Abstract
Abstract
Objective
To identify the types of conditions reported in peer-reviewed literature that result in chronic musculoskeletal lower limb pain in children and adolescents and explore the alignment of these conditions with the chronic pain reporting codes indexed in the International Classification of Diseases 11th Revision (ICD-11).
Design
This scoping review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.
Data sources
Five electronic databases were searched (Medline, EMBASE, PsycINFO, CINAHL and the Cochrane Library).
Eligibility criteria
Articles involving children and adolescents under 18 years and reporting on chronic musculoskeletal pain of the lower limb were included.
Data extraction and synthesis
We assigned an ICD-11 code to each condition based on details reported in the study. We recorded whether any of the presenting conditions were linked to an ICD-11 chronic pain manifestation code.
Results
From 12 343 records, 418 papers were included. There were 124 unique conditions associated with chronic lower limb pain, the most commonly reported being chronic widespread musculoskeletal pain (24 studies) and juvenile idiopathic arthritis (26 studies). Only 11.1% of presenting conditions were linked to an ICD-11 chronic pain manifestation code.
Conclusion
Most presenting conditions associated with chronic pain in the lower limb do not have a chronic pain manifestation code in the new global standard for recording health information. This means chronic pain associated with common lower limb conditions may remain invisible in global statistics.
Keywords: Chronic Pain, Adolescent, Community child health, Paediatric orthopaedics
STRENGTHS AND LIMITATIONS OF THIS STUDY.
We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews and a registered protocol to guide this review.
We used the International Classification of Diseases 11th Revision for recording diagnostic health information to classify conditions and chronic pain.
Only studies published in English were included.
One reviewer extracted data due to the breadth of data collected.
No studies had a risk of bias or quality assessment.
Introduction
Chronic pain, defined as pain lasting for more than 3 months, can occur in 20.8% (95% CI 19.2 to 22.4%) of children and adolescents.1 2 Children and adolescents face difficulties as a result of chronic pain including reduced participation in daily activities, such as attending school, playing with their peers and engaging in physical activity.3 Chronic pain negatively impacts quality of life and increases the risk of psychological disturbances such as anxiety and depression.24,6 The lower limb (foot, ankle, leg, knee, thigh and hip) is one of the most common sites of chronic musculoskeletal pain in children and adolescents, accounting for almost 40% of all childhood chronic disease pain patterns.3 7 The onset of chronic lower limb pain in childhood tends to occur before children enter formal schooling,8 but diagnoses vary considerably. It is likely to persist for up to 4 years following their first episode.9
Children commonly experience chronic pain for 12 months prior to seeing a professional with additional experience in managing chronic pain such as a pain medicine specialist or allied health professional such as a physiotherapist, psychologist or occupational therapist.9 Adequate education, identification and assessment at early stages in the pain journey are pivotal in minimising any pain chronification risk. This is because children and their families initially present to primary care or community-based health professionals such as allied health, well before specialist consultation.10 11 To enable adequate care from the outset, primary care clinicians and community-based healthcare professionals may benefit from specific evidence-based guidelines to provide optimal and early diagnosis and treatment of chronic pain in children and adolescents prior to engaging with specialist services.12
Population-level research conducted in Australia shows that children and adolescents musculoskeletal lower limb presentations to general practice are twice as common as spinal and trunk problems.12 The authors of the study,12 however, noted that they could not distinguish presentations that were acute or chronic in nature, highlighting the need for a standardised system to collect such data. Recently, the International Classification of Diseases (ICD) framework (https://icd.who.int/en) was revised to include chronic pain as a separate disease category.13 14 Incorporating chronic pain classifications into the ICD 11th Revision (ICD-11) allows to capture health statistics, hence making chronic pain more visible as a public health issue.15 This is an important goal to address the under-recognition of chronic pain in children and adolescents and improve health outcomes.16 While the ICD-11 may better highlight the burden of chronic pain in children and adolescents, its usefulness is yet to be explored in the context of chronic musculoskeletal pain in the lower limb of children and adolescents.17
The primary aim of this scoping review was to identify the breadth and types of conditions reported in peer-reviewed literature that may result in chronic lower limb pain in children and adolescents. The secondary aim was to explore the alignment of these conditions with the new chronic pain reporting codes indexed in the ICD-11. This secondary aim served as an exercise to field test the usefulness of the ICD-11 in capturing cases in which certain health conditions are associated with chronic musculoskeletal pain of the lower limb. Scoping review methodology was chosen to ensure a broad approach guided data capture.
Methods
This scoping review was conducted in accordance with the Joanna Briggs Institute methodology for scoping reviews.18 We reported the review in line with Preferred Reporting Items for Systematic Reviews and Meta-Analyses reporting guidelines for scoping reviews (PRISMA-ScR). A protocol for this scoping review was registered on Open Science Framework on 3 March 2023 (https://doi.org/10.17605/OSF.IO/2RYV6).
This scoping review was overseen by a steering group of 15 paediatric and methodological experts assembled by the research team. The group comprised 10 paediatric healthcare professionals who routinely support children who experience chronic musculoskeletal lower limb pain. These included a rheumatologist, endocrinologist, general practitioner, orthopaedic surgeon, paediatrician, psychologist, pharmacist, two physiotherapists/clinical researchers and a podiatrist/clinical researcher. We also were supported by three methodology experts and two consumer representatives with an interest in chronic lower limb pain in children and adolescents. The role of the steering group was to provide input into the search strategy and resolve disagreements in the categorisation of conditions according to the ICD-11. This steering group also established which conditions included in this review were musculoskeletal in nature which aligned with the funding directions and aims.
Eligibility criteria
Studies were eligible for inclusion if they were available in English, sampled a paediatric population (<18 years of age or mean or median population <18 years of age)19 and reported on the presence of chronic or persistent musculoskeletal pain in the lower limb. Chronic or persistent musculoskeletal pain was defined as studies describing pain lasting for longer than 3 months that originates in the joints, bones, muscles, tendons and related soft tissues.7 For the purposes of this review, the lower limb included the hip, thigh, knee, leg, ankle and foot but excluded the pelvis, pubic symphysis and sacroiliac joints. This review included randomised controlled trials, observational studies and case reports and series to ensure study conclusions were based on the primary analysis of human data. These eligibility criteria were chosen to ensure only conditions relevant to chronic musculoskeletal pain were included and aligned with the overall research aim of the funder. Therefore, pain that was dermatological or neuropathic/potentially neuropathic in nature was excluded (eg, chronic regional pain syndrome), and work-related pain or articles describing a region of pain without a diagnostic name (eg, juvenile idiopathic arthritis) or condition (eg, primary chronic musculoskeletal pain) were excluded. Papers that were trial protocols, editorials, opinion pieces or where no data were presented were excluded. In studies with mixed populations (eg, in terms of age, location of pain and mechanisms of pain such as neuropathic pain), only data from participants that met this review’s eligibility criteria were included: individuals less than 18 years of age with chronic musculoskeletal pain of the lower limb.
Information sources and search strategy
An initial, limited search of PubMed and Google Scholar was conducted to identify any papers on the topic of “chronic lower limb pain”, “musculoskeletal pain” and “paediatric pain”. To ensure a comprehensive search of the literature, a clinical research librarian assisted in the development of a systematic search strategy for each of the databases. Five electronic databases were then searched, including Medline, EMBASE, PsycINFO, CINAHL and the Cochrane Library using keywords such as “chronic pain”, “lower extremity” and “paediatric”. The full electronic search strategy for Medline is presented in table 1 (for all strategies, see online supplemental table 1), which was adapted for each of the included databases. No limitations were placed on publication date or status. The initial search was conducted from database inception until 4 May 2022 and then updated on 25 July 2024. Studies meeting the eligibility criteria were uploaded onto EndNote V.X9 (Clarivate Analytics, PA, USA) and then exported to Covidence Systematic Review Software (Veritas Health Innovation, Melbourne, Australia) for de-duplication and screening.
Table 1. Full search strategy for Medline.
| Search | Query |
| 1 | Lower Extremity/ or Leg/ or Hip/ or Knee/ or Ankle/ or Foot/ |
| 2 | (leg* or hip* or knee* or ankle* or foot or feet or lower limb* or lower extremit*).mp. |
| 3 | 1 or 2 |
| 4 | Chronic Pain/ or arthralgia/ or musculoskeletal pain/ or nociceptive pain/ or pain, postoperative/ or neuralgia/ |
| 5 | ((persistent or chronic or ongoing or long-term or nociceptive or musculoskeletal or post-operative or joint or neuropathic or nerve) adj3 pain).mp. |
| 6 | arthralgia.mp. |
| 7 | 4 or 5 or 6 |
| 8 | 3 and 7 |
| 9 | Infant/ or Child/ or Child, Preschool/ or Adolescent/ |
| 10 | (baby or babies or neonate* or newborn or child* or infant* or toddler* or paediatric* or pediatric* or teen* or adolesc* or pre-pubesc* or prepubesc* or youth* or juvenile).mp. |
| 11 | 9 or 10 |
| 12 | 8 and 11 |
| 13 | exp animals/ not humans.sh. |
Selection of sources of evidence
Two reviewers (CW and VP) independently screened titles and abstracts of papers based on the eligibility criteria. In the event of disagreements, a third reviewer (EI) was consulted to reach a consensus. Full texts were screened independently by two of five reviewers (CW, VP, EI, LD and MS). Any concerns regarding the eligibility of a study were resolved by consensus among the authors first and then by the steering group in cases where the musculoskeletal nature of the conditions reported was unclear. Extensive efforts were made to retrieve full-text records through multiple physical and digital sources including two university libraries and a hospital library. Due to the data capture strategies and volume of data, we did not use any citation chaining methods.
Data charting process and data items
Data from eligible studies were extracted into a purpose-built spreadsheet in Microsoft Excel. Data items included first author, year of publication, type of study design, the country/countries in which the study was conducted, the age groups researched, duration of pain described in the study, lower limb location of pain and the specific condition(s) that were reported to be associated with chronic musculoskeletal pain of the lower limb.
Data were extracted by one reviewer. Following extraction, one reviewer (EI, LD, VP, CW or MS) independently used the ICD-11 (https://icd.who.int/en) to assign a code to each of the conditions presented in the studies. The ICD-11 browser V.2022.02 release (https://icd.who.int/en) was used for coding. All codes were then discussed during regular meetings between reviewers (EI, LD, VP, CW and MS) to ensure coding consistency and agreement, where several cases or diagnoses were independently coded differently by reviewers and all similar condition codes were checked to ensure correct alignment and decisions. We did not record the number of disagreements in coding. Coding was done to the level at which the paper provided sufficient detail about the condition. Given the scope of this review, we did not contact the authors of papers with the necessary missing information. Disagreements were resolved through discussion and adjudication by a third reviewer or steering group experts if a resolution could not be found. Using the ICD-11, each study was assigned a ‘parent’ code (a two-digit code) to facilitate hierarchical organisation of the data. In studies which reported more than one condition, multiple codes were assigned to reflect the number of conditions reported. We also recorded cases which had multiple parent codes. Where a presenting condition was aligned with a secondary chronic pain manifestation code, this was also recorded within the spreadsheet. An ICD manifestation code describes the manifestation, symptoms or signs of the underlying disease (eg, pain) rather than the disease itself. Only codes that reflected the primary condition/s and, if different, the pain conditions were recorded. For example, FB82.00 (chondromalacia patellae) is linked to the manifestation code MG30.31 (chronic secondary musculoskeletal pain associated with structural changes). Manifestation codes in the ICD-11 refer to the manifestation of the disease (eg, chronic pain), not the disease itself. Therefore, all chronic pain manifestation codes refer to chronic secondary pain conditions, not chronic primary pain conditions.
Data synthesis
Data were summarised descriptively using frequencies and percentages to characterise the published literature (eg, country, study design, sample size, age and sex of participants). To address the review aims, data were also summarised descriptively to determine types and percentage of conditions associated with chronic lower limb pain in children and adolescents. This was achieved by analysing the ICD-11 parent codes of the relevant conditions, which were then categorised into primary and secondary chronic pain groups, according to the definitions provided by Treede et al.7 In addition, conditions relating to the same anatomical structure or physiological process were grouped under a single broad heading. For example, conditions associated with joint instability of the hip, patella and ankle were merged and grouped under ‘joint instability of the lower limb’. Finally, the alignment of these conditions with the new chronic pain classification system was explored by determining whether any presenting conditions (where the pain was not a result of chronic primary pain) were indexed with a chronic pain manifestation code in the ICD-11.
Patient and public involvement
There were two consumer representatives. One who had lived experience of a child with chronic lower limb pain and supporting families with chronic lower limb pain. The other provided support and education to health professionals who provide services to children who have chronic lower limb pain.
Results
Characteristics of included studies
A total of 12 343 records were identified through the database searches. After duplicates were removed, records were combined where they reported on same data, and titles and abstracts were screened, 1409 papers were downloaded for full-text screening, with a final of 418 studies (from 422 reports where 4 described data from the same population) included in the review (figure 1). A common reason for exclusion was that studies did not report on participants with chronic and/or persistent pain.
Figure 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart of records screened and included in the scoping review.
Of the 418 studies included in this review (online supplemental table 2), most studies were case reports (n=220 studies) or retrospective medical record reviews (n=54) which were published in the 2010s (n=220/418), conducted in the USA (n=143/418 studies) and sampled adolescents between 11 and 17 years of age (n=179/418 studies). Of those studies that reported sex (336 studies), studies sampled more females (n=4782) than males (n=2556) in total. No paper included in this review sampled infants less than a year old (table 2).
Table 2. Characteristics of included studies.
| Type of study design | N=418 | % |
| Case report | 220 | 52.6 |
| Case series | 30 | 7.2 |
| Cohort | 40 | 9.6 |
| Cross-sectional | 53 | 12.7 |
| Longitudinal | 9 | 2.2 |
| Randomised controlled trial | 10 | 2.4 |
| Retrospective medical record review | 54 | 12.9 |
| Review | 2 | 0.5 |
| Country of data collection | ||
| Australia | 15 | 3.6 |
| Canada | 8 | 1.9 |
| China | 12 | 2.9 |
| Denmark | 11 | 2.6 |
| France | 10 | 2.4 |
| Germany | 12 | 2.9 |
| India | 19 | 4.5 |
| Italy | 16 | 3.8 |
| Japan | 18 | 4.3 |
| Spain | 8 | 1.9 |
| Turkey | 22 | 5.3 |
| UK | 20 | 4.8 |
| USA | 143 | 34.2 |
| Other* | 104 | 24.9 |
| Decade of publication | ||
| 1980s | 2 | 0.5 |
| 1990s | 27 | 6.5 |
| 2000s | 76 | 18.2 |
| 2010s | 220 | 52.6 |
| 2020–2024 | 93 | 22.2 |
| Age groups† | ||
| Infancy (0–1 years) | 0 | 0.0 |
| Childhood (2–10 years of age) | 79 | 18.9 |
| Adolescence (11–17 years) | 179 | 42.8 |
| Mixed age groups (0–17 years) | 160 | 38.3 |
| Sex | ||
| Males (total N) | 2556 | 34.8 |
| Females (total N) | 4782 | 65.2 |
| Studies in which sex was not reported | 79 | – |
Algeria (1), Austria (1), Bangladesh (1), Belgium (1), Bolivia (1), Bosnia (1), Brazil (1), Bulgaria (2), Croatia (2), Czech Republic (1), Egypt (1), Finland (4), Greece (5), Hong Kong (1), Hungary (2), Indonesia (1), Iran (2), Ireland (3), Israel (2), Kenya (1), Korea (6), Lebanon (1), Libya (1), Macedonia (1), Malaysia (4), Mexico (2), Nepal (1), Netherlands (6), New Zealand (1), Nigeria (2), Norway (4), Oman (1), Pakistan (3), Poland (4), Portugal (4), Qatar (2), Saudi Arabia (2), South Africa (2), Sri Lanka (1), Sweden (5), Switzerland (3), Taiwan (3), Thailand (5), Ukraine (2), and multiple countries in Africa (1).
Based on the American Academy of Paediatrics; Aadolescence is divided into 3three groups according to this classification but was collapsed into one category for the purposes of this review (>10 years of age). Late adolescence, being 18–21 years of age, was excluded from this study.
Conditions related to chronic musculoskeletal pain of the lower limb
Discounting duplicate conditions, this review found 124 unique conditions that were associated with chronic musculoskeletal lower limb pain in children and adolescents (online supplemental table 3). The most commonly reported health conditions identified resulting in chronic lower limb pain in children and adolescents were juvenile idiopathic arthritis (n=26/418 studies), chronic widespread musculoskeletal pain (n=24/418 studies), spasticity-related musculoskeletal pain in cerebral palsy (n=20/418 studies), post-surgical pain (n=13/418 studies), osteoid osteoma (n=14/418 studies) and post-fracture (n=14/418 studies) (table 3).
Table 3. Chronic musculoskeletal pain of the lower limb.
| N=418 studies | % | |
| Most common conditions reported | ||
| Juvenile idiopathic arthritis | 26 | 6.2 |
| Chronic widespread musculoskeletal pain | 24 | 5.7 |
| Spasticity-related musculoskeletal pain from cerebral palsy | 20 | 4.8 |
| Osteoid osteoma | 14 | 3.3 |
| Fracture | 14 | 3.3 |
| Post-surgical pain | 16 | 3.8 |
| ICD-11 parent codes | N=463 cases | |
| 1: Certain infectious or parasitic diseases | 11 | 2.4 |
| 2: Neoplasms | 24 | 5.2 |
| 3: Diseases of the blood or blood-forming organs | 10 | 2.2 |
| 4: Diseases of the immune system | 19 | 4.1 |
| 5: Endocrine, nutritional or metabolic diseases | 13 | 2.8 |
| 6: Mental, behavioural or neurodevelopmental disorders | 1 | 0.2 |
| 7: Sleep-wake disorders | 1 | 0.2 |
| 8: Diseases of the nervous system | 35 | 7.6 |
| 11: Diseases of the circulatory system | 1 | 0.2 |
| 12: Diseases of the respiratory system | 2 | 0.4 |
| 13: Diseases of the digestive system | 2 | 0.4 |
| 14: Diseases of the skin* | 1 | 0.2 |
| 15: Diseases of the musculoskeletal system or connective tissue | 176 | 38.0 |
| 20: Developmental anomalies | 55 | 11.9 |
| 21: Symptoms, signs or clinical findings, not elsewhere classified | 48 | 10.4 |
| 22: Injury, poisoning or certain other consequences of external causes | 28 | 6.0 |
| 23: External causes of morbidity and mortality | 2 | 0.4 |
| X: Extension codes | 34 | 7.3 |
| Presence of a chronic pain manifestation code in cases where chronic pain was not the primary condition | 46/415 cases | 11.1 |
| Duration of pain | N=418 studies | % |
| Pain at least ≥3 months | 143 | 34.2 |
| Pain at least ≥6 months | 65 | 15.6 |
| Pain at least ≥12 months | 113 | 27.0 |
| Chronic, but not specified | 97 | 23.2 |
| Location of pain | N=418 | |
| Hip | 73 | 17.5 |
| Thigh/groin | 7 | 1.7 |
| Knee | 111 | 26.6 |
| Leg | 9 | 2.6 |
| Ankle | 42 | 10.0 |
| Foot (including toes) | 32 | 7.7 |
| Widespread lower limb | 44 | 10.5 |
| Mixed cases | 96 | 23.0 |
This referred to one case related to ‘malformations involving cutaneous blood vessels’ (Code EF2Z).
The most common description of pain was having pain for at least 3 months (n=143/418 studies) or for longer than a year (n=113/418 studies). Most commonly, studies reported pain related to the knee only (n=111/418 studies), mixed cases of various locations of the lower limb (n=96 studies) or the hip only (n=76/418 studies) (table 3).
Conditions related to chronic musculoskeletal pain of the lower limb based on the ICD-11
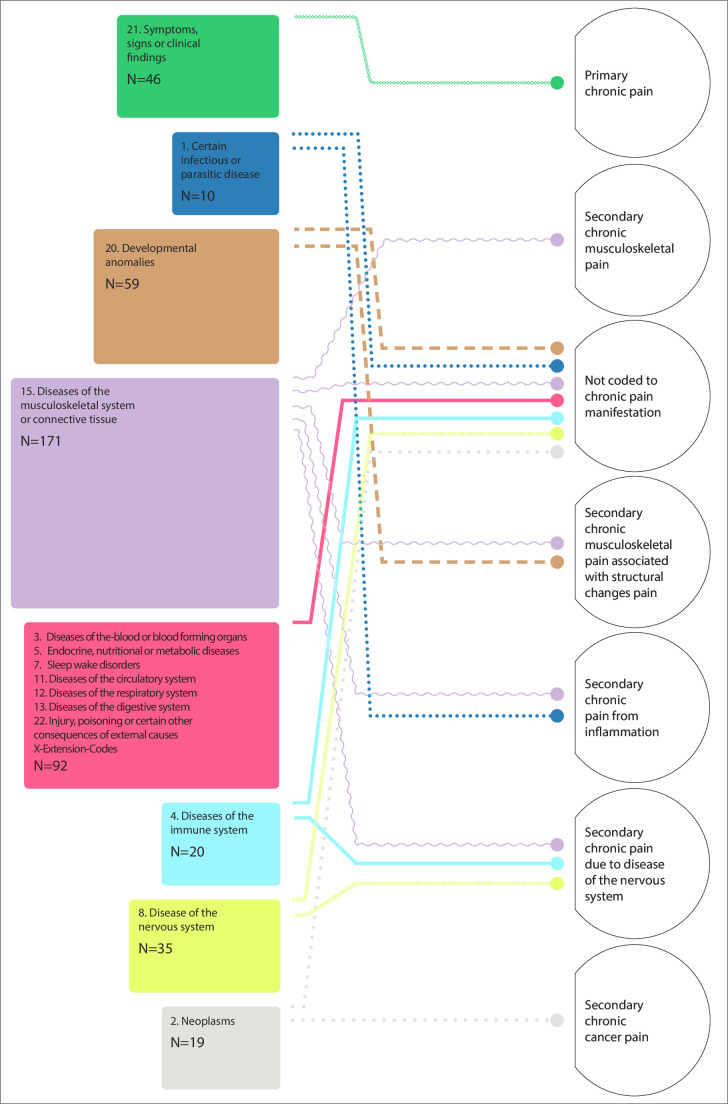
All records could be assigned an ICD-11 code. Out of the 27 parent codes available on the ICD-11 classification system (ICD-11 codes: 01–26, V and X), 18 codes were associated with chronic lower limb pain (ICD-11 codes: 1–8, 11–15, 20–23, X) (table 3). In total, 432 parent codes were assigned to the conditions of participants in the studies (figure 2). The parent codes that were used most frequently were 15: Diseases of the musculoskeletal system or connective tissue (n=165 conditions), 20: Developmental anomalies (n=54 conditions), 21: Symptoms, signs or clinical findings, not elsewhere classified (n=43 conditions), X: Extension codes (n=34 conditions), 8: Diseases of the nervous system (n=32 conditions) and 22: Injury, poisoning or certain other consequences of external causes (n=24 conditions). Several other parent codes (ICD-11 codes: 6, 7, 11–14 and 23) were used for less than five conditions.
Figure 2. The coding of primary and secondary chronic pain conditions of the lower limb in children and adolescents using the International Classification of Diseases 11th Revision (ICD-11) in the peer-reviewed literature. N is the number of codes assigned within each category. Parent codes 6: (mental, behavioural or neurodevelopmental disorders, n=1), 14: (diseases of the skin, n=1 relating to malformations involving cutaneous blood vessels, Code EF2Z) and 23: (external causes of morbidity and mortality, n=2) were omitted from this figure for brevity.
Alignment of the chronic pain classification with the ICD-11 or condition linked with chronic pain manifestation code
Chronic pain was reported as the presenting condition in 48 conditions in this review and assigned the parent code 21: (symptoms, signs or clinical findings, not elsewhere classified) and then the code MG30: (chronic pain). These also included the codes MG30.2: (chronic post-surgical or post-traumatic pain) (n=13 conditions), MG30.0: (chronic primary pain) (n=9 conditions) and MG30.Y: (other specified chronic pain) (n=9 conditions).
For cases in which chronic pain was not the presenting condition (n=415 conditions, ie, chronic secondary pain), only 46 conditions (11.1% of 415 conditions or 13.7% of the 124 unique conditions once duplicates were removed) were linked to a chronic pain manifestation code (MG30) (online supplemental file 2)). These 46 conditions included chronic secondary musculoskeletal pain associated with structural changes (n=20), chronic secondary musculoskeletal pain (n=9), chronic cancer pain (n=8), chronic secondary musculoskeletal pain from persistent inflammation (n=6) and chronic musculoskeletal pain due to disease of the nervous system (n=3) (see figure 2).
Discussion
This scoping review identified 124 unique conditions reported in the literature that may be associated with chronic musculoskeletal pain of the lower limb in children and adolescents. Most studies reported chronic pain as a symptom (eg, chronic secondary musculoskeletal pain from juvenile idiopathic arthritis) rather than a disease in its own right (eg, chronic primary pain such as chronic widespread musculoskeletal pain). The findings of this review suggest that there is considerable variability in the cause of secondary chronic lower limb pain investigated in the peer-reviewed literature.20 The ICD-11 coding system aligned with the plethora of chronic pain conditions was presented. However, only 11.1% of all presenting conditions in the review had a manifestation code linked to chronic pain. This highlights the possibility that the global burden of chronic musculoskeletal pain of the lower limb in children and adolescents may not be adequately captured by the ICD-11 due to the under-utilisation of manifestation codes.
The number of conditions that result in lower limb musculoskeletal chronic pain was extensive. As a result, this breadth will result in diversity in health professionals who may be involved in care. Given the breadth of conditions the review found that may result in chronic musculoskeletal lower limb pain, there is a need for health professionals to be aware of multiple paediatric musculoskeletal health conditions that may result in chronic pain.21 This is currently an international focus.21 This finding also lends itself to consistency in guidelines that are multidisciplinary and not just focused on a single health profession. These opportunities are in place for conditions such as juvenile idiopathic arthritis, the most commonly reported condition in the literature. This condition has a number of guidelines on medication management with limited consideration for chronic musculoskeletal lower limb pain.22
This review highlights that, due to the lack of manifestation codes, there is potential of the ICD-11 in under-reporting diseases that may result in chronic musculoskeletal pain of the lower limb in children and adolescents. The under-recognition of chronic musculoskeletal pain in children and adolescents16 may have far-reaching detrimental impacts on children and adolescents,23 families24 and society16 including the under-assessment and under-management of chronic pain. Making chronic musculoskeletal pain of the lower limb in children and adolescents visible first requires capturing the burden in order to facilitate the adequate allocation of funding and resources. While the ICD-11 offers a potential solution for health systems to enable the evaluation of the burden, the problem of chronic pain needs to be made more visible by incorporating manifestation codes in all potential conditions that could lead to chronic pain. Because manifestation codes are linked to primary health conditions, ensuring that chronic pain manifestation codes exist for those health conditions that are associated with pain may ensure that health professionals, researchers and policymakers are able to select these manifestation codes when inputting data. This presents opportunities for data capture and practice reform.
Limitations of this review arise from the result of the large number of studies included in this review; data from studies were extracted by one reviewer only. We also acknowledge that only English-language papers were included in this review. This may mean that a large number of region-specific conditions resulting in chronic musculoskeletal lower limb pain in children and adolescents were not captured. Another limitation of this review was the inclusion of a large number of case reports. It is important to consider the rate of conditions reported in studies (eg, rate of studies reporting juvenile idiopathic arthritis) does not correspond with the general population prevalence. Future research reporting on the breadth of conditions resulting in chronic lower limb pain may consider aligning findings with condition-specific prevalence rates. Lastly, the assignment of ICD-11 codes was based on what was reported in papers included in this review, and while we extensively consulted with our steering committee, the reported information may have not covered all the required criteria of that diagnosis.
Conclusion
Many conditions may be associated with chronic musculoskeletal lower limb pain in children and adolescents as investigated in the peer-reviewed literature. While the ICD-11 captures chronic pain classifications related to primary and secondary pain conditions, chronic secondary pain must be made more visible by having the ability to link conditions to chronic pain manifestation codes. This may allow clinicians, researchers and policymakers to better estimate the burden of chronic musculoskeletal pain of the lower limb in children and adolescents. Increasing the visibility of chronic musculoskeletal pain in children and adolescents will allow a more equitable distribution of funding and resources for the development of strategies for the appropriate identification of children and adolescents with chronic musculoskeletal lower limb pain.
supplementary material
Acknowledgements
We would like to acknowledge Jeremy Cullis, Clinical Research Librarian at Macquarie University, for his guidance in the development of the search strategies for this scoping review. We would also like to acknowledge and thank Jim Hsu at Monash University for his work designing Figure 2.
Footnotes
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2023-082801).
Provenance and peer review: Not commissioned; externally peer-reviewed.
Patient consent for publication: Not applicable.
Ethics approval: Not applicable.
Patient and public involvement: Patients and/or the public were involved in the design, conduct, report or dissemination plans of this research. Refer to the Methods section for further details.
Data availability free text: The full dataset generated during the current study are available from the corresponding author on reasonable request. An abbreviated version of all data used for analysis in this review is available in the online supplemental tables 2 and 3.
Contributor Information
Emre Ilhan, Email: emre.ilhan@mq.edu.au.
Luke Davies, Email: LUKE.DAVIES@MONASH.EDU.
Verity Pacey, Email: verity.pacey@mq.edu.au.
Mitchell Smith, Email: mitchell.smith@monash.edu.
Jane Munro, Email: jane.munro@rch.org.au.
Craig Munns, Email: c.munns@uq.edu.au.
Elizabeth Sturgiss, Email: elizabeth.sturgiss@monash.edu.
Nicole Williams, Email: Nicole.williams01@adelaide.edu.au.
Louise Tofts, Email: louise.tofts@mq.edu.au.
Vance Locke, Email: v.locke@ecu.edu.au.
Terry Haines, Email: terry.haines@monash.edu.
Sue E Brennan, Email: sue.brennan@monash.edu.
Stephen Maloney, Email: stephen.maloney@monash.edu.
Mitchell N Sarkies, Email: Mitchell.sarkies@sydney.edu.au.
Ornella Clavisi, Email: Ornella@msk.org.au.
Dan Miles, Email: dan.miles@podiatry.org.au.
Lisa Nissen, Email: l.nissen@uq.edu.au.
Cylie Williams, Email: cylie.williams@monash.edu.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.Palermo TM. Impact of recurrent and chronic pain on child and family daily functioning: a critical review of the literature. J Dev Behav Pediatr. 2000;21:58–69. doi: 10.1097/00004703-200002000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Chambers CT, Dol J, Tutelman PR, et al. The prevalence of chronic pain in children and adolescents: a systematic review update and meta-analysis. Pain. 2024;165:2215–34. doi: 10.1097/j.pain.0000000000003267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.King S, Chambers CT, Huguet A, et al. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain. 2011;152:2729–38. doi: 10.1016/j.pain.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 4.Miró J, Roman-Juan J, Sánchez-Rodríguez E, et al. Chronic Pain and High Impact Chronic Pain in Children and Adolescents: A Cross-Sectional Study. J Pain. 2023;24:812–23. doi: 10.1016/j.jpain.2022.12.007. [DOI] [PubMed] [Google Scholar]
- 5.Wager J, Brown D, Kupitz A, et al. Prevalence and associated psychosocial and health factors of chronic pain in adolescents: Differences by sex and age. Eur J Pain. 2020;24:761–72. doi: 10.1002/ejp.1526. [DOI] [PubMed] [Google Scholar]
- 6.Mikkelsen HT, Haraldstad K, Helseth S, et al. Pain and health-related quality of life in adolescents and the mediating role of self-esteem and self-efficacy: a cross-sectional study including adolescents and parents. BMC Psychol. 2021;9:128. doi: 10.1186/s40359-021-00629-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Treede R-D, Rief W, Barke A, et al. Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11) Pain. 2019;160:19–27. doi: 10.1097/j.pain.0000000000001384. [DOI] [PubMed] [Google Scholar]
- 8.Williams CM, Menz HB, Lazzarini PA, et al. Australian children’s foot, ankle and leg problems in primary care: a secondary analysis of the Bettering the Evaluation and Care of Health (BEACH) data. BMJ Open. 2022;12:e062063. doi: 10.1136/bmjopen-2022-062063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shebeshi D, Allingham S, Tardif H, et al. Electronic Persistent Pain Outcomes Collaboration Annual Data Report 2021. Australian Health Services Research Institute: University of Wollongong; 2022. [Google Scholar]
- 10.Morlion B, Coluzzi F, Aldington D, et al. Pain chronification: what should a non-pain medicine specialist know? Curr Med Res Opin. 2018;34:1169–78. doi: 10.1080/03007995.2018.1449738. [DOI] [PubMed] [Google Scholar]
- 11.Wager J, Szybalski K, Schenk S, et al. Predictors of treatment outcome in children with medically unexplained pain seeking primary care: A prospective cohort study. Eur J Pain. 2019;23:1507–18. doi: 10.1002/ejp.1426. [DOI] [PubMed] [Google Scholar]
- 12.Henschke N, Harrison C, McKay D, et al. Musculoskeletal conditions in children and adolescents managed in Australian primary care. BMC Musculoskelet Disord. 2014;15:164. doi: 10.1186/1471-2474-15-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dahlhamer J, Lucas J, Zelaya C, et al. Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67:1001–6. doi: 10.15585/mmwr.mm6736a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Raffaeli W, Arnaudo E. Pain as a disease: an overview. J Pain Res. 2017;10:2003–8. doi: 10.2147/JPR.S138864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van der Linden R, Bolt T, Veen M. “If it can’t be coded, it doesn’t exist”. A historical-philosophical analysis of the new ICD-11 classification of chronic pain. Stud Hist Philos Sci. 2022;94:121–32. doi: 10.1016/j.shpsa.2022.06.003. [DOI] [PubMed] [Google Scholar]
- 16.Eccleston C, Fisher E, Howard RF, et al. Delivering transformative action in paediatric pain: a Lancet Child & Adolescent Health Commission. Lancet Child Adolesc Health. 2021;5:47–87. doi: 10.1016/S2352-4642(20)30277-7. [DOI] [PubMed] [Google Scholar]
- 17.Matthews E, Murray G, McCarthy K. ICD-11 Classification of Pediatric Chronic Pain Referrals in Ireland, with Secondary Analysis of Primary vs Secondary Pain Conditions. Pain Med. 2021;22:2533–41. doi: 10.1093/pm/pnab116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peters MG, McInerney P, Munn Z, et al. JBI Manual for Evidence Synthesis. In: Aromataris E MZ, Ed. 2020. https://synthesismanual.jbi.global/2020 Available. [Google Scholar]
- 19.Hardin AP, Hackell JM, Committee on Practice and Ambulatory Medicine Age Limit of Pediatrics. Pediatrics. 2017;140:e20172151. doi: 10.1542/peds.2017-2151. [DOI] [PubMed] [Google Scholar]
- 20.Zinboonyahgoon N, Luansritisakul C, Eiamtanasate S, et al. Comparing the ICD-11 chronic pain classification with ICD-10: how can the new coding system make chronic pain visible? A study in a tertiary care pain clinic setting. Pain. 2021;162:1995–2001. doi: 10.1097/j.pain.0000000000002196. [DOI] [PubMed] [Google Scholar]
- 21.Foster HE, Scott C, Tiderius CJ, et al. The paediatric global musculoskeletal task force - “towards better MSK health for all.”. Pediatr Rheumatol Online J. 2020;18:60.:60. doi: 10.1186/s12969-020-00451-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Munro J, Brun S, Rawlin M, et al. Clinical Guideline for the Diagnosis and Management of Juvenile Idiopathic Arthritis. The National Health and Medical Research Council of Australian Goverment; 2009. pp. 1–43. [Google Scholar]
- 23.Tian F, Guittar P, Moore-Clingenpeel M, et al. Healthcare Use Patterns and Economic Burden of Chronic Musculoskeletal Pain in Children before Diagnosis. J Pediatr. 2018;197:172–6. doi: 10.1016/j.jpeds.2018.01.076. [DOI] [PubMed] [Google Scholar]
- 24.Ho IK, Goldschneider KR, Kashikar-Zuck S, et al. Healthcare Utilization and Indirect Burden among Families of Pediatric Patients with Chronic Pain. J Musculoskelet Pain. 2008;16:155–64. doi: 10.1080/10582450802161853. [DOI] [Google Scholar]