Abstract
PURPOSE
Cancer continues to be a significant public health concern. Sub-Saharan Africa (SSA) struggles with a lack of proper infrastructure and adequate cancer care workforce. This has led to some countries relying on referrals of cancer care to countries with higher income levels. In some instances, patients refer themselves. Some countries have made it their goal to attract patients from other countries, a term that has been referred to as medical tourism. In this article, we explore the current status of oncology-related medical tourism in SSA.
METHODS
This was a cross-sectional study. The study participants included oncologists, surgeons, and any other physicians who take care of patients with cancer. A predesigned questionnaire was distributed through African Organization for Research and Training in Cancer member mailing list and through study team personal contacts and social media.
RESULTS
A total of 52 participants from 17 African countries with a 1.6:2 male to female ratio responded to the survey. Most (55.8%) of the respondents were from Eastern African countries. The majority (92%) of study participants reported that they knew patients who referred themselves abroad, whereas 75% referred patients abroad, and the most common (94%) referral destination was India. The most common (93%) reason for referral was perception of a higher quality of care in foreign health institutions.
CONCLUSION
The findings suggest the need to improve local health care systems including building trust of the system among general population. The study highlights potential financial toxicity, and it adds to the current emphasis on return of investment on homegrown workforce and cancer treatment infrastructure.
The study findings on medical tourism for cancer treatment in Africa highlights the need to improve local healthcare systems.
INTRODUCTION
In 2022, over 61% of new global cancer cases occurred in low- and low-middle-income countries.1 Despite significant advancements in cancer care over the past several decades, access to diagnosis and treatment in many low- and middle-income settings remains inadequate.2 Many patients in low- and middle-income countries experience significant barriers accessing adequate cancer care, including a limited skilled workforce,3 low availability of essential medicines,4-6 and lack of access to the necessary but resource-intensive treatment options—such as linear accelerators for the delivery of radiation therapy7,8 and bone marrow stem-cell transplants.9
CONTEXT
Key Objective
To analyze trends, trajectories, and perspectives on medical tourism for cancer treatment from African countries, focusing on factors driving this trend and its effect on local health care systems.
Knowledge Generated
The main reasons for medical tourism in oncology include perceived higher care quality, better technology, and mistrust in local systems. Commonly referred cancers are breast, hematological malignancies, and prostate. Medical tourism poses financial burdens and ethical issues, such as inequity and loss of care continuity.
Relevance
The findings emphasize improving local health care, building trust, and regulating medical tourism to reduce economic loss and enhance health care equity in African countries.
Medical tourism is a practice where patients travel abroad to receive health care services and treatment outside of their home country.10 With innovations abound in technology and travel, medical tourism offers an opportunity for individuals to seek higher quality or more affordable care than what is offered in their home country. Many health care fields engage in medical tourism, including plastic surgery, dental care, and reproductive care. However, oncology treatments have experienced the fastest growing market in medical tourism, with a compound annual growth rate of 21.9% over the last 10 years.11 For many patients, medical tourism provides the possibility of obtaining access to cancer treatments and care that are inaccessible or unavailable in their home countries.12 However, medical tourism is also riddled with ethical issues such as inequity of health care provision among the local population and foreign patients, and conflicts of interest among key players including health care providers.13
Due to limited cancer care resources and workforce in Africa, many African patients with cancer are misdiagnosed or experience delayed diagnosis, and some countries lack cancer care facilities or the full array of cancer diagnostics and treatments. Thus, some patients with the financial means may prefer to travel abroad for treatment. The goal of this study was to gain knowledge on the prevalence and patterns and to understand providers' perspectives of cancer medical tourism in Africa.
METHODS
Study Design, Population, and Settings
This was a cross-sectional study that used a detailed survey to garner comprehensive, robust data on the practice of medical tourism for patients with cancer in Africa. The study participants included oncologists, surgeons, and any other physicians who take care of patients with cancer. The intention was to recruit a diverse group of participants in terms of career stage (early, mid, late) and African region representation. This study was approved by the Research Ethics Board of Queen's University.
Questionnaire Design and Distribution
The survey was designed by the core study team with expertise in public health, medical, surgical, and radiation oncology. It was first piloted among the study team. The final questionnaire took about 20 minutes to complete. Using data collection software Qualtrics, the survey was distributed via the African Organization for Research and Training in Cancer mailing list to a network of professionals involved in cancer care in sub-Saharan Africa (SSA), with a target to recruit at least three oncologists per country. Additionally, the study team shared the survey to their personal contacts and social media networks. The survey elicited detailed information regarding physicians' estimates of medical tourism in cancer in their cancer centers and their perspectives on the validity and reasoning behind medical tourism. In addition, additional quantitative information, such as approximate number of referrals per year, was collected in the survey. This study focused on SSA given that most patients who travel abroad for cancer care come from this region. The survey was in English as the majority of clinicians practicing in non–English-speaking countries have a good command of English language.
Data Collection
The core questions explored two types of medical tourism: referral by local physicians and self-referral by patients. Survey questions further explored available regulatory measures for cancer medical tourism in Africa, main types of cancer most referred abroad, barriers and challenges associated with medical tourism, and potential ethical issues in cancer medical tourism.
Data Analysis
Data were captured in Qualtrics and exported into IBM SPSS (version 27.0 for Windows, Armonk, NY, 2021) for statistical analysis. Univariable methods (frequencies and percentages for categorical data, and medians and quartiles for quantitative data) were used to analyze survey responses.
RESULTS
Sociodemographic Characteristics of Study Participants
A total of 52 participants from 17 African countries with a 1.6:2 male to female ratio responded to the survey. Half of the participants (50%) had <5 years of practice experience as oncologists and only 12% had more than 15 years of experience as an oncologist. Most (55.8%) of the respondents were from Eastern African countries including Tanzania (19.2%), Kenya (15.4%), and Rwanda (11.5%). Others were from Western Africa (23.1%), Southern Africa (17.3%), and Northern Africa (3.8%). The most common oncology specialty among respondents was clinical oncology (50.0%) and medical oncology (13.5%). Almost all participants (90.2%) reported having the capacity to offer chemotherapy, radiotherapy (62.7%), cancer surgery (56.9%), and cancer immunotherapy (43.1%; Table 1).
TABLE 1.
The Sociodemographic Characteristics of the Respondents
| Variable | Frequency | % |
|---|---|---|
| Sex (n = 52) | ||
| Male | 32 | 61.5 |
| Female | 20 | 38.5 |
| Years worked as oncologist (n = 50) | ||
| <5 | 25 | 50.0 |
| 5-9 | 9 | 18.0 |
| 10-14 | 10 | 20.0 |
| 15+ | 6 | 12.0 |
| Missing | 2 | — |
| Country of practice (n = 52) | ||
| Carbo Verde | 1 | 1.9 |
| Ethiopia | 1 | 1.9 |
| Ghana | 6 | 11.5 |
| Kenya | 8 | 15.4 |
| Malawi | 4 | 7.7 |
| Mauritius | 1 | 1.9 |
| Mozambique | 1 | 1.9 |
| Morocco | 1 | 1.9 |
| Niger | 1 | 1.9 |
| Nigeria | 3 | 5.8 |
| Rwanda | 6 | 11.5 |
| Senegal | 1 | 1.9 |
| Sudan | 1 | 1.9 |
| Tanzania | 10 | 19.2 |
| Uganda | 3 | 5.8 |
| Zambia | 3 | 5.8 |
| Zimbabwe | 1 | 1.9 |
| Treatment offered (n = 51) | ||
| Cancer surgery | 29 | 56.9 |
| Chemotherapy | 46 | 90.2 |
| Radiotherapy | 32 | 62.7 |
| Cancer immunotherapy | 22 | 43.1 |
| Missing | 1 | — |
| Oncology specialty (n = 52) | ||
| Clinical oncology | 26 | 50.0 |
| General surgery | 2 | 3.8 |
| Gynecology | 2 | 3.8 |
| Hematology | 3 | 5.8 |
| Medical oncology | 7 | 13.5 |
| Others | 7 | 13.5 |
| Pediatric oncology | 2 | 3.8 |
| Radiation oncology | 3 | 5.8 |
Referral Patterns by the Respondents
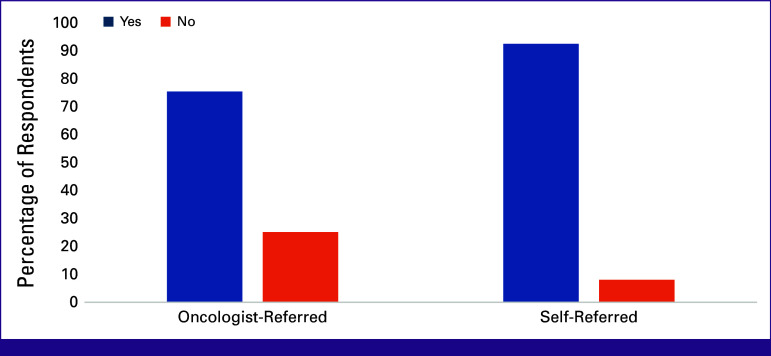
The referral pattern of patients for cancer treatment is shown in Figure 1. The majority (92%) of study participants reported that they know patients who refer themselves, whereas 75% reported having referred patients abroad for cancer treatment. Respondents in Southern Africa had the highest average number (10.0 [3.5-13.5]) of yearly referrals for cancer treatment abroad, whereas respondents from North Africa had the lowest (0.5 [0.0-1.0]; Table 2).
FIG 1.
The prevalence and pattern of referral for cancer treatment.
TABLE 2.
Regional Referrals for Cancer Medical Tourism
| Variable | Average No. of Patients Referred Abroad Per Year |
|---|---|
| East Africa—median (IQR) | 3.5 (1.0-5.75) |
| West Africa—median (IQR) | 2.0 (1.0-7.0) |
| North Africa—median (IQR) | 0.5 (0.0-1.0) |
| South Africa—median (IQR) | 10 (3.5-13.5) |
| Total—median (IQR) | 3.5 (1.0-10.0) |
The referral destinations of patients for cancer treatment are shown in Figure 2. When asked where they mostly refer patients, the most common (94%) referral destination was India, followed by African countries (38.5%). For referrals within Africa, the most common destinations were South Africa (75%), Kenya (25%), Tunisia (10%), Morocco (10%), and Tanzania (10%).
FIG 2.
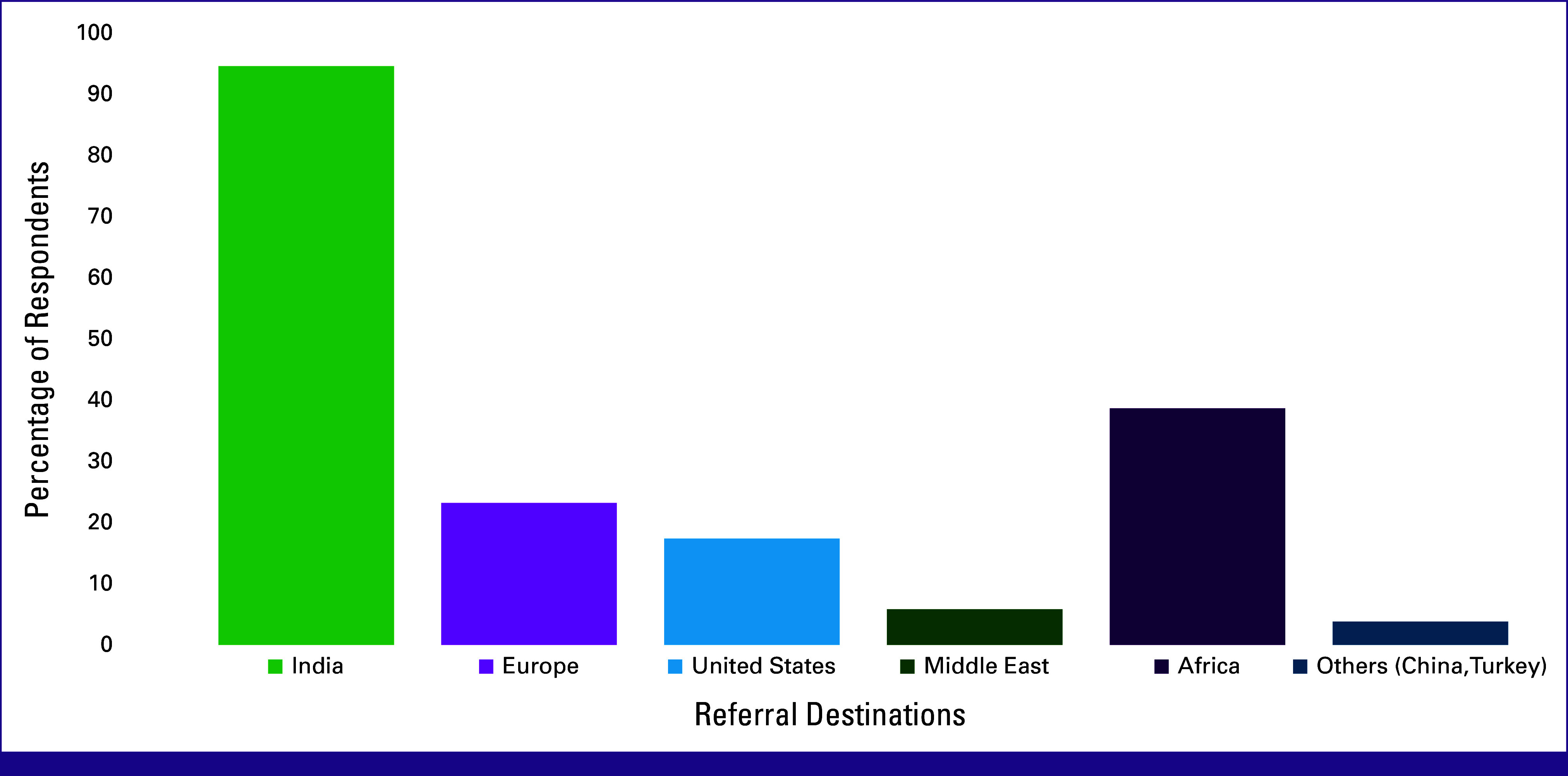
Destination of cancer care referrals.
Oncologists’ Perception and Factors Affecting Referrals
The responses were on a scale of 1-7, with 1 being most common and 7 being least common. However, for the purpose of reporting, we grouped 1-3 as most common, 4 as neutral, and 5-7 as least common. When the respondents were asked why African patients with cancer receive treatment abroad rather than in their local health institution, the most common (93%) reason was perception of a higher quality of care in foreign health institutions. This is closely followed by mistrust in the local health system (71%, 30/42) and social prestige or affluence associated with international treatment (61%, 25/41; Table 3).
TABLE 3.
Respondents’ Perceptions of Patients Who Self-Refer for Oncology Treatment Abroad
| Variable | N | Rating | ||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
| Reasons why patients self-refer for treatment abroad rather than receive treatment locally from most common (1) to least common (7) | ||||||||
| Mistrust in system | 42 | 12 (28.6) | 10 (23.8) | 8 (19.0) | 3 (7.1) | 4 (9.5) | 4 (9.5) | 1 (2.4) |
| Solicitation from referral system abroad | 40 | 2 (5.0) | 2 (5.0) | 11 (27.5) | 8 (20.0) | 7 (17.5) | 6 (15.0) | 4 (10.0) |
| Perception of higher quality of care abroad | 43 | 25 (58.1) | 10 (23.3) | 3 (7.0) | 2 (4.7) | — | — | 3 (7.0) |
| Perception of better provider communication abroad | 42 | 5 (11.9) | 6 (14.3) | 6 (14.3) | 9 (21.4) | 9 (21.4) | 7 (16.7) | — |
| Fear of stigma | 41 | 1 (2.4) | 3 (7.3) | 5 (12.2) | 5 (12.2) | 9 (22.0) | 13 (31.7) | 5 (12.2) |
| Social prestige or affluence associated with international treatment | 41 | 6 (14.6) | 7 (17.1) | 12 (29.3) | 6 (14.6) | 5 (12.2) | 3 (7.3) | 2 (4.9) |
| Lower cost of services abroad | 41 | 3 (7.3) | 1 (2.4) | — | 2 (4.9) | 2 (4.9) | 5 (12.2) | 28 (68.3) |
| Cancer type with the most unwarranted self-referrals (1) to cancer type with the fewest (6) | 1 | 2 | 3 | 4 | 5 | 6 | ||
| Breast self-referrals | 43 | 21 (48.8) | 9 (20.9) | 5 (11.6) | 1 (2.3) | 4 (9.3) | 3 (7.0) | — |
| Colorectal self-referrals | 43 | 4 (9.3) | 12 (27.9) | 11 (25.6) | 6 (14.0) | 8 (18.6) | 2 (4.7) | — |
| Cervix self-referrals | 43 | 2 (4.7) | 8 (18.6) | 4 (9.3) | 1 (2.3) | 6 (14.0) | 22 (51.2) | — |
| Prostate self-referrals | 43 | 7 (16.3) | 8 (18.6) | 10 (23.3) | 9 (20.9) | 5 (11.6) | 4 (9.3) | — |
| Head and neck self-referrals | 43 | 4 (9.3) | 5 (11.6) | 5 (11.6) | 8 (18.6) | 13 (30.2) | 8 (18.6) | — |
| Hematological malignancies self-referrals | 43 | 11 (25.6) | 5 (11.6) | 2 (4.7) | 7 (16.3) | 6 (14.0) | 12 (27.9) | — |
| Challenges patients face when self-referring (1 being the greatest challenge and 7 being the smallest) | ||||||||
| Receiving lower quality care | 42 | 3 (7.1) | 2 (4.8) | 1 (2.4) | 5 (11.9) | 7 (16.7) | 5 (11.9) | 19 (45.2) |
| Aggressive, unwarranted treatment | 43 | 7 (16.3) | 5 (11.6) | 11 (25.6) | 7 (16.3) | 5 (11.6) | 7 (16.3) | 1 (2.3) |
| Overuse of tests | 43 | 12 (27.9) | 11 (25.6) | 5 (11.6) | 3 (7.0) | 6 (14.0) | 5 (11.6) | 1 (2.3) |
| Expenses—treatment, travel, accommodation | 45 | 33 (73.3) | 4 (8.9) | 3 (6.7) | 1 (2.2) | 1 (2.2) | 1 (2.2) | 2 (4.4) |
| Loss of continuity of care | 43 | 6 (14.0) | 11 (25.6) | 11 (25.6) | 7 (16.3) | 4 (9.3) | 2 (4.7) | 2 (4.7) |
| Loss of valuable time | 44 | 2 (4.5) | 6 (13.6) | 6 (13.6) | 6 (13.6) | 13 (29.5) | 8 (18.2) | 3 (6.8) |
| Poor outcomes/complications of treatment from inadequate follow-up | 44 | 3 (6.8) | 4 (9.1) | 5 (11.4) | 7 (15.9) | 7 (15.9) | 9 (20.5) | 9 (20.5) |
Breast cancer (49%, 21/43), hematological malignancies, (26%, 11/43), and prostate cancer (16%, 7/43) are the three types of cancer for which the respondents thought patients' self-referral for treatment abroad was unwarranted.
The respondents rated treatment, travel, accommodation expenses (73%, 33/45), and the overuse of tests (28%, 12/43) as the greatest challenges patients face when they refer themselves for cancer treatment abroad (Table 3).
Table 4 shows that 56.5% (n = 26/50) of the respondents agree that when patients with cancer refer themselves for treatment abroad, the referral is justified. Almost half (46.9%, 23/49) of the respondents believe that unwarranted self-referrals by patients with cancer are less prevalent when compared with the past.
TABLE 4.
Perceptions of the Respondents About the Validity of Self-Referrals for Cancer Treatment Abroad
| Variable | Frequency | % |
|---|---|---|
| Agreement—self-referral abroad is valid (n = 50) | ||
| Strongly agree | 10 | 21.7 |
| Agree | 16 | 34.8 |
| Neither agree nor disagree | 10 | 21.7 |
| Strongly disagree | 2 | 4.3 |
| Disagree | 8 | 17.4 |
| Missing | 2 | — |
| Are patients traveling abroad with unwarranted self-referrals (n = 49) | ||
| Less frequently than in the past | 23 | 46.9 |
| More frequently than in the past | 16 | 32.7 |
| The same amount as always | 10 | 20.4 |
| Missing | 3 | — |
The majority (51%, 24/47) of respondents refer their patients with cancer for treatment abroad because of greater availability of technology (eg, radiotherapy), followed by the availability of more skilled workforce in the receiving country (23.4%, 11/47) and higher quality of care in the receiving country (15%, 7/47). A third of respondents reported to have been influenced to refer a high-profile patient abroad for cancer treatment (Table 5).
TABLE 5.
Factors That Influence Referrals for Cancer Treatment Abroad
| Variable | Frequency | % |
|---|---|---|
| Primary influence on your decision to refer a patient abroad for cancer care (n = 47) | ||
| Greater availability of care providers in receiving country | 1 | 2.1 |
| Greater availability of medicine in receiving country | 3 | 6.4 |
| Greater availability of technology (ie, radiotherapy) | 24 | 51.1 |
| Higher quality of care in receiving country | 7 | 14.9 |
| Lower cost of care in receiving country | 1 | 2.1 |
| More skilled/specialized workforce in receiving country | 11 | 23.4 |
| Missing | 5 | — |
| Primary influence on patients deciding to self-refer abroad for cancer care (n = 50) | ||
| Greater availability of care providers in receiving country | 1 | 2.0 |
| Greater availability of medicine in receiving country | 2 | 4.0 |
| Greater availability of technology (ie, radiotherapy) | 15 | 30.0 |
| Higher quality of care in receiving country | 10 | 20.0 |
| Lower cost of care in receiving country | 1 | 2.0 |
| Mistrust in local system | 11 | 22.0 |
| More skilled/specialized workforce in receiving country | 10 | 20.0 |
| Missing | 2 | — |
| Have you been influenced to refer a high-profile patient for treatment abroad (n = 51) | ||
| Yes | 15 | 29.4 |
| No | 36 | 70.6 |
| Missing | 1 | — |
| Do you receive any incentives to refer patients abroad? (n = 52) | ||
| Yes—by receiving hospital | 1 | 1.9 |
| No | 51 | 98.1 |
| Have you ever been pressured or bribed to refer a patient abroad? (n = 52) | ||
| Yes—by a patient | 5 | 9.6 |
| Yes—by a receiving hospital | 3 | 5.8 |
| No | 44 | 84.6 |
Concerning the awareness of the respondents about outside centers soliciting their patients for referral, most (52%, 23/48) are not aware. Those aware (48%, 23/48) mentioned ads of better treatment, solicitations from foreign health care facilities, organized screening by foreign hospitals and online consults, and social media as examples of solicitations (Table 6). The majority (86%, 44/51) agree that their patients seeking medical care abroad constitutes some economic loss to their country.
TABLE 6.
Oncologists’ Awareness About Solicitation for Referrals and Economic Impact of Referrals
| Variable | Frequency | % |
|---|---|---|
| Are you aware of your patients being solicited for referrals from outside centers? (ie, advertisement of better medical treatment in the destination country) (n = 48) | ||
| Yes (please list examples) | 23 | 47.9 |
| No | 25 | 52.1 |
| Missing | 4 | — |
| Examples of solicitations (n = 19) | ||
| Ads of better treatment | 1 | 5.2 |
| Solicitations from foreign health care facilities | 15 | 78.9 |
| Organized screening by foreign hospitals and online consults | 1 | 5.2 |
| Social media | 1 | 5.2 |
| Through medical insurance companies | 1 | 5.2 |
| Missing | 4 | — |
| Agreement with statement: There is economic loss in my country due to patients traveling abroad (n = 51) | ||
| Strongly agree | 25 | 49.0 |
| Agree | 19 | 37.3 |
| Neither agree nor disagree | 5 | 9.8 |
| Disagree | 2 | 3.9 |
| Strongly disagree | — | — |
| Missing | 1 | — |
Government and Cancer Medical Tourism
Fifty-five percent (n = 28/52) of the respondents reported that their governments sponsor referral abroad for cancer treatment. Of the respondents whose governments sponsor referrals, the majority (71%, 20/28) reported that most referrals are for complex oncologic surgeries. Sixty-one percent (17/28) reported bone marrow transplant (60.7%), 39% (11/28) liver transplant, and 39% (11/28) radiotherapy. Among the cancer types that are commonly referred through government sponsorship, 46% (13/28) reported breast cancer, 39% (11/28) leukemia, 36% (10/28) multiple myeloma, 29% (8/28) colorectal cancer, and 29% (8/28) prostate cancer (Table 7).
TABLE 7.
The Role of the Government in Medical Tourism in the Country of the Respondents
| Variable | Frequency | % |
|---|---|---|
| Government has a sponsorship program for referring patients abroad | ||
| Yes | 28 | 54.9 |
| No | 23 | 45.1 |
| Missing | 1 | — |
| Government-sponsored abroad treatment types (n = 28) | ||
| Bone marrow transplant | 17 | 60.7 |
| Liver transplant | 11 | 39.3 |
| Complex oncologic surgeries | 20 | 71.4 |
| Brachytherapy | 7 | 25.0 |
| Radiotherapy | 11 | 39.3 |
| Chemotherapy for all cancers | 5 | 17.9 |
| Chemotherapy for certain cancers | 6 | 21.4 |
| Immunotherapy | 9 | 32.1 |
| Others | 9 | 32.1 |
| Government-sponsored abroad cancer types (n = 28) | ||
| Bladder | 0 | 0.0 |
| Breast | 13 | 46.4 |
| Cervical | 3 | 10.7 |
| CNS | 5 | 17.9 |
| Colorectal | 8 | 28.6 |
| Eye | 1 | 3.6 |
| Kidney | 1 | 3.6 |
| Larynx | 4 | 14.3 |
| Leukemia | 11 | 39.3 |
| Liver | 4 | 14.3 |
| Lung | 5 | 17.9 |
| Lymphoma | 6 | 21.4 |
| Melanoma | 3 | 10.7 |
| Multiple myeloma | 10 | 35.7 |
| Esophageal | 4 | 14.3 |
| Ovarian | 1 | 3.6 |
| Pancreatic | 3 | 10.7 |
| Prostate | 8 | 28.6 |
| Stomach | 2 | 7.1 |
| Testicular | 0 | 0.0 |
| Thyroid | 3 | 10.7 |
| Other | 3 | 10.7 |
| What elements of care are covered by the government? (n = 28) | ||
| Medical bill and transport | 5 | 17.9 |
| Medical bill and living expenses | 1 | 3.6 |
| Medical bill only | 8 | 28.6 |
| Medical bill, living expenses and transport | 14 | 50.0 |
| When referring a patient abroad for government-sponsored treatment, is there a regulatory board/committee or approval mechanism in place that you adhere to? (n = 28) | ||
| Yes | 25 | 89.3 |
| No | 1 | 3.6 |
| Unsure | 2 | 7.1 |
| How equitable is the state-sponsored referral process? (n = 28) | ||
| Occasionally, patients who do not satisfy criteria are sponsored | 1 | 3.8 |
| Only those who satisfy criteria are sponsored | 12 | 46.2 |
| Patients with connections and affluence are more likely to be sponsored | 13 | 50 |
| Missing | 2 | — |
Half (50%, 14/28) of the respondents reported that government sponsorship covers medical bills, living expenses, and transport; 29% (8/28) of respondents reported that their government sponsorship covers medical bills only; and 18% (5/28) reported that their government sponsorship covers medical bills and transport. A large proportion (89.3%, 25/28) of respondents noted having a regulatory board or approval mechanism that they adhere to. Half (50%, 13/26) of the respondents reported that patients with connections and affluence are more likely to be sponsored by the State for treatment abroad. Eight respondents (15%) reported to have been directly bribed by either the patients or the receiving hospitals or pressured by government officials (those receiving government support) to refer a patient abroad (Table 6).
DISCUSSION
This study aimed to explore the status of cancer medical tourism in Africa. According to the responses from the cancer care providers surveyed, five major findings were identified. First, the majority of self-referrals for treatment abroad are primarily due to a perception of a higher quality of care in foreign health institutions. Second, oncologists in Africa refer patients abroad predominantly because of the greater availability of technology, such as radiotherapy. Third, in surveyed participants, India is the most common destination for patients with cancer from Africa seeking cancer treatment abroad. Fourth, ethical concerns and challenges, including loss of continuity in care, significant treatment expenses, and inequity in access to government-sponsored medical tourism, are prevalent. Fifth, medical tourism is associated with economic losses for African countries. These findings align with existing literature. The trend of self-referral and physician referrals for treatment abroad due to perceived higher quality and availability of technology is consistent with findings in global studies on medical tourism. However, as reported by Al-Shamsi et al,14 it remains questionable whether patients go to seek specialized care abroad or whether, as shown by our study, they seek care abroad due to a lack of trust in their local health care system. It is estimated that only 10% of self-referred patients with cancer truly go to seek specialized care that is unavailable in the local settings.14 Benedetti et al15 also suggest that the main reasons for medical tourism include seeking second opinion, enrollment in clinical trials, and specialized care unavailable in the referring country. Concerns shared by several cancer physicians in Africa align with concerns listed by Benedetti et al15 that medical tourism can pose an impediment to optimal care. The author reports these kinds of referrals are associated with delays, as some receiving hospitals face challenges of incomplete data and may need to restart investigations. Additionally, logistical complications may cause further delays, such as receiving approvals from local sponsoring agencies or acquiring visas. These delays can result in disease progression.15
Our findings indicate that India is the most common destination that has been previously reported by several other authors. For example, Zakaria et al16 found that three fourths of their study participants had self-referred to India for treatment. India has positioned itself as a medical tourism destination for both low- and high-income countries.17 The majority of patients in the study by Zakaria et al16 noted availability of highly experienced doctors, low cost of medical treatment and facilities, and the ability to get high-quality, fast services as some of the pulling factors of patients to India. Many of our respondents acknowledged the potential economic losses to their home countries that may occur because of medical tourism. The annual expenditure of Nigerians on international health services is estimated to be $1 billion in US dollars with 60% of the money spent on oncology, orthopedics, nephrology, and cardiology.18 At the level of the individual patients and families, the financial toxicities and catastrophic expenditure associated with medical tourism can be staggering for middle- and low-middle-class families who are not affluent enough and may exhaust their resources in seeking care abroad. This further exacerbates social inequalities and needs to be investigated. Inequities are also seen when government resources for medical tourism are diverted to affluent and influential patients, thus compounding economic losses.
Despite its value for treatments and diagnostics not locally available, medical tourism in cancer care is not without challenges. Concerns regarding the quality and safety of care, including the consistency of standards, postoperative complications, and infection rates, remain significant. These concerns are compounded by ethical issues, such as the potential diversion of health care resources in the host country from the local population to foreign patients.14,15 Moreover, the continuity of care poses a challenge, especially when patients return to their home countries and face difficulties receiving follow-up treatment or managing complications.19 Managing postmedical tourism complication can increase the workload of local providers and the risk of financial toxicities for patients and burden the overall health system.20 This aspect of medical tourism, including the legal and ethical ramifications, is often overlooked in the decision-making process, underscoring a need for a more holistic consideration of patient care.
It is notable that the trend of self-referral indicates a significant trust deficit in local health care systems, possibly due to perceived inadequacies in care quality and technology. The preference for health systems abroad as a medical tourism destination may reflect competitive advantage in offering cost-effective yet technologically advanced medical treatments. However, there are concerns regarding the active solicitation of patients by foreign health systems and the variation in quality of care provided. Finally, the economic implications of medical tourism underscore a paradox where the pursuit of high-quality health care abroad by a few potentially undermines the health care system's robustness in the home country, diverting much-needed resources and attention.
To our knowledge, this is the first study exploring cancer provider's perceptions on medical tourism in SSA, and it has several limitations. First, there could be biases in respondent selection. Second, there is lack of patients' voice included in this study, as qualitative methodologies were not used. Third, the study sample is relatively small and does not include representation from all African countries, thus limiting the study's generalizability to all of Africa. Fourth, the survey was conducted in English only, which could have limited participation by non–English-speaking providers. Finally, we did not have a precise number of total oncologists/surgeons or other physician treating cancers in SSA as a denominator; hence, we cannot ascertain the response rate.
The study's findings suggest a need for policy interventions at both national and regional levels in Africa. Improving local health care systems, particularly cancer care infrastructure and technology, could mitigate the need for medical tourism. For example, government-sponsored complex cancer surgery accounts for 70% of the referral, highlighting gap in cancer surgery and the potential return on investment in upscaling cancer treatment infrastructure and workforce. If medical tourism is to continue, there is a need for the implementation of ethical guidelines and regulatory frameworks to govern medical tourism and protect the interests of patients and local health care systems. Promoting regional medical tourism within Africa accompanied by robust legal and financial governmental agreements could be a strategic approach to retain health care expenditures within the continent. In addition, our findings highlight the need for further research in the medical, ethical, and economic ramifications of medical tourism in Africa both at the level of the individual patient, their families, and community and at the national and regional levels.
In conclusion, this study sheds light on the complex dynamics of medical tourism for cancer treatment from Africa, highlighting critical areas for improvement in local health care systems, ethical considerations, and disproportionate economic effects. The findings provide a foundation for policymakers and health care providers to develop strategies that balance the benefits of global health care access with the sustainability and efficacy of local health systems in SSA. However, further studies on this topic targeting diverse groups such as French-speaking countries, North Africa, patient advocacy groups, and policymakers are needed.
AUTHOR CONTRIBUTIONS
Conception and design: Fidel Rubagumya, Laura Carson, Eulade Rugengamanzi, Nazik Hammad
Administrative support: Laura Carson, Daniel Afolayan, Godwin Abdiel Nnko
Provision of study materials or patients: Fidel Rubagumya, Godwin Abdiel Nnko
Collection and assembly of data: Fidel Rubagumya, Daniel Afolayan, Eulade Rugengamanzi, Godwin Abdiel Nnko, Omar Abdihamid, Verna Vanderpuye, Nazik Hammad
Data analysis and interpretation: Fidel Rubagumya, Daniel Afolayan, Eulade Rugengamanzi, Verna Vanderpuye, Nazik Hammad
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Fidel Rubagumya
Research Funding: Pfizer, Conquer Cancer, the ASCO Foundation
Verna Vanderpuye
Other Relationship: Elsevier, BIO USAWA
No other potential conflicts of interest were reported.
REFERENCES
- 1.Cancer Today. https://gco.iarc.who.int/today/ [Google Scholar]
- 2.WHO : WHO Report on Cancer: Setting Priorities, Investing Wisely and Providing Care for All. 2020. https://www.who.int/publications-detail-redirect/9789240001299 [Google Scholar]
- 3.Fundytus A, Sullivan R, Vanderpuye V, et al. : Delivery of global cancer care: An International Study of Medical Oncology Workload. JCO Glob Oncol 10.1200/JGO.17.00126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fundytus A, Sengar M, Lombe D, et al. : Access to cancer medicines deemed essential by oncologists in 82 countries: An International, Cross-Sectional Survey. Lancet Oncol 22:1367-1377, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barrios C, de Lima Lopes G, Yusof MM, et al. : Barriers in access to oncology drugs—A global crisis. Nat Rev Clin Oncol 20:7-15, 2023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bazargani YT, Ugurlu M, de Boer A, et al. : Selection of essential medicines for the prevention and treatment of cardiovascular diseases in low and middle income countries. BMC Cardiovasc Disord 18:126, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abdel-Wahab M, Bourque JM, Pynda Y, et al. : Status of radiotherapy resources in Africa: An International Atomic Energy Agency analysis. Lancet Oncol 14:e168-e175, 2013 [DOI] [PubMed] [Google Scholar]
- 8.Elmore SNC, Polo A, Bourque JM, et al. : Radiotherapy resources in Africa: An International Atomic Energy Agency update and analysis of projected needs. Lancet Oncol 22:e391-e399, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baldomero H, Aljurf M, Zaidi SZA, et al. : Narrowing the gap for hematopoietic stem cell transplantation in the East-Mediterranean/African region: Comparison with global HSCT indications and trends. Bone Marrow Transplant 54:402-417, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klímová B, Kuča K: Medical tourism: Its research and implications for public health. Cent Eur J Public Health 28:226-229, 2020 [DOI] [PubMed] [Google Scholar]
- 11.Medical Tourism Market Size, Share | Growth | Forecast—2032. https://www.alliedmarketresearch.com/medical-tourism-market [Google Scholar]
- 12.Rotem A, Toker A, Mor-Yossef S: [Medical tourism: Changing a world trend into a national resource]. Harefuah 148:30-33, 2009, 88 [PubMed] [Google Scholar]
- 13.Mogaka JJO, Mupara L, Tsoka-Gwegweni JM: Ethical issues associated with medical tourism in Africa. J Mark Access Health Policy 5:1309770, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al-Shamsi HO, Al-Hajeili M, Alrawi S: Chasing the cure around the globe: Medical tourism for cancer care from developing countries. JCO Glob Oncol 10.1200/JGO.17.00087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Benedetti DJ, Golshan M, Kesselheim JC: Going the distance: Ethical issues arising when patients seek cancer care from international settings. JCO Glob Oncol 10.1200/JGO.17.00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zakaria M, Islam MA, Islam MK, et al. : Determinants of Bangladeshi patients’ decision-making process and satisfaction toward medical tourism in India. Front Public Health 11:1137929, 2023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nisa H, Sharma DSK: Status and growth of medical tourism in India. J Namib Stud Hist Polit Cult 35:5004-5011, 2023 [Google Scholar]
- 18.Abubakar M, Basiru S, Oluyemi J, et al. : Medical tourism in Nigeria: Challenges and remedies to health care system development. Int J Dev Manag Rev 13:225, 2018 [Google Scholar]
- 19.Moghavvemi S, Mogan K, Ghazali EM: The issue, challenges and risk of post- surgery treatment abroad among medical tourists from doctors’ perspective. J Qual Assur Hospitality Tourism 45:1-32, 2023 [Google Scholar]
- 20.Adeoye AO: Assessing the associated medical, legal, and social issues in medical tourism and its implications for Nigeria. Pan Afr Med J 45:145, 2023 [DOI] [PMC free article] [PubMed] [Google Scholar]