarakatsianos V, Engström B, Samuelsson K, Forssblad M, Stålman A. Increased knee laxity with hamstring tendon autograft compared to patellar tendon autograft: a cohort study of 5462 patients with primary anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):381-388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. de Abreu-e-Silva GM, Baumfeld DS, Bueno EL, Pfeilsticker RM, de Andrade MA, Nunes TA. Clinical and three-dimensional computed tomographic comparison between ACL transportal versus ACL transtibial single-bundle reconstructions with hamstrings. Knee. 2014;21(6):1203-1209. [DOI] [PubMed] [Google Scholar]
- 12. de Andrade ALL, Sardeli AV, Garcia TA, Livani B, Belangero WD. Time-dependent effect of platelet-rich plasma in reducing donor-site pain after anterior cruciate ligament reconstruction. Am J Sports Med. 2021;49(10):2854-2858. [DOI] [PubMed] [Google Scholar]
- 13. Flannery SW, Murray MM, Badger GJ, et al. Early MRI-based quantitative outcomes are associated with a positive functional performance trajectory from 6 to 24 months post–ACL surgery. Knee Surg Sports Traumatol Arthrosc. 2023;31(5):1690-1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gaudot F, Chalencon F, Nourissat G, et al. Impact of anterior knee pain on mid-term outcome after anterior cruciate ligament reconstruction. Rev Chir Orthop. 2008;94(8Suppl):372-374. [DOI] [PubMed] [Google Scholar]
- 15. Gifstad T, Sole A, Strand T, Uppheim G, Grontvedt T, Drogset JO. Long-term follow-up of patellar tendon grafts or hamstring tendon grafts in endoscopic ACL reconstructions. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):576-583. [DOI] [PubMed] [Google Scholar]
- 16. Grasso S, Linklater J, Li Q, Parker DA. Validation of an MRI protocol for routine quantitative assessment of tunnel position in anterior cruciate ligament reconstruction. Am J Sports Med. 2018;46(7):1624-1631. [DOI] [PubMed] [Google Scholar]
- 17. Hacken BA, Keyt LK, Leland DP, et al. A novel scoring instrument to assess donor site morbidity after anterior cruciate ligament reconstruction with a patellar tendon autograft at 2-year follow-up using contemporary graft-harvesting techniques. Orthop J Sports Med. 2020;8(6):2325967120925482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Harrer M, Cuijpers P, Furukawa TA, Ebert DD. Doing Meta-Analysis with R: A Hands-On Guide. Chapman & Hall/CRC Press; 2021. [Google Scholar]
- 19. He X, Yang XG, Feng JT, et al. Clinical outcomes of the central third patellar tendon versus four-strand hamstring tendon autograft used for anterior cruciate ligament reconstruction: a systematic review and subgroup meta-analysis of randomized controlled trials. Injury. 2020;51(8):1714-1725. [DOI] [PubMed] [Google Scholar]
- 20. Ibrahim SA, Al-Kussary IM, Al-Misfer AR, Al-Mutairi HQ, Ghafar SA, El Noor TA. Clinical evaluation of arthroscopically assisted anterior cruciate ligament reconstruction: patellar tendon versus gracilis and semitendinosus autograft. Arthroscopy. 2005;21(4):412-417. [DOI] [PubMed] [Google Scholar]
- 21. Johnson AA, Ott MQ, Dogucu M. Bayes Rules! An Introduction to Applied Bayesian Modeling. Chapman and Hall/CRC; 2022. [Google Scholar]
- 22. King E, Richter C, Jackson M, et al. Factors influencing return to play and second anterior cruciate ligament injury rates in level 1 athletes after primary anterior cruciate ligament reconstruction: 2-year follow-up on 1432 reconstructions at a single center. Am J Sports Med. 2020;48(4):812-824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Konrads C, Reppenhagen S, Plumhoff P, Hoberg M, Rudert M, Barthel T. No significant difference in clinical outcome and knee stability between patellar tendon and semitendinosus tendon in anterior cruciate ligament reconstruction. Arch Orthop Trauma Surg. 2016;136(4):521-525. [DOI] [PubMed] [Google Scholar]
- 24. Laboute E, James-Belin E, Puig PL, Trouve P, Verhaeghe E. Graft failure is more frequent after hamstring than patellar tendon autograft. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3537-3546. [DOI] [PubMed] [Google Scholar]
- 25. Laxdal G, Kartus J, Ejerhed L, et al. Outcome and risk factors after anterior cruciate ligament reconstruction: a follow-up study of 948 patients. Arthroscopy. 2005;21(8):958-964. [DOI] [PubMed] [Google Scholar]
- 26. Laxdal G, Sernert N, Ejerhed L, Karlsson J, Kartus JT. A prospective comparison of bone-patellar tendon-bone and hamstring tendon grafts for anterior cruciate ligament reconstruction in male patients. Knee Surg Sports Traumatol Arthrosc. 2007;15(2):115-125. [DOI] [PubMed] [Google Scholar]
- 27. Leys T, Salmon L, Waller A, Linklater J, Pinczewski L. Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med. 2012;40(3):595-605. [DOI] [PubMed] [Google Scholar]
- 28. Liden M, Ejerhed L, Sernert N, Laxdal G, Kartus J. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: a prospective, randomized study with a 7-year follow-up. Am J Sports Med. 2007;35(5):740-748. [DOI] [PubMed] [Google Scholar]
- 29. Lutz PM, Achtnich A, Schütte V, Woertler K, Imhoff AB, Willinger L. Anterior cruciate ligament autograft maturation on sequential postoperative MRI is not correlated with clinical outcome and anterior knee stability. Knee Surg Sports Traumatol Arthrosc. 2022;30(10):3258-3267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Maestroni L, Papadopoulos K, Turner A, Korakakis V, Read P. Relationships between physical capacities and biomechanical variables during movement tasks in athletic populations following anterior cruciate ligament reconstruction. Phys Ther Sport. 2021;48:209-218. [DOI] [PubMed] [Google Scholar]
- 31. Maestroni L, Read P, Turner A, Korakakis V, Papadopoulos K. Strength, rate of force development, power and reactive strength in adult male athletic populations post anterior cruciate ligament reconstruction—a systematic review and meta-analysis. Phys Ther Sport. 2021;47:91-110. [DOI] [PubMed] [Google Scholar]
- 32. Marques FDS, Barbosa PHB, Alves PR, et al. Anterior knee pain after anterior cruciate ligament reconstruction. Orthop J Sports Med. 2020;8(10):232596712096108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Matsumoto A, Yoshiya S, Muratsu H, et al. A comparison of bone-patellar tendon-bone and bone-hamstring tendon-bone autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34(2):213-219. [DOI] [PubMed] [Google Scholar]
- 34. Niki Y, Hakozaki A, Iwamoto W, et al. Factors affecting anterior knee pain following anatomic double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20(8):1543-1549. [DOI] [PubMed] [Google Scholar]
- 35. Poehling-Monaghan KL, Salem H, Ross KE, et al. Long-term outcomes in anterior cruciate ligament reconstruction: a systematic review of patellar tendon versus hamstring autografts. Orthop J Sports Med. 2017;5:2325967117709735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rabuck SJ, Baraga MG, Fu FH. Anterior cruciate ligament healing and advances in imaging. Clin Sports Med. 2013;32(1):13-20. [DOI] [PubMed] [Google Scholar]
- 37. Rahardja R, Zhu M, Love H, Clatworthy MG, Monk AP, Young SW. Effect of graft choice on revision and contralateral anterior cruciate ligament reconstruction: results from the New Zealand ACL Registry. Am J Sports Med. 2020;48(1):63-69. [DOI] [PubMed] [Google Scholar]
- 38. Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind M. Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: results from the Danish registry of knee ligament reconstruction. Am J Sports Med. 2014;42(2):278-284. [DOI] [PubMed] [Google Scholar]
- 39. Rousseau R, Labruyere C, Kajetanek C, Deschamps O, Makridis KG, Djian P. Complications after anterior cruciate ligament reconstruction and their relation to the type of graft: a prospective study of 958 cases. Am J Sports Med. 2019;47(11):2543-2549. [DOI] [PubMed] [Google Scholar]
- 40. Sadoghi P, Muller PE, Jansson V, van Griensven M, Kropfl A, Fischmeister MF. Reconstruction of the anterior cruciate ligament: a clinical comparison of bone-patellar tendon-bone single bundle versus semitendinosus and gracilis double bundle technique. Int Orthop. 2011;35(1):127-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sajovic M, Strahovnik A, Dernovsek MZ, Skaza K. Quality of life and clinical outcome comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: an 11-year follow-up of a randomized controlled trial. Am J Sports Med. 2011;39(10):2161-2169. [DOI] [PubMed] [Google Scholar]
- 42. Sanchis-Alfonso V, Montesinos-Berry E, Subvas-Lopez A, Monllau JC. Anterior knee pain after ACL reconstruction: how to avoid it. In: Sanchis-Alfonso V, Monllau JC, eds. The ACL-Deficient Knee: A Problem Solving Approach. Springer-Verlag; 2013:357-372. [Google Scholar]
- 43. Shelbourne KD, Freeman H, Gray T. Osteoarthritis after anterior cruciate ligament reconstruction: the importance of regaining and maintaining full range of motion. Sports Health. 2012;4(1):79-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Shelbourne KD, Larance S, Noy R. Prevention of anterior knee pain after anterior cruciate ligament reconstruction. In: Sanchis- Alfonso V, ed. Anterior Knee Pain and Patellar Instability. Springer Verlag; 2006:283-293. [Google Scholar]
- 45. Shelbourne KD, Trumper RV. Preventing anterior knee pain after anterior cruciate ligament reconstruction. Am J Sports Med. 1997;25(1):41-47. [DOI] [PubMed] [Google Scholar]
- 46. Taketomi S, Inui H, Yamagami R, et al. Bone-patellar tendon-bone autograft versus hamstring tendon autograft for anatomical anterior cruciate ligament reconstruction with three-dimensional validation of femoral and tibial tunnel positions. J Knee Surg. 2018;31(9):866-874. [DOI] [PubMed] [Google Scholar]
- 47. Tan SHS, Lau BPH, Krishna L. Outcomes of anterior cruciate ligament reconstruction in females using patellar-tendon-bone versus hamstring autografts: a systematic review and meta-analysis. J Knee Surg. 2019;32(8):770-787. [DOI] [PubMed] [Google Scholar]
- 48. Webster KE, Feller JA, Hartnett N, Leigh WB, Richmond AK. Comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction: a 15-year follow-up of a randomized controlled trial. Am J Sports Med. 2016;44(1):83-90. [DOI] [PubMed] [Google Scholar]
- 49. Xie X, Liu X, Chen Z, Yu Y, Peng S, Li Q. A meta-analysis of bone–patellar tendon–bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee. 2015;22(2):100-110. [DOI] [PubMed] [Google Scholar]
- 50. Zaffagnini S, Marcacci M, Lo PM, Giordano G, Iacono F, Neri MP. Prospective and randomized evaluation of ACL reconstruction with three techniques: a clinical and radiographic evaluation at 5 years follow-up. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1060-1069. [DOI] [PubMed] [Google Scholar]
- 51. Zhao L, Lu M, Deng M, Xing J, He L, Wang C. Outcome of bone–patellar tendon–bone vs hamstring tendon autograft for anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials with a 5-year minimum follow-up. Medicine (Baltimore). 2020;99(48):e23476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Zhou P, Liu JC, Deng XT, Li Z. Hamstring autograft versus patellar tendon autograft for anterior cruciate ligament reconstruction, which graft has a higher contralateral anterior cruciate ligament injury rate? A meta-analysis of 5561 patients following the PRISMA guidelines. Medicine (Baltimore). 2020;99(31):e21540. [DOI] [PMC free article] [PubMed] [Google Scholar]